2010 ECC overview cole v0.2
- 1. New Changes to Old Friends An overview of the 2010 ECC recommendations for ADULT CPR and Emergency Cardiovascular Care (ECC)
- 2. Objectives Discuss the 2010 changes to ECC and CPR Discuss and review the importance of CPR, and the clinical methods to maximize its effectiveness
- 3. Credit where Credit is Due Adapted from presentation by Ahamed Idris, MD, Professor of Emergency Medicine University of Texas Southwestern Medical Center at Dallas American Heart Association Circulation documents
- 4. Special Thanks Dr. Peter Safar Father of Resuscitation medicine Helped develop CPR Directly responsible for the research used today in therapeutic hypothermia.
- 5. EVIDENCE BASED MEDICINE? Using material from: Sayre MR, O’Connor RE, Atkins DL, Billi JE, Callaway CW, Shuster M, Eigel B, Montgomery WH, Hickey RW, Jacobs I, Nadkarni VM, Morley PT, Semenko TI, Hazinski MF. Part 2: evidence evaluation and management of potential or perceived conflicts of interest: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122(suppl 3):S657–S664.
- 6. Levels of Evidence Used to be 7 (or 8 ) different ILCOR levels of Evidence (LOE). In 2010 ILCOR reduced these to 5. The AHA has broken these into three broad categories Level A – Highest standard of evidence. Level B – Most common. Level C – Anecdotal case reports, consensus opinions, retrospective studies, small studies, previous standard of care without evidence to contrary
- 8. KEY POINT: “ A recommendation with Level of Evidence B or C does not imply that the recommendation is weak. Many important clinical questions addressed in the guidelines do not lend themselves to clinical trials. Even though randomized trials are not available, there may be a very clear clinical consensus that a particular test or therapy is useful or effective.” 2010 AHA ECC Guidelines Circulation 2010;122;S657-S664
- 9. Classes of Recommendations Most previous classes retained with better clarifications and descriptions. “ Class Indeterminate” recommendations, which were used in 2005, are not included in the 2010 AHA Guidelines for CPR and ECC. The elimination of the term “Class Indeterminate” is consistent with the ACCF–AHA Classes of Recommendation. When the AHA writing groups felt that the evidence was insufficient to offer a recommendation either for or against the use of a drug or intervention, no recommendation was given.
- 11. ETHICAL CONSIDERATIONS IN ECC Using material from: Morrison LJ, Kierzek G, Diekema DS, Sayre MR, Silvers SM, Idris AH, Mancini ME. Part 3: ethics: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122(suppl 3):S665–S675.
- 12. ECC and DEATH New TERMS DNR: DNAR: Do not attempt Resuscitation AND: Allow Natural Death Principle of Futility Defined as <1% chance of success or positive outcome.
- 13. Withholding Resuscitation Mild changes in verbage: Situations where attempts to perform CPR would place the rescuer at risk of serious injury or mortal peril ● Obvious clinical signs of irreversible death (eg, rigor-mortis, dependent lividity, decapitation, transection, or decomposition) A valid, signed, and dated advance directive indicating that resuscitation is not desired, or a valid, signed, and dated DNAR order
- 14. Termination of Resuscitation- BLS when ALS is not available or delayed. All 3 of the following criteria must be present before moving to the ambulance for transport , to consider terminating BLS resuscitative attempts for adult victims of out-of-hospital cardiac arrest: Arrest was not witnessed by EMS provider or first responder; No return of spontaneous circulation (ROSC) after 3 full rounds of CPR and automated external defibrillator (AED) analysis; and no AED shocks were delivered. This is to be used in conjunction with consultation with real time on line medical control. (Class IIb, LOE A).
- 15. Termination of Resuscitation- ALS All 3 of the following criteria must be present before moving to the ambulance for transport , to consider terminating BLS and ALS resuscitative attempts for adult victims of out-of-hospital cardiac arrest: Arrest was not witnessed by EMS provider or first responder; No return of spontaneous circulation (ROSC) after “full ALS care” (defined as 20 minutes of ALS and an advanced airway. and no AED shocks were delivered prior to ALS arrival. (Class IIa, LOE B).
