Burns- A comprehensive discussion
- 1. BURNS A Comprehensive Discussion Dr Avijit Banerjee( Surgery PGT SOUTH EASTERN RAILWAY) Dr Anjana Malhotra ( MS,MCh,DNB)
- 2. History • A 45 year old gentleman was brought to the casualty of BNR hospital on 27th March of 2017 at 10:00AM • He had an accidental burn while he was cooking in his kerosene fuelled stove oven, which burst into flames due to probable mishandling • Intravenous access was achieved in the casualty itself and fluid resuscitation was started. • Primary dressing was done as he was transferred to the Burns ICU
- 3. On examination The TBSA was estimated by using the Wallace “rule- of-nines” Depth of wound was assessed
- 7. • He had an approximately 55% burn of which 30% was full thickness and 25% was mixed superficial and deep dermal. • Initial fluid resuscitation was planned according to Parkland formula, with the help of crystalloids in the 1st 24 hours.
- 9. Acute Fluid Management of Large Burns
- 10. Zone of coagulation Zone of stasisZone of hyperaemia Burn Zones
- 11. Pathophysiology : Overview Suppressed Cardiac Output Electrolyte imbalances because of intercellular ion shifts in burnt tissue Insulin and cortisol requirements increase Hyperglycemia If hypovolemia is not corrected GI and Renal Systems are the first to be affected
- 12. Local Response In Burnt Tissue Histamine, prostaglandins and bradykinin Locally altered connections in the basement membrane and increased endothelial permeability Transudation of large osmotically active intravascular protein out of the capillaries into burnt tissue causing leakage of water from capillary circulation into burnt tissue-LOCAL BURN WOUND OEDEMA Integrins are broken -> exposure of hydrophilic proteoglycans -> Further water is driven into interstitial space
- 13. Pathophysiology Release of CYTOKINES from burnt wound Interleukin 1,8 ; TNF –alpha -> leukocytes are attracted to wound -> Neutrophil degranulation Release of proteases and Free Radicles (Reactive oxygen species/ROS) Cytotoxic to normal tissue Complement Activation Further disruption of dermal microvasculature Local tissue necrosis
- 14. Systemic Response Large volume release of cytokines and inflammatory mediators leads to leaky microvasculature, vasodilatation and reduced CO Profound efflux of intravascular volume into the interstitial space Capillary integrity of the nonburned tissue returns to normal at 24 HOURS. But, water continues to collect in the interstitial space of non burned tissue because of decreased oncotic pressure due to loss of plasma protein into the burnt tissue
- 15. CARDIAC Massive cytokine release -- -Vasodilatation Low C.O and hypo perfusion Deranged Zone of stasis RFT tissue death DYSFUNCTION Decrease in Circulating blood volume due to serum loss
- 16. RESUSCITATION 1) MAINTAIN END ORGAN PERFUSION BY FLUID RESUSCITATION Until vascular permeability is restored and interstitial losses are minimized. Takes upto 48 Hours in burned area 2) LIMITING FLUID OVERLOAD - Pulmonary edema - Abdominal compartment syndrome - Conversion of partial thickness to full thickness burns
- 18. RESUSCITATION CRYSTALLOIDS - RINGERS LACTATE Na+ (130 meq/L) K+ (4 meq/L) Although hypo-osmolar when compared to plasma it is effective at restoring extracellular sodium deficits - Lactate is metabolized in the liver to Hco3- (Alkalinizing effect)
- 19. RESUSCITATION - NORMAL SALINE - Not Used because Na+ and Cl- dissociate to cause ACIDEMIA which worsens the lactic acidosis in the first 24 hours - HYPERTONIC SALINE - Was used as it was thought it may decrease the requirement of fluid and compartment syndrome and edema caused -> Hypernatremia -> Renal failure -> Increased mortality NO ROLE NOW
- 20. RESUSCITATION - Colloids are added when 1) PARKLAND not enough to resuscitate 2) Albumin (< 1.2- 1.5 g/dl) because of massive fluid intake -> 5% Albumin is usually administered Usually given after 24hours in the ratio of 1:3 with crystalloids
- 21. RESUSCITATION High dose ASCORBIC ACID during the first 24 hours * Decreases fluid volume needed Side effects – Oxalate nephropathy
