Acute Mental Status Changes[1]
- 1. Acute Mental Status Changes in the Intensive Care Unit Danagra Georgia Ikossi, MD Stanford General Surgery Resident 10/24/2006
- 2. Just because you’re nuts, it doesn’t mean you’re not sick… the ongoing search for organic causes Brief review of Delirium, Seizures and Stroke “ ICU Psychosis” How do you know if they’re confused? (J. Am. Ger. Soc. 2005) Why do they become delirious? (Critical Care 2001) Does delirium portend a poor outcome? (JAMA 2004) Geriatrics: Delirium plus dementia, what to do? (J. Am. Ger. Soc. 2005)
- 3. Disorders of Mentation Abnormalities of mental function Conciousness: Arousal (awake?) Awareness (responsive?) Cognition: Orientation (accurate perception of experiences) Judgment and Reasoning (ability to process data and generate meaningful information) Memory (ability to store and retrieve information)
- 4. Levels of Conciousness Awake: aroused and aware Somnolent: easily aroused and aware Stuporous: aroused with difficulty, impaired awareness Comatose: unarousable and unaware Vegetative state: aroused but unaware
- 5. Etiology of depressed level of consciousness In non head injured patients SMASHED S ubstrate deficiencies (glucose, thiamine) M eningoencephalitis or M ental illness (malingering, psychogenic coma) A lcohol or A ccident (CVA) S eizures H yper-capnia, -glycemia, -thyroid, -thermia OR H ypo-xia, -tension, -thyroid, -thermia E lectrolyte abnormalities (hyperNa, hypoNa, hyperCa) and E ncephalopathies D rugs
- 6. Glascow Coma Scale: GCS Max 15 Min 3 “ T” denotes intubation Eye Opening 4 Spontaneous 3 To Speech 2 To Pain 1 None Verbal 5 Oriented 4 Confused 3 Inappropriate 2 Incomprehensible 1 None 1 None 2 Abnormal Extension 3 Abnormal Flexion 4 Withdraws 5 Localizes 6 Obeys Commands Motor
- 7. Predictive value of GCS at 1 hour: GCS <6, 70% will not regain “satisfactory neurologic recovery” At 3 days, GCS<6, 100% negative outcome
- 8. Septic Encephalopahthy Can be caused by any infection aside from CNS infections Early sign of sepsis Advanced cases progress to multiple abscesses throughout brain matter Similar biochemical changes to hepatic encephalopathy Increased aromatic amino acids, decreased branched chain amino acids in plasma
- 9. Delirium Most common mental disorder in the hospitalized geriatric patient Up to 87% of elderly pts As many as 75% are not recognized by the physician caring for the patient Characterized by: acute mental status change and inattention and disorganized thought or altered level of consciousness -- Hallmark: acute onset and fluctuating clinical course Most often drug related (40%) - but all other organic causes must be ruled out
- 10. DSM-IV Diagnosis of Delirium A. Reduced ability to maintain and shift attention to external stimuli B. Disorganized thinking, as indicated by rambling, irrelevant, or incoherent speech C. At least two of the following: 1. Reduced level of consciousness 2. Perceptual disturbances: misinterpretations, illusions, or hallucinations 3. Disturbance of sleep–wake cycle with insomnia or daytime sleepiness 4. Increased or decreased psychomotor activity 5. Disorientation to time, place, or person 6. Memory impairment D. Abrupt onset of symptoms (hours to days), with daily fluctuation E. Either one of the following: 1. Evidence from history, physical examination, or laboratory tests of specific organic etiologic factor(s) 2. Exclusion of non-organic mental disorders when no etiologic organic factor can be identified
- 11. Delirium Hypoactive delirium: Characterized by lethargy rather than agitation Most common form in the elderly Dementia and Delerium: Both have attention deficits and disordered thought Dementia is not acute and is not fluctuating 75% of delirium in hospital is superimposed on dementia Hospitalization can cause transient or permanent decompensation in the functioning of a patient with preexisting dementia
- 12. Delirium Management identify and eradicate the cause Sedatives for patient protection Post-op use haloperidol Recommends: mild anxiety – 0.5 to 2mg Moderate – 5-10mg severe 10-20mg Double the dose if no response in 20 minutes and redose. Add ativan if partial response.) THIS IS MUCH MORE THAN WE USE “ Maldonado Protocol” AKA: H2A 4am, 10am, 4pm, 10pm increased dose at 10pm for sleep-wake cycle preservation typically start at 2&1mg
- 13. Important to differentiate Delirium from DTs Delirium Tremens Alcohol withdrawal Do not use haldol (lowers seizure threshold) Benzodiazepines are primary treatment Clonidine (alpha-2-agonist) for associated hypertension (also eases withdrawal centrally) \ Valium: Onset 1-2 min, lasts as long as 12 hrs (active metabolite) 10/10/10 (q8 hrs x 3) Ativan: Slow onset (5-15 min) and longest duration (10-20hrs) Versed: Fast onset, short acting Lipid soluble, prolonged sedation if used long term
- 14. Cocaine Related Delirium Treated like Delirium Tremens Benzos, not haldol
- 15. Who becomes delirious? Prospective analysis of over 800 ICU patients in Turkish hospital 11% rate of DSM diagnosis of delirium Collected clinical data and performed stepwise conditional logistic regression to identify predictors of development of delirium (compared to controls) Infection, fever, hypotension, anemia, and “respiratory diseases”. Hypocalcemia, hyponatremia, uremia, increased hepatic enzymes, hyperamylasemia, hyperbilirubinemia, metabolic acidosis Aldemir et al Critical Care 2001
- 16. Delirium, Dementia or Both? Delirium is a risk factor for increased ICU and Hospital length of stay In the geriatric population, becomes difficult to differentiate between underlying dementia and delirium Group at Brown did a prospective study of 118 patients in ICU Baseline dementia diagnosis given by family on Blessed Dementia Scale Delirium diagnosed by CAM and CAM-ICU scales Ely et al JAGS, May 2003
- 17. Blessed-Dementia Scale Activity One point for each, unless otherwise indicated. CHANGES IN PERFORMANCE OF EVERYDAY ACTIVITIES Inability to perform household tasks Inability to cope with small sums of money Inability to remember shortlist of items; for example, in shopping list Inability to find way about indoors Inability to find way about familiar streets more… CHANGES IN HABITS Eating Dressing Sphincter control CHANGES IN PERSONALITY, INTERESTS, DRIVE Increased rigidity Increased egocentricity Impairment of regard of feeling for others Coarsening of affect More….
