AGT notes
- 1. AGT’s Notes compiled by Dr. Pawan Kumar
- 2. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 2 INDEX Page No. 1) Anatomy 02 2) Physiology 06 3) Proforma for cardiac case 09 4) Cardiopulmonary bypass 55 5) Valvular heart disease 70 6) Surgery for valvular heart disease 87 7) Congenital acyanotic heart disease 103 8) Congenital cyanotic heart disease 132 9) Cardiac catheterization 166 10)Coronary artery disease 171 11)Constriction & cardiac tumors 186 12)Aorta, lung & mediastinum 189 13)Trauma & CPR 204 14)X-Rays 206 15)Vascular 208 16)Drugs & First’s 214 17)Instruments 223 18)Surgeons 240 19)Journals 245
- 3. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 3 ANATOMY Q-Where is the term ‘cardiac’ derived from? A-In Greek ‘Kardia’ means ‘Heart’. Q-What is the long axis of the heart? A-It runs from the right shoulder to the left hypochondrium. Q-What is distribution of cardiac mass with respect to midline? A-1/3rd of the cardiac mass lies on the right & 2/3rd on the left. Q-When is a vessel termed as an arteriole or capillaries? A-When diameter is 0.3mm and just visible to the naked eye they are called arterioles. Capillaries are ½ - 1 mm in length and 7μm diameter allowing RBC’s to pass in a single file. Q-Describe the anatomy of bony thorax. A-Upper 6 ribs join with the vertebrae posteriorly & the sternum anteriorly. Ribs 7 – 10 articulate with the vertebral elements posteriorly and then fuse their anterior costal cartilage into the flexible costal margin. 11th and 12th ribs articulate with thoracic vertebrae but are unattached anteriorly. They are referred to as floating ribs. Q-What is the direction of intercostal muscle? A-It is as follows: Muscle Direction External: Hands in front pocket Internal: Hands in back pocket Transversus thoracis: Irregular Q-Describe the anatomy of intercostal arteries. A- Anterior ICA: The Anterior ICA and vein arise from the ITA. Posterior ICA: arise from descending thoracic aorta – 3 – 12 in number. The first two posterior ICA arise from the costocervical trunk. Post IC Veins drain into the azygous and hemiazygous respectively Post ICA bifurcates into 2. Ant and post ICA anastomose near the mid clavicular line The internal mammary artery lies between the sternum and the transverses thoracis. Q-Describe the surface anatomy of valves. A-It is as follows: All the 4 valves lie posterior to the sternum on an oblique line joining the 3rd left sternocostal joint with the 6th right sternocostal joint.
- 4. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 4 Site of auscultation: Pulmonary: left 2nd ICS just left of the sternum Aortic: Right 2nd ICS just right of the sternum Mitral: apex (5th ICS) Tricuspid: 5th ICS on the right of the sternum Q-Describe the nerve supply of heart. A-It is as follows: Sympathetic – cervical sympathetic ganglia & the upper thoracic sympathetic trunk. Parasympathetic- From the Vagus-single cervical branch in neck, 1-2 cervicothoracic branches at inlet and 2-4 thoracic cardiac branches from main branch in thorax. Right vagus supplies the SA node while the left vagus supplies the AV node. Q-Describe briefly the embryology of heart. A- -3rd week- fusion of 2 endocardial tubes forms the primitive heart. -The muscular wall of this to be begins to contract, caudal to cranial -5 sacculations develop, viz., sinus venosus, atrium, ventricle, bulbous cordis & truncus arteriosus. -Constriction between the atria & the ventricle becomes the AV/ coronary sulcus -The paired vessels projecting cranially from the truncus arteriosus, arch posteriorly to form the dorsal aorta, are the first aortic arches -Also the heart is suspended from the posterior wall of the embryo in a dorsal mesocardium -Extensive growth of the heart, relative to the surroundings thoracic structure, causes the primitive heart tube to undergo folding into an ‘S’ shape. -The venous portion of the heart (cardinal veins, sinus venosus & primitive atrium) form the base of the heart, while the primitive ventricle projects anteriorly into the pericardial cavity & the ascending truncus arteriosus exits the pericardial sac superiorly. Fate of dorsal mesocardium- the breakdown of the dorsal mesocardium between the arterial end (bulbous cordis & venous end of primitive atrium) results in the formation of the transverse pericardial sinus. This is the adult heart is demonstrated between the great arteries & the great veins Formation of 4 Chambered heart-4th week of development the partitioning of the primitive heart into 4 chambers begin. Each of the primitive atrium & ventricles begin to separate by saggittal ingrowths, the atrioventricular endocardial cushions. . Their fusion during 5th week results in a partitioned 2-chamber heart with 2 AV canals communicating between the atria & ventricles. Formation of aorta & PA- 5th week a spiral septum forms in the truncus & descends in a clockwise fashion to separated into 2 tubes.
- 5. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 5 Q-Define Mediastinum & its describe its divisions? A- Def. of mediastinum- A septum that divides the thoracic cavity & contains all thoracic viscera, except the lung’s. It extends from posterior aspect of sternum to the bodies of vertebrae & from thoracic inlet superiorly to the diaphragm inferiorly. It is divided by an imaginary line thru’ the sternal angle to T4 / T5 space, the mediastinum is divided into superior & inferior. Inferior is further divided into anterior, middle & posterior. Q-What are the contents of the Mediastinum? A-The contents are: Superior Mediastinum: 1. Retrosternal structures. - Thymus - Great veins. 2. Prevertebral - Trachea - Esophagus - Lt. recurrent laryngeal nerve - Thoracic duct 3. Intermediate - Vagus n - Phrenic n - Aortic arch & 3 branches Q-What thoracic structure is not included in the mediastinum? A-Lungs. Q-What is the fate of aortic arches? A-The aortic arches connect the ventrally placed heart to the paired dorsal aortae. The paired dorsal aortae fuse to form a single aorta caudally. 1st arch (Mandibular arch)- Maxillary artery 2nd arch (hyoid arch)- Hyoid & Stapedial artery. 3rd arch– Rt. & Lt. common carotid 4th arch- on the left side- Arch of aorta between the left CCA & Left SCA On the right side- Right SCA 5th arch – Both sides disappear. 6th arch– Pulmonary arteries & ductus Q-Describe the surface marking of lungs. A-Oblique fissure: anteriorly- 4th rib to anterior axillary line, posteriorly- the 6th rib (level of posterior axillary line) to the vertebral border of the scapula Upper lobe: above 4th rib Middle lobe: between 4th & 6th rib Lower lobe: below 6th rib
- 6. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 6 Q-What is the auscultatory triangle? A-Is formed by: - Lower margin of trapezius - Vertebra - Upper border of latissimus dorsi Q-What is the meaning of term ‘Diaphragm’? A-In greek; ‘Dia’ means thru’ & ‘phragma’ means partition. Q-What is the meaning of term ‘Coarctation’? A-In Latin coarctere means to contract. Q-What is the importance of angle of Louis? A-It corresponds to: - The level of 4th vertebra - Tracheal bifurcation - Arch of aorta traverses the thorax from right to left in a posterolateral direction - Site of 2nd ICS Q-What is the nerve supply of the diaphragm? A-The diaphragm is supplied by the phrenic nerves. [Note:If quadriplegia also involves the diaphragm, it is termed as Pentaplegia.] Q-When does the heart starts beating in an embryo? A-22 days. Q-Why is LA O2% 99% and not 100%? A-Due to drainage into the PV & LA of the: - Bronchial veins - Thebesian veins
- 7. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 7 PHYSIOLOGY Q-What is Ohms law? A-Current= (potential difference)/ (resistance) Q-What is Poiseulle’s law? A-Flow is directly proportional to the 4th power of radius & inversely proportional to the length of narrowing. Hence, Pressure= flow x impedance Systemic BP= systemic flow (CoP) x SVR SVR in Wood units 1 wood= 80 dynes.sec.cm-5 Q-What are the phases of a cardiac electrical cycle? A- Phase 0: rapid depolarization- due to influx of Na+ Phase I: initial repolarization- influx of Cl- Phase II: plateau- balance of K+ outflow with Ca2+ inflow Phase III: late repolarization- continuing K+ efflux Phase IV: resting phase Q-Describe ECG correlation with phase of electrical cycle. A-is Phase 0 & I- QRS complex Phase II- ST segment Phase III- T wave Q-What is the rate of normal coronary blood flow? A-It is 70- 90 ml/100 gm of myocardium/ min Q-What is the rate of myocardial oxygen extraction? A- Normal myocardium- 75% extracted Stressed myocardium- 100% extracted Normally other organs- 25% extracted [Note: Significance of above:Unlike other organs the myocardium cannot extract more oxygen when required. It requires an increase in blood flow.] Q-How is Ejection fraction calculated? A-Ratio of stroke volume to end diastolic volume [(EDV-ESV)/EDV] x 100 Normally 67 8%. Q-Is normal endothelium negatively charged A-Yes.
- 8. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 8 Q-What is the O2 demand of myocardium? A-The O2 demand of myocardium is: < 25ml/100gm/min- exercising 9 ml/100 gm/min- normal 3ml/ 100 gm/ min- beating empty (on bypass) 0.3 ml/ 100 gm/min- arrested with cardioplegia Q-What is Ventricular remodeling A-A series of physiologic adaptations of the ventricles to changes in ventricular filling conditions. Q-Why does the cardiac muscle not get fatigued? A-Due to: 1) Increased blood supply 2) Increased number of mitochondria Q-What is the contribution of the atrial contraction to CoP? A- Normally: 20% In atrial fibrillation: 0% In HOCM: 60- 70% (Thus if a patient of HOCM develops atrial fibrillation, rapid development of pulmonary edema) Q-What is the normal pulmonary blood flow in a fetus A- - 1st trimester 0% - 2nd trimester 3% - 3rd trimester 10% After birth PVR is 2/3rd of SVR. Later it falls due to: - Closure of PDA (within 2 weeks) - Closure of PFO Q-What is the saturation of veins at various sites in the body? A- - Coronary sinus= 25% - Infrarenal IVC=60% - Renal vein= 80% - Suprahepatic IVC= 70% Q-What is the normal PVR/ SVR? A-= 2/10
- 9. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 9 Q-What is the definition of low CoP? A-Post operatively, for convalescence, CoP required is: - On POD1= 2 lit/min/m2 - On POD2= 2.5 lit/ min/m2 If CoP < 1.5 lit/min/m2 then the incidence of death is high A mixed venous PO2 < 30 mm Hg is s/o low CoP & a mixed venous PO2 < 23 mm Hg indicates a severe reduction of CoP. Q-What is the relation of fever & metabolism? A-For every 1C increase in temperature: a) Metabolic rate increases by 12% b) HR increases by 15 beats/ min c) Insensible waterloss 300- 500 ml/m2/day
- 10. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 10 PROFORMA FOR HISTORY TAKING IN A LONG CARDIAC CASE THE BASIC OUTLINE 1) Personal particulars: Name, age, sex, occupation, religion & residence. 2) Chief complaints: Dyspnea, Palpitations, Cough with/ without expectoration, Hemoptysis, Chest pain, Syncopal attacks. 3) ODP of each 4) H/o CCF 5) H/o Thromboembolic episode 6) H/o Infective endocarditis, 7) H/o cyanosis/ cyanotic spells/ squatting episodes 8) H/o Rheumatic fever 9) H/o Pressure symptoms- hoarseness of voice, dysphagia 10) Treatment history 11) Personal history 12) Family history.
- 11. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 11 NAME For: 1) For establishing a rapport with the patient 2) May give an idea about the religion/ race AGE For: 1) Will give an idea about the illness & also helps in ruling out certain illnesses. Eg: a. Syphilitic AR- Incubation period is ≈ 9 years. Thus considering an infection at 11-12 years of age, the patient has to be a minimum of 20 years of age for a diagnosis of syphilitic heart disease. b. RHD with valvular lesions is extremely rare before 5 years of age (Infact the earliest RHD-MS requiring surgery was reported by Stanley John as 6 years in are view of 3724 pts undergoing CMC-in Circulation 1983 and also the earliest RHD-MR requiring surgery was reported at 4 years by Alain Carpentier in a review of 951 patients for reconstruction-in Circulation 2001.) c. A bicuspid AV degeneration is seen after the 3rd decade of life. 2) A decision about the prosthesis to be implanted depending upon the age. 3) In congenital heart disease, to get an idea about: - Cyanosis, in a child, presenting at birth - CCF present in a child (Eg. A newborn or infant with CCF will suggest a large shunt) SEX For: 1) Certain ailments are more common in certain sexes. Eg: a. Males have a higher incidence of: - Hypetrophic subaortic stenosis - Congenital valvar AS - d TGA - Coarctation aorta b. Females have a higher incidence of: - Osteum secundum ASD - PDA - Isolated MS - Isolated MR 2) If the patient is a female of childbearing age, the advice of surgery (of any kind) & also the type of surgery (type of valve) will vary.
- 12. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 12 OCCUPATION For: 1) Respiratory ailments. 2) Sedentary lifestyle- higher chances of coronary artery disease. RELIGION For: If a bioprosthetic valve is being planned then - In a Muslim- a porcine valve may not be preffered, & - In a Hindu- a bovine valve may not be preffered. RESIDENCE For: 1) Higher attitude patients have a higher tendency for Secundum ASD’s & also earlier development of PH in the same. 2) Higher attitude patients have a higher tendency for PDA 3) People from tropical areas (Eg: Kerala) have a higher incidence of endomyocardial fibrosis. 4) Aortoarteritis is more common in south India 5) Hydatid cyst is commoner in Punjab & Madurai. DYSPNEA Definition: Abnormally uncomfortable awareness of ones own breathing. Divided into 4 grades, similar to NYHA classification. NYHA classification: The New York Heart Association: has 4 components, viz; Dyspnea, palpitations, fatigue & angina. Presently followed is the 7th edition of NYHA (laid down in 1994.) NYHA I: In a patient with heart disease with no limitation of physical activity. Ordinary physical activity does not cause dyspnea, palpitations, fatigue or angina. NYHA II: In a patient with heart disease with mild limitation of physical activity. Comfortable at rest but ordinary physical activity causes dyspnea, palpitations, fatigue or angina. NYHA III: In a patient with heart disease with moderate limitation of physical activity. Comfortable at rest but less than ordinary physical activity causes dyspnea, palpitations, fatigue or angina. NYHA IV: In a patient with heart disease with marked limitation of physical activity. Symptoms are present at rest & increase on exertion. [Note:PND is not included in the NYHA classification.]
