2. Gastric Ca Management 2020.pptx2. Gastric Ca Management 2020.pptx
- 1. MANAGMENT OF GASTRIC CARCINOMA MODERATOR : Dr. HAILU,ASSISTANT PROF. General and upper GI surgery By- Tsion Tilahun (GSRIII) JULY 2020
- 2. OUTLINE 2 • Introduction • Epidemiology • Clinical presentation • Diagnostic workups and staging • Treatment
- 4. Anatomy • Innervation: – Parasympathetic via the vagus. • Left anterior and right posterior. – Sympathetic via the celiac plexus. 12/27/2024 4
- 5. Lymphatic drainage 12/27/2024 5 Zone 1 , draining the pyloric portion of the greater curve. Zone 2 , draining from the upper half of the greater curve. Zone 3 , drains the proximal two-thirds of the stomach and the upper lesser curve, and surrounds the left gastric artery. Zone 4, drains the distal portion of the lesser curve and pylorus All four drain into the celiac group of nodes and into the thoracic duct.
- 6. 12/27/2024 6 Zone 1 Zone 2 Zone 3 Zone 4
- 7. Lymphatic drainage of the stomach & LND Stations draining the stomach as to the JRSGC Stations 3-6 are commonly removed with D1 gastrectomy Stations 1, 2, & 7 -12 are commonly removed with D2 gastrectomy
- 8. Epidemiology 4th MC Ca in the world the 2nd leading cause of Ca death M:F = 3:2 It’s a disease of the elders with peak incidence in the 7th decade of life More common in low socioeconomic class citizens It is more common & has a higher mortality in African Americans, Asian Americans, & Hispanics compared with whites)
- 9. Cont.. Incidence <10 (US) Vs 40 /100000 (highest in Asia, Latin America & Caribbean) It has decreased by 2/3 in the past 50 yrs. mostly in intestinal histology , the distal Ca Its the MC cancer in Japan as a result screening in Japan was started in the 1970s since then the MR has decreased by 50% Globally there is proximal migration of tumors seen so the distribution currently is closer to 40% distal, 30% middle, & 30% proximal
- 10. Ethiopia
- 11. Epid..cont. 1. PRIMARY MALIGNANT NEOPLASMS OF THE STOMACH The three most common neoplasms are: • Adenocarcinoma (95%) • Lymphoma (4%) • Malignant GIST (1%) Other rare malignancies: • Carcinoid • Angiosarcoma • Carcino-sarcoma • Squamous cell carcinoma 2. Secondary involvement • Due to heamatogenous metastasis from other sites (e.g., melanoma or breast) • More commonly, malignant tumors from adjacent organs invade the stomach by direct extension (e.g., colon or pancreas ) or by peritoneal seeding (e.g., ovary) 3
- 12. Risk factors Nutritional Low fruit and vegetable Salted meat/fish High nitrate High complex carbohydrate Environmental Poor food preparation Lack of refrigeration contaminated drinking water Smoking Medical H-pylori Gastric atrophy Pernicious anemia Polyps Menetrier disease EBV Prior gastric surgery Other Low socio-economic Male gender 12
- 13. 13 Diet High salted meat/fish and pickled foods Damage stomach mucosa and increases the susceptibility to carcinogenesis High nitrate N-nitroso(carcinogen) Intake of green, leafy vegetables and citrus fruits, which contain antioxidants such as ascorbate and beta-carotene is protective Smoking Increases risk by 60% in men and 20%in women
- 14. 12/27/2024 14 Genetics commonly affected genes are P53,COX 2 and CDH1 gene Hereditary diffuse gastric cancer Inactivates e-cadherin (cell adhesion molecule) 2 of more gastric cancer cases in the 1st /2nd degree relatives with age<50 80% increased risk Lynch syndrome(HNPCC) – intestinal type and 10% higher risk Familial adenomatous polyposis - 10% increased risk Li-fraumeni syndrome – P53 gene mutation
- 15. Risk Factors 15 Helicobacter pylori Classified as definite carcinogen Associated with 6x increases risk in developing adenocarcinoma Triggers inflammation at the corpus mucosa that results in atrophy and intestinal metaplasia Alterations depend on both the presence of bacterial proteins and the host immune response The cagA strain causes more mucosal inflammation and thus a higher risk of gastric cancer