- 22. Monitoring RESUSCITATION TRADITIONAL 1- UOP 2- MAP 3- Serum Lactate * increased mortality if elevated even after 48 hours * If normalizes by-24 hours increased survival rates 4 - CVP – Not reliable 5 - PCWP RECENT 1- TRANSPULMONARY THERMODILUTION 2- PULSE CONTOUR ANALYSIS 3- TRANS OESOPHAGEAL ECHOCARDIOGRAPHY 4- PERCUTANEOUS GAS TENSION OF THE SKIN
- 23. Monitoring RESUSCITATION 1- Trans Pulmonary Thermo Dilution (TPTD) * No cardiac disease * Patient – paralyzed and should be on ventilator Needs a Central Line and Arterial line 2- Pulse Contour Analysis (PCA) * Measures the Intra Thoracic Blood Volume -> more fluids - > more edema * No benefit in survival Needs an arterial line
- 24. Monitoring RESUSCITATION 3- TRANS OESOPHAGEAL ECHOCARDIOGRAPHY * Systematic review by Maybauer et al -> No improvement in outcome 4- PERCUTANEOUS GAS TENSION OF THE SKIN Measured using a FIBREOPTIC device in the skin * Subcutaneous pH is a marker of poor skin perfusion *Reduction occurred before decrease in MAP
- 25. • Since patient came with singed nasal vibrissae and burns of his face we evaluated him for any inhalation injury
- 26. INHALATION INJURY 1- Present in 1/3rd to 1/2 of all burn injuries, but accounts for 90% of all burn related mortality 2- Burn critical care units have highest rates of ventilator associated pneumonia & probability of death increases from 40- 60% when a burn patient of inhalation injury has pneumonia
- 27. Mechanism of Destruction 1- Upper airway injury 2- Lower airway injury 3- Pulmonary parenchymal injury 4- Systemic toxicity
- 28. Mechanism of Destruction 1- Upper airway injury : Heat denaturates protein Activates complement cascade & release of Histamine Release of Xanthine oxidase and release of ROS Combine with Nitric oxide (NO) in the endothelium to produce airway edema Pro inflammatory cytokines attract neutrophils to that area Further increase in ROS *Further fluid resuscitation increases edema
- 29. Mechanism of Destruction 2- Lower airway : Usually protected by the upper airway except if there are chemicals in the smoke 3- Lung Parenchyma Injury Injuries are delayed & depend on the severity of the inhalation injury & patient’s response to it Edema , decreased pulmonary compliance from extra vascular lung water & pulmonary lymph inactivation of surfactant Ventilation perfusion mismatch leading to Hypoxia and ARDS 4- Systemic Toxicity Chemicals /cytotoxic liquid
- 30. Diagnosis of Inhalation Injury Grade Class Description 1 No injury Absence of carbonaceous deposits, erythema, edema, bronchorrhea or obstruction 2 Mild injury Minor or patchy areas of carbonaceous deposits, erythema, bronchorrhea or bronchial obstruction 3 Moderate injury Moderate degree of erythema, carbonaceous deposits, bronchorrhea or bronchial obstruction 4 Severe injury Severe inflammation with friability, copious carbonaceous deposits, bronchorrhea or obstruction 5 Massive injury Evidence of mucosal sloughing, necrosis, endoluminal obstruction
- 31. Conservative management 1- Bronchodilatation 2- Muscarinic receptor antagonist Ipratropium or Tiotropium 3- Nebulization – - NAC 20% - 3ML - Heparin 5000-10,000 Alternating every 4 hours Anti-oxidants and free radical scavenger
- 32. Inhalation injury – Ventilatory management
- 33. Intubation: Early Vs Late • Thermal Injury to upper airway – Extensive fascial & circumferential neck burns – high risk of rapid airway oedema formation – catastrophic obstruction • Early Intubation – prevent hypoxic injury • Tube fixation – adhesive tapes will not stick to extensive burn areas, so cotton ties
- 34. Tracheostomy Vs Intubation • Full thickness burns to the face requiring reconstruction with TBSA greater than 60% • Acute loss of airway • Prolonged respiratory failure
- 35. Conventional Ventilation • Low tidal volume : 6 – 8 ml/kg, monitor peak pressure & mean airway pressure (Target < 30) • Respiratory Rate : 10 – 18 breaths per minute • PEEP: 4 – 8 cm H2O • FiO2: Initially 100% & gradually decrease upto 35%
- 36. Supportive Care • Regular airway suctioning • Therapeutic bronchoscopy with aggressive pulmonary toilet to remove copious secretion • Therapeutic coughing & chest physiotherapy • Oral care • Regular changing of posture • Early Ambulation