- 16. Why Terminate? Termination of Resuscitative Efforts and Transport Implications : Field termination reduces unnecessary transport to the hospital by 60% with the BLS rule and 40% with the ALS rule, reducing associated road hazards that put the provider, patient, and public at risk. In addition field termination reduces inadvertent paramedic exposure to potential biohazards and the higher cost of ED pronouncement. More importantly the quality of CPR is compromised during transport, and survival is linked to optimizing scene care rather than rushing to hospital.
- 17. Termination of Resuscitation in Pediatrics No predictors of neonatal or pediatric (infant or child) out-of hospital resuscitation success or failure have been established. No validated clinical decision rules have been derived and evaluated. Further research in this area is needed. In the absence of clinical decision rules for the neonatal or pediatric OHCA victim, the responsible prehospital provider should follow BLS pediatric and advanced cardiovascular life support protocols and consult with real-time medical direction or transport the victim to the most appropriate facility per local directives.
- 18. Other Ethical Questions we did not discuss that are in the AHA documents In hospital cardiac arrest ethical decisions Withholding and withdrawing care in the newborn and neonate, especially pre-term and low birthweight Organ and Tissue Donation after resuscitation. Ethics of resuscitation research Ethics of training on the newly dead
- 19. CPR: W.I.N. (What's Important Now)
- 20. 90% of all changes to 2010 ECC are right in the BLS segment. Builds on and further enhances the changes and research discussed in the 2005 guidelines. COMPRESSIONS are the single most emphasized segment of resuscitation. GOOD and SUSTAINED Coronary Perfusion Pressure is the GOAL!
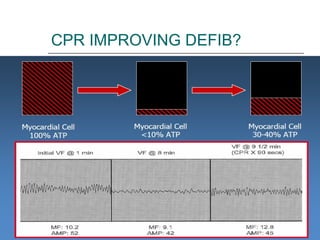
- 21. Understanding CPP? Coronary Perfusion Pressure (CPP) is essential to ROSC When arrest is present for more than a few minutes, the myocardium is depleted of oxygen and metabolic substrates. A brief period of (good and sustained) chest compressions can deliver oxygen and energy substrates (i.e. ATP) ,increasing the likelihood that a shock may terminate VF (defibrillation) and a perfusing rhythm will return (ie, ROSC). Without this, a shock may result in “SECONDARY ASYSTOLE” GOOD and SUSTAINED CPP results in higher levels of myocardial ATP and survival.
- 22. 3 Phase Model
- 23. Understanding Coronary Perfusion Pressure Note this is Aortic Pressure. CPP is “roughly” half Aortic Pressure.
- 24. ROSC Associated with CPP
- 25. Overview of ECC 2010 Changes
- 26. Hands Only CPR??? Single biggest change “Hands Only CPR” AKA: Compression only CPR for lay persons.
- 27. Hands Only CPR??? Of note, some healthcare providers and laypersons indicate that reluctance to perform mouth-to-mouth ventilation for victims of cardiac arrest is a theoretical and potential barrier to performing bystander CPR. When actual bystanders were interviewed, however, such reluctance was not expressed; panic was cited as the major obstacle to laypersons performance of bystander CPR. The simpler Hands-Only technique may help overcome panic and hesitation to act in both regards.
- 28. KEY POINT: HANDS ONLY CPR MAY IMPROVE ROSC BY 7% OVER TRADITIONAL CPR in LAY RESCUERS This presumes that traditional CPR with ventilation will eventually be performed. The exact interval in which hands only CPR is more beneficial over traditional CPR is not known.
- 29. CAB??? Sequence change to chest compressions before rescue breaths (CAB rather than ABC) This is expected to reduce time from assessment of responsiveness to first compression by 30 or more seconds. This reduction in time during this critical period early in the arrest is expected to improve survival and also response to first shock.
- 30. Pulse Check? Studies have shown that both lay rescuers and healthcare providers have difficulty detecting a pulse. The lay rescuer should not check for a pulse and should assume that cardiac arrest is present if an adult suddenly collapses or an unresponsive victim is not breathing normally. Healthcare providers also may take too long to check for a pulse. The healthcare provider should take no more than 10 seconds to check for a pulse and, if the rescuer does not definitely feel a pulse within that time period, the rescuer should begin CPR .
- 31. Look, Listen, and Feel? Confusion in Agonal Respirations vs. Good Respirations. The rescuer should treat the victim who has occasional gasps as if he or she is not breathing (Class I,LOE C). The HCP will combine their assessment for respirations with assessment for responsiveness The Layperson will assume that if the patient is completely unresponsive they have ineffective respirations.