- 13. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 13 Q-Is there any classification besides NYHA? A-The following are the classification systems: 1- Canadian cardiovascular society classification CSS - only angina (of) 2- Specific activity scale (of Goldman)- most specific- calculation of metabolic equivalents (1 MET= 2.5 ml/ Kg/ min) Dyspnea is cardinal manifestation of LV failure. The increase in severity is in the following order: Dyspnea on exertion → PND → Orthopnoea → Dyspnea at rest → pulmonary edema. Orthopnoea: In the recumbent position there is decreased pooling in the lower limbs & abdomen → blood is displaced from extrathoracic compartment to thoracic compartment → Failure of LV to pump blood → Increased pulmonary venous congestion & capillary pressure → Interstitial edema → leading too: 1) Decrease in lung compliance + 2) Increase in airway pressure + 3) Ventilation perfusion mismatch. → all leading to dyspnea. It occurs rapidly, within1-2 minutes of lying down & is relieved on sitting. Cough accompanies due to increased pulmonary congestion. A non-productive cough present in CCF is considered as “ dyspnea equivalent” and in recumbency is considered as “ Orthopnea equivalent” Trepopnea: Orthopnea limited to one lateral position. ? due to distortion of great vessels. Platypnea: Dyspnea relieved on lying down. Reasons are not known. Paroxysmal nocturnal dyspnea: The patient awakes suddenly with a feeling of severe anxiety & breathlessness. Associated bronchospasm (due to edema of bronchial mucosa) may be present. [Note:Also called as cardiac asthma due to associated wheeze.] It receives a longer time to get relieved. Reasons for PND are: 1) Slow absorption of extracellular fluid from the dependent areas & resultant increase in blood volume 2) Elevation of diaphragm 3) Decrease LV adrenergic support during sleep 4) Depression of respiratory center during sleep 5) Transient nocturnal arrhythmias.
- 14. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 14 Q-What are the reasons for dyspnea in CCF/ LVF? A- 1) Pulmonary function depressed → increased interstitial fluid → decreased lung compliance → increase airway pressure. 2) Respiratory muscle dysfunction. COUGH For: 1) Feature of LVF- considered as dyspnea equivalent. 2) Impending pulmonary edema 3) Chronic bronchitis 4) Brassy cough relieved on bending forward- arch aneurysm 1), 2) & 4) are posture related. HEMOPTYSIS Definition: Expectoration of blood. Ranges from streaky blood stained sputum to gross hemoptysis. Types: True- tracheobronchial & alveolar False- oral/ nasopharyngeal Q-What are the causes of hemoptysis in a patient with MS? A-Causes of hemoptysis in a patient with MS/ LVF (Paul Wood, 1954) are: 1) Pulmonary apoplexy/ sudden hemorrhage- profuse, rarely life threatening, due to rupture of dilated thin walled bronchial veins caused by acute rise in left atrial pressure. (This is not seen generally due to chronicity which causes the vein walls to become thick)- stops on its own. 2) Blood stained sputum associated with PND. 3) Pink frothy sputum seen in pulmonary edema due to rupture of alveolar capillaries. 4) Pulmonary infarction- due to PA embolism. 5) Following chronic bronchitis due to edematous bronchial mucosa. CHEST PAIN Chest pain may divided into 3 categories- - Ischemic cardiac - Non ischemic cardiac - Non cardiac
- 15. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 15 Ischemic cardiac: 1) Coronary artery disease (decrease supply) 2) LVH/ RVH (increase demand) Non ischemic cardiac: 1) Pericarditis 2) Dilatation of the PA 3) Dissection of aorta Non cardiac: 1) Pulmonary embolism 2) Pleural 3) Esophageal 4) Skeletal PALPITATIONS Definition: Awareness of beating of ones own heart. Occurs due to following cardiac physiological alterations: 1) Change in heart rate 2) Change in rhythm & 3) Augmentation of contractility Other causes of palpitations are: -Thyrotoxicosis -Hypoglycemia -Fever -Drugs Q-What are causes of palpitations in the first decade of life? A-Possible causes are: 1) RHD with vale affection 2) Ebsteins 3) C-TGA SYNCOPE Definition: An association of: - Generalized weakness of muscles with a loss of postural tone - Inability to stand upright & - A loss of consciousness. Q-What are the causes of syncope in a cardiac patient? A-Cardiac causes of syncope maybe due to:
- 16. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 16 1) Decreased cardiac output: - LVOT obstruction- AS, hypertrophic subaortic stenosis - Obstruction to pulmonary blood flow- severe PS/ pulmonary atresia, cyanotic spell, pulmonary embolism - Myocardial- massive MI - Pericardial- tamponade 2) Arrhythmias: - Bradyarrhythmias - Tachyarrhythmias 3) CNS- embolism/ hypoperfusion - LA thrombus, arch aorta aneurysm with thrombus - LA myxomas - Vegetations - Others- carotid artery stenosis, vasovagal, rupture of IC aneurysm due to hypertension. H/O CONGESTIVE CARDIAC FAILURE Ask history in form of: - Edema feet & puffiness of face - Distension of abdomen - Pain in the right upper abdomen - Anorexia, nausea & vomiting - Chest pain (15% of cases of CCF) due to RVH - Oliguria & nocturia (due to fluid retention with redistribution at night) Q-Who proposed the forward & backward failure theory of CCF? A- Backward theory- James Hope (1832) Forward theory- Mackenzie (1913) H/O THROMBOEMBOLIC EPISODES Ask for affection of the following organs: 1) CNS- loss of consciousness - Transient (TIA) - Prolonged with neurological deficit - Convulsions 2) Other organs: - Hematuria - Abdominal pain - Limb pain - Coronary pain
- 17. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 17 Q-What are the ‘intracardiac’ causes of systemic embolization? A-Intracardiac source of embolus may be in from of: 1) Thrombus 2) Vegetations 3) Myxomas 4) Paradoxical embolism 5) Plaques (rarely) Q-Are a particular subset of patient more prone embolization? A-Yes. Tendency for embolization is directly related to: - Age - Size of LAA - Atrial fibrillation Tendency for embolization is inversely related to: - Cardiac output. Q-Discuss the characteristics of thromboembolism secondary to intracardiac clots. A-It is usually the fresh clot that embolize (only a minority of patients with h/o recent TEE have clots found in the LAA). 50% of TEE are cerebral & is recurrent/ multiple in 25% of above. Q-Which is the commonest cyanotic congenital heart diseases to produce CNS complications? A- 1) Tricuspid atresia- 35% incidence beyond the age of 3- 4 years) 2) TOF H/O INFECTIVE ENDOCARDITIS Definition: A microbial infection of the endocardium. 1st stage in the formation of non thrombotic bacterial endocarditis (NBTE), which gets infected later. NBTE form over areas of: - Endocardial injury - Turbulence Areas of affection: - Tends to occur in high-pressure areas; thus more on the left side. - Areas where the blood flows thru’ a narrow orifice; from high to low pressure. Eg. distal to a coarctation, in VSD on the RV side, for PDA on the PA side. Q-In which condition is endocarditis rare? A-Endocarditis is rare in low flow states, eg., ASD.
- 18. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 18 Q-Discuss clinical features of IE. A-The clinical features of IE are due to: 1) Constitutional features of infection, 2) Local destruction 3) Embolization of vegetation leading to - Infarction - Infection 4) Other area of infection due to persistent bacteremia 5) Immune reactions. Thus the symptoms of IE are: - Onset after ≈ 2 weeks of precipitating event - gradual onset with mild fever & malaise if the organism is of low virulence (streptococcus) or acute onset with high fever if the organism is of high pathogenecity ( staph) - Fever- low or high, is present in all patients with IE. (*except in elderly, congenital heart disease, fungal IE) - Fever is generally low grade (< 39.4°C) - Arthralgia & arthritis - Symptoms of embolization are: - Hematuria - Hematemesis - Limb ischemia. - Worsening of symptoms/ CCF- due to leaflet destruction Q-What are the signs of IE? A-The signs of IE are: - Constitutional- fever - Local destruction resulting in – - new murmur - change in preexisting murmur - CCF -Splenomegaly & petechia ≈ 30% of patients with long duration. Petechia are usually seen on conjunctiva, palate, buccal mucosa, upper extremity. -Roth spots- over retinal hemorrhages with clear center. -Osler nodes- tender nodules on fingers/ toe pads- believed to be due to deposition of immune complexes -Janeway lesions- seen in acute endocarditis- are small hemorrhages with nodular charater seen on palm & soles. -Clubbing- long standing disease. -Embolization- especially pulmonary emboli are seen in IV drug abusers with Rt. sided IE & in also from Lt. sided IE with a Lt.→ Rt. shunt. -Mycotic aneurysm -CNS manifestation- due to embolization & cerebral abscess -Glomerulonephritis- due to immune complexes & embolization
- 19. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 19 Q-What are characteristics of endocarditis? A-Endocarditis occurs more frequently in regurgitant lesions than stenotic lesions & is characteristically on the atrial surface of MV & ventricular surface of AV. Q-What is D/D of IE? A- - Acute rheumatic fever - Myxomas Q-What are the procedures, that do not require antibiotic prophylaxis, in a patient with prosthetic valves? A-They are: - Dental picking - Upper GI scopy - Primary bronchoscopy - Clean surgery- Eg. Elective cesarean section - Shedding of primary tooth - IUCD insertion Q-Discuss antibiotic prophylaxis for various invasive procedures. A- For oral/ dental/ upper GI procedures: Regimen I: 3 gm Amoxycillin prior & 1.5 gm Amoxycillin 6 hours post procedure Regimen II: 1 gm Erythromicin prior & 500 mg E’mycin 6 hours post procedure For lower GI/ GUT procedures: Regimen I: IV Amoxycillin (3 gm) + IV Genta (1.5 mg/Kg) ½ hour prior to the procedure & 1.5 gm Amoxycillin 6 hours post procedure. Regimen II: IV Vancomycin (1 gm) + IV Genta (1.5 mg/Kg) ½ hour prior to the procedure. Q-No IE prophylaxis is required in which cardiac lesions? A- 1) ASD- unoperated or operated 2) MV prolapse 3) Coronary artery disease/ post CABG Q-Classify postoperative IE? A-IE can be classified as: Early < 60 days postoperative Late > 60 days postoperative Early is due to intraoperative or immediate postoperative contamination. Mechanical > Bioprosthetic > Homograft IE is more in the early period However in the late period, IE is equal in all the kinds of valves.
- 20. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 20 Q-Discuss the treatment of IE. A- Streptococcal: Penicillin G 6 lac units 6 hourly- 4 weeks +/- Gentaminicn 1.5 mg/ Kg/day Staphylococcal: Vancomycin 15 mg/Kg/dose 12 hrly- 4 weeks +/- Gentaminicn 1.5 mg/ Kg/day Q-What are reason for postponing cardiac surgery in patient’s with IE who otherwise require surgery for endocarditis? A- 1) CNS- acute hemorrhagic stroke (< 10 days) 2) Renal- Acute glomerulonephritis leading to renal failure. 3) Thrombocytopenia H/O CYANOSIS & CYANOTIC SPELLS Definition: Bluish discoloration of nails, skins & mucus membranes due to an increase in the amount of reduced hemoglobin (< 5 gm%) in the capillary blood. Types: - central - peripheral - abnormal pigments -mixed -differential Pathophysiology: When the amount of reduced Hb is > 5 gm% the blood appears dark, giving the tissues a bluish hue. This is seen earliest in the warm areas (areas with increased capillary circulation.) Q-What is the etiology of peripheral cyanosis? A-Peripheral cyanosis is due to slowing of blood; hence causing increased tissue O2 extraction. This is visible over the nose tip, ear lobule & tips of fingers. Q-What are the causes of central cyanosis? A-Causes of central cyanosis are: 1) Cardiac- a. Congenital cyanotic b. Eisenmengerization c. CCF 2) Pulmonary- a. COPD b. Bronchiectasis c. Massive collapse & fibrosis 3) High altitude
- 21. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 21 Q-What are the causes of peripheral cyanosis? A-Causes of peripheral cyanosis are: 1) Cold/ vasoconstriction 2) Shock 3) Increased viscosity of blood Q-What are the causes for mixed cyanosis? A-Causes are- 1) Acute LVF 2) Severe MS (incipient pulmonary edema & vasoconstriction) Q-What are the abnormal pigments that can produce cyanosis like picture? A-They are: Methhemoglobin, sulphhemoglobin etc. Q-Discuss ‘differential cyanosis’? A-It is seen in- 1) Only of lower limbs with/ without left upper limb in - PDA with PH with Rt. To Lt. Shunt. With preductal coarctation - Severe coarctation 2) Only upper limbs in - PDA with PH with rt. to lt. Shunt along with TGA - Coarctation with TGA Q-What is the D/D between central cyanosis & peripheral cyanosis? A-In central cyanosis there is: 1) Good peripheral warmth 2) Clubbing Q-Which are the conditions were cyanosis cannot occur? A-Cyanosis cannot occur in: 1) Severe anemia (Hb< 5 gm%), 2) Carbon monoxide poisoning [Note:In Indians cyanosis is apparent when the O% is < 85%. When < 65%, intense cyanosis.] Q-In which conditions a patient may appear blue but there is no cyanosis? A-The conditions are: 1) Sulphhemoglobinemia/ methhemoglobinemia 2) Silver poisoning 3) Aniline dye workers 4) Extreme cold environment
- 22. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 22 Q-Which conditions can mask cyanosis? A- 1) Anemia 2) Dark complexion. CYANOTIC SPELLS Synonym: Hypoxic spell/ paroxysmal hyperapnea Q-Define cyanotic spell? A-A typical spell is characterized by a progressive increase in rate & depth of respiration & culminates in paroxysmal hyperapnea, deepening of cyanosis, limpness, syncope & occasionally convulsions or death. Q-What does the EEG during a spell reveal? A-EEG during a spell is similar to that of an acute hypoxic episode. Q-Does the incidence of cyanotic spell vary with age? A-The incidence of cyanotic spells increases after 2-6 months of age due to: 1) Replacement of fetal Hb by adult Hb 2) More activity of child 3) Closure of PDA & decreases after 2 years of age due to: 1) The os infundibulum getting fixed (fibrotic changes in the infundibulum) 2) Child has learned as to how to avoid a spell 3) Collaterals grow 4) Improved Hb Q-Which conditions are associated with cyanotic spell? A-Cyanotic spells are seen in: -Tetrology of Fallot - DORV, VSD, PS - VSD, PS - TGA, VSD, PS - ASD, PS - TA Ib/IIb Q-What are the triggering factors for cyanotic spells? A-The triggering factors for a cyanotic spell are: 1) Spontaneous 2) Crying 3) Feeding 4) Bowel movements *particularly seen if stress occurs immediately after an infant has waken up from a long deep sleep.