- 37. Monitoring • Regular ABG • Bronchoscopy • Daily Chest Radiography • Hemodynamic monitoring
- 38. HFPV • High Frequency Percussive Ventilation – VDR, Volumetric Diffuse Respiratory Ventilator • Combines both subtidal, high frequency (400 – 1000 breaths per min) and tidal, low frequency (0 – 20 breaths per min) • Effective in providing positive airway pressure with lower peak and mean pressure - ↑FRC – better gas exchange
- 39. APRV • Airway Pressure Release Ventilation • Continuous positive pressure at high levels and intermittent release of airway pressure • More effective alveolar recruitment – due to lower peak but higher mean airway pressure
- 40. PRVC • Pressure Regulated Volume Control • Adjust the pressure support over the course of few breaths to achieve a preset tidal volume
- 41. ECMO • Extracorporeal membrane oxygenation (ECMO) • Considered - high predicted mortality - High APACHE II score & High Murray score - A PaO2/FiO2 less than 150
- 42. Weaning • Improving oxygenation & better ABG study • Minimum ventilatory support • Haemodynamic stability • SBT: Initially 1 hour per day & gradually increasing the time period
- 44. • Surgical procedures such as early escharotomy and fasciotomy, followed by burn excision is a key component to the multidisciplinary care of the burn patient. • Early excision and skin grafting to achieve wound closure have been shown to reduce infection rates reduce length of hospital stay improve survival in burn patients
- 45. TIME OF BURN WOUND EXCISION
- 46. Techniques of Burn Wound Excision • EXCISION OF A SMALL BURN • TANGENTIAL EXCISION • FASCIAL EXCISION
- 47. TANGENTIAL EXCISION • The meticulous removal of burned skin while preserving underlying viable tissue • Body contours are better preserved with tangential excision than with fascial-level excision, which removes underlying subcutaneous fat • Originally described by Janzekovic, who observed that deep skin graft donor sites could be grafted with thinner split-thickness skin grafts taken from another area • The Goulian knife, Watson knife, and the Versajet Hydrosurgery System are used for tangential excision • Noninvasive imaging tools available for predicting burn depth and healing time in adult burns include laser Doppler imaging (LDI), which is the current gold standard; infrared thermography (IRT); and spectrophotometric intracutaneous analysis (SIA)
- 50. FASCIAL EXCISION • Skin and subcutaneous tissue are excised en-bloc using electrocautery • Fascial excision can limit the amount of blood loss because control of the deeper perforating vessels is achieved during the excision, bypassing the extensive capillary network present in the skin and subcutaneous tissue • Indicated in cases of life-threatening invasive wound infection or sepsis, particularly fungal infections such as Aspergillus and Mucor
- 51. Fascial-level excision using cutting diathermy
- 52. CONTROLLING BLOOD LOSS DURING BURN EXCISION • The simplest measure is to operate within 24 h of the burn injury • Adjunctive measures to limit blood loss include tourniquets for the extremities, pre-debridement tumescent infiltration with epinephrine solutions, topical application of epinephrine 1: 10 000–1: 20 000, fibrin sealant, autologous platelet gel, calcium-enriched alginate sheets, and immediate bandaging with delayed grafting • Tumescent solution = 1.6 mL of 1 : 1000 epinephrine is added to 500 mL of 0.45% normal saline solution
- 53. Antimicrobial use in burns
- 54. BICU
- 57. Local Anti Microbials SPECTRUM WOUND HEALING HONEY Broad Spectrum Active against fungus . Debriding action . Decreases inflammatory changes . Poor eschar penetration Sodium Hypochlorite Comprehensive . enhances wound healing . Better at 0.0005% SILVER Gram +ve Gram –ve Fungal . Some resistance is emerging . MDR pathogens are resistant MAFENIDE Very good against PSUDOMONAS Penetrates eschar .Sulphur Allergy .Painful application . Metabolic acidosis from CARBONIC ANHYDRASE inhibition