- 18. CAM ICU SCORE 1. Acute Onset or Fluctuating Course Absent Present acute change in mental status from baseline? OR did the abnormal behavior fluctuate during the past 24 hours? 2. Inattention Absent Present Did the patient have difficulty focusing attention as evidenced by scores less than 8 on either the auditory or visual component of the Attention Screening Examination (ASE)? 3. Disorganized Thinking Absent Present Does the patient have disorganized or incoherent thinking as evidenced by incorrect answers to 2 or more of the following 4 questions and/or demonstrate an inability to follow commands? Questions (Alternate Set A and Set B): 2 sets of logic questions (does a stone float? Does a leaf float?) 4. Altered Level of Consciousness Absent Present Is the patient’s level of consciousness anything other than alert (e.g. vigilant, lethargic or stuporous), or is VAMASS < or > 3 (and not decreased due to sedation)? Alert : Looks around spontaneously, fully aware of environment, interacts appropriately. Vigilant : Hyperalert. Lethargic : Drowsy but easily aroused. Unaware of some elements in the environment, or no appropriate spontaneous interaction with interviewer. Becomes fully aware and appropriate with minimal noxious stimulation. Stupor : Becomes incompletely aware with strong noxious stimulation. Can be aroused only by vigorous and repeated stimuli. As soon as stimulus removed, subject lapses back into unresponsive state. Overall CAM ICU Score: If 1 + 2, and either 3 or 4 is present, patient has delirium. Yes No
- 19. 30% of pts had baseline dementia 14% were depressed 31% had delirium on first interview 70% had delirium sometime during hospitalization Most ICU delirium persisted after leaving ICU Patients with dementia had 2.4x risk of developing delirium during hospital stay compared to matched pts without delirium
- 20. Delirium and mortality 275 patients over 1 year, prospectively enrolled, CAM-ICU and Richmond Agitation-Sedation scale used 81% delirious at some point during ICU stay Compared to well matched controls: Increased mortality (34% vs 15%) Increased length of stay (by 10 days on average) Adjusted Hazard Ratios: 3.4 for mortality and 2.0 for LOS
- 21. Perspective on ICU Psychosis Until the 1990s, ICU pts were sedated and paralyzed and the changes in mental status went unrecognized Once the deleterious effects of longterm paralysis and sedation were realized, there was a decrease in the use of paralytics and sedatives It was realized that patients had changes in mental status Risk factors include: preexisting mental illness, severity of illness, advanced age, medical comorbidity, sleep deprivation and medications Polderman Critical Care 2005
- 22. ‘ ICU psychosis’ was almost ‘normal’consequence of prolonged ICU stay Diagnosis is challenging with hypoactive delirium (more common) Many intensivists use a “wait and see” approach to treatment Others use Haldol liberally – beware the side effects, EPS
- 23. Authors suggest: Basic prevention: Avoid sleep deprivation, increase cognitive stimulation, talk to the patient, play music, early mobilization, avoid dehydration, electrolyte disturbances, and hypoxia High index of suspicion, frequent screening Treatment should be more prompt (prevent sequelae) Stop offending drugs (benzos and narcotics misused to treat “confusion”) Treat with antipsychotics – drug of choice remains haloperidol Monitor for prolonged QT Interacts with multiple othe drugs common in ICU Neuroleptics not well studied in the ICU may be helpful in non-agtated delerium (risperdol, olanzapine, ziprasidone)
- 24. AACM and SCCM Guidelines Critical Care Medicine 2001 Recommendation: Grade B: Routine use of CAM-ICU by nursing to diagnose delerium Drugs: Haldol works by antagonizing dopamine effects in cerebrum and basal ganglia Half life is 18-58 hours Dose dependent QT prolongation, increases risk of ventricular arrhythmias, 3.6% Torsades de Pointes Doses of 20mg at a time have been associated with ventricular arrhythmias Pre-exisiting cardiac disease increases the risk EPS risk is higher with PO haldol and BZOs can mask EPS EPS symptoms can be seen days after stopping drug Can last for 2 weeks in self-limited cases Treat by d/c haldol, give diphenhydramine or benztropine mesylate.
