2b. malignant nasal paranasal sinus ca.pptx
- 2. Epidemiology • Maxillary sinus ca – 70% • Ethmoid(20%),frontal(3%),sphenoid(1%) sinus ca – extremely rare • 3% of head and neck malignacies • M > F ( 2 : 1 ) • Age – 6th & 7th decades • Carpenters, saw mill workers • Occupational exposure • Smoking • Alcohol
- 3. Occupational agents correlated with sinonasal cancer
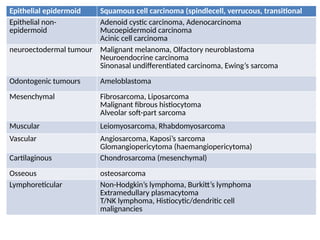
- 4. Epithelial epidermoid Squamous cell carcinoma (spindlecell, verrucous, transitional Epithelial non- epidermoid Adenoid cystic carcinoma, Adenocarcinoma Mucoepidermoid carcinoma Acinic cell carcinoma neuroectodermal tumour Malignant melanoma, Olfactory neuroblastoma Neuroendocrine carcinoma Sinonasal undifferentiated carcinoma, Ewing’s sarcoma Odontogenic tumours Ameloblastoma Mesenchymal Fibrosarcoma, Liposarcoma Malignant fibrous histiocytoma Alveolar soft-part sarcoma Muscular Leiomyosarcoma, Rhabdomyosarcoma Vascular Angiosarcoma, Kaposi’s sarcoma Glomangiopericytoma (haemangiopericytoma) Cartilaginous Chondrosarcoma (mesenchymal) Osseous osteosarcoma Lymphoreticular Non-Hodgkin’s lymphoma, Burkitt’s lymphoma Extramedullary plasmacytoma T/NK lymphoma, Histiocytic/dendritic cell malignancies
- 5. Squamous cell carcinoma • Squamous cell carcinoma remains the most common sinonasal malignancy • The majority probably arise in the maxillary sinus • Rarely the nasal septum or columella are the primary site. • These tumours have a particularly poor prognosis due to the possibility of bilateral metastatic spread to cervical nodes.
- 6. ADENOCARCINOMA • Aout 30 per cent of patients with this condition are woodworkers. • These tumours usually arise in the middle meatus and spread into the ethmoid • Adenocarcinoma is generally rather radioresistant but combined therapy is usually offered. • Many patients require a craniofacial but in selected cases have been treated successfully by an endoscopic resection.
- 7. Adenoid cystic carcinoma • Propensity to spread along perineural lymphatics which compromises attempts at excision. • known to produce blood-borne metastases, classically to the lung while lymphatic spread is rare. • Treatment is generally combined surgery and radiotherapy
- 8. OLFACTORY NEUROBLASTOMA (OR) ESTHESIONEUROBLASTOMA • classically arises from olfactory epithelium in the upper nasal vault • The presence of a mass in the upper nasal cavity with associated skull base erosion is typical. • bimodal peak in the second/third and sixth/seventh decades. • Cervical metastases have been described in up to 23%. • These are routinely resected in craniofacial approaches • Endoscopic resection is being increasingly offered for this tumour particularly when it arises from the middle and superior turbinates. • should always be combined with radiotherapy.