- 59. Antimicrobials in BURN INJURY 1- Defining infection in a patient of burns is challenging in the light of hyper dynamic , hyper metabolic and proinflammatory presentation 2- Clinical pulmonary infection score for pneumonia cannot be adopted & validated in burn patients. So, pneumonia in burns is only diagnosed if clinically suspected & BAL quantitative culture of greater than or equal to 106 colony forming units 3- Local burn wound -> colour change Green Pseudomonas Black/Violet - Invasive infection Loss of graft Conversion of partial thickness to full thickness wounds
- 60. Anti Microbial Use 4- Beware of FUNGAL INFECTION Aspergillus – Grey Brown Candida - Purulent Mucor - Black stain
- 61. SIRS criteria cannot be followed for burn patients ABA Consensus Conference in 2007 , Mann and SALINAS 1- Heart rate > 130 beats /min 2- MAP < 60 mm of Hg 3- Base deficit < -6 4 - Temperature < 36 5 - Vaso active medication required 6- Serum glucose > 150 mg/dl
- 62. BIOMARKERS Procalcitonin - Released within 3 hours of endotoxin exposure & peaks at 14 hours * Released from monocytes - It is normally elevated in burns to three folds > 1.5 ng/ml are specific and sensitive - May be used to see response to treatment and decrease duration of antibiotic usage
- 63. Systemic Anti Microbials - Prophylactic antibiotics not shown to improve mortality - Choose according to the local ANTIBIOGRAM - Hyper metabolism -> changes in Pharmacokinetics and Pharmacodynamics
- 65. TECHNIQUES OF WOUND CLOSURE
- 66. Skin substitutes and bio scaffolds
- 67. Why do we need ● In cases of excessive burn there is paucity of autologus skin especially in lower limb burns. ● Harvesting autologus skin often increases the burn percentage, leading to more derangement of homeostasis.
- 68. WHAT IS THE IDEAL BURN WOUND COVERAGE? • Something that replaces function of dermis and epidermis in full thickness loss. • Able to resist infection • Able to prevent water loss • Able to withstand the shear forces • Cost effective • Widely available • Long shelf life and easy to store • Lack of antigenicity • Flexible in thickness • Durable with long-term wound stability • Can be conformed to irregular wound surfaces • Easy to be secured and applied
- 69. Temporary skin substitutes 1. For dressing on donor sites to facilitate epithelialisation and pain control. 2. For dressing on clean superficial wounds until epithelialisation. 3. To provide temporary physiological closure of deep dermal and full thickness wounds after excision while awaiting autografting. 4. As sandwich graft technique over the widely meshed autografts. 5. As a “test” graft in questionable wound beds.
- 70. CLASSIFICATIONS Class I: Temporary impervious dressing materials a) single layer materials • naturally occurring or biological dressing substitute, e.g. amniotic membrane, potato peel • synthetic dressing substitute, e.g. synthetic polymer sheet (Tegaderm®, Opsite®), polymer foam or spray b) bi-layered tissue engineered materials, e.g. TransCyte®
- 71. Classifications Class II: Single layer durable skin substitutes • Epidermal substitutes, e.g. cultured epithelial autograft (CEA), Apligraft® • Dermal substitutes • bovine collagen sheet, e.g. Kollagen® • porcine collagen sheet • bovine dermal matrix, e.g. Matriderm® • human dermal matrix, e.g. Alloderm®
- 72. Classifications Class III: Composite skin substitutes a) Skin graft • Allograft • Xenograft b) Tissue engineered skin • Dermal regeneration template, e.g. Integra® • Biobrane®
- 73. Amnion ● One of the most effective biological skin substitutes ● Reduces loss of protein, electrolytes and fluids, decreases the risk infection, minimises pain, accelerates wound healing and good handling properties. ● Primarily used for covering partial-thickness burns until complete healing
- 74. Cultured epithelial autografts • The autologous keratinocytes are isolated, cultured and expanded into sheets over periods of 3–5 weeks. • The technique of suspension in fibrin glue has reduced the time for clinical use to 2 weeks. • Avoids the mesh aspect of split skin autografts and discomfort of donor site after skin harvesting. • Limited by the fragility and difficulty of handling, unpredictable take rate and high cost.