- 16. 16 Pernicious anemia Destruction of parietal and chief cells by autoimmune reaction Achlorhydria that accompanies this condition favors bacterial proliferation, which generates carcinogenic nitrosamines from nitrates Blood group A 20% incidence Mostly associated with diffuse gastric cancer
- 17. 17 Epstein–Barr virus (EBV) Detected in 2-16% of gastric adenocarcinoma Role in gastric carcinogenesis is not yet established Higher frequency in tumors of the proximal and Male predominance Previous gastric surgery Occur after ten of surgery Overall risk is 3-10% Pathogenesis related to bile reflux , achlorhydria and atrophic gastritis
- 18. Clinical features Vague discomfort and/or indigestion Epigastric pain that is constant, non-radiating, and unrelieved by food ingestion Diffuse mural disease may present with early satiety due to decreased distensiability so weight loss , anorexia and other constitutional SmS Proximal tumors may present with dysphagia where as antral tumors as GOO May Presents as either acute UGIB with frank heamatemesis (5-15%) or most commonly as occult GIB with some form of anemia (40%) with melena (ulcerated lesions)
- 19. Clinical.. P/E is unremarkable i.e. cachexia , pallor , Palpable abdominal mass , HSM , jaundice, or ascites as an evidence of metastasis • left supraclavicular node(Virchow’s) • Periumbilical node (sister marry joseph node) • Left axillary node(irish) • Peritoneal spread can present with an enlarged ovary (Krukenberg's tumor or a mass in the cul-de-sac on rectal examination (Blumer's shelf.
- 20. Clinical.. • Paraneoplastic manifestations • Dermatologic findings like diffuse seborrheic keratoses (sign of Leser-Trelat) or acanthosis nigricans which is characterized by velvety and darkly pigmented patches on skin folds. • Neither finding is specific for gastric cancer. • Other paraneoplastic abnormalities that can occur in gastric cancer include:- - microangiopathic hemolytic anemia -membranous nephropathy -hypercoagulable states (Trousseau's syndrome). Polyarteritis nodosa has been reported as the single manifestation of an early and surgically curable gastric cancer
- 21. Diagnostic workups and staging • CBC , chemistry panel, LFTs, Serum-Albumin and coagulation studies, OBT • Two main modalities for gastric cancer screening upper endoscopy (Gold standard) contrast radiography • false-negative barium studies can occur in as many as 50 percent of cases • barium study may be superior to upper endoscopy is in patients with linitis plastica
- 22. • barium study may be superior to upper endoscopy is in patients with linitis plastica
- 23. Tumor markers like CEA, CA-125, CA-19-9, B- HCG serum pepsinogen, Serum trefoil factor 3 (TFF3), microRNAs
- 24. SCREENING Controversial • Universal screening:- Japan, for individuals older than 50 years with conventional double-contrast barium radiograph with photofluorography every year or upper endoscopy every two to three years . In Korea, upper endoscopy is recommended every two years for individuals aged 40 to 75 years • Selective screening of high-risk subgroups individuals at increased risk for gastric cancer include those with the following Gastric adenomas Pernicious anemia Gastric intestinal metaplasia Familial adenomatous polyposis Lynch syndrome Peutz-Jeghers syndrome Juvenile polyposis syndrome
- 25. STAGING EVALUATION Complete clinical or preoperative staging of patients with gastric cancer includes: • Physical examination, including evaluation of appropriate nodal areas (especially left supraclavicular nodes) as well as the abdomen and rectal examination. • CT scans of abdomen and pelvis, chest CT is not very accurate for assessing the depth of tumor invasion of the stomach wall or regional nodal • Endoscopic ultrasound (EUS) may provide more accurate staging evaluation of the tumor and nodal stage(>5mm) than CT and also allows for preoperative biopsies.(80% accurate) • Staging laparoscopy and peritoneal cytology :advantage of directly visualizing the liver surface, peritoneum, and local lymph nodes, and permitting biopsy of any suspicious lesions