- 23. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 23 Q-What are the various theories of cyanotic spell? A-The theories of spell are: 1) Proposed by Guntheroth & Morgan: presence of a vulnerable respiratory control mechanism, which is especially sensitive after a prolonged sleep. It reacts to a sudden increase in cardiac output (occurring due to waking up from sleep) Increased venous return Increased Rt. To Lt. Shunt Fall in PO2 and rise in PCO2 Hyperapnea Increased CoP A vicious cycle sets in with the increased CoP leading to increased venous return. 2) Proposed by Wood: There is infundibular spasm due to increased sympathetic activity (this theory does not explain the spells in pulmonary atresia) 3) Proposed by Young: Atrial tachycardia leading to increased right to left shunt. 4) Decreased RV diastolic filling due to dehydration. Q-Describe the treatment of spell. A-The treatment consists of: O2 + Knee chest position + Morphine/ buprenorphine (0.1 mg/ Kg, max up to 0.2 mg/ Kg, not to be repeated within 4 hrs) + NaHCO3- 1-2 meq/Kg/ dose IV Propranolol 0.05- 0.1 mg/ Kg/ dose, slow IV +/ - IV Phenylephrine 1-3 ug/ Kg infusion Ketamine –2 to 10 mg/ Kg & Intubation BT shunt Other options available are: - If duct dependent- PGE1/ duct stenting - If TGA- BAS Q-Is the mortality of emergency BTS higher than that for elective shunt? A-Yes, the mortality for an emergency BT shunt is much higher than for an elective shunt (15% vs. 1%)
- 24. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 24 Q-Describe the prevention of cyanotic spells. A-The following will help in preventing repeated spells: 1) Avoid precipitating cause- eg. Vasodilators 2) Iron supplements 3) Treat RTI promptly 4) Blood letting 5) Optimization of propranolol therapy 6) Plan surgical management Q-Which drugs worsen cyanosis? A-The following worsen cyanosis: 1) Digoxin 2) Vasodilators SQUATTING EPISODES Q-Discuss ‘squatting episodes’? A-History of squatting, for relief of symptoms, is hallmark of Tetrology of Fallot. Squatting helps by: 1) Increasing the SVR by kinking the femoral arteries decreasing the rt. to lt. Shunt. 2) Decreased return of a more deoxygenated blood to the heart from the lower limbs, by kinking the femoral veins. 3) Pushing relatively ‘more oxygenated’ venous blood from the abdominal viscera to the heart, 4) Relaxation of sympathetic overdrive by resting. Q-What are the various ‘squatting equivalents’? A-They are the following: 3 were described by Taussig in 1947: 1) Knee chest position while sitting on the ground 2) Legs folded underneath the body (like a ‘namaz’ position) 3) Lying down. 2 more added, to the list, by Lurie in 1953: 4) Standing with legs crossed 5) Parent holding the baby against owns abdomen with the babies LL flexed. Q-What are the types of squatters? A-There are 2 types of squatters: Rapid- mainly adult, & Slow
- 25. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 25 H/O RHEUMATIC FEVER -Ask for h/o sore throat followed by fleeting arthritis. Definition: It is an acute non-suppurative immune mediated inflammatory disease, usually in children, that follows a few weeks after an attack of pharyngitis; caused by group A hemolytic streptococci. Q-What are the reasons for increased prevalence in developing nations? A-The exact reasons are not known. It is believed to be due to: - Increased urbanization (due to increased droplet infection), - Overcrowding ( ” ). [Note:There is no proof to suggest that nutritional factor has a role in RF.] Q-Discuss the etiopathogenesis of RF. A-The causative agent is group A hemolytic streptococci however in 1/3rd of the patients there is no h/o sore throat nor blood culture yield e/o streptococcal infection. Pathogenesis is not known & is believed to be an immune reaction to bacterial allergy or an autoimmunity. Q-Describe Aschoff bodies. A-Aschoff bodies have the following features: - May be seen if there is cardiac involvement secondary to RF - Seen in the myocardium & endocardium (rarely over the valves) - Most frequently seen in the; IVS & posterior surface of LV/ LA. - They are discrete lesions, < 1mm diameter, formed by a collection of round cells, fibroblasts & MN giant cells, surrounded by a zone of PMN cells & lymphocytes. - Particularly situated around small blood vessels. Q-What are the clinical features of RF? A-The clinical features of rheumatic fever are: - symptoms begin usually 2-3 weeks after an episode of acute pharyngitis. -fever (is always present, except in chorea) -fever lasts for 2-3 weeks. -Other features that may follow are: 1) Arthritis: It is a fleeting arthritis affecting large joints with no residual deficit. Generally affected joints are: - Knee - Ankle - Elbow - Wrist Each joint remains inflamed for 1-7 days & complete episode lasts for 3 weeks.
- 26. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 26 Q-RF can affect which other joint? A-RF can rarely affect the following joints: - Shoulder - Hip - Small joints. *Rarely a deformity may be left behind- Jaccoud’s arthritis. 2) Subcutaneous nodules: (These are considered pathognomic of rheumatic fever.) They are: - Less than 2 cm diameter - Freely mobile overlying skin - Site: Over bony prominences especially skull, galae aponeurotica. For examining for these nodules, ask the patient to squat & keep the elbows on the knees & wrists folded beneath the chin. Now palpate the shin, extensor aspect of elbow, occiput & mid back, i.e., over & around the spine & scapula. 3) Erythema marginatum: These are: - rapidly evolving small macules papules large circles with raised & well defined edges which blanch on pressure. - Disappear within few hours. - Site; trunk, limbs. Very rare on the face. 4) Chorea (St. Vitus dance): These are: - Characterized by involuntary, non repetitive, jerky movements which decrease during sleep and increase with anxiety. - In children any gender, but post puberty mainly in girls, - The patient becomes irritable & produces jerky movements, grimacing involuntarily & has slurred speech. - Generally seen along with carditis or nodules. Q-How can rheumatic chorea be diagnosed clinically? A-When the child is asked to extend the arms there is a tendency to flexion at the wrist & hyperextension of the fingers. Q-Who was St. Vitus? A-St. Vitus was a roman catholic priest who patronized epileptics & actors. 5) Carditis: It is essentially a pancarditis. 50% of cases of rheumatic fever have carditis. Endocarditis- ¾ th of patients developing carditis have a new murmur, which may be - Apical pan systolic murmur; due to myocarditis (the commonest murmur) - Apical mid diastolic murmur, Carrey Coombs murmur, - PA systolic murmur, due to fever, anemia.
- 27. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 27 Myocarditis- - Important feature of myocarditis is progressive dilatation of LA & LV. Pericarditis- 2 types - Acute fibrinous - Effusion (pericarditis is associated with severe forms of carditis.) Q-What is the incidence of CCF in patients with rheumatic carditis? A-CCF occurs in 10% of patients with rheumatic carditis. [Note:Prolongation of PR interval is temporary but may persist for months (reason is not known)] [Note:Rheumatic fever may lick the joints but certainly bites the heart.] [Note:Rheumatic fever mainly affects the left side of the heart (reason unknown)] Q-Discuss Jones criteria. A- Original criteria were described by T. Duckett Jones in 1944. Currently the 4th edition (updated in 1992) of Jones criteria is accepted. The criteria is as follows: Major Minor Carditis Clinical- - Fever - Arthralgia - H/o rheumatic fever/RHD Polyarthritis Investigations- - Presence of acute phase reactants (CRP, ESR, leucocytosis) - PR interval prolongation Subcutaneous nodules Erythema marginatum Chorea + E/o of streptococcal infection, in form of - ASLO +ve, or - + ve throat culture, or - h/o scarlet fever. The diagnosis of rheumatic fever, by modified Jones criteria, is by - 2 major criteria + e/o streptococcal infection, or - 1 major & 2 minor criteria + e/o streptococcal infection. If there is no supporting e/o streptococcal infection then a diagnosis of rheumatic fever should not be accepted, except in 2 conditions: - only signs of chorea, or - only signs of carditis.
- 28. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 28 (This is because the infection may have occurred few months back & hence the antibody titres may have returned too normal.) [Note:In India polyarthralgia is included as major criteria (in 1994 by Padmavati & Khanna)] Q-What is average duration of rheumatic fever? A-The average duration of an attack of rheumatic fever is 3 months. In cases of carditis, it may continue for nearly 6 months. Q-Discuss ASLO. A-Described by Todd in 1932. Normal levels are upto 333 Todd units- in children & Upto 250 Todd units in adults. Most specific test for rheumatic fever is AntiDNAase antibody levels. Normal levels are upto 240 Todd units- in children & Upto 120 Todd units in adults. Q-What is the D/D of streptococcal pharyngitis? A- - viral: characterized by more malaise & rhinitis. - Other bacterial. Q-What is the risk of recurrence of RF? A-Risk of recurrence of rheumatic fever is 65% & subsequently the risk decreases with time. Q-What are the WHO recommendations for rheumatic fever? A-The WHO recommendations are to treat all sore throat as due to group A hemolytic streptococci unless proved otherwise. The prophylaxis is: Single injection of 12 lac units Benzathine penicillin (if wt. > 27 Kg) & Single injection of 6 lac units Benzathine penicillin (if wt. < 27 Kg) Or Oral Erythromycin 20 mg/Kg/day for 10 days. Q-Discuss the treatment of rheumatic fever. A-Treatment of rheumatic carditis is 3 fold: 1) Treatment of CCF- bed rest, salt restriction, digoxin, diuretics 2) Treatment of Carditis- Aspirin- 100 mg/kg/day in 8-10 divided doses for 1 month if symptoms persist after few days of starting aspirin add Prednisolone 1-2 mg/ Kg/ day & reduce aspirin. 3) Treatment of rheumatic fever. Q-What is the incidence of valvular affection of RHD? A-The incidence of valvular affection of RHD: MV- 70-80%, MV + AV- 20- 25%, Only AV- 5- 8%, TV- 30- 50% (autopsy)
- 29. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 29 Q-Which places in India have a high prevalence of RHD? A-The areas are: - Kutch - Dhulia Q-What are the first auscultatory manifestation of carditis in rheumatic fever? A-They are: 1) Pansystolic murmur of MR (between Grade 2-4) Occasionally 2) Carrey Coombs murmur & 3) Flow murmur across the PV PRESSURE SYMPTOMS These are - Hoarseness of voice & - Dysphagia Q-What is hoarseness of voice, secondary to cardiac cause, termed as? A-Otner’s syndrome. Q-What are the causes of hoarseness of voice in a cardiac case? A-Reason for hoarseness are: Due to compression on the left recurrent laryngeal nerve by - Dilated LA - Tracheobronchial LN - Enlarged PA - Arch aorta or proximal descending thoracic aortic aneurysm - Aneurysm of ductal ampulla Q-Enumerate the cardiac related reasons for dysphagia? A-Due to pressure on esophagus by: - Arch/ descending thoracic aortic aneurysm - Aberrant Rt. Subclavian artery- dysphagia lusoria - LA enlargement - Rt. Aortic arch TREATMENT HISTORY Ask for - Drugs taken - Since when - Any surgical procedure advised or performed.
- 30. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 30 MEDICAL ILLNESS IN PAST Ask for - Diabetes- important for CAD, post operative wound healing - Hypertension - Tuberculosis- ask for presence of low grade fever with/ without rigors in evening, anorexia, weight loss, hemoptysis, scars or sinuses. - Syphilis - Bleeding disorder- for intra op & post op anticoagulation - Hematemesis/ malena- for intra op & post op anticoagulation - Maternal diabetes- higher incidence of child having TGA, VSD - Maternal SLE- higher incidence of child having congenital complete heart block - Drugs taken & illness during pregnancy (see below). Q-What is the importance of maternal illness & treatment history during gestation? A- Significant illness during pregnancy: Rubella can cause congenital rubella syndrome Importance of drugs during pregnancy: Drug Fetal cardiac anomaly Associated defects Alcohol VSD Growth & mental retardation, microcephaly Phenytoin PS, AS, coarctation, PDA Hypertelorism, growth & mental retardation Lithium Ebsteins, Tricuspid atresia Thalidomide# Tetrology of Fallot/ Truncus Phacomelia Warfarin PS, PDA Teratogenic #Thalidomide has been reintroduced for the treatment of – erhythema nodosum leprosum, multiple myeloma. Q-What are the teratogenic effects of warfarin? A-They are: 1st trimester- affects cartilage development, additional CVS malformations (PDA, PS) 2nd trimester- still born, spontaneous abortion, CNS abnormality (? Due to IC bleed). PERSONAL HISTORY Ask for history of paan consumption as; - paan contains betel nut which is rich in aracholine, which in turn may lead to bronchospasm.
- 31. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 31 FAMILY HISTORY Significance of family history is for - Coronary artery disease - Congenital heart disease, - Consanguineous marriage, - Age of the parent; at time of birth of child (patient). Q-Discuss the importance of family history for congenital heart disease? A-(From an article by Nora & Nora, Circulation 1978) The % risk of an offspring having a CHD if the parent has the disease: Disease % in offspring if father is % in offspring if mother is affected affected Congenital AS 3% 13% ASD 1.5% 4.5% AV canal 1% 14% Tetrology of Fallot 1.5% 2.5% VSD 2% 10% PDA 2.5% 4% The % of risk of a baby being affected if a sibling is affected: Disease % in 1st sibling % in 2nd sibling ASD 3% 8% Tetrology of Fallot 3% 8% VSD 3% 10% PDA 3% 10% [Note:If a parent & sibling, both are involved then the risk of another sibling having the heart disease is very high.] Q-What is the importance of consanguineous marriage? A-The importance lies for autosomal dominant & recessive conditions. For autosomal dominant conditions like: - Holt Oram syndrome - Noonans syndrome - Williams syndrome - Marfans syndrome. For autosomal recessive conditions like: - Ellis Van Creveld syndrome, - Kartegners syndrome Q-What is the significance of age of parents? A-The significance of age is as follows: - Increased paternal age: Higher incidence of Noonan’s - Increased maternal age: Higher incidence of Down’s syndrome
- 32. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 32 PROFORMA OF GENERAL EXAMINATION 1) Built & nutrition 2) Temperature 3) Pulse- site, rate, rhythm, character, character, radio radial delay, radio femoral delay, apex pulse deficit, condition of vessel wall, peripheral pulsations. 4) Respiration 5) Blood pressure- site & body decubitus, 6) JVP 7) Pallor 8) Icterus 9) Clubbing 10) Cyanosis 11) Signs of CCF 12) Peripheral signs of wide pulse pressure 13) Signs of Marfans 14) Signs of tuberculosis 15) Facial/ skeletal abnormality.