- 9. Ohngren's Line · Line running from medial canthus to angle of mandible · Prognosis of suprastructure tumors worse (This was before advent of craniofacial resection)
- 10. Natural history & spread Maxillary ca
- 11. Natural history & spread - contd Ethmoidal ca
- 12. Natural history & spread – contd… Sphenoid sinus ca Frontal sinus ca
- 13. Lymphatic Drainage • Usually sparse-10% incidence of cervical LNE • If tumor extension into skin of face, nasal cavity, NPX -> ↑ed incidence of LN->Assocated with poor prognosis • First echelon: submandibular nodes • Second echelon: subdigastric nodes - same side • Contralateral mets. extremely rare
- 14. Clinical features Maxillary sinus ca • Facial swelling, pain, paresthesia of cheek • Epistaxis, nasal discharge, obstruction • Ill fitting dentures, alveolar/palatal mass • Proptosis, diplopia, impaired vision, orbital pain Ethmoid sinus ca • Headache • Referred pain to nasal, retrobulbar region • SC mass at inner canthus, nasal obstruction,discharge, diplopia & proptosis
- 15. Work up • H & P • Routine blood examination • CXR- Adenocystic ca • CT/MRI • Dental evaluation • Baseline ophthalmologic examn • Baseline speech & swallowing assessment • Fiberoptic endoscopic examination & Bx
- 16. Computed Tomography • Bone erosion – orbit, cribiform plate – fovea, post max sinus wall – sphenoid, post wall of frontal sinus • 85% accuracy • ? Tumor vs. inflammation vs. secretions • Limitation-periorbital involvement • CT Chest for Adenocystic ca
- 17. MRI • Superior to CT - multiplanar - Detect intracranial, perineural & leptomeningeal spread • Inflammatory tissue & secretions - intense T2 • Tumor - intermediate T1 & T2 (low signal) • 94% accuracy • gadolinium (enhancement) 98% accuracy
- 18. Primary tumor (T) Maxillary sinus: TX Primarytumorcannotbe assessed T0 No evidence ofprimarytumor Tis Carcinoma insitu T1 Tumor limited to maxillarysinus mucosa with noerosionordestructionofbone T2 Tumor causingbone erosionordestruction, includingextension into the hard palate and/or middlenasalmeatus, exceptextension to posteriorwallofthe maxillarysinus and pterygoidplates T3 Tumor invades anyofthe following:bone ofthe posteriorwallofthe maxillarysinus, subcutaneous tissues, flooror medial wallofthe orbit, pterygoid fossa, ethmoidsinuses T4a Moderatelyadvanced localdisease Tumor invades theanteriororbitalcontents, skinofthe cheek, pterygoid plates, infratemporalfossa, cribriformplate, sphenoidorfrontalsinuses T4b Veryadvanced localdisease Tumor invades anyofthe following: orbitalapex, dura, brain, middle cranialfossa, cranial nerves otherthan maxillarydivisionoftrigeminalnerve (V2), nasopharynx, orclivus
- 19. AJCC- Nasal cavity & Ethmoid Sinus Tx - Primary tm cannot be assessed To - no evidence of primary tm Tis - carcinoma in situ T1 - Tm restricted to any one subsite with or without bony invasion T2 - invading two subsite in a single region or extending to involve an adjacent region within the nasoethmoidal complex T3 - invade medial wall/ floor of orbit, maxillary sinus,palate/ cribiform plate T4a - invade ant orbital contents, skin of nose /cheek, ant cranial fossa, pterygoid plates,sphenoid/ frontal sinus T4b - orbital apex, dura, brain,mid cranial fossa, cr nerves, nasopharynx/ clivus
- 20. Staging – contd… Nx - regional nodal status cannot be assessed, No - No regional lymph node metastasis N1 - single I/L clinically +ve lymph node ≤ 3cm N2 - metastasis in ipsilateral, bilateral, contralateral node N2a - single I/L +ve LN >3cm <6cm N2b - multiple, I/L +ve LN <6cm N2c - B/L or C/L LN <6cm N3 - any LN > 6cm Mx - distant metastasis cannot be assessed Mo - No distant metastasis M1 -distant metastasis
- 21. Staging – contd… Stagewise distribution stage I - T1N0M0 stage II – T2N0M0 stage III – T3N0M0 OR T1-T3N1M0 stage IV : - IVA -T4N0-1M0 any TN2 M0 - IVB any TN3M0 - IVC any T any N, M1
- 22. Treatment options Maxillary sinus ca • Surgery • Radiotherapy - definitive - pre op RT - post op RT • Combined modality ( Sx + RT) • Chemotherapy - Neo adjuvant - Concomitant
- 24. Stagewise Treatment – contd…
- 25. Surgery Contraindications - extension thr ant. Fossa - involvement of both optic n. - post. extension into sphenoid sinus - invasion of middle cranial fossa - extension into NPx - inoperable neck node & distant mets
- 26. • CRANIOFACIAL RESECTION • MIDFACIAL DEGLOVING • LATERAL RHINOTOMY • MAXILLECTOMY • ENDOSCOPIC RESECTION • TOTAL RHINECTOMY
- 27. Craniofacial resection • the ‘gold standard’ for tumours affecting the anterior skull base. CONTRAINDICATIONS • Extensive frontal lobe and/or middle cranial fossa involvement or bilateral orbital invasion/optic chiasm. • Certain histologies, such as mucosal malignant melanoma where extent of surgery does not influence outcome • those where surgery is not appropriate, such as sinonasal undifferentiated carcinoma, lymphoma, plasmacytoma. • Distant metastasis.