- 32. A simultaneous, choreographed approach? Much more emphasis on the team approach; and a realistic recognition of what and how PARAMEDICS do their job! Recognition that resuscitation is not a “linier” process (Step A, THEN Step B, etc) but a simultaneous series of actions. “… .in a highly specialized environment, such as a critical care unit of a hospital, many of the individual components of CPR (compression-ventilation-defibrillation) may be managed simultaneously. This approach requires choreography among many highly-trained rescuers who work as an integrated team. In the pre-hospital setting, the order of the CPR components performed by the healthcare provider may switch between a sequenced and choreographed model depending on the proficiency of the provider and the availability of resources.” - Circulation . 2010;122[suppl 3]:S676 –S684. “ It is reasonable for healthcare providers to tailor the sequence of rescue actions to the most likely cause of arrest.” THIS MEANS NO MORE COOK-BOOK MEDICINE!!!!!
- 35. 2005 to 2010 changes HCP only, Checking for “DEFNITE pulse”. HCP Only PULSE CHECK Component of CPR 2005 ECC recommendations 2010 ECC Recommendations DEPTH OF COMPRESSION 1 ½ - 2 inches Greater than 2 inches RATE 100 /MINUTE At least 100 /MIN VENTILATION 8-10 /MINUTE 8-10 /MINUTE CHEST RECOIL 100% 100% INTURUPTIONS Minimized Less than 10 seconds goal
- 36. SOME THINGS REMAIN IMPORTANT RATE DEPTH RELEASE UNINTERRUPTED DECREASED VENTILATION 5 KEY ASPECTS OF GOOD CPR!
- 37. Compression Rate (at least 100 / Minute) Rate per minute is NOT a function of “speed” of compressions only, but a function of both speed ands minimizing no-flow periods (discussed later) for a total compressions/minute. Compressions rates as high as 130 resulted in favorable outcomes Compression rates <87/minute saw rapid drop off in ROSC. NEW RECOMMENDATION: At LEAST 100/minute. Better too fast than too slow.
- 38. Compression Rate… Percent segments within 10 cpm of AHA Guidelines 31 % 36.9% Abella, et al 2005 Circulation 76 % 75 % 58 % 42%
- 39. Compression Rate Target = ~100/min with complete release Reality = 60/min due to “No Flow Ratio” Quality of Cardiopulmonary Resuscitation During Out-of-Hospital Cardiac Arrest Wik, et al. JAMA 2005
- 40. Compression DEPTH (At least 2 inches) Previous studies show that only about 27% of compressions were deep enough (Wik, 2005) 0% (none) were too deep. NEW GIUDELINES: The adult sternum should be depressed at least 2 inches (5 cm) (Class IIa, LOE B), with chest compression and chest recoil/relaxation times approximately equal (Class IIb, LOE C).
- 41. Compression DEPTH Target = 38-51 mm with complete release Reality = only 27% achieve target Quality of Cardiopulmonary Resuscitation During Out-of-Hospital Cardiac Arrest Wik, et al. JAMA 2005
- 42. Complete RELEASE/RECOIL (Full) Complete Recoil essential to reduce intrathoracic pressure between compressions. Reducing recoil improves hemodynamics in arrest, and improves Coronary Perfusion Pressure (CPP) Incomplete chest wall recoil can be reduced during CPR by using electronic recording devices that provide real-time feedback. Niles D, Nysaether J, Sutton R, Nishisaki A, Abella BS, Arbogast K, Maltese MR, Berg RA, Helfaer M, Nadkarni V. Leaning is common during in-hospital pediatric CPR, and decreased with automated corrective feedback. Resuscitation. 2009;80:553–557
- 43. Intra-thoracic Pressure and CPR?
