34061_TORCH_maranich.ppt
- 2. TORCH Infections • T=toxoplasmosis • O=other (syphilis) • R=rubella • C=cytomegalovirus (CMV) • H=herpes simplex (HSV)
- 3. • You are taking care of a term newborn male with birth weight/length <10th %ile. Physical exam is normal except for a slightly enlarged liver span. A CBC is significant for low platelets. • What, if anything, do you worry about? • How do you proceed with a work-up?
- 4. Index of Suspicion • When do you think of TORCH infections? • IUGR infants • HSM • Thrombocytopenia • Unusual rash • Concerning maternal history • “Classic” findings of any specific infection
- 5. Diagnosing TORCH Infection !!!!!!DO NOT USE TORCH TITERS!!!!!!
- 6. Diagnosing TORCH Infection • Good maternal/prenatal history • Remember most infections of concern are mild illnesses often unrecognized • Thorough exam of infant • Directed labs/studies based on most likely diagnosis… • Again, DO NOT USE TORCH TITERS!
- 7. Screening TORCH Infections • Retrospective study of 75/182 infants with IUGR who were screened for TORCH infections • 1/75 with clinical findings, 11/75 with abnl lab findings • All patients screened: • TORCH titers, urine CMV culture, head US • Only 3 diagnosed with infection • NONE by TORCH titer!! • Overall cost of all tests = $51,715 • “Shotgun” screening approach NOT cost effective nor particularly useful • Diagnostic work-up should be logical and directed by history/exam findings Khan, NA, Kazzi, SN. Yield and costs of screening growth-retarded infants for torch
- 8. Toxoplasmosis • Caused by protozoan – Toxoplasma gondii • Domestic cat is the definitive host with infections via: • Ingestion of cysts (meats, garden products) • Contact with oocysts in feces • Much higher prevalence of infection in European countries (ie France, Greece) • Acute infection usually asymptomatic • 1/3 risk of fetal infection with primary maternal infection in pregnancy • Infection rate higher with infxn in 3rd trimester • Fetal death higher with infxn in 1st trimester
- 9. Clinical Manifestations • Most (70-90%) are asymptomatic at birth • Classic triad of symptoms: • Chorioretinitis • Hydrocephalus • Intracranial calcifications • Other symptoms include fever, rash, HSM, microcephaly, seizures, jaundice, thrombocytopenia, lymphadenopathy • Initially asymptomatic infants are still at high risk of developing abnormalities, especially chorioretinitis
- 10. Chorioretinitis of congenital toxo
- 11. Diagnosis • Maternal IgG testing indicates past infection (but when…?) • Can be isolated in culture from placenta, umbilical cord, infant serum • PCR testing on WBC, CSF, placenta • Not standardized • Newborn serologies with IgM/IgA
- 12. Toxo Screening • Prenatal testing with varied sensitivity not useful for screening • Neonatal screening with IgM testing implemented in some areas • Identifies infected asymptomatic infants who may benefit from therapy
- 13. Prevention and Treatment • Treatment for pregnant mothers diagnosed with acute toxo • Spiramycin daily • Macrolide antibiotic • Small studies have shown this reduces likelihood of congenital transmission (up to 50%) • If infant diagnosed prenatally, treat mom • Spiramycin, pyrimethamine (anti-malarial, dihydrofolate reductase inhib), and sulfadiazine (sulfa antibiotic) • Leucovorin rescue with pyrimethamine • Symptomatic infants • Pyrimethamine (with leucovorin rescue) and sulfadiazine • Treatment for 12 months total • Asymptomatic infants • Course of same medications • Improved neurologic and developmental outcomes demonstrated (compared to untreated pts or those treated for only one month)
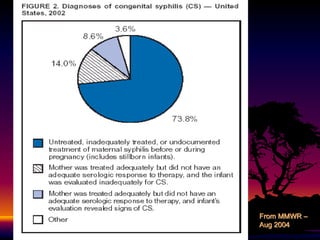
- 14. Syphilis • Treponema pallidum (spirochete) • Transmitted via sexual contact • Placental transmission as early as 6wks gestation • Typically occurs during second half • Mom with primary or secondary syphilis more likely to transmit than latent disease • Large decrease in congenital syphilis since late 1990s • In 2002, only 11.2 cases/100,000 live births reported
- 15. From MMWR – Aug 2004
- 16. From MMWR – Aug 2004
- 17. Congenital Syphilis • 2/3 of affected live-born infants are asymptomatic at birth • Clinical symptoms split into early or late (2 years is cutoff) • 3 major classifications: • Fetal effects • Early effects • Late effects
- 18. Clinical Manifestations • Fetal: • Stillbirth • Neonatal death • Hydrops fetalis • Intrauterine death in 25% • Perinatal mortality in 25-30% if untreated
- 19. Clinical Manifestations • Early congenital (typically 1st 5 weeks): • Cutaneous lesions (palms/soles) • HSM • Jaundice • Anemia • Snuffles • Periostitis and metaphysial dystrophy • Funisitis (umbilical cord vasculitis)
- 20. Periostitis of long bones seen in neonatal syphilis
- 21. Clinical Manifestations • Late congenital: • Frontal bossing • Short maxilla • High palatal arch • Hutchinson teeth • 8th nerve deafness • Saddle nose • Perioral fissures • Can be prevented with appropriate treatment
- 22. Hutchinson teeth – late result of congenital syphilis
- 23. Diagnosing Syphilis (Not in Newborns) • Available serologic testing • RPR/VDRL: nontreponemal test • Sensitive but NOT specific • Quantitative, so can follow to determine disease activity and treatment response • MHA-TP/FTA-ABS: specific treponemal test • Used for confirmatory testing • Qualitative, once positive always positive • RPR/VDRL screen in ALL pregnant women early in pregnancy and at time of birth • This is easily treated!!