- 28. INCISION • Following bilateral temporary tarsorrhaphies, an extended lateral rhinotomy is made on the side of maximal tumour involvement
- 29. TECHNIQUE • The soft tissues of the face are mobilized by subperiostial elevation to expose the nasal bones, frontal processes of the maxilla and frontal bone up to the hairline via an extended lateral rhinotomy. • Through the lateral rhinotomy, the upper lateral cartilage is separated from the nasal bone to allow complete retraction of the nasal ala. • The orbital periosteum is elevated to expose the lacrimal fossa and the medial orbital wall. The nasolacrimal duct is often transacted obliquely at this point • anterior and posterior ethmoidal arteries are divided after bipolar coagulation. • If the lamina has been eroded by tumour, the adjacent periorbita should be resected for frozen section assessment
- 30. • A shield-shaped craniotomy is performed above the level of the supraorbital rim to include the frontal sinus. usually approximately 3x3x3.5 cm size. • The frontal sinus which has been opened by this manoeuvre is cleared of its mucosa and the posterior wall removed combined with a wide dissection of the dura. • Dissection around the cribriform plate and crista galli is facilitated by the use of the operating microscope. • This dissection continues until the cribriform plate is exposed and continues on to the jugum of the sphenoid. • In cases of olfactory neuroblastoma routinely the olfactory bulb and tracts are removed in continuity. • The anterior and posterior ethmoidal arteries are coagulated with the bipolar diathermy although care must be exercised as the optic nerve is approached.
- 33. • Osteotomies are performed around the cribriform plate through the ethmoidal and sphenoid roofs. • The posterior osteotomy crosses the planum sphenoidale to include the anterior face of the sphenoid and the nasal septum is separated by quadrilateral cuts. • The specimen is mobilized this can be removed, haemostasis achieved and the cavity inspected for further resection. • fashion a large middle meatal antrostomy to prevent subsequent infection. • dura has small defects which can be repaired primarily but more with fascia lata held in place with fibrin glue to which a split-skin graft taken from the thigh is applied inferiorly. • The frontal bone flap is replaced and secured with miniplates. • The periosteum and subcutaneous layer is closed with absorbable sutures and skin with clips or fine skin sutures. A pressure dressing is applied to both the head and leg.
- 34. POST OP CARE • Patients are kept in a neutral position of approximately 15 degree for the first 2 or 3 days and then gently elevated. • The urinary catheter is removed on the second or third day and facial sutures after 5–7 days. • The anticonvulsant is continued for 6 weeks following the operation and patients must douche the nose long term.
- 35. • Complications are: • IMMEDIATE: • – convulsions • – haemorrhage • – air embolism • INTERMEDIATE: • – cerebrovascular accident • – confusion • – pulmonary embolism • – meningitis • – aerocele • LONG TERM: • – haemorrhage • – frontal abscess/encephalitis • – bone necrosis/fistula • – cerebrospinal fluid leak • – epilepsy • – epiphora • – diplopia • – serous otitis media • – sinusitis/mucocele • – cellulitis • – pituitary deficiency
- 36. MIDFACIAL DEGLOVING • The degloving approach affords excellent access to the middle third of the face. • Indicated in malignant tumours affecting the nasal cavity,maxilla,ethmoids,sphenoid, pterygopalatine and infratemporal fossae. INCISION • After temporary tarrsoraphies, a bilateral sublabial incision is made from maxillary tuberosity to tuberosity down to bone • Routine rhinoplasty intercartilaginous incisions are made extending into a transfixion incision along the dorsal and caudal borders of the cartilaginous septum,separating it from the medial crura of the lower lateral cartilages. • The circumferential incisions are joined across the floor of the nose just anterior to the pryriform aperture.