- 28. 12/27/2024 28 T1 T2 T3 T4a T4b N0 Stage Ia Stage Ib Stage IIa Stage IIb Stage IIIb N1 Stage Ib Stage IIa Stage IIb Stage IIIa Stage IIIb N2 Stage IIa Stage IIb Stage IIIa Stage IIIb Stage IIIc N3 Stage IIb Stage IIIa Stage IIIb Stage IIIc Stage IIIc M1 Stage IV Stage IV Stage IV Stage IV Stage IV
- 29. Treatment Treat …. Core point of treatment • Extent of surgical resection resection • Extent of lymph node dissection • Chemo radio therapy
- 30. Surgery • The goal of curative surgery is complete resection of all tumor with a grossly negative margin of at least 5 cm as well with an adequate lymphadenectomy performed (R0 resection) Indicators of unresectabiliy • distant metastases • invasion of a major vascular structure, such as the aorta ,hepatic artery ,celiac axis/proximal splenic artery • Lymph nodes behind or inferior to the pancreas, aorto-caval region, into the mediastinum, or in the porta hepatis • Distal splenic artery involvement is not an indicator of unresectability
- 31. Surg…. Distal radical subtotal gastrectomy is standard operation Reconstruction is by billroth II gastrojejunotomy or Roux –en- gastrojejunostomy . Total gasrectomy with Roux-en-Y esophagojejunostomy may be required for R0 resection and proximal gastric adenoma,large midgastric lesions or infiltrative disease (eg, linitis plastica)
- 32. Techniques 1.Begin at pylorus with high ligation of R gastroepiploic artery 2 along the greather curvature 3 spare LGEA and short gastric vesels (not for sub total) 4 posterior antrum separted from anterior pancreas and base of the transverse mesocolon by division of fine connective tissue attachements.
- 33. Cont.. 5.Gastrohepatic ligament is incised , leser curvature is dissected 6. Dissection is extended toward the celiac axis 7. Proximal duodenum is divided (care for common bile duct and hepatic artery
- 34. • Proximal loop of jejunum is chosen and apposed to stomach. • Jejunum can be delivered through incision in the transverse mesocolon or anterior to transverse mesocolon (malignance)
- 35. Endoscopic Resection General guidelines for endoscopic resection of early gastric cancer ;(T1a) 1. Tumor limited to the mucosa, 2. No lymphovascular invasion, 3. Tumor smaller than 2 cm, 4. No ulceration, and 5. Well or moderately differentiated histopathology
- 36. Extent of lymph node dissection More than 15 respected lymph node is required • D1 lymphadenectomy - dissection of the perigastric lymph nodes only(3-6) • D2 lymphadenectomy removal of nodes along the hepatic, left gastric, celiac and splenic arteries & in the splenic hilum (stations 1- 12). • D3 dissection is a D2+ per aortic .
- 37. D1 vs D2 Lymphadenectomy
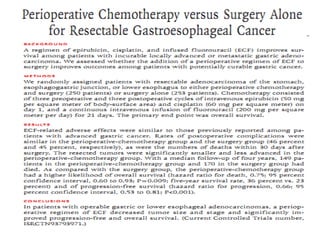
- 43. Chemotherapy and Chemoradiotherapy • Neoadjuvant/perioperative chemotherapy • Neoadjuvant chemoradiotherapy
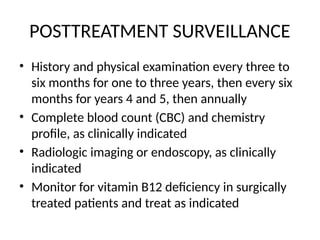
- 46. POSTTREATMENT SURVEILLANCE • History and physical examination every three to six months for one to three years, then every six months for years 4 and 5, then annually • Complete blood count (CBC) and chemistry profile, as clinically indicated • Radiologic imaging or endoscopy, as clinically indicated • Monitor for vitamin B12 deficiency in surgically treated patients and treat as indicated
- 47. Gastric GIST • Originally thought to be a type of smooth muscle sarcoma, • they are now known to be a distinct tumor derived from the interstitial cells of Cajal, an intestinal pacemaker cell. • They are most commonly found in the stomach (40% to 60%), small intestine (30%), and colon (15%). 57