- 33. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 33 BUILT AND NUTRITION Describe that- - The patient is comfortably sitting in bed, - The built of patient (optional) Q-What are the postures, of significance, in a cardiovascular case? A- - Leg hanging down- in PVD, - Squatting Q-What are types of built? A-Types of built are: - Ectomorphic- light bones, small stature, - Endomorphic- stocky, increased soft tissue, - Mesomorphic- between the two. Q-What are the parameters of ‘nutrition’ A-They are: - age dependent- weight, height - age independent- arm circumference Q-How is the estimated weight & height of child for an age calculated? A-The following formula may be followed for weight: At birth= 2.5- 3.5 kg A-Age in years 3- 12 months- (A + 9)/ 2 1- 6 years- 2A + 8 7- 12 years- (7A- 5)/ 2 Height chart- estimated height of child for the age is as follows; At birth- 50cm, At 1 year= 75 cm At 2 years= 85 cm 1-12 years= (Age x 6) + 77 cm Q-How is the arm circumference measured? A-Using Shakirs tapes for that age- there are 3 zones comprising of red, orange & green. Q-Define ‘low birth weight’? A-Weight < 2.5 Kg is considered low birth weight. (In India, 30-35% of newborn are low birth weight) Q-What is very low birth weight? A-Weight of <1.5 kg is considered very low birth weight.
- 34. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 34 Q-Discuss normal ‘milestones’. A-Normal developmental milestones are (in general & in brief): 1 mnth- when made of sit with support cannot hold head, but recognizes faces & smiles 4 mnths- can sit with support & hold head 8 mnths- can sit on own hands in front. 10 mnths- sit up on own with hands folded & can say monosyllables (mama/ dada) 12 mnths- stands & takes steps with support 18 mnths- walk on own 2 years- runs & talk toilet 3 years- climb stairs up- one stair with the same foot 4 years- climb stairs down- one stair with the same foot 5 years- can stand on 1 leg, dresses & undresses 6 years- stands on one leg with eyes closed. Counts till 20- 30. Q-What are the congenital disorders which are associated with cardiac pathologies & additional systemic manifestations (that might be evident on clinical examination)? A-They are: a) Muscoloskeletal Disorder Cardiac defect Other abnormality Holt Oram syndrome ASD Hypoplastic thumb & radius Ellis Van Creveld syn ASD Dwarfism & polydactly Noonans PV dysplasia Web neck, pectus excavatum Kartegners Dextrocardia Sinusitis, bronchiectasis b) Connective tissue Disorder Cardiac defect Other abnormality Marfans AR Mentioned later Osteogenesis imperfecta AR Dwarfism & polydactly Ehler Danlos MR Hyperelastic skin Pseudoxanthoma elasticum Arterial wall disease c) Endocrine Disorder Cardiac defect Other abnormality Hypothyroidism CCF, bradycardia Hyperthyroidism Atrial fibrillation Cushings Hypertension Addisons Hypotension Phaeochromocytoma Hypertension
- 35. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 35 d) Metabolic & chromosomal Disorder Cardiac defect Other abnormality Mucopolysaccharoidosis Multivalvar Physical & mental retardation Downs Endocardial cushion defects Turners Coarctation Q-Describe ‘characteristic’ facial abnormalities that maybe seen in a cardiac case? A- Facies Cardiac Disorder - Elfine facies Williams syndrome - Conotruncal facies AV cushion defects-TOF/ TGA/ DORV/ TA - Downs syndrome Endocardial cushion defects - Turners syn (slanting eyes Coarctation micrognathia, web neck) - Di Georges syndrome Truncus (conotruncal facies) - Noonans syn (hypertelorism PV dysplasia low set ears, slanting eyes) Q-What comprises conotruncal facies? A-The following features makeup for conotruncal facies: - low set ears, - slanting eyes, - periorbital edema, - slit mouth PULSE Definition: A wave produced by cardiac systole that advances in the peripheral arterial tree in the peripheral direction. The components of a description of pulse include: 1) Rate: Normal 60 –90 beats/ min *Tachycardia in a.f.- if ventricular rate> 85/ min 2) Rhythm: - Regularly regular- nsr - Irregularly irregular- a.f. - Regularly irregular- Unifocal ectopics
- 36. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 36 3) Volume: High volume in- - AR, MR, PDA, VSD - High output states- fever, anemia, pregnancy, Beri beri, thyrotoxicosis - Increased stroke volume- complete heart block Low volume in- - LVOT obstruction - Myocardial cause - Pericardial Varying volume in: - Pulsus alterans- sinus rhythm of alternating beats of varying volume- seen in LVF 4) Character: Normal pulse has a- anacrotic wave t- tidal wave n- dicrotic notch d- dicrotic wave Q-What are various types of pulses? A- a) Anacrotic pulse- slow rising well sustained- seen in AS b) Dicrotic pulse- 2 beats palpable; the percussion wave & the dicrotic wave- seen in fever, CCF c) Pulsus besferiens- 2 betas palpable in systole, rapidly rising pulse; the anacrotic wave & the tidal wave- seen in AS with AR, idiopathic hypertrophic subaortic stenosis. d) Pulsus parvus et tardus- slow rising & slow falling- seen in AS e) Pulsus alterans- alternate strong & weak pulsations- seen in LVF f) Pulsus bigeminus- regularly irregular with high volume- seen in unifocal ectopics. g) Pulsus paradoxus- Normally the systolic BP falls by 10 mm Hg during inspiration. This phenomenon is seen due to: i. Increased venous return to the right heart & pooling in the PV circulation decreased return to LA/LV decreased CoP. ii. Movement of the IVS to the left due to RV filling decreased LV filling. When the SBP falls more than 10 mm Hg, in inspiration, it is termed as pulsus paradoxus. It is a misnomer, as it is nothing but exaggeration of the normal. (*The paradox is that while the heart sound is heard, the pulse may not be felt) Q-What are causes of pulsus paradoxus? A-Causes are: 1) Cardiac- tamponade, constrictive pericarditis. 2) Pulmonary- Asthma, emphysema 3) SVC obstruction [Note:Reverse pulsus paradoxus- It is seen in patients with CPAP, on ventilator]
- 37. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 37 h) Waterhammer pulse- rapid upstroke & rapid downstroke, characteristic rapidly rising & rapidly falling pulse with high volume. Causes:I) High output states- fever, anemia, pregnancy, Beri beri, thyrotoxicosis II) Cardiac- AR, RSOV, PDA, AP window 5) Radioradial, radiofemoral delay & apex pulse deficit Q-When can radiofemoral delay be appreciated? A-If more than 40 millisec difference is present. Q-What are the reasons of radioradial delay? A-They are: - SVAS, - Coarctation aorta with involvement of SCA or with origin of the right SCA distal to the coarct segment - BT shunt- classic or rarely modified Q-What is the normal time delay between the apex beat & a peripheral pulse? A-The time difference normally between apex beat & a peripheral pulse is: - Carotid artery= 30 millisec - Brachial artery= 60 millisec - Femoral artery= 75 millisec - Radial artery= 80 millisec JUGULAR VENOUS PULSE Q-Why is JVP seen in the internal jugular vein? A-It is easier to recognize pulsations in the EJV than IJV but still the EJV is not used as an indicator of RA pressure due to: 1) Presence of valves in EJV 2) EJV passes thru’ more fascial planes & may be affected by extrinsic compression. 3) IJV is in a straight line with RA. Q-Describe the technique of measurement of JVP? A-Patient is kept in reclining position (at 45) & the neck is supported to relax neck muscles (especially the sternomastoid) normally 5-9 cm of H2O from the mid RA or 0-4 cm from the sternal angle of Louis (center of RA lies ≈ 5 cm below the sternal angle). [Note:In a healthy individual, at an angle of 45, the mean level is invisible. However the a & v waves will be visible just above the clavicle (sternal angle).] Q-How to differentiate JVP with carotid pulse? A-The JVP is characterized by: - postural variation, - decrease in impulses with inspiration & - not palpable impulse/ pulse.
- 38. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 38 Q-Describe the components of normal JVP. A-A normal JVP has: ‘a’ wave: Due to Rt. Atrial contraction. Normally ‘a’ is the largest positive wave. ‘a’ wave absent in- atrial fibrillation. Tall ‘a’waves in- TS, tricuspid atresia, RA myxoma, pulmonary hypertension, PS with intact IVS Cannon ‘a’ waves in- complete heart block, when the RV contacts against a closed TV, ectopic beats. ‘c’ wave: Produced by; 1) impulse of carotid artery on adjacent veins, 2) bulging of the TV into the RA. ‘c’ is not normally seen & it merges with the ‘a’wave to form the and colleagues complex. ‘x’descent: Due to venous filling of the RA during which the RA is relaxed & TV is closed. ‘v’ wave: Due to continuing RA filling against a closed TV. ‘v’waves are prominent in- TR, constrictive pericarditis. ‘y’ descent: Due to the opening of the TV, corresponds to the S3. Rapid y descent is seen in- TR, constrictive pericarditis Slow y descent is seen in- TS Q-How is a raised JVP, secondary to a cardiac cause, differentiated from an elevated JVP due to SVC obstruction? A-The JVP, which is raised in SVC obstruction, will show variation with respiration. Q-What is Kussmauls sign? A-Normally the JVP lowers during inspiration. But in constrictive pericarditis, there is an increase in JVP on inspiration. Q-Discuss Hepatojugular reflex. A-Normally when sustained pressure is applied to the right hypochondrium, initially the JVP rises due to increased hepatic venous return, but rapidly returns to normal. But in overt CCF, continuous sustained pressure (30 sec) will keep the JVP persistently high as the failing heart cannot compensate for the increased venous return. Removal of pressure will lead to an abrupt fall by > 4 cm H2O.
- 39. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 39 BLOOD PRESSURE Q-Describe the ‘cuff’ that is used to measure the BP. A: Name- Riva Rocci cuff Optimum length of cuff- 2/3rd the circumference of the limb wih the center of the cuff overlying the artery Optimum width of cuff- 20% more than the diameter of the limb. Normal width of cuff in adults is 12 cm for upper limb & 15 cm for lower limb (if the width is narrower, a higher pressure will be recorded) Q-How is lower limb BP measured? A-For measurement of lower limb BP the patient lies prone & a 18 cm cuff is applied above the level of the knee. Auscultation is carried out in the popliteal fossa. Q-What are phases of Korotkoffs sound? A-(from Hutchisons manual) There are 5 phases: 1st phase- peak systolic pressure, 2nd & 3rd phase- due to turbulent blood flow thru’ a partially occluded artery. 4th phase- muffling of sound, & is 7-10 mm Hg above the true DBP. 5th phase- absent sound- true DBP. Q-When is Korotkoff’s 4th phase used for measuring DBP? A-In physiological conditions like pregnancy & pathological conditions like AR, PDA and RASOV. Q-What are the values of ‘normal’ BP in children? A-A rough formula is as follows: SBP= 90 + (age in years x 5)/ 2 DBP= 60 ± 20 m Hg [Note:Normally the right UL BP is slightly higher than the left UL.] Q-What conditions are associated with an abnormally high right UL BP? A-The following conditions are associated with a abnormally high right uppel limb BP: 1) Interrupted arch 2) Supravalvar AS 3) Coarctation involving the left SCA. Q-Does gravity affect BP? A-For a distance above or below the level of the heart, subtract or add 0.77 mm Hg/cm. Q-What is Ossler’s sign? A-Ossler’s sign is pseudohypertension that is seen in Moenckbergs degeneration, where the artery is sclerotic. Thus even with a lower systemic BP, the recording obtained is high as the cuff is unable to occlude the artery (as it would normally do on inflation.)
- 40. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 40 CLUBBING Definition: Bulbous enlargement of the soft parts of the terminal phalanges with both horizontal & transverse curving of the nails. Grades: 4 grades: I) Softening of the nail bed II) Obliteration of angle of nail bed III) Increase in the curvature of nail- parrot beak/ drum stick appearance IV) Swelling in all dimensions with X ray e/o subperiosteal new bone formation (hypertrophic pulmonary osteoarthropathy) Q-What are the theories of clubbing? A-There is interstitial edema & dilatation of arterioles & capillaries due to: 1) Serotonin theory- increased fibrous tissue deposition 2) Hypoxia- stimulating opening of AV fistulae to increase blood flow to fingers & toes 3) Reduced Ferritin in venous blood escapes oxygenation in the lung & enters systemic circulation & acts as a stimulant for dilatation of AV anastomosis. 4) Neuronal theory Q-What is Pseudoclubbing? A-In hyperparathyroidism, resorption of bone leads to bulging of fingertips. However the nail curvature is normal. Q-What are the causes of clubbing? A-The causes are: 1) Generalized clubbing: i. Pulmonary- brochiectasis, lung abscess, bronchogenic carcinoma, ii. Cardiac- cyanotic HD, Eisenmengerisation, infective endocarditis iii. Alimentary- ulcerative colitis, crohns disease, cirrhosis iv. Endocrine- myxedema, acromegaly v. Others- idiopathic, hereditary 2) Only UL clubbing- IV drug abusers 3) Only LL clubbing - in farmers who work bare feet. 4) Unilateral limb clubbing - pancoast tumor, subclavian artery aneurysm 5) Unidigital clubbing - gout Q-Which conditions are associated with clubbing but without cyanosis? A-The following: - Infective endocarditis - Non cardiac etiologies
- 41. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 41 Q-What are the objective signs of clubbing? A- 1) Schamroths window- normal diamond shaped space in between two approximated nails. Lost in clubbing. 2) Distal phalyngeal depth > interphalyngeal depth. If more than 1, then clubbing is advanced. 3) Lowibonds angle- acute angle formed by the nail bed. Disappears with clubbing. CYANOSIS Please see history proforma detail of cyanosis (page 19). EDEMA FEET *Location of edema in CCF depends upon the posture of the patient. In patients who are mobile, the edema is checked by pressing against distal anterior tibia & fibula. In patients who are recumbent, edema is checked over the sacrum & dorsal spine. PALLOR Q-Describe clinical estimation of hemoglobin. A-Rough estimate of hemoglobin: Palmar crease pale- Hb < 7 gm% Venous hum- < 5 gm% Functional PS- < 5 gm%. ICTERUS Q-Describe clinical estimation of jaundice. A-A rough estimate of depth of jaundice: Face > 5 gm% total bilirubin Trunk> 10 gm% Lower limbs> 20 gm%.