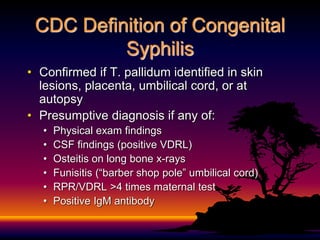
- 24. CDC Definition of Congenital Syphilis • Confirmed if T. pallidum identified in skin lesions, placenta, umbilical cord, or at autopsy • Presumptive diagnosis if any of: • Physical exam findings • CSF findings (positive VDRL) • Osteitis on long bone x-rays • Funisitis (“barber shop pole” umbilical cord) • RPR/VDRL >4 times maternal test • Positive IgM antibody
- 25. Diagnosing Congenital Syphilis • IgG can represent maternal antibody, not infant infection • This is VERY intricate and often confusing • Consult your RedBook (or peds ID folks) when faced with this situation
- 26. Treatment • Penicillin G is THE drug of choice for ALL syphilis infections • Maternal treatment during pregnancy very effective (overall 98% success) • Treat newborn if: • They meet CDC diagnostic criteria • Mom was treated <4wks before delivery • Mom treated with non-PCN med • Maternal titers do not show adequate response (less than 4-fold decline)
- 27. Rubella • Single-stranded RNA virus • Vaccine-preventable disease • No longer considered endemic in the U.S. • Mild, self-limiting illness • Infection earlier in pregnancy has a higher probability of affected infant
- 28. Copyright ©2006 American Academy of Pediatrics Meissner, H. C. et al. Pediatrics 2006;117:933-935 Reported rubella and CRS: United States, 1966-2004
- 29. Clinical Manifestations • Sensorineural hearing loss (50-75%) • Cataracts and glaucoma (20-50%) • Cardiac malformations (20-50%) • Neurologic (10-20%) • Others to include growth retardation, bone disease, HSM, thrombocytopenia, “blueberry muffin” lesions
- 30. “Blueberry muffin” spots representing extramedullary hematopoesis
- 31. Diagnosis • Maternal IgG may represent immunization or past infection - Useless! • Can isolate virus from nasal secretions • Less frequently from throat, blood, urine, CSF • Serologic testing • IgM = recent postnatal or congenital infection • Rising monthly IgG titers suggest congenital infection • Diagnosis after 1 year of age difficult to establish
- 32. Treatment • Prevention…immunize, immunize, immunize! • Supportive care only with parent education
- 33. Cytomegalovirus (CMV) • Most common congenital viral infection • ~40,000 infants per year in the U.S. • Mild, self limiting illness • Transmission can occur with primary infection or reactivation of virus • 40% risk of transmission in primary infxn • Studies suggest increased risk of transmission later in pregnancy • However, more severe sequalae associated with earlier acquisition
- 34. Clinical Manifestations • 90% are asymptomatic at birth! • Up to 15% develop symptoms later, notably sensorineural hearing loss • Symptomatic infection • SGA, HSM, petechiae, jaundice, chorioretinitis, periventricular calcifications, neurological deficits • >80% develop long term complications • Hearing loss, vision impairment, developmental delay
- 36. Diagnosis • Maternal IgG shows only past infection • Infection common – this is useless • Viral isolation from urine or saliva in 1st 3weeks of life • Afterwards may represent post-natal infection • Viral load and DNA copies can be assessed by PCR • Less useful for diagnosis, but helps in following viral activity in patient • Serologies not helpful given high antibody in population
- 37. Treatment • Ganciclovir x6wks in symptomatic infants • Studies show improvement or no progression of hearing loss at 6mos • No other outcomes evaluated (development, etc.) • Neutropenia often leads to cessation of therapy • Treatment currently not recommended in asymptomatic infants due to side effects • Area of active research to include use of valgancyclovir, treating asx patients, etc.
- 38. Herpes Simplex (HSV) • HSV1 or HSV2 • Primarily transmitted through infected maternal genital tract • Rationale for C-section delivery prior to membrane rupture • Primary infection with greater transmission risk than reactivation
- 39. Clinical Manifestations • Most are asymptomatic at birth • 3 patterns of ~ equal frequency with symptoms between birth and 4wks: • Skin, eyes, mouth (SEM) • CNS disease • Disseminated disease (present earliest) • Initial manifestations very nonspecific with skin lesions NOT necessarily present
- 40. Presentations of congenital HSV
- 41. Diagnosis • Culture of maternal lesions if present at delivery • Cultures in infant: • Skin lesions, oro/nasopharynx, eyes, urine, blood, rectum/stool, CSF • CSF PCR • Serologies again not helpful given high prevalence of HSV antibodies in population
- 42. Treatment • High dose acyclovir 60mg/kg/day divided q8hrs • X21days for disseminated, CNS disease • X14days for SEM • Ocular involvement requires topical therapy as well
- 44. Which TORCH Infection Presents With… • Snuffles? • syphilis • Chorioretinitis, hydrocephalus, and intracranial calcifications? • toxo • Blueberry muffin lesions? • rubella • Periventricular calcifications? • CMV • No symptoms? • All of them
- 45. Which TORCH Infections Can Absolutely Be Prevented? • Rubella • Syphilis
- 46. When Are TORCH Titers Helpful in Diagnosing Congenital Infection? • NEVER!
- 47. Questions?