- 75. Xenograft • Porcine or amphibian skin. • Can be fresh, refrigerated or lyophilized. • The recent modifications to the porcine skin include aldehyde cross-linking and silver ion impregnation to increase the antimicrobial properties. • Amphibian skin is less allergenic • Never gets taken.
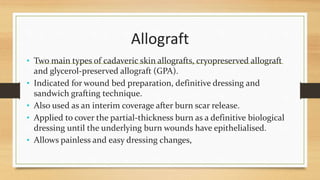
- 76. Allograft • Two main types of cadaveric skin allografts, cryopreserved allograft and glycerol-preserved allograft (GPA). • Indicated for wound bed preparation, definitive dressing and sandwich grafting technique. • Also used as an interim coverage after burn scar release. • Applied to cover the partial-thickness burn as a definitive biological dressing until the underlying burn wounds have epithelialised. • Allows painless and easy dressing changes,
- 78. • Gets revascularized only to be rejected 2-3 weeks. • When the skin allograft is used for sandwich grafting technique to overlay the autograft, the allograft prevents desiccation of the wound bed in the interstices of widely expanded autografts and also reduces bacterial colonisation. The autograft is protected from shear. The epithelialisation of the wound bed is also accelerated when skin allograft is applied.
- 80. Synthetic skin substitutes Integra® Acellular and bilaminar: bovine collagen matrix and chondroitin-6- sulphate (dermal analogous), recovered with a thin lamina of silicone Biobrane Bilaminar: nylon mesh filled with type I porcine collagen and covered by a thin lamina of silicone Apligraft Bilaminar: bovine collagen I populated by live neonatal fibroblasts and covered with a layer of epithelial cells (neonatal keratinocytes) Orcel Keratinocytes and human fibroblasts cultivated separately in type I bovine collagen Alloderm Acellular dermal matrix derived from human skin of cadaver
- 81. INTEGRA
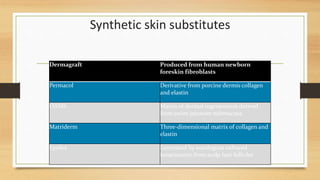
- 82. Synthetic skin substitutes Dermagraft Produced from human newborn foreskin fibroblasts Permacol Derivative from porcine dermis collagen and elastin OASIS Matrix of dermal regeneration derived from swine jejunum submucosa Matriderm Three-dimensional matrix of collagen and elastin Epidex Generated by autologous cultured keratinocyte from scalp hair follicles
- 83. Stem Cells and Burns Tried since 1975, • Common sources, ● Epithelial origin ● Mesenchymal stem cell ● Adipose tissue derived ● Umbilical cord derived ● Muscle satellite cell ● Still in experimental levels, in search of bilaminar skin containing dermal-epidermal components.
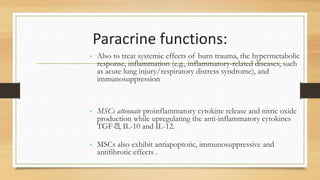
- 84. Paracrine functions: • Also to treat systemic effects of burn trauma, the hypermetabolic response, inflammation (e.g., inflammatory-related diseases, such as acute lung injury/respiratory distress syndrome), and immunosuppression • MSCs attenuate proinflammatory cytokine release and nitric oxide production while upregulating the anti-inflammatory cytokines TGF- , IL-10 and IL-12. • MSCs also exhibit antiapoptotic, immunosuppressive and antifibrotic effects .