- 42. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 42 TUBERCULOSIS Q-What are the peripheral signs of TB? A-They are: - lean thin individuals - phlyecten (medial) - saddle nose - scars & sinuses on neck - deformity of chest wall & spine - scrofuloderma - lupus vulgaris - errhythema nodosum - thickened spermatic cord Q-What are the CVS manifestations of TB? A-They maybe in form of: 1) Pericardial effusion 2) Constrictive pericarditis 3) IVS granulomatous lesion 4) Aortoarteritis (of aorta & rarely causing a PA aneurysm- called the Rasmusen’s aneurysm). PERIPHERAL SIGNS OF AR Q-What are the peripheral signs of AR? A-They are: 1) Wide pulse pressure. - mild= 40- 60 mm Hg - moderate= 60- 80 mm Hg - severe= > 80 mm Hg 2) Hills sign- Difference between the systolic BP of LL & UL. - mild AR= 20 –40 mm Hg difference - moderate= 40- 60 mm Hg - severe= > 60 mm Hg Q-What is reason for a Hill’s sign? A-Believed to be due to: a) Impaired reading recording due to excessive muscle bulk of thigh thus requiring higher pressure in the cuff to occlude the artery b) Augmentation of the systolic wavefront by wave amplification, as the it travels into the aorta to the periphery 3) Alfred de Musset sign (He was a poet)- increased pulsations of the head & neck vessels. 4) Lighthouse sign- alternating blanching & perspiration of the forehead, 5) Landolfe’s sign- pupillary dilatation & contraction 6) Becker’s sign- Retinal artery pulsations. 7) Muller’s sign- pulsating uvula
- 43. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 43 8) Corigan’s sign- dancing carotids 9) Quinke’s sign- pulsatile capillary filling of nail bed on application of pressure over the nails. 10) Waterhammer pulse- brisk upstroke, brisk downstroke with high volume, felt even thru’ a less sensitive area like palm. 11) Locomotor brachials. 12) Mayne’s sign- < in DBP by > 15 mm Hg when BP is measured with arm hanging & later with arm raised. 13) Austin Flint murmur- is due to: a. Regurgitant jet hitting AML, b. The coming together of 2 jets, ie, AR jet & The LA to LV jet, to create turbulence, c. Increased LVEDP [Note:Even in severe AR an Austin Flint murmur may not be heard due to calcific AML or an eccentric jet.] 14) Rosenbach sign- liver pulsations, 15) Gerhardt’s sign- splenic pulsations, 16) Duroziez murmur- on ausculatation over femoral artery, with pressure a systiloc murmur heard distally & a diastolic murmur proximally 17) Lincoln sign- toe movements with cardiac contraction, 18) Traube’s sign- pistol shot femorals, 19) Shiley’s sign- Pulsating cervix. MARFAN’S SYNDROME Described in 1896 by Antine Marfan. 65-70% are by genetic transmission (caused due to mutation of the FBN1 gene on chromosome 15.) Q-What are the organ systems affected & diagnosis in Marfans? A-The organ systems affected are CVS, Occular, pulmonary, skeletal & skin. Diagnostic criteria laid down by Ghent: 1) Skeletal: Major- - Pectus escavatum/ carinatum - Upper segment/ lower segment< 0.8 - Arm span/ height > 1.05 - Walker Murdoch sign (wrist sign)- little finger can go across the opposite wrist and touch the thumb - Steinberg sign (thumb sign)- thumb flexed and if it protrudes out of the medial aspect of the hand, sign is +ve - Metacarpal index> 8.4 (radiological length of 2,3,4 & 5 metacarpal added & indexed to the added central diameter of the above metacarpals) - Scoliosis - Angle of elbow> 160º.
- 44. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 44 Minor- - high arched palate- uvula not seen - oblong head, - endopthalmus - down sloping eyes 2 major or 1 major + 2 minor criterion required for the skeletal system to qualify as a +ve system. 2) Occular: Major- - subluxation of lens (mainly upward- characteristic feature of Marfans) Minor- - flat cornea - axial length of globe > 23.5 mm, - hypoplastic iris/ ciliary muscle 1 major or 2 minor criterion required for the occular system to qualify as a +ve system 3) CVS: Major- - dilatation of ascending aorta (> 40 mm) with/ without AR with dilated sinuses of valsalva - dissection of any portion of the aorta Minor - MVP with/ without MR - Dilatation of MPA > 20 mm without peripheral PA stenosis, in age < 40 years. 1 major or 1 minor criterion required for the CVS system to qualify as a +ve system 4) Dura: Major- - lumbosacral dural ectasia Minor- none 1 major criteria required for the dura system to qualify as a +ve system 5) Pulmonary: Minor only- - spontaneous pneumothorax - blebs 6) Cutaneous: Minor only- - stretch marks - spontaneous hernia
- 45. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 45 For the diagnosis of Marfans; 1) Genetic analysis +ve, 1 system +ve & one criteria of any other system, or 2) If genetic analysis not possible, then 2 systems should be +ve & 1 criteria from a 3rd system. Q-At what age are the CVS manifestations of marfans generally seen? A-Around 30 years of age. The other features can manifest at any age. Q-In a patient with Marfans when is replacement of aortic root recommended? A-If root > 40 mm, pregnancy not advised till root replacement. If root > 45 mm, advised root replacement in all. Q-What is the chance of transmission of Marfans to child. A-50%. FACIAL ABNORMALITY Q-Describe characteristic facial abnormality that maybe seen in patients with heart disease? A- - Elfine facies Williams syndrome - Conotruncal facies AV cushion defects-TOF/ TGA/ DORV/ TA - Downs syn Endocardial cushion defects - Turners syn (slanting eyes Coarctation micrognathia, web neck) - Di Georges syn Truncus (conotruncal facies) - Noonans syn (hypertelorism PV dysplasia low set ears, slanting eyes) Q-When is the ear low set? A-When a line is drawn from the outer canthus backwards, and it lies above the upper ear helix.
- 46. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 46 CVS EXAMINATION GENERAL PROFORMA Inspection: 1) Chest- symmetery 2) Precordium 3) Apex impulse 4) Any other pulsations: - parasternal - suprasternal - epigastric - neck - left 2nd ICS 5) Dilated veins 6) Scars & sinuses 7) Traile’s sign Palpation: 1) Apex impulse 2) Diastolic shock 3) Thrill 4) Other pulsations 5) Trailes sign Percussion: 1) Left heart border 2) Right heart border 3) Left 2nd ICS Ausculatation: 1) S1 2) S2 3) S3/ S4 4) Murmurs 5) Other sounds
- 47. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 47 INSPECTION PRECORDIUM: Anterior aspect of the chest wall overlying the heart. Normal precordium is smooth with same contour as the opposite chest wall. Q-What are the causes of bulging precordium? A-Is seen in: - Cardiomegaly - Pericardial effusion - Mediastinal tumor - Pleural effusion - Chest wall deformity Q-What are the causes of retracted precordium? A-Is seen in: - Fibrosis of lung - Congenital chest wall deformity APEX IMPULSE: Lowermost & outermost area of the seen cardiac impulse. Normally is in the left 5th ICS inside the midclavicular line. Q-When is the apex impulse absent/ not seen? A-It may not be seen in presence of: - Pendulous breast - Overlying rib (then turn the patient to left lateral decubitus & examine) - Pleural effusion - Emphysema - Pericardial effusion/ constrictive pericarditis. Q-What is the normal location of the apex impulse in children? A-< 3-4 years of age the apex impulse lies in the left 4th ICS, in the midclavicular line. Q-Which conditions are associated with ‘double apical impulse’? A-Seen in: - LV aneurysm - HOCM - Constrictive pericarditis - Subaortic stenosis Q-When is apical impulse considered diffuse? A-If the impulse is > 1 ICS or > 5 cm diameter.
- 48. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 48 PULSATIONS: A) Juxtaapical- seen in: - Ventricular aneurysm - HOCM - Constrictive pericarditis B) Epigastric- seen in: - RVH - Aneurysm aorta - Hepatic pulsations D/D between the above is by the 3-finger test. C) Left 2nd ICS- seen in: - Dilated PA - Aneurysm aorta - Enlarged LA - L-posed aorta D) Suprasternal- seen in: - Arch aorta aneurysm - AR - Hyperkinetic state E) On right side- seen in - Dextrocardia - Ascending aortic aneurysm F) Back- seen in: - Suzzmans sign for coarctation of aorta G) Right sternoclavicular joint- seen in: - Ascending aortic aneurysm - Right sided aortic arch H) In neck- seen in: - AR - Hyperkinetic state DILATED VEINS OVER THE CHEST WALL: Seen in: - SVC/ IVC obstruction - CCF SCARS: Of previous surgical procedure
- 49. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 49 PALPATION APEX BEAT: It is lowermost & outermost point where the cardiac impulse is felt. It can be: - heaving - hyperdynamic - tapping. Q-Describe the characteristics of apex beat? A-They are: Normal- It is: - localized to I ICS or < 2.5 cm diameter - inside MCL - lasting for < 50% systole - felt as gentle tap Tapping- Seen in RVH, It is: - just a tap, not lifting finger - localized - only in early diastole - no paramedical retraction Hyperdynamic- Seen in LVVO (Eg. AR, PDA, MR), It is: - diffuse, ie, > 2 ICS or > 5 cm diameter or > 2 finger width - ill sustained (< 2/3 rd systole) - outside MCL (generally) - forcible Heaving- Seen in LV pressure overload (Eg. AS), It is: - diffuse, - sustained (> 2/3 rd systole) - forceful PARASTERNAL HEAVE: It is a systolic impulse felt in the left parasternal region due to: - RVH - Rarely due to aneurysmal descending aorta/ enlarged LA Q-Describe grading of parasternal heave. A-There is no grading of parasternal heave described. However a classification that may be followed is: - Grade I- gentle tap to the palpating hand (ulnar surface of hand) - Grade II- lifts the hand but can be pressed by applying force to the hand - Grade III- lifts the hand even on applying pressure Q-What is Herztosis? A-A highly pulsatile precordium is termed as Hertztosis. It is seen in chronic MR or multivalvular regurgitant lesions.
- 50. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 50 TRACHEAL TUG (OLIVER’S SIGN) Technique- Raise the chin of the patient→ apply firm pressure on both the sides of cricoid cartilage with one hand (thumb & index finger) or 2 hands → a downward tug is felt by the fingers with each heart beat. It is seen in- arch aneurysms & mediastinal masses DIASTOLIC SHOCK: It is palpable 2nd heart sound. THRILL: It is a palpable murmur & feels like the purring of a cat. [Note:Diastolic thrills are better felt than systolic.] [Note:Thrill is present in stenotic lesions & absent in regurgitant (as the turbulence produced by low flow is coarse).] PERCUSSION The finger should be placed along the length of the ICS. The static finger is the pleximeter while the striking finger the flexiform. Left border: Technique: start from the 4th or 5th ICS in midaxillary line & come medially. The left heart border should coincide with the apex. If outside apex- consider pericardial effusion. Upper border: for 2nd & 3rd space paramedially on the left side. If dullness is present in the left 2nd / 3rd ICS anteriorly, the possibilities are- - Pericardial effusion - Aneurysm aorta - Dilated PA - L posed aorta - Ductal ampulla aneurysm Right heart border: Technique: percuss in the midclavicular line till liver dullness → come one space higher→ percuss medially till sternum. Normally Rt. HB should be retrosternal. If dullness present, it may suggest: - pericardial effusion - right atrial enlrgement - aneurysm ascending aorta - dextrocardia
- 51. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 51 AUSCULTATION The areas for auscultation are: Mitral area Left 5th ICS inside the MCL Tricuspid area Lower end of sternum Aortic area 2nd right ICS Erb’s area 3rd left ICS Pulmonary area 2nd left ICS 1ST HEART SOUND: Q-What are the causes of split 1st heart sound? A- - Electrical- - RBBB - VPB - Mechanical- - MS - TS - Myxoma - Ebsteins Q-What is a normal 1st heart sound? A-A sound that is normal by character (no split) & intensity (experience). Q-When is S1 considered loud? A-When: - louder than A2 at the apex - equals/ louder than S2 at base. Q-Why is the 1st heart sound split in Ebsteins? A-Due to: - RBBB - RV dilatation Q-What are the causes of a loud 1st heart sound? A-S 1 maybe loud in: 1) Sinus tachycardia 2) Normally in children 3) High flow states- fever, anemia, pregnancy, thyrotoxicosis 4) Increased ventricular filling- MS, TS 5) Lt. To rt. Shunt- ASD, VSD, PDA 6) Short PR interval
- 52. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 52 Q-What are the causes for a soft 1st heart sound? A- 1) Poor conduction of sound- thick chest wall, emphysema, pleural & pericardial effusions. 2) MR, TR 3) Calcific MS 4) Long PR interval [Note:S 1 is normally single & heard all over the precordium] Q-What is the cause of a ‘reverse split’ of 1st heart sound? A-Due to: 1) MS 2) LA myxoma Q-Normally why does the MV close earlier than the TV? A-Due to septal activation being from left to right. SECOND HEART SOUND: Normally A2 is audible in all areas while P2 is audible only in the pulmonary area & for a short distance from the left sternal border. Q-What is the normal splitting of S 2? A-Normal spitting of the 2nd heart sound is: During inspiration= 0.06 sec During expiration= 0.02 sec Q-When is P2 considered loud? A-P2 is loud if: - it is heard at the apex - same or louder than A2 in the pulmonary area. Q-When is A2 considered loud? A-A2 is loud if: - it is louder than P2 in the pulmonary area. Q-What are the causes of a widely split S2? A-The causes are: -Electrical- - RBBB -Mechanical- - ASD - VSD - PS - RVF - MR - TAPVC
- 53. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 53 Q-What are the causes of a reverse split S2? A-The causes are: -Electrical- - LBBB - WPW syndrome -Mechanical- - AS - PDA - Coarctation - Systemic HT - LVF Q-Enumerate causes of Single S2? A-A single S2 maybe due to: -A2 or P2 being soft - AS - PS - TOF -A2 & P2 summation - VSD.PH - Single ventricle - Truncus Q-What causes of Loud P2? A-Pulmonary hypertension causes loud P2. A rough estimate of PH can be obtained & is mentioned below. If P2= A2 Mild PHT, PASP 30- 40 mm Hg If P2> A2 moderate PHT, PASP 40- 75 mm Hg A very loud P2 severe PHT, PASP > 75 mm Hg) Q-What causes a loud A2? A-Systemic hypertension causes loud A2. Q-What is the movement of S2 split in relation to respiration? A-During expiration, A2 & P2 nearly overlap. With inspiration, it is the P2 which moves away. The A2 is fixed. THIRD HEART SOUND: Heard in the following conditions: 1) Normally till 30 years age 2) Normally in pregnancy 3) MR 4) TR 5) CCF 6) Myocardial infarction.