- 44. Importance of complete recoil
- 45. Get EVERY Compression Right Critical pressure for ROSC (Paradis et al. JAMA 1990;263:3257-8) Abella, et al 2005 Circulation
- 46. Cerebral Perfusion Pressures and Recoil Abella, et al 2005 Circulation
- 47. INTURRUPTIONS Pausing for procedures intubation, IV, pulse check, etc.). Pausing for rhythm analysis. Pausing after shock to await post-shock rhythm. Pausing to charge, clear, and shock. Unaware of importance of CPR in “big picture”
- 48. No-Flow Ratio (Interruption of CPR) Target = less than 20% Reality = 48% Quality of Cardiopulmonary Resuscitation During Out-of-Hospital Cardiac Arrest Wik, et al. JAMA 2005
- 49. KEY POINT: “… High-quality CPR is important not only at the onset but throughout the course of resuscitation. Defibrillation and advanced care should be interfaced in a way that minimizes any interruption in CPR.” AHA 2010 Guidelines
- 50. DECREASING VENTILATION CPR with Advanced Airway: 8 – 10 breaths/minute Post-resuscitation: 10 – 12/min
- 51. Compression-Ventilation Ratio Ventilation rate = 12/min Compression rate = 78/min. Large amplitude waves = ventilations. Small amplitude waves = compressions. Each strip records 16 seconds of time
- 52. Reality Sucks… Compression: Ventilation Ratio 2:1 47-48 Breaths a minute 47 Nails in a coffin!
- 53. Prolonged Ventilations Ventilation Duration = 4.36 seconds / breath Ventilation Rate = 11 breaths / minute % time under Positive Pressure = 80%
- 54. Everyone sucks! Milwaukee Mean Ventilation Rate: 37/minute AFTER 2 months training: 22/minute Dallas 30/minute Tuscan 34/minute Chicago >30/minute
- 55. Effect of Vent. Rate on CPP 12 RR /minute CPP 23.4 ± 1.0mmHg MIP 7.1 ± 0.7 mmHg/min 20 RR /minute CPP 19.5 ± 1.8 mmHg MIP 11.6 ± 0.7 mmHg/min 30 RR /minute CPP 16.9 ± 1.8 mmHg MIP 17.5 ± 1.0 mmHg/min
- 56. CPR Prompts
- 57. CPR Feedback? CPR FEEDBACK?
- 58. CPR Feed Back? Several studies have demonstrated improvement in chest compression rate, depth, chest recoil, ventilation rate, and indicators of blood flow such as end-tidal CO2 (PETCO2) when real-time feedback or prompt devices are used to guide CPR performance. However, there are no studies to date that demonstrate a significant improvement in patient survival related to the use of CPR feedback devices during actual cardiac arrest events. Other CPR feedback devices with accelerometers may overestimate compression depth when compressions are performed on a soft surface such as a mattress because the depth of sternal movement may be partly due to movement of the mattress rather than anterior-posterior (AP) compression of the chest. Nevertheless, real-time CPR prompting and feedback technology such as visual and auditory prompting devices can improve the quality of CPR (Class IIa, LOE B).
- 59. CPR Marathon? Howard Snitzer, 59, survived 96 minutes of CPR with no neuro Deficits. http://abcnews.go.com/Health/96-minute-cpr-marathon-saves-minnesota-mans-life/story?id=13048099
- 60. CPR Gadgets, Gizmo’s and Ideas
- 61. Interposed Abdominal Compression-CPR (IAC-CPR) Conventional chest compressions combined with alternating abdominal compressions to improve aortic pressure and thus CPP. Mixed Results in in-hospital studies, but overall positive. Limited Out of Hospital Studies. No Adult complications but 1 report of traumatic pancreatitis in a pediatric patient. IAC-CPR may be considered during in-hospital resuscitation when sufficient personnel trained in its use are available (Class IIb, LOE B). There is insufficient evidence to recommend for or against the use of IAC-CPR in the out-of-hospital setting or in children.
- 62. Active Compression-Decompression CPR ( ACD-CPR) Small studies showed improvement, but a Cochrane Meta- review of over 1000 patients did not. ACD-CPR may be considered for use when providers are adequately trained and monitored (Class IIb, LOE B).
- 63. Impedance Threshold Device (ITD) Used both with ETT, Face Mask, and other advanced Airways. The ITD limits air entry into the lungs during the decompression phase of CPR, creating negative intrathoracic pressure and improving venous return to the heart and cardiac output during CPR. Major reviews have shown some survival to hospital improvement, but this may be multi-factorial. The ITD may be considered by trained personnel as a CPR adjunct in adult cardiac arrest (Class IIb, LOE B).