- 48. Cont. • They vary considerably in their presentation and clinical course, ranging from small benign tumors to massive lesions with necrosis, hemorrhage, and wide metastases. • can manifest at any age, peak age >50 years. • an equal male-to-female ratio or a slight male predominance • Most GISTs manifest symptomatically, typically with bleeding or vague abdominal pain or discomfort. • Many patients remain asymptomatic, and their tumors are discovered incidentally at the time of other surgery or, increasingly, during imaging performed for other indications
- 49. GIST cont… • They are frequently identified by immunohistochemical staining for the c-kit proto- oncogene (CD117), which is overexpressed in 95% of these tumors, and for CD34, which is positive in 60% to 70% of GISTs. • Investigations are same with gastric adenocarcinoma 58
- 50. Suggested guideline for assessing malignant potential of GIST of different sizes and mitotic rate 1. Benign (no tumor-related mortality) -No larger than 2 cm, no more than 5 mitoses/50 HPF 2.Probably benign (<3% with progressive disease) - >2 cm but ≤5 cm; no more than 5 mitoses/50 HPF 3.Uncertain or low malignant potential -No larger than 2 cm; >5 mitoses/50 HPF 4.Low to moderate malignant potential (12%-15% tumor-related mortality) ->10 cm; no more than 5 mitoses/HPF • >2 cm but ≤5 cm; >5 mitoses/50 HPF 5.High malignant potential (49%-86% tumor-related mortality) • ->5 cm but ≤10 cm; >5 mitoses/50 HPF • >10 cm; >5 mitoses/50 HPF 59
- 51. TREATMENT • The mainstay of treatment is complete surgical resection • Tumors greater than 2 cm in diameter should be resected • Tumors that are less than 2 cm and have high-risk features on endoscopy and EUS, such as irregular borders, ulceration, and heterogeneity, should be resected • tumors without such features can be observed with repeat endoscopy and EUS at 6- to 12-month intervals • Depending on tumor size, options of resection include: wide local excision Enucleation sleeve gastrectomy total gastrectomy, with or without en bloc resection of adjacent organs. • No lymph node dissection is required as lymph node metastases are rare. 60
- 52. Adjuvant Therapy for GIST • tyrosine kinase inhibitor imatinib (Gleevec) is used as adjuvant , neoadjuvant and palliative therapy. • In patients with metastatic or unresectable disease, imatinib (400 mg daily) showed an overall 2-year survival of 70% compared with 25% for patients on traditional chemotherapy. • In the adjuvant setting, tumors 3 cm or larger who underwent complete resection and were treated with imatinib for 1 year had a recurrence rate of 8% compared with 20% for untreated patients • Minimum of 3 years as adjuvant following complete resection . Indications for tyrosine kinase inhibitor moderate to high risk for recurrence or metastasis(>3cm or >5mitosis/hpf) after resection of resectable ds For unresectable tumour as neoadjuvant, optimal duration of tx uncertain. For metastatic disease and patients with resected primary disease at moderate risk of recurrence, indefinite treatment with imatinib . 61
- 53. • Five-year survival following resection for GIST is about 50%. • Most patients with low-grade lesions are cured (80% 5-year survival), but most patients with high-grade lesions are not (30% 5-year survival). 62
- 54. Reference 1. SCHWARTZ’S PRINCIPLES OF SURGERY , 11th edition 2. Maingot’s ABDOMINAL OPERATIONS 13th edition 3. Shackelford’s SURGERYof the ALIMENTARY TRACT, 8th edition 4. Uptodate 21.6 5. Zollenger atlas of surgical operation 9th edition. 7. Kobayashi T, Kimura T. [Long-term outcome of preoperative chemothe rapy with 5'-deoxy-5-fluorouridine (5'-DFUR) for gastric can cer]. 8. Gan To Kagaku Ryoho 2000; 27:1521. Nio Y, Koike M, Omori H, et al. A randomized consent desig n trial of neoadjuvant chemotherapy with tegafur plus uracil 69
Editor's Notes
- #7: level N1 (i.e., stations 3 to 6), level N2 (i.e., stations 1, 2, 7, 8, and 11), and level N3 (i.e., stations 9, 10, and 12) nodes.