- 54. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 54 Q-What causes appearance of the 3rd & 4th heart sounds? A-The 3rd & the 4th heart sound are due to abnormal filling patterns in the ventricles. LVS3- during early rapid filling LVS4- during atrial systole FOURTH HEART SOUND: *It represents a decreased compliance/ increased stiffness of the LV/RV. *It is best heard with the bell of the stethescope with the patient in the left lateral position. MURMUR Q-Describe the grading of murmur. A-Grading of murmur was described by Levine & freeman in 1933. I- III: are without thrill IV- VI: are with thrill Grade I: very faint murmur Grade II: faint but easily audible Grade III: loud without thrill Grade IV: loud with thrill Grade V: Louder, heard else where, with the side of the stethoscope placed sideways Grade VI: Heard with the stethoscope lifted away from the chest wall. [Note:Earlier the systolic murmurs were divided into 6 grades & the diastolic murmurs into 4 grades] Q-Which systolic murmurs are significant? A-All systolic murmurs ≥ grade III are hemodynamically significant. Q-Discuss murmurs in child. A-Diastolic murmurs are always organic. Systolic murmurs: - Pansystolic- always organic; due to VSD, MR, TR - Ejection systolic- organic if has associated a. Symptoms b. Cardiomegaly c. > grade III d. associated ejection click Q-Describe the D/D between hypertensive PR Vs Normotensive PR. A- Hypertensive PR Normotensive PR Murmur Decresendo Cresendo decresendo P2 loud soft RVH + - Etiology All conditions with increased PAP APVS, post IE PV, idiopathic dilatation of PA, RVOT patch
- 55. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 55 Q-What are the causes of continuous murmur? A-The causes are: In a acyanotic: 1) PDA 2) AP window 3) RASOV into RA/ RV 4) Gerbodie defect 5) Coronary artery- RA fistula 6) Peripheral PS 7) ALCAPA In a cyanotic: 1) With PDA 2) Bronchial collaterals 3) Pulmonary AV fistula 4) Surgically created shunts Q-What is the D/D of apical murmur in CHD? A-Apical murmur maybe due to: 1) ASD with MVP 2) Primum ASD 3) Ebsteins with c TGA OTHER SOUNDS: -Opening snap Q-Besides MS, what are the other causes of an opening snap. A-The possible causes maybe: From the Mitral valve From the tricuspid valve MR ASD PDA TR VSD Ebsteins. Q-When is the characteristic of a continuous/ machinery murmur? A-It crosses over the 2nd heart sound.
- 56. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 56 CARDIOPULMONARY BYPASS Q-What should include a Prebypass checklist? A-It should include: - Occlusion - Heparin - ACT=__________ - Line pressure - Cool to_____C - Clamp off - Anesthesia - Bubble detector Q-How are flow rates calculated on pump? A- = BSA x 2.5 L/ m2 < 7 Kg 120- 200 ml/ min 7- 10 Kg 100- 150 ml/ min 10- 20 Kg 80- 120 ml/ min > 20 Kg 2.4 L/ min/ m2 All to maintain a mixed venous O% of 60- 70% Q-What are the various levels of Hypothermia? A- Mild 32- 35C Moderate 28- 32C Severe 18- 28C Profound 15-18C Q-What are the considerations for conducting CPB during pregnancy? A-The considerations are: 1) Avoid CPB, if possible (avoid the surgery) 2) If possible, perform during the 2nd trimester 3) Continuous fetal heart rate monitoring 4) Keep high flow rates (> 3 liters/ min/ m2) 5) Avoid acidosis & low PaO2 6) Maintain perfusion pressure above 65 mm Hg, for adequate blood flow to the uterus 7) Low priming volume (for lesser hemodilution) 8) Hct > 22% 9) Turn patient to left (15- 20) to keep gravid uterus off the IVC 10) Do not cool 11) Restrict cardioplegia to minimum & aspirate away, if possible (to avoid hyperkalemia) 12) Strict Act monitoring
- 57. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 57 13) Avoid alpha agonist 14) Avoid SNP (cyanide toxicity to fetus) 15) Administer tocolytics Maternal mortality= 3% Fetal mortality= 19% Q-Can LMWH be administered in pregnancy? A-No, as it crosses the placental barrier. Q-What are normal blood volumes? A- Children= 85 ml/ Kg Adults= 65 ml/ Kg Q-How to calculate the amount of autologous blood to be removed? A- Volume to be removed= {Total bld volume x (Initial Hct- Desired Hct)}/ mean Hct Q-How to calculate the amount of blood to be added? A- Volume of blood = [(Bv + Pv) x Desired Hct – Bv x Hct of patient]/ Hct donor blood to be added (ml) Bv= blood volume of patient Pv= priming volume Q-What is the height difference between the patient & the reservoir, during CPB? A-It should be 25- 30 inches. Q-What are the ways of confirming cardioplegia delivery? A-Indicators of cardioplegia delivery are: 1) Aortic root distension 2) Heart stopping immediately 3) Generalized cooling of the myocardium 4) Coronary veins become bright red & distended 5) Blood returning from opposite coronary ostia if direct coronary injection being given Q-When does the myocardial activity continue even after delivery of cardioplegia? A-The possibilities are: 1) Partially applied aortic clamp 2) AR 3) Incomplete venous drainage 4) K+ not added
- 58. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 58 Q-What are the types of pumps? A-The pumps can be classified as: Positive Displacement - Roller - Peristaltic (affinity) - Blade Centrifugal - Vortex (Biopump) - Impeller o Radial o Axial o Mixed Q-What are the specifications of the ‘Biopump’? A- Priming volume= 86 ml Inlet/ outlet ID= 3/8 inch (9.5 mm) Maximum operating pressure= 1100 mm Hg Outer housing of polycarbonate Q-What is secondary cardioplegia? A-Is used when, due to poor myocardial protection, the patient cannot be weaned off bypass. It comprises of high potassium, substrate enhanced cardioplegia administered over 15- 20 minutes. The benefits are: 1) Channelising post ischemic O2 uptake towards reparative processes rather than wasting the aerobic energy towards needless electromechanical work 2) Restores synchronous contraction Later the heart is allowed to beat empty for upto 30 minutes. Q-What is ‘Kiss approach’ for open-heart surgery? A-It was advocated by Victor Solomon. KISS stands for “Keep It Simple and Safe”. Q-What are the reasons & management of High K+ on bypass? A-Reasons are: 1) Suction hemolysis 2) Priming with banked blood 3) Small tip aortic cannula (hemolysis) 4) Prolonged CPB Management includes: 1) Calcium 2) NaHCO3 3) Glucose insulin 4) Lasix
- 59. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 59 Q-What are the advantages of Mannitol during CPB? A-Advantages are: 1) Cardioprotective/ neuroprotective 2) Renoprotective- increase urine formation 3) Maintains oncotic pressure 4) O2 free radical scavenger Q-Based on O2 dissociation curve mention disadvantages of conventional cardioplegia? A-They are: 1) Hypothermia- causes shift to left hence O2 is not easily released from Hb 2) Alkalosis- shift to left hence O2 is not easily released from Hb These actions are negated by: 1) Tissue acidosis- shift to right hence O2 is released from Hb 2) Hypercarbia- shift to right hence O2 is released from Hb Q-What is the importance of 2,3 DPG in cardiac surgery? A- 2,3 DPG is low in banked blood increased amount used shift of curve to left less O2 available for tissues Q-Why on bypass a high PaO2 is maintained? A-A high PaO2 is required as on CPB the Hct is low. Hence for a higher O2 content of blood a high high PaO2 has to be administered. Q-What is Heparin rebound? A-Post CPB, after neutralization of heparin with protamine, the heparin that is bound to plasma proteins does not get neutralized. This is released later (after few hours) leading to free heparin in blood. Q-What is Pulmonoplegia? A-Infusion of pulmonary artery with cold preservation solution prior to its procurement for transplantation. Q-What are the disadvantages of fibrillatory arrest? A-It can cause subendocardial ischemia & necrosis. Q-What is ‘electroplegia’? A-For CABG on bypass- stimulate the vagus to arrest the heart transiently to enable a stitch & then remove stimulus (experimental). Q-What are the various counterpulsation techniques? A-They are: 1) IABP 2) BASH (Body acceleration synchronous heart beat) 3) Pneumatic bandages over the body 4) Withdraw blood from one femoral artery during systole & inject into the other during diastole.
- 60. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 60 Q-What is the concept of hemodilution? A-It was introduced by By Zuhdi & Gott (1962) Advantages of hemodilution are: 1) Decrease in viscosity leading to decreased SVR (hence increased perfusion) & also requirements of lower flows 2) No use of blood products for prime- less chance of transmission of blood mediated diseases, less load on the blood bank & for Jehovah’s witnesses 3) Increased urine formation Q-What are absolute contraindications for retrograde cardioplegia? A-They are: 1) Left SVC 2) Unroofed coronary sinus Q-What is the amount of blood pushed, per revolution, thru’ the tubing used in CPB? A- 3/8th tube= 22ml 1/4th tube= 12 ml Q-Decsribe the causes of gas embolization during CPB? A-Incidence= 1/ 8,000 open hearts Causes are: 1) Inattention to level of oxygenator (generally seen after starting vasodilators. Prevention- minimum level required for next 15 secs should be maintained. Use of bubble detector, detecting bubble > 1cc ) 2) Inadequate debubbling of the system before CPB 3) Poor surgical technique 4) Sudden return of cardiac activity 5) Break in the integrity of the oxygenator & connections 6) Clotted oxygenator 7) Air entry thru’ the cardioplegia line 8) Runaway pump 9) Reversal of the LV/ aortic vent 10) Rapid cooling & rewarming Q-How to monitor gas emboli on CPB? A-By using: 1) Infrared sensors on the arterial line 2) Carotid artery Doppler monitoring Q-Ennumerate ways of preventing of air embolism? A-Air embolism can be prevented by: 1) Attention to reservoir level 2) Light on arterial line 3) Arterial filter 4) Sensors on reservoir level/ arterial line
- 61. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 61 Q-What actions are to be taken if air has entered thru’ the arterial line? A-The following actions are to be taken. - Cooling of patient & administration of 100% oxygen - Head low - Increase depth of anesthesia with thiopentone - Administer mannitol & corticosteroids - Retrograde cerebral perfusion Q-What are the problems of venting thru’ the aorta? A-The problems are: 1) Faster rewarming (as blood passes thru’ the entire left side of heart) 2) LV distension possibility 3) Has to be stopped during cardioplegia Q-When is definite indication of venting the PA? A-RA myxoma. Q-Enumerate techniques for achieving ‘pulsatile flow’ during CPB? A-Techniques are: 1) Additional pump after oxygenator 2) IABP 3) After removal of cross clamp allowing the beating heart to be partially full 4) Changing revolution of pump constantly [Note:Historical technique- Cross circulation] Q-What are the various anomalies of coronary sinus? A-They are: 1) Absent coronary sinus (left SVC into LA- Ragib’s defect) 2) Hypoplastic coronary sinus- some veins opening directly into RA 3) Atretic coronary sinus 4) Dilated coronary sinus - without L-R shunt: Lt. SVC into coronary sinus - with L-R shunt: intracardiac TAPVC 5) Unroofed coronary sinus Q-Describe St. Thomas hospital cardioplegia solution. A- First described by Mark Brainbridge & Hearse. St. Thomas I in 1975 & St. Thomas II in 1981. (St. Thomas Hospital is in London.)