- 64. Mechanical Piston Devices L.U.C.A.S., THUMPER, ETC In 3 Studies the use of a mechanical piston device for CPR improved end-tidal CO2 and mean arterial pressure during adult cardiac arrest resuscitation. No long term benefit over manual CPR discovered (yet) There is insufficient evidence to support or refute the routine use of mechanical piston devices in the treatment of cardiac arrest. Use of such devices during specific cercumstances when manual CPR is difficult may be done (Class IIb, LOE C).
- 66. Load-Distributing Band CPR or Vest CPR (LDB-CPR) Auto-Pulse is the most common Initial repots were very positive, however a large study showed poor neurological outcomes. Further studies pending. The LDB may be considered for use by properly trained personnel in specific settings for the treatment of cardiac arrest (Class IIb, LOE B). However, there is insufficient evidence to support the routine use of the LDB in the treatment of cardiac arrest
- 68. Electrical Therapies: Overview For every minute that passes between collapse and defibrillation, survival rates from witnessed VF SCA decrease 7% to 10% if no CPR is provided. When bystander CPR is provided, the decrease in survival rates is more gradual and averages 3% to 4% per minute from collapse to defibrillation. CPR prolongs VF, delays the onset of asystole, and extends the window of time during which defibrillation can occur. Basic CPR alone, however, is unlikely to terminate VF and restore a perfusing rhythm (exception: Lightning strikes)
- 69. CPR and AED: EQUALLY IMPRORTANT Delays to either the start of CPR or the start of defibrillation reduce survival from SCA. In the 1990s, some predicted that CPR could be rendered obsolete by the widespread development of community AED programs. However, Cobb (MD for Seattle/King County Medic One System) noted that as more of Seattle’s first responders were equipped with AEDs, survival rates from SCA unexpectedly fell . This decline was attributed to reduced emphasis on CPR, and there is growing evidence to support this view.
- 70. TWO MAJOR QUESTIONS : CPR First or Defib First? Number of shocks to be delivered in a sequence before the rescuer resumes CPR (this was also evaluated in 2005)
- 71. CPR or Defib First? In un-witnessed arrest, or arrest 4-5 minutes (or longer) without good sustained CPR, a 1 ½ to 3 minute cycle of high quality CPR may improve the chance of ROSC, Survival to discharge, and 1 year survival.
- 73. Effects of “Progress”…. 1978 1975 1980s and 1990’s King County/Seattle Medic One EMS System Data, Cobb, 1999
- 75. CPR FIRST? % ROSC
- 76. CPR FIRST BEFORE DEFIB? The rate of survival improved (24 percent to 30 percent) when CPR was initiated prior to external defibrillation, especially in patients with delayed initial response intervals (longer than 4 minutes): 27 percent with CPR versus 17 percent without CPR first. The overall proportion that survived with favorable neurologic recovery also improved from 17 percent to 23 percent . Cobb LA et al. Influence of cardiopulmonary resuscitation prior to defibrillation in patients with out-of-hospital ventricular fibrillation.JAMA 1999 Apr 7 281 1182-1188.
- 78. CPR First? When an out-of-hospital cardiac arrest is not witnessed by EMS personnel, EMS may initiate CPR while checking the ECG rhythm and preparing for defibrillation. There is insufficient evidence to determine if 1 1⁄2 to 3 minutes of CPR should ALWAYS be provided prior to defibrillation. EMS system medical directors may consider implementing a protocol that allows EMS responders to provide a cycle of CPR while preparing for defibrillation of patients found by EMS personnel to be in VF.
- 79. CPR First The exact role of CPR first is unclear, but may be implemented by medical director (Class IIb, LOE B).
- 80. Reducing Time to Shock A reduction of even a few seconds in the interval from pausing compressions to shock delivery can increase the probability of shock success.
- 82. Reducing Time to Shock Scene Management CPR during “charging” Performing CPR while a defibrillator is readied for use is strongly recommended for all patients in cardiac arrest (Class I, LOE B).
- 83. 1 shock vs. 3 shocks (stacked) 20o5 ECC recommended a single shock sequence. 2 new studies have confirmed this recommendation. Biphasic 1 st shock success comparable to 3 stacked monophasic shock success Subsequent shocks in a stacked shock sequence have a very low incremental benefit, especially when compared to the benefit of good and sustained CPR.