- 38. • The soft tissues of the midface are elevated subperiosteally up to the infraorbital nerve on each side to display the pyriform aperture. • The soft tissues over the nasal bridge are elevated as far as the root of the nose and laterally to complete the mobilization from below so that the mid-third of the face is completely elevated and can be lifted superiorly over the nasal skeleton. • nasal cavities and maxillary sinuses can be opened using drills, hammers and osteotomes. • maxillary and sphenopalatine arteries accessed and ligated
- 41. • ethmoids, sphenoid, nasopharynx and structures posterior and lateral to the maxillae are reached for further resection. • Closure of the incisions must be done with care to avoid complications, using absorbable suture material. • The bridge of the nose may be taped or a rhinoplasty dressing applied for a few days. • After pack removal patients advised to use saline douching daily until crusting settles.
- 42. Lateral rhinotomy • Indicated in any malignant tumour affecting the nasal septum,lateral wall and extending into ethmoid, sphenoid, maxillary sinuses and up to the anterior skull base INCISION • After a temporary tarrsoraphy, the incision runs from the level of the medial canthus, midway between the canthus and nasal bridge in the nasomaxillary groove, curving round the lower ala into the nasal cavity
- 43. TECHNIQUE • Through the incision, the orbital periosteum can be dissected from the lamina and the nasolacrimal duct mobilized.The duct can be transected obliquely adjacent to the sac. • Anterior and posterior ethmoidal arteries ligated • An en bloc or piecemeal removal of lateral nasal wall done including the pyriform aperture,nasal bone,frontal process of maxilla,anterior maxillary wall,medial orbital wall and rim,ethmoids lamina pipyracea and lacrymal fossa depending upon extend of tumour. • The sphenoid sinus can be opened,frontal can be accesed,orbital periosteum can be resected if required
- 44. MAXILLECTOMY • Malignant tumors of maxilla involving all walls with/without orbital extension. INCISION -Weber-Fergusson incision extends 1cm lateral to the lateral canthus and medially 3mm below the lower eyelash.at medial canthus incision curves inferiorly into nasomaxillay groove down to alar margin.it continues medially to the midline where it turns at right angle dividing the upper lip. -incision extends round the upper alveolus in the gingivobuccal sulcus upto maxillary tuberosity.medially incision pass to hard palate between the central incisors as far as junction of hard and soft palate,then crosses laterally to the poserior aspect of maxillary tuberosity
- 46. TECHNIQUE • The entire soft tissue of cheek are raised subperiosteally off the maxilla from the pyriform apperture to the zygomatic arch including buccinator • The orbicularis oculi left intact around the eye but the orbital periosteum is incised at the bony rim allowing dissection of orbital contents.infraorbital neurovascular bundle is cut at the infra orbital foramen. • Osteotomies are made through the zygoma beneath the infraorbital rim,across the frontal process of maxilla,into pyriform fossa,inferiorly through the central upper alveolus.lateral nasal wall divided below the superior turbinate. • Mobilization of maxilla completed by seperating the tuberosity from the pterygoid plates.
- 49. • A variety of reconstructions are available. • At its simplest,a split skin graft can be applied to the cavity wall held in place with quilting incisions,biological glues,and a temporary gutta percha prosthesis. • Alternatively a free flap can be utilized, e.g. rectus abdominis, latissimus dorsi, radial or fibula osteocutaneous flaps with osseointegration • Repairing lost orbital support decreases the risk of globe malposition, diplopia and disturbance of extraocular muscle function. • Small defects in the floor can be left, larger ones can be repaired using a fascia lata sling secured to the margins of the bony defect
- 50. • Extensive spread of the tumour anteriorly into the facial skin may necessitate sacrifice of this with repair using a local pedicled or free microvascular flap. • More frequently, extension occurs posteriorly into the pterygoid region which adversely affects prognosis. • Limited areas of pterygoid muscle can be removed. • clearance of the pterygopalatine and infratemporal fossae can be undertaken.
- 51. Reconstruction and Prosthetic Rehabilitation Aim : • - prevent contracture of the check • -to separate oral & nasal cavities • -to provide support for the globe . • -An obturator should be made preoperatively from an impression of the hard palate
- 53. Tumours with bad prognosis 1- Advanced maxillary cancer . 2- lesions involving pterygoid plates or pterygopalatine fossa . 3- lesions involving brain , dura , nasopharynx , sphenoid . 4- lesions involving orbital contents
- 54. Follow up • 3 mths after Rx - baseline physical examn - CT, MRI or PET CT • 1st 3 yrs – every 4 mths • 4th & 5th yr – every 6 mths • Then - annually