- 62. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 62 Composition is: (All in per liter of solution) St. Thomas 1 (Trade name: MacCarthy) St. Thomas 2 (Trade name: Plegisol) NaCl (mmol/L) 144 110 KCl (mmol/L) 20 16 MgCl 16 16 CaCl2 2.4 1.2 NaHCO3 - 10 Procaine 1.0 - PH 5.5- 7.0 7.8 Osmolarity 300- 320 285- 300 St. Thomas 1 prepared by adding 1 ampoule (16 + 16 + 1) to 1 liter ringer lactate Q-How much is the pressure with which the cardioplegia solution is pumped? A-A maximum of 100 mm Hg difference between the pumphead & aorta. Q-What happens if cardioplegia is administered at a high pressure? A-It can result in rupture of capillaries & arterioles. Q-What are the advantages of snugging SVC/ IVC on bypass? A-The advantages are: 1) For RA/ RV surgery 2) During accidental opening of the RA during left sided surgery 3) Prevents early rewarming of the heart Q-What is the pressure at which cardioplegia is delivered? A- Antegrade cardioplegia: 120 mm Hg- 1st cardioplegia : 75 mm Hg- 2nd cardioplegia Retrograde cardioplegia: 25 mm Hg Q-Why is the LCA the first to be perfused during direct osteal cardioplegia delivery? A-Because: 1) The LV will be arrested first 2) It is easily seen. Q-How much the Hct is maintained on bypass? A-Normally 20- 25%. Lower Hct is required to be maintained with hypothermia Mild 25% Hct Moderate 22- 25% Hct Severe 18- 22% Hct
- 63. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 63 Q-What is the Hct of cardioplegia? A- 10% Q-What are the advantages of blood in cardioplegia? A-They are: 1) Acts as buffer 2) Has O2 carrying capacity 3) Provides substrates for metabolic demands of myocardium 4) Free O2 radical scavengers 5) Anti-edema action due to high colloid osmotic pressure Q-What are the disadvantages of blood cardioplegia? A-They are: 1) Increased viscosity, leading to stagnation 2) Shift of O2 dissociation curve to left, hence O2 not readily released 3) The high amount of O2 & substrates are not really required Q-What are the various additives to cardioplegia? A-They are mentioned below: ADDITIVE FUNCTION Potassium, Magnesium & procaine For immediate arrest Hypothermia (10- 20C) For decreased metabolism Glucose As substrate for metabolism Oxygen/ blood Substrate Glutamate & aspartate Substrate Bicarbonate/ THAM/ phosphate Buffer (to provide optimum environment for metabolism) FFP/ albumin Colloid (provide osmotic pressure & hence preventing cellular edema) Mannitol For reducing edema Methylprednisole For preventing edema Q-What is normal heart O2 uptake & what is the concept of warm induction? A-The heart uptakes O2 over time & not by dose. Hence during warm induction, it is important to deliver the cardioplegia over a period of 5 minutes. This is followed by delivery of cold cardioplegia over 3 minutes. The strategy of warm induction is especially useful in energy-depleted hearts like; - Cardiogenic shock - Left main disease with unstable angina - LVF Q-What is the purpose of periodic cardioplegia? A-It is for: 1) Maintaining arrest 2) Hypothermia 3) Buffer for acidosis
- 64. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 64 4) Provision of O2 5) Provide substrate 6) Wash out metabolites 7) Counteract tissue edema Q-What are the types of membrane oxygenators? A-They are: 1) Hollow fibre - cross current - counter current 2) silastic membrane Q-Mention technicalities of the hollow fibre design. A- 1) O2 flows thru’ the hollow fibres & blood from the outside 2) O2 depends upon the blender 3) CO2 diffusion is passive 4) The resistance to blood is high by the oxygenator, hence the pump is placed prior to the oxygenator 5) Heat exchange is prior to oxygenator (blood passes over water filled coils) Q-Mention technicalities of a silastic membrane design. A- 1) An envelope of silicone rubber membrane is wrapped over a central spool. The O2 passes inside the envelope & the blood thru’ the windings. 2) Rest as with hollow fibre design (points 2- 5) Q-What is the speed of cooling and rewarming during CPB? A-Cooling occurs more rapidly than rewarming 0.1- 1.5C/ min Vs 0.3 – 0.5C/ min Q-What is the temperature gradient between blood & water (heating bucket) during rewarming & cooling? A-It should be always 10C. If it is more then: - during fast cooling: when the cold blood reaches the patient O2, CO2. & nitrogen will bubble out at the aortic end - during rapid rewarming: when the warm blood reaches the heat exchanger, bubbles will form. Q-Mention specifications of arterial filters. A-They are: - 25-40 um - at flow of 7 lit/min, gradient across filter is 30 mm Hg - 200 ml is required for priming
- 65. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 65 Q-Provide brief description of ‘Cell savers’. A-Introduced by Ansell (J Thorac Cardiovasc Surg, 1982) Principle is as follows: - blood sucked (by wall suction power) - to this heparin added - 20 um filter to remove clots/ debris - RBC’s washed - Centrifuge to concentrate - Transfer to plastic bag for infusion Q-Briefly describe total body retrograde perfusion? A-First described by Yasuura, J Thorac Cardiovasc Surg 1994. Total flow of 300- 500 ml/ min is administered at 13- 15C, at a pressure 30 mm Hg Q-What is Post pericardiotomy syndrome? A-It is seen 1- 2 weeks after CPB & lasts for 3- 5 weeks. It is characterised by fever, malaise, leucocytosis, pericardial effusion, pericardial rub, and pleuritic chest pain. It responds well to NSAID’s +/- steroids. Etiology- not known (? Viral mediated) Q-Discuss strategies for CPB induced complication. A-The following are the strategies: 1) Heparin coated tubes to reduce blood activationby: Heparin coating technique: - Ionic bonds: Eg. Duraflo II (Baxter) - Covalent bonding: heparin is attached to spacer arms (100 A long). Eq. Carmeda (Medtronic) 2) Controlled activation of complements by - Use of aprotinin - Gp IIb/IIIa receptor antagonist to prevent platelet activation (experimental) Q-What is reperfusion injury? A-It is defined as, “the functional, metabolic & structural alterations caused by restoring blood flow after a period of temporary ischemia.” Pathophysiology: It is due to: 1) Intracellular calcium accumulation 2) O2 free radical release 3) No reflow phenomenon 4) Cellular edema Q-How can reperfusion injury be avoided? A-By providing an environment that is: 1) Hyperosmolar 2) Substrate enriched 3) Hypocalcemic 4) Contains O2 free radical scavenger
- 66. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 66 Q-What are the various sources of oxygen free radicals? A-They are: 1) Lipid peroxidation 2) Neutrophil mitochondria (superoxide dismutase) 3) Conversion of hypoxanthine to xanthine 4) Arachidonic acid metabolism 5) Heber Wiess reaction Q-What is ‘No reflow’ phenomenon? A-It is a regional vascular occlusion, in the brain & probably other organs, leading to a no reflow phenomenon after reperfusion of the tissues. Initially thought to be due to hypothermia, but is now believed to be a response due to hypoxic endothelial cell damage. Q-What are intraoperative signs of inadequate myocardial protection? A-They are: 1) Difficulty in defibrillating heart 2) Discoloration of heart 3) Poor contractility 4) Abnormal ECG; - ST elevation - Low voltage - Wide QRS & loss of R Q-What are the indication for topical cooling? A-The indications are: 1) During AVR when RCA ostia is not present or cannot be perfused 2) Coronary artery disease with occluded RCA, where RV protection is not possible 3) Individual preference of surgeon. Q-What are the disadvantages of topical cooling? A-They are: 1) Phrenic nerve injury 2) If the heart is taken out of the pericardial well, for OM/ PD anastomosis: the effect is lost 3) High incidence of atelectasis & pleural effusion Q-Describe the protocol of Heparin administration for CPB. A-Baseline ACT at incision -300 IU/ Kg heparin (porcine or bovine) prior to cannulation -add 2 U/ ml heparin to prime ( 5,000 U in adult) -3 minute waitACTif > 300 secs CPB may be established -if temperature< 30C- maintain ACT > 400 secs & if temperature < 24C- maintain ACT > 500 secs -if ACT < 300 secs after administration of upto 900 U/ Kg heparin, it is heprin resistance. Administer 2 units FFP &/ or 1,000- 2,000 units AT III concentrate
- 67. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 67 Q-Describe Protamine administration protocol post CPB. A-As follows: -2-3 mg protamine per 100 U heparin administered -Check ACT, if within 10 secs of post incision baseline ACT, there is no coagulopathy. If more than 10 secs- suggests coagulopathy- add 25 mg more protamine -Add 20 mg protamine for each 500 ml of heparinised pump blood. -No protamine is required to cover cell saver blood. Q-Is there any rate & site prefernce for protamine administration? A-Recommended is a maximum of 5 mg/ min (in an adult) of protamine. No difference has been noted on the site of administration, i.e., left or right “It is the rate of administration & not the the site of administration” Wakefield (Surgery, 1996) demonstrated a significant drop in the BP, HR & CoP with a rapid administration of protamine to reverse heparin. Q-What are the reasons for heparin rebound? A-2 reasons are implicated 1) Release of heparin bound to plasma proteins 2) Release of heparin bound to endothelium Maximum is within 1-3 hours, can appear as late as 6 hours. It should be suspected if signs of bleeding appear after a period of dryness in the operating field. Q-Can LMWH be used for conducting CPB? A-Yes. Disadvantages of LMWH for conducting CPB are: - No effective dosage known - Inadequate reversal with protamine Q-Describe the protocol followed for using LMWH for CPB. A-Anticoagulation protocol with LMWH is as follows (A. Carpentier) - LMWH- 75 mg/ m2- IV bolus (Additional 10 mg for every unit of blood added to the prime) - If expected CPB < 60 minutes- monitor ACT - If expected CPB > 60 minutes- monitor anti Xa activity - If Anti Xa activity is > 1 IU/ml the proceed with aortic cannulation - Repeat Anti Xa activity 1 hourly & if it is < 1.4 IU/ml, add 40 mg/m2 of LMWH every 1 hour Results with the above policy: 1) Protamine reversal was partial 2) Postoperative bleeding was more with LMWH 3) No effect on decreasing the requirements of blood or blood products (due to CPB induced coagulopathy) [Note:LMWH is used only if unfractionated heparin is contraindicated]
- 68. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 68 Q-What are the advantages of venting heart, during CPB? A-They are: 1) Prevents LV distension 2) Decreases wall tension 3) Increased subendocardial blood flow 4) Maintains a dry field Q-Discuss the pathophysiology of ‘ill effects’ of CPB. A-Ill effects are due to: 1) Abnormal hemodynamics: a) non pulsatile flow b) decreased perfusion pressure c) decreased colloid osmotic pressure d) hypothermia 2) Adsorbed plasma proteins: viz. fibrinogen, albumin, Factor XII 3) Activation of blood constituents (most important mediator of morbidity due to CPB). Blood constituents activated are a) plasma protein systems, viz i. contact system: Factor XII, Factor XI, prekallikrein, high molecular weight kininogen ii. intrinsic coagulation pathway (major stimulus for coagulation during CPB) iii. extrinsic coagulation pathway iv. complement system v. fibrinolytic system b) blood cells, viz. i. platelets ii. neutrophils (mediate much of the inflammatory response due to CPB) iii. monocytes iv. lymphocytes v. endothelial cells Q-What are the various emboli produced during CPB? A-They are: 1) Fibrin 2) Platelet aggregates 3) Neutrophil RBC debris 4) Gaseous (nitrogen, oxygen) 5) Spallated material
- 69. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 69 GENERAL POINTS Q-Enumerate the complications related to patient positioning? A- Supine: 1) Occipital alopecia- avoided by ½ hourly change of position of head position in OT & ICU Lateral decubitus: 1) Neck injury while rotating 2) Eye injury due to corneal ulceration 3) Compression of axillary plexus (keep axillary roll) 4) Kinking of axillary/ subclavian artery 5) Compression over the lateral peroneal nerve of the dependent leg Q-What are the nerve injuries seen secondary to mid sternotomy? A-Incidence of nerve injury to upper limb is 2- 18%. Believed to be due to 1st rib compression of the brachial plexus during sternal retraction. Prevented by: - limited retraction - caudally placed chest spreader Usually resolves within 6 months. Q-In which conditions is there higher chances of injury to the innominate artery (prior to sternotomy) during suprasternal dissection? A- 1) AR 2) Systemic hypertension 3) Arch aneurysm Q-What is the ideal way of aortic cannulation. A-Side clamp incise pursestring cannulate Q-What are the possibilities if post aortic cannulation, there is no blood in the cannula? A-The possibilities are: 1) Abutting against wall- blood will come on turning the cannula, 2) Dissection- there will be no change with the movement of the cannula. Q-How much is accepted occlusion level? A-< 1 cm/min Q-What is the ‘rated flow’ of an oxygenator? A-At 37C the flow at which the oxygenator can oxygenate blood to 100%. Q-How should one proceed if the cross clamp is loose & has to be reapplied? A-Take another cross clamp & apply distally and then remove the 1st clamp.
- 70. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 70 Q-How the azygous vein identified intraoperatively? A-It is: - present at the pericardial fold - located posteriorly - dark in color. Q-What is Gott shunt? A-Made of TDMAC (tridodecyl methyl ammonium chloride) with heparin coating. It is inserted from the LV apex to the ascending aorta/ descending aorta. Q-Who was Adam Kiewicz? A-German, in1881, described the spinal blood supply.
- 71. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 71 VALVUHAR HEART DISEASE GENERAL Q-What are the echo predictors of embolism in a patient with infective endocarditis? A-(By JACC, 2001) Increased chances are if it is: - a mobile vegetation - > 10 mm vegetation (if > 15 mm vegetation then chance of embolisation is 80%) Q-What are type of prosthetic valve endocarditis? A- - Early; within 60 days - Late; after 60 days Risk of prosthetic valve endocarditis is greatest within the first 6 months after surgery, especially the first 6 weeks. < 12 months- organism is usually staph aureus > 12 months- organism is usually streptococcus Q-What is the difference between prosthetic valve endocarditis & native valve endocarditis? A-NVE is largely confined to leaflet. In PVE, the infection commonly extends beyond the valve ring, into the annulus & para annular tissue. Q-Discuss the burden of rheumatic fever & CHD in Indians? A-Padmavati, IHJ 2002 Total population of India= 1,027 million 34% are below 15 years CHD: 4- 12/ 1000 live births 1,12,000 are added to CHD total every year RHD: 5 lac children (< 15 yrs) have RHD 14 lac of total population have RHD 0.09% of the population has RHD 50,000 are added every year to the total. Q-What is the pattern of rheumatic fever in Indians? A-IHJ 2002, Chandigarh. The following manifestation pattern is seen during the 1st & 2nd attacks of rheumatic fever. Symptom Incidence during 1st attack Incidence during 2nd attack Fever 75% 70% Arthritis 60% 60% Arhtralgia 40% 20% Carditis 22% 70% Chorea 16% 10% [Note:Incidence of anaphylaxis to penidura: 0.8- 4/ 10,000 courses of penidura.]