- 84. Updated Energy Recommendations: Monophasic (of anyone still has them) use the MAX possible dose for all shocks. Monophasic AEDs can still use old settings. In the absence of biphasic defibrillators, monophasic defibrillators are acceptable (Class IIb, LOE B). BiPhasic shocks should follow manufacturers recommendations (Class I, LOE B). When this is not known, Defib at the maximal dose is acceptable (Class IIb, LOE C).
- 85. Multi-phasic Defibrilators Data from animal studies suggest that multiphasic waveforms (triphasic, quadriphasic, or higher) may defibrillate at lower energies and induce less postshock myocardial dysfunction. Human trials are pending “ Current” based Defib also under exploration.
- 86. PEDIATRIC Defib Discussed in more detail later In pediatric defibrillation, there are limited data regarding the lowest effective dose or the upper limit for safe defibrillation. Initial monophasic doses of 2 J/kg are effective in terminating 18% to 50% of VF and 48% of VF using similar doses of biphasic energy. However, even with higher energies (up to 9J/kg), defibrillation has been successful with no clear adverse effects. Thus, for pediatric patients, it is acceptable to use an initial dose of 2 to 4 J/kg (Class IIa, LOE C), but for ease of teaching an initial dose of 2 J/kg may be considered. For refractory VF, it is reasonable to increase the dose to 4 J/kg. Subsequent energy levels should be at least 4 J/kg, and higher energy levels may be considered, not to exceed 10 J/kg or the adult maximum dose (Class IIb, LOE C).
- 87. CPR integration after Defibrillation Similar to 2005 recommendations, there is no pulse check after defib Immediate CPR should be performed, even if an organized rhythm is seen. (Class I, LOE B)
- 88. Defib and an ICD Allow 30 – 60 seconds after an ICD shock prior to a manual/AED shock. A/P placement of pads prefered, but A/L placement acceptable. Place pads at least 8 cm away from ICD/Pacer
- 89. In Hospital AED programs Limited evidence, but consensus supports this approach, especially in low acuity and unmonitored wards. In Hospital AED programs have resulted in a lower collapse to shock interval. Goal is less than 3 minutes to shock from collapse.
- 90. VT and TdP: To Sync or not to Sync? VT (w/Pulse) Treat as SVT: SYNC TdP (w/Pulse) treat as VT W/O pulse: DEFIB VT and TDP W/O Pulse: DEFIB
- 91. PACING No Longer Recommended for ROUTINE use in Asystole and PEA (Class III, LOE B). This is due to “may interrupt CPR” PACING still Ok for Refractory Bradycardia, and 3 rd AVB’s
- 92. AIRWAY
- 93. Cric Pressure (Really???) Cricoid pressure in nonarrest patients may offer some measure of protection to the airway from aspiration and gastric insufflation during bag-mask ventilation. However, it also may impede ventilation and interfere with placement of a supraglottic airway or intubation. If cricoid pressure is used in special circumstances during cardiac arrest, the pressure should be adjusted, relaxed, or released if it impedes ventilation or advanced airway placement. The routine use of cricoid pressure in cardiac arrest is not recommended (Class III, LOE C).
- 94. FiO2 (During Arrest) Use of 100% inspired oxygen (FIO21.0) as soon as it becomes available is reasonable during resuscitation from cardiac arrest (Class IIa, LOE C).
- 95. FiO2 (post arrest) Increasing Data that hyper-oxia may increase incidence of poor neurological outcomes and increased pulmonary injury. Exact FiO2 recommendations have not been determined. In the post arrest phase, if equipment is available, titration of FiO2 to SPO2 04% is recommended (Class I, LOE C).
- 96. Passive O2 delivery during arrest Passive O2 delivary via ETT (Boussignac tube, or standard ETT) as well as via NRB, has been reviewed. In theory, because ventilation requirements are lower than normal during cardiac arrest, oxygen supplied by passive delivery is likely to be sufficient for several minutes after onset of cardiac arrest with a patent upper airway. The studies involved resulted in improved outcomes., but it is unsure what role (if any) passive O2 had. At this time there is insufficient evidence to support the removal of ventilations from CPR performed by ACLS providers.
- 97. ETT There are no studies directly addressing the timing of advanced airway placement and outcome during resuscitation from cardiac arrest. Although insertion of an endotracheal tube can be accomplished during ongoing chest compressions, intubation frequently is associated with interruption of compressions for many seconds. EMS Should be doing all first attempts DURING CPR. Placement of a supraglottic airway is a reasonable alternative to endotracheal intubation and can be done successfully without interrupting chest compressions.