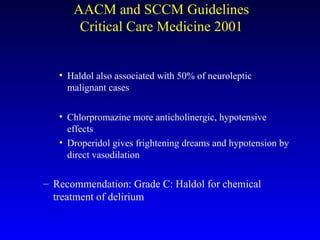
- 25. Haldol also associated with 50% of neuroleptic malignant cases Chlorpromazine more anticholinergic, hypotensive effects Droperidol gives frightening dreams and hypotension by direct vasodilation Recommendation: Grade C: Haldol for chemical treatment of delirium AACM and SCCM Guidelines Critical Care Medicine 2001
- 26. Recommendation: Grade B: non-pharmacologic methods to increase and improve sleep with sedative/hypnotics as adjuncts. Titrate the environmental stimuli Sleep environment should be assessed Ear plugs help Single bed rooms, quiet time Day/night lighting and noise levels Relaxation techniques deep breathing exercises music therapy massage for 5-10 minutes AACM and SCCM Guidelines Critical Care Medicine 2001
- 27. Seizures Second most common neurologic complication in ICU Movements Tonic contractions (sustained contractions) Atonic contraction (no movement) Clonic contraction (periodic contractions with regular frequency and amplitude) Myoclonus (periodic contractions with irregular amplitude and frequency) Automatisms (lipsmacking, chewing, etc)
- 28. Generalized Seizures Symetric and syncrhonous electrical discharge of the entire cerebral cortex May or may not be accompanied by muscular contraction (if none, absence or petit-mal) Partial Seizures Electrical discharges that are confined to a restricted part of cortex Simple partial (does not impair consciousness) Complex partial (does impair consciousness) Temporal lobe seizures: motionless stare and automatisms Epilepsia partialis continua: persistent tonic-clonic movements of facial and limb muscles unilaterally Status Epilepticus more than 30 minutes of continuous seizure activity 2 or more sequential seizures without intervening consciousness
- 29. New Onset Seizures Drug intoxication (amphetamies, cocaine, phenocyclidine, cipro, imipenam, lidocaine, PCN, theophylline, TCA) Drug withdrawal (EtOH, BZO, Barbiturates, Opiates) Infection (Meningoencephalitis, abscess) Ischemia (focal or diffuse) Space occupying lesion (tumors or bleeds) Metabolic derrangement (hepatic encephalopathy, uremia, hypo-glycemia, -natremia, -calcemia)
- 30. Evaluation: Examination looking for lateralizing signs Review of medications Imaging (CT) Procedural diagnostics (LP, labs, blood cultures) Management: BZO Valium 0.2mg/kg IV stops 80% of seizures within 5 min, effect lasts 30 min Ativan 0.1mg/kg is as effective and lasts 12-24hrs Dilantin 20mg/kg following valium, aim for 20mg/l therapeutic serum level
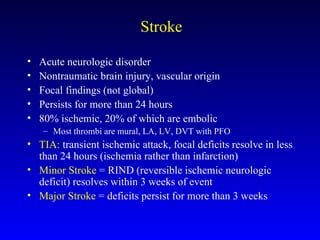
- 31. Stroke Acute neurologic disorder Nontraumatic brain injury, vascular origin Focal findings (not global) Persists for more than 24 hours 80% ischemic, 20% of which are embolic Most thrombi are mural, LA, LV, DVT with PFO TIA: transient ischemic attack, focal deficits resolve in less than 24 hours (ischemia rather than infarction) Minor Stroke = RIND (reversible ischemic neurologic deficit) resolves within 3 weeks of event Major Stroke = deficits persist for more than 3 weeks
- 32. Evaluation: common things you’ll see at the bedside Full neuro exam, looking for focal deficits Seixures in 10% of cases, focal and within first 24 hours Fever in 50% of strokes (not with TIA) – look for other sources Coma and LOC are not common – more likely hemorrhage, massive infarct with edema, brainstem infarction, seizure (absence) or postictal state Aphasia – Left MCA distribution Weakness in contralateral limbs (can also have other metabolic causes)
- 33. Diagnostic Studies Time is brain Coags, Chemistries: hypoglycemia, hyponatremia, ARF ECG: Afib? CT head: 70% sensitivity for infarct, 90% for hemorrhage - critical to distinguish btwn these Better if after 24 hours for infarct MRI: more sensitive esp for brainstem and cerebellar strokes
- 34. Diagnostics and Treatment ICP: monitoring not recommended routinely Elevate HOB 30 degrees Do not use measures that will decrease CBF minimize suctioning ( HTN) Do not hyperventilate (reduces CBF) Steroids not recommended Hyperosmolar therapy can be used if edema is severe (Mannitol, HTS)