- 85. GENE THERAPY • For the treatment of acute and chronic non-healing wounds combined gene delivery with stem cell therapy appears promising . • Gene therapy involves the insertion of a gene into recipient cells by viral transfection, naked DNA application, high pressure injection or liposomal vectors • To enhance the therapeutic response -development of 3D scaffolds or matrices is of vital importance,
- 86. • Burns induces a hyper metabolic and catabolic state which is more severe and lasts much longer than trauma or sepsis • If unchecked it results in loss of lean muscle mass, immune compromise and impaired wound healing Nutrition in burns
- 88. Nutrition in burns • Early vs Late (< > 24hrs) • Enteral vs Parenteral • Continous vs Intermitent • Prepyloric vs Postpyloric
- 89. Requirements • Calorie requirements ( Curreri formula – 24kcal per kg + 40kcal x TBSA ) • Indirect calorimetry • OBESITY? • Macronutrient requirement GLUCOSE 60% ( 7GM/KG/DAY ) LIPIDS 20% PROTEINS 20% ( 1.5 -2 GM/KG / DAY in adults and 2.5 -4gm/kg/day in children ) NON PROTEIN CALORIES / NITROGEN : 100-150 KCAL /1GM
- 90. • MICRONUTRIENTS • IMMUNONUTRITION Omega 3 fatty acid Arginine / Histidine Glutamine Vitamin A and C
- 91. Monitoring • BODY WEIGHT • NITROGEN BALANCE ( N2 BALANCE = N2 INTAKE IN 24HRS – [1.25x(UUN + 4)] • SERUM PROTEINS • EXERCISE TOLERANCE • IMPEDANCE BIOTHESIOMETRY
- 92. OVERFEEDING • DIFFICULT WEANING • FATTY LIVER – IMMUNE DYSFUNCTION • AZOTEMIA • HYPERGLYCEMIA
- 93. Miscellaneous points in burn care
- 94. Metabolic And Endocrine Considerations Persistent hypermetabolic response caused by catecholamines, cortisol, glucagon and proinflammatory mediators. Full body catabolism ,muscle protein degradation, insulin resistance and increased risk of infection. Flow phase and if left untreated physiologic exhaustion ensues
- 95. Pharmacologic modification • Recombitant Human Growth Hormone at 0.2 mg/kg/day • Oxandrolone • Insulin to keep blood glucose levels below 140 mg/dl • Metformin • Exenatide-Glucagon like Peptide • Propranolol • Ketoconazole
- 96. VENOUS THROMBOEMBOLISM - 50-70 % centers routinely give preventive prophylaxis - 22% only intermittent pneumatic compression - ACCP guidelines 2008 – Chemoprophylaxis for burns But, removed in 2012 guidelines - Scoring system
- 97. VENOUS THROMBOEMBOLISM - LMWH better than Unfractioned Heparin (UFH) - Chance of HIT because burn patients are already platelet depleted - 40mg enoxaparin may be insufficient dose - NO level 1 evidence regarding the risk or benefits of chemoprophylaxis after thermal injury -
- 98. TRANSFUSIONS 1- Keep Hemoglobin above 7gm% 2- Give RBC:PLASMA:PLATELETS -> 1:1:1 As compared to a ratio of RBC:FFP -> 4:1
- 99. CVC - CLABSI - High rates of infection in burns because : 1) Vascular access lines are near the burn wound 2) Frequent transient bacteremia does occur during wound manipulation 3) Burn ICU LOS is prolonged Recommendations : * Change the vascular access lines in 3-7 days * Antibiotic impregnated IVC * 3% Chlorhexidine gluconate washes
- 100. “YOU WILL NEVER FIND A STRONGER WILLED PERSON THAN THE BURN SURVIVOR FOR THEY HAVE SUFFERED THE WORST INJURY TO THE HUMAN BODY ANYONE CAN ENDURE AND SURVIVE” Gary R. Graham
- 106. Role of free flaps in burns
- 107. Free Flaps used in different areas • Foot • Head and Neck • Upper limb
- 108. Foot
- 109. Post Op = 1 Month
- 110. Post Op = 3 Months
- 111. Post Op = 6 Months
- 112. Head and Neck
- 113. Post Op
- 114. Delayed Post Op
- 115. FaceBurns
- 119. Expander Placement
- 120. Immediate Post Op
- 121. Upper Limb
- 123. THANK YOU
























































































![Monitoring
• BODY WEIGHT
• NITROGEN BALANCE ( N2 BALANCE = N2 INTAKE IN 24HRS – [1.25x(UUN
+ 4)]
• SERUM PROTEINS
• EXERCISE TOLERANCE
• IMPEDANCE BIOTHESIOMETRY](https://image.slidesharecdn.com/burnsss-180429030740/85/Burns-A-comprehensive-discussion-91-320.jpg)