- 98. ETT Continued In a registry study of 25,006 in-hospital cardiac arrests, earlier time to invasive airway (5 minutes) was not associated with improved ROSC but was associated with improved 24-hour survival. In an urban out-of-hospital setting, intubation that was achieved in 12 minutes was associated with better survival than intubation achieved in 13 minutes
- 99. ETT (MORE GOOD NEWS) In out-of-hospital urban and rural settings, patients intubated during resuscitation had a better survival rate than patients who were not intubated, whereas in an in-hospital setting, patients who required intubation during CPR had a worse survival rate. Jennings PA, Cameron P, Walker T, Bernard S, Smith K. Out-of-hospitalcardiac arrest in Victoria: rural and urban outcomes. Med J Aust. 2006;185:135–139. Dumot JA, Burval DJ, Sprung J, Waters JH, Mraovic B, Karafa MT, Mascha EJ, Bourke DL. Outcome of adult cardiopulmonary resuscitations at a tertiary referral center including results of “limited” resuscitations. Arch Intern Med. 2001;161:1751–1758.
- 100. ETT (Moral of story) There are two pitfalls of ETT placement: 1- Interruption of CPR 2- Poor Placement practices. Therefore, Place during CPR if possible, and optimize first attempt (bougie, etc) If you CANT do this, then use a supraglottic airway. If you cant o this, perhaps you should not be a paramedic? Hmmmmmm……
- 101. ETT The provider should weigh the need for minimally interrupted compressions against the need for insertion of an endotracheal tube or supraglottic airway. If advanced airway placement will interrupt chest compressions, providers may consider deferring insertion of the airway until the patient fails to respond to initial CPR and defibrillation attempts or demonstrates ROSC (Class IIb, LOE C).
- 102. Securing the Tube Commercial Device (Class I, LOE C). C-Collar and/or LSB (Class IIb, LOE C)
- 103. Monitoring of ETT Continuous Waveform PETCO2 (Class I, LOE A). Colormetric or Non-Waveform PETCO2 (Class IIa, LOE b) when Cont waveform is not available. HOWEVER, not superior to auscultation and visualization. EDD (Class IIa, LOE B) for initial but not continuous monitoring.
- 104. ACLS
- 107. ACLS – BIG CHANGE “… vascular access, drug delivery, and advanced airway placement should not cause significant interruptions in chest compression or delay defibrillation.” “ There is insufficient evidence to recommend a specific timing or sequence (order) of drug administration and advanced airway placement during cardiac arrest. In most cases the timing and sequence of these secondary interventions will depend on the number of providers participating in the resuscitation and their skill levels. Timing and sequence will also be affected by whether vascular access has been established or an advanced airway placed before cardiac arrest.”
- 108. ACLS- Vasopressors EPI: Higher doses may be indicated to treat specific problems, such as a -blocker or calcium channel blocker overdose. (Class IIb, LOE A). 1 dose of vasopressin 40 units IV/IO may replace either the first or second dose of epinephrine in the treatment of cardiac arrest (Class IIb, LOE A). There are no alternative vasopressors (norepinephrine, phenylephrine) with proven survival benefit compared with epinephrine in arrest.
- 109. ACLS- Vasopressors in arrest The peak effect of an intravenous (IV)/intraosseous (IO) vasopressor given as a bolus dose during CPR is delayed for at least 1 to 2 minutes. Therefore the exact timing to give vasopressors has not been determined.
- 110. ACLS- Vasopressors in arrest Potentially, if a vasopressor is given with ROSC, care could be compromised. Pausing for rhythm checks during the 2 min cycle is not recommended, but monitoring of PETCO2 is. If PETCO2 abruptly increases to a normal value (35 to 40 mm Hg), it is reasonable to consider that this is an indicator of ROSC (Class IIa, LOE B). Vasopressors may be deferred until next rhythm check.
- 111. ACLS- Anti-arrhythmics Amiodarone (Class IIb, LOE A) remains a primary recommendation Lidocaine (Class IIb, LOE B) as a secondary due to lack of research. Procainimide may be more effective in terminating VF than lidocaine, but dosage regimen is cumbersome. Mag Sulfate only for TdP (Class IIb, LOE B).