- #8: Gastric cancer is the 14th most common cancer and cause of cancer death in the USA, with an estimated 22,000 new cases/year and more than 10,000 deaths
- #9: Although there has been an increase in proximal tumors in Japan, most are distal gastric cancers
- #11: Benign tumors : -Polyp -Leiomyoma -Inflammatory lesions -Heterotopic pancreas
- #13: Dietary nitrates have been impugned as a possible cause of gastric cancer. Gastric bacteria (more common in the achlorhydric stomach of patients with atrophic gastritis, a risk factor for gastric cancer) convert nitrate into nitrite, a proven carcinogen.
- #19: Unfortunately most patients present in later stages of disease, with evidence of metastatic or locally advanced tumor
- #23: erum pepsinogen — A low serum pepsinogen I concentration and a low serum pepsinogen I/II ratio are suggestive of the presence of atrophic gastritis, a risk factor for gastric cancer. Serum trefoil factor 3 (TFF3) is a small stable protein expressed in the goblet cells of the small and large intestine and in gastric intestinal metaplasia. In one study, the sensitivity and specificity of serum TFF3 for detection of gastric cancer were both 81 percent compared with 45 and 88 percent, respectively, At least three microRNAs (miRNAs), miRNA-421, miRNA 18a, and miR-106a, are highly expressed in gastric cancers and are detectable in peripheral blood and gastric aspirates [13-15]. Assays for multiple miRNAs may further
- #47: They are rarely associated with familial syndromes such as GISTparaganglioma syndrome (Carney triad), neurofibromatosis and von Hippel-Lindau disease, but most develop de novo.
- #51: Recurrence rates are approximately 40%, and most patients who experience recurrence demonstrate metastasis to the liver, with one third having only isolated local recurrence. Recurrence can occur 20 years later, and long-term follow-up is warranted. Long-term disease-free survival is approximately 50%, with 20% to 80% of patients dying of their disease. Although there are no dichotomous criteria that are able to define benign versus malignant lesions histologically, the most important risk factors for malignancy are tumor size larger than 10 cm and more than five mitoses/50 high-power fields (HPF). Based on a long-term follow-up study of 1700 patients with gastric GISTs, guidelines for assessing malignant potential based on the combination of these two factors have been developed
- #52: However, as a result of current trials, for patients with metastatic disease and patients with resected primary disease at moderate risk of recurrence, indefinite treatment with imatinib has been approved by the U.S. Food and Drug Administration. These findings led to the development of effective systemic therapies in the form of small molecule tyrosine kinase inhibitors (TKIs), of which the prototype is imatinib . These agents block signaling via KIT and PDGFRA by binding to the adenosine triphosphate-binding pocket required for phosphorylation and activation of the receptor. The end result is inhibition of tumor proliferation. We recommend adjuvant treatment with a tyrosine kinase inhibitor ( imatinib 400 mg daily) for a minimum of three years rather than one year in patients who have a completely resected primary high-risk GIST The optimal duration of neoadjuvant imatinib is uncertain, and we individualize this decision based upon drug tolerance, tumor location and extent, and the urgency of surgical treatment.



















































![Reference
1. SCHWARTZ’S PRINCIPLES OF SURGERY , 11th
edition
2. Maingot’s ABDOMINAL OPERATIONS 13th
edition
3. Shackelford’s SURGERYof the ALIMENTARY TRACT, 8th
edition
4. Uptodate 21.6
5. Zollenger atlas of surgical operation 9th
edition.
7. Kobayashi
T, Kimura T. [Long-term outcome of preoperative chemothe
rapy with 5'-deoxy-5-fluorouridine (5'-DFUR) for gastric can
cer].
8. Gan To Kagaku Ryoho 2000; 27:1521.
Nio Y, Koike M, Omori H, et al. A randomized consent desig
n trial of
neoadjuvant chemotherapy with tegafur plus uracil
69](https://image.slidesharecdn.com/2-241227234420-2cf89361/85/2-Gastric-Ca-Management-2020-pptx2-Gastric-Ca-Management-2020-pptx-54-320.jpg)