- 112. ACLS- Atropine Atropine gone for Aystole/PEA “ There is no evidence that atropine has detrimental effects during bradycardic or asystolic cardiac arrest.” “… Available evidence suggests that the routine use of atropine during PEA or asystole is unlikely to have a therapeutic benefit (Class IIb, LOE B). For this reason atropine has been removed from the cardiac arrest algorithm.”
- 113. ACLS- BiCarb In some special resuscitation situations, such as preexisting metabolic acidosis, hyperkalemia, or tricyclic antidepressant overdose, bicarbonate can be beneficial However, routine use of sodium bicarbonate is not recommended for patients in cardiac arrest (Class III, LOE B). What Defines ROUTINE???? Does prolonged down time count?
- 114. ACLS- Vascular Access Several human and animal studies indicate that delay of drugs may effect ROSC. These were multi-factorial and small. That said, vascular access should be a priority, as long as it does not interrupt CPR. It is reasonable for providers to establish IO access if IV access is not readily available (Class IIa, LOE C). THIS DOES NOT MANDATE IO PLACEMENT INSTEAD OF IV. Central Venous Access (Class IIb, LOE C) for the appropriately trained provider. Peak drug concentrations are higher and drug circulation times shorter
- 115. ACLS- Precordial Thump is BAAACK! Precordial thump was associated with ROSC when administered promptly to patients with responder-witnessed asystolic arrest in one study (huh?) and Pulseless VT/VF in another. Not likely to be effective but should do “no apparent harm.” The precordial thump may be considered for termination of witnessed monitored unstable ventricular tachyarrhythmias when a defibrillator is not immediately ready for use (Class IIb, LOE B), but should not delay CPR and shock delivery.
- 116. ACLS- EARLY PCI FOR MI ARRESTS TdP, Hx of MI S/S prior to arrest, recurrent/refractory VT/VF
- 117. BradyCardias Atropine remains (Class IIa, LOE B). THEN Pacing High AVB (Class IIb, LOE C). Refractory to atropine (Class IIa, LOE C) Dopamine Not a“New Dose” to TYPO, BEGIN @ 2-10 mcg/kg/min, then Titrate Epi Drips @2-10 mcg/min Iisoproterenol @2-10 mcg/min
- 119. TachyCardias Adenocard – No change Procainimide – No Change Ca Channel Blockers Diltizem or Verapamil K channel blockers Sotalol 100 mg (or 1.5 mg/kg) (Class IIb, LOE B) can be considered. May be more effective than Lidocaine Lidocaine is “less effective” in stable VT than Procainimide, Amiodarone, or Sotalol Still an option (Class IIb, LOE B)
- 120. Tachycardia’s : A-Fib Beta -blockers and nondihydropyridine calcium channel blockers such as diltiazem are the drugs of choice for acute rate control in most individuals with atrial fibrillation and rapid ventricular response (Class IIa, LOE A).
- 123. POST ARREST CARE
- 124. Drugs Note: Epi Dose Dopamine Dose Milrinone
- 125. Vasoactive Drugs More emphasis on crystaloid fluids as well.
- 127. Questions?
- 128. “ It is up to us to save the world.” - Peter Safar
































![A simultaneous, choreographed approach? Much more emphasis on the team approach; and a realistic recognition of what and how PARAMEDICS do their job! Recognition that resuscitation is not a “linier” process (Step A, THEN Step B, etc) but a simultaneous series of actions. “… .in a highly specialized environment, such as a critical care unit of a hospital, many of the individual components of CPR (compression-ventilation-defibrillation) may be managed simultaneously. This approach requires choreography among many highly-trained rescuers who work as an integrated team. In the pre-hospital setting, the order of the CPR components performed by the healthcare provider may switch between a sequenced and choreographed model depending on the proficiency of the provider and the availability of resources.” - Circulation . 2010;122[suppl 3]:S676 –S684. “ It is reasonable for healthcare providers to tailor the sequence of rescue actions to the most likely cause of arrest.” THIS MEANS NO MORE COOK-BOOK MEDICINE!!!!! ](https://image.slidesharecdn.com/2010eccoverviewcolev0-2-110310094010-phpapp01/85/2010-ECC-overview-cole-v0-2-32-320.jpg)