- 72. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 72 Q-Describe the prophylaxis against RHD? A-AHA guidelines (1995)- Dajani et al (Journal- Pediatrics, 1995) Primary prophylaxis: Consider all sore throat as streptococcal infection and treat (unless throat swab proves otherwise. The prophylaxis consists of- Agent Dose Mode Duration Benzathine penicillin G 6 lac units for 27 Kg 12 lac units for > 27 Kg intramuscular Single Penicillin V (phenoxymethylpenicillin) Children: 250 mg, 2-3 times daily Adolescents & adults: 500 mg 2-3 times daily Oral 10 days For those allergic to penicillin: Erythromycin Estolate Ethylsuccinate Azithromycin 20- 40 mg/ Kg/ day, 2-4 times, max 1gm/ day 20- 40 mg/ Kg/ day, 2-4 times max 1gm/ day 40 mg/ Kg/ day, 2-4 times max 1gm/ day 500 mg on first day & later 250 mg/ day for 4 days Oral Oral Oral Oral 10 days 10 days 10 days 5 days Secondary prohylaxis: 3 subgroups of patients Group Prophylaxis Rheumatic fever + Carditis + Valvular heart disease + For 10 years & till atleast 40 years of age, with consideration of lifelong therapy (especially in endemic areas) Rheumatic fever + Carditis + Valvular heart disease - Atleast for 10 years or into adulthood; whichever is longer Rheumatic fever + Carditis - Valvular heart disease - Atleast 5 years or till 21 years of age, whichever is longer Prophylaxis is using: 1) Benzathine penicillin: if > 27 Kg- 12 lac units If 27 Kg- 6 lac units 4 weekly in developed countries 3 weekly in developing countries 2) Penicillin V 250 mg BD- 3) Erythromicin 250 mg BD- 4) Sulphadiazine: 1 gm OD if > 27 Kg 500 mg OD if< 27 Kg
- 73. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 73 Q-What is the potential for vaccines against rheumatic fever? A- (from IHJ 2002) Vaccine strategies are: 1) Against M protein- due to nearly 93 types, a polyvalent vaccine is required. Also there is risk of cross reactivity with the heart tissues 2) Against bacterial attachment to mucosal surface (against fibronectin binding protein) Limitation of an above vaccine project: is a lack of animal model. Q-Why is barium impregnated in the silicone ball of a Starr Edward valve? A-To: 1) Reduce the wear & tear 2) Make it radio opaque Q-Which are the conditions with 50% cardiomegaly & requiring surgery? A-The conditions are: 2) TOF 3) Isolated AS 4) Constrictive Pericarditis Q-What are the ECG D/D of 100% cardiomegaly? A- - Dilated cardiomyopathy – RBBB, VPCs - Pericardial effusion – low voltage QRS - Ebstein’s anomaly - waves Q-What are the prerequisites for elective cardioversion of atrial fibrillation? A-The patient should be: 1) Fasting, 2) Anesthetized, & 3) Anticoagulated The shock should coincide with the ‘R’ wave of the ECG Q-What is Internal cardioversion? A-If external has failed. The electrodes are placed in the right atrium & coronary sinus Q-What are the causes of acute deterioration, in a patient with valvular heart disease? A-It maybe due to: 1) Atrial fibrillation 2) IE 3) Carditis 4) LRTI
- 74. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 74 Q-Which conditions are characterized by cough which is relieved on bending forward? A-In 1) arch aneurysm 2) APVS Q-What is the incidence of atrial fibrillation? A- In general population: 0.4- 2% In > 60 years age group: 10% Q-What is the importance of atrial fibrillation? A-Atrial fibrillation is associated with: Increased morbidity & mortality. In MS if atrial fibrillation is present the mortality is increased by 17 times In coronary artery disease if atrial fibrillation is present the mortality is increased by 7 times. Q-Discuss digoxin & ECG. A- Digitalization: Mirror image tick sign of ST segment with isoelectric ST segment & upright T wave Toxicity: Mirror image tick sign with ST depression & T inversion Q-What are the orifices of the normal mitral valve? A-They are: - Primary- at the annular level (not affected in RHD) - Secondary- cuspal level - Tertiary- chordal level Q-What are the criteria for a giant LA? A-They are: 1) Kawazoe (Ann Thorac Surg 1982) - LV compression- bowing of posterior wall of LV by > 30 mm in the long axis view - X Ray: a) carinal angle > 120 b) left bronchus/ trachea ratio < 0.4 c) right CTR > 0.6 2) Piccolli criteria: LA dimension (AP) on echo > 65mm Q-What are the ways of dealing with large LA? A-If the LA is: < 8 cm- Kawazoe plication > 8 cm- Batista extended resection with autotransplantation
- 75. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 75 Q-What are commissural leaflets? A-Sometimes accessory leaflet tissue is present at the commissures of MV, termed as commissural leaflets. It is functionless. Q-When to term as pulmonary hypertension? A-When Mean PAP> 20 mm Hg Peak SPAP > 30 mm Hg Q-What cardiac conditions are associated with a high risk of mortality in pregnancy? A-There is increased risk of mortality if: A-if following heart diseases present 1) Eisenmengerization 2) LVEF < 20% 3) Marfan’s with ascending aorta > 40 mm diameter Q-What is dilated coronary sinus a feature of? A- 1) CCF 2) Intracardiac TAPVC 3) Left SVC into coronary sinus MITRAL STENOSIS Etiology: 1) RHD 2) Congenital 3) Lutembachers 4) Endomyocardial fibrosis 5) Hurlers syndrome ( 1 iduronidase deficiency) Signs: - Pulsus parvus - Tapping apex - Diastolic shock - Diastolic thrill - Heart sounds- Loud S1, Loud P2, OS- may/ may not be present - Murmur- middiastolic murmur with a presystolic accentuation heard over the apex, radiating to the axilla, best heard with the bell of the stethoscope, with the patient in left lateral position & breath held in expiration & increased on clinching the fists. [Note:The sign of severity of MS is the S2- OS interval (shorter the interval, more severe is the stenosis)]
- 76. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 76 Q-Discuss D/D of MS? A- 1) TS- will have no sign of PH, different site of murmur, increase in murmur on inspiration 2) LA myxoma- will have constitutional symptoms, postural syncope, tumor plop. 3) LA thrombus. 4) Cor triatriatum Q-How does a patient of MS improve spontaneously? A-Due to: 1) Development of TR 2) Development of PH 3) Development of precapillary stenosis (secondary MS) Q-What is earliest age reported for rheumatic fever? A-3 years of age (Padmavati). Q-What is the earliest age reported for rheumatic MS, requiring intervention? A-6 years (reported by Stanley John, circulation 1983). Q-What is the earliest age reported for rheumatic MR, requiring intervention? A-4 years, Carpentier (Circulation 2001). Q-What are the indications for operating a patient with MS? A- 1) Moderate/ severe MS with Class III or more symptoms. 2) Asymptomatic MS if - LA clot - Thromboembolism - Pulmonary hypertension (PASP > 60 mm Hg) - RV dysfunction (RVID (D) > 17 mm/m2) - Critical MS (area < 0.7 cm2) - ? atrial fibrillation - Hemoptysis Q-Compare OS Vs LVS3. A- OS LVS3 High pitched (not palpable) Low pitched (palpable) Heard best with diaphragm heard best with bell No change with respiration ↑ with expiration
- 77. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 77 Q-What decides the severity of MS? A-The A2- OS interval decides the severity of MS. 0.08- .12 sec mild (LAP 15 mm Hg) 0.04- 0.08 sec moderate (LAP 20 mm Hg) 0.04 sec severe (LAP 25 mm Hg) Q-What are the reasons for loud S1 in MS? A-Due to tensing of MV leaflets due to late closure of a fully opened MV. Q-What is the reason for an OS? A-It is due to tensing of MV after it opens in diastole. Q-Describe conversion of jet velocity to peak systolic gradient. A-mm Hg= 4V2 Eg. If v= 3 m/sec Pressure= 4 x 32= 36 mm Hg Q-What is Gorlins index? A- Valve area= Flow --------------------------------------------------- C x 44.3 x square root of pressure gradient C (constant) for AV= 1, & for MV= 0.85 Q-What is pathological difference between TS & MS? A-In TS there is rarely: 1) Affection of the subvalve & 2) Calcification Q-What is change is size of the MV annulus during systole? A-The MV annular size changes by 26% (due to contraction of the basoconstrictor muscle comprising of bulbospiral & sinospiral muscles) Q-What is the incidence of TB in MS? A-Low. Q-Discuss ECG correlation with severity of MS. A-ECG will reveal the following 1) LAE 2) PH- strain pattern 3) RVH & RAE 4) Axis (mild: 90- 100°, moderate: 100- 110°, severe: > 110°) 5) Rhythm.
- 78. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 78 Q-How is size of inoue balloon, for BMV, calculated? A-Size of balloon= {height (cm)/ 10} + 10 Q-During BMV why a pigtail is kept in the aorta? A-To avoid damage to the NCC during septal puncture. MITRAL REGURGITATION Etiology: Organic- 1) RHD 2) Mitral valve prolapse 3) Infective endocarditis 4) Papillary muscle dysfunction 5) Endomyocardial fibrosis 6) Collagen disorder- Marfans, SLE 7) Ruptured chordae- secondary to infection & trauma 8) Congenital 9) Os primum defect 10) Methysergide therapy Functional- 1) AV disease 2) Systemic hypertension 3) Cardiomyopathy 4) Ischemia Signs: - Waterhammer pulse - Apex- hyperdynamic - Systolic murmur - Heart sounds: S1 soft, P2 loud, widening of A2- P2 split (due to early closure of MV), LVS3/S4 may be present - Murmur- A pansystolic blowing murmur, best heard at apex, radiating to axilla & back (thru’AML) or Lt. Parasternal region (thru’ PML), with patient in left lateral position, with diaphragm of stethoscope, exercising (clinching fists), no relation of respiration, flow murmur across MV. [Note:The sign of severity of MR is the presence of LVS3] Q-What is Carvallo’s sign? A-It is to differentiate between TR Vs MR. With inspiration if the loudness of murmur, it is a TR murmur. Q-Which MV disease is associated with a midsystolic murmur? A-MV prolapse.
- 79. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 79 Q-What are the reasons for a normal CT ratio in a patient with MR? A-Reasons are: - Acute MR (infective endocarditis, post MI MR, trauma, post BMV/OMC/CMV) Q-What are the reasons for silent MR? A-Reasons are: - Paravalvar leak - Post myocardial infarction MR - Obesity - Emphysematous chest AORTIC STENOSIS Etiology: 1) Valvar - rheumatic - congenital - atherosclerotic - degenerative 2) Subvalvar - idiopathic subaortic stenosis - HOCM 3) Supraaortic - diffuse hypoplastic - hourglass - membrane shelf Signs: - pulsus parvus et tardus - heaving apex - systolic thrill over the aortic area & carotids - Heart sounds- S1 normal, S2: soft A2 with narrow A2- P2 split, LVS3/ S4 may be present, ejection click may be present. - Murmur- Harsh ejection systolic murmur, cresendo decresendo in nature, heard best over the aortic area & apex, radiating to carotids, heard best with the diaphragm of the stethoscope with the patient sitting & leaning forward & breath held in expiration. Findings of severe AS are: - increased harshness of murmur - late peaking of murmur - soft S2 - pulsus parvus et tardus [Note:The sign of severity of AS is the late peaking of murmur]
- 80. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 80 Q-What is the difference between degenerative & rheumatic AS? A- - In degenerative: mainly first involves the cusps - In rheumatic: mainly first involves the commissures Q-What is the incidence of sudden death in AS. A-Sudden death is considered high traditionally however recent studies have shown that the incidence of sudden death, in AS, is low (provided the patient is asymptomatic). Q-Discuss severity of AS on echo. A-JACC 1998. Jet velocity peak gradient valve area Mild < 3m/sec <36 mm Hg >1.5 cm2 Moderate 3-4 m/sec 36- 64 mm Hg 1- 1.5 cm2 Severe > 4 m/sec > 64 mm Hg < 1 cm2 (Area of normal aortic valve= 3- 4 cm2) Q-What is the rate of progression of AS? A-As follows: - Degenerative >> rheumatic - Jet velocity: 0.3 m/sec/year increase - Valve area: 0.1 cm2/ year decrease - Mean transaortic gradient: 7mm Hg/ year increase Q-What are the guidelines for FU of patient of asymptomatic AS? A-(JACC 1998) as follows: - Mild AS: 5 years - Moderate AS: 2 years Q-What is the outcome of asymptomatic AS? A-As follows: - Excellent prognosis - Once symptomatic- prompt surgery Q-What is the incidence of becoming symptomatic in a patient with severe AS? A- - 40% are symptomatic by 2 years - 80% are symtomatic by 3 years (hence strict FU is required for these patients, but can wait for surgery till symptoms appear). Q-What is Gallverdin dissociation of AS? A-Described by Gallaverdin in 1925. In patients with a severe calcific AS, a high velocity ventricular ejection produces a loud midsystolic murmur in aortic area & vibrations of the AV during systole creates a soft apical musical murmur.
- 81. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 81 Q-Discuss indications for surgery in a patient with AS. A-Surgical intervention recommended in AS if: 1) Moderate/ severe AS with symptoms- angina/ palpitations/ dyspnea/ syncope/ presyncope 2) Moderate/ severe AS with ECG e/o ischemia 3) Asymptomatic AS if- - Decrease in LV systolic function - Woman with AS, contemplating pregnancy - Occupation involving increased exertion - Critical AS ( < 0.6 cm2) in whom symptoms are shortly inevitable - Other concomitant procedures - LVPWT > 15 mm Q-Which patients of AS are associated with prolonged PR interval? A-It maybe seen in: - Digoxin toxicity - Calcification/abscess extending into the AV node - Rheumatic carditis Q-What is the significance of atrial fibrillation in AV disease? A-Presence of AF in AV disease indicates: - Coexistant MV disease - Terminal stage AORTIC REGURGITATION: Etiology: 1) RHD 2) Syphilis 3) Infective endocarditis 4) Congenital- bicuspid AV, VSD 5) Connective tissue disorders- SLE, Marfans, RA 6) Dissection of aorta 7) Severe hypertension 8) Trauma Signs: - Waterhammer pulse &other peripheral signs of AR - Hyperdynamic apex - Diastolic thrill (very rare) - Heart sounds- S1 normal, S2: Loud A2 with narrowing of A2 P2 split, LVS3/S4 may be present - Murmur- Early diastolic murmur, decresendo in nature, best heard over the aortic area, sternum & to the left, radiating to apex, heard best with the
- 82. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 82 diaphragm of the stethoscope with the patient sitting, leaning forward & breath held in expiration. - Austin Flint murmur may be present - Murmur of functional AS may be present (with/ without a thrill)- this is the only functional murmur that may be present with a thrill. [Note:The sign of severity of AR is the length of murmur] Q-What does the site of murmur of AR suggest? A-If heard best in: - Erbs area- there is no dilatation of the aortic root- rheumatic - Aortic area- there is dilatation of the aortic root- Marfans (connective tissue) Q-Describe the clinical detection of acute AR. A-Acute AR is suggested by the presence of: - acute onset of symptoms - soft S1- due to closure of MV even before the onset of ventricular systole, due to acute LVVO. - Absence of peripheral signs of AR (If there is echo e/o MV preclosure, then the prognosis is grave, unless immediate surgical intervention is done) Q-What is the importance of Austin Flint murmur? A-Its presence suggests that at least moderate AR is present. Q-What are the causes of Austin Flint murmur? A-Reasons advocated are: - AR jet hitting upon the AML hence producing vibrations - AR jet hitting the jet coming from LA to LV. Q-Why is the AR murmur never more than Grade III? A-As it is high pitched (& hence there is no thrill too). Q-Discuss Syphilitic AR. A-It has the following features: - minimum 9 years post primary syphilis - congenital syphilis is very rarely affects the AV - often associated with coronary osteal narrowing- angina, importance is for impaired cardioplegia delivery Q-Describe the criteria for dilated aortic root. A- - Displacement of coronary ostia > 20 mm from the annulus - Diameter of annulus > 1.5 times normal (in Marfans > 1.34 times; operate)
- 83. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 83 Q-What is Muller’s maneuver? A-Opposite of Valsalva (i.e., breath with nostrils closed). Q-What are the criteria for operating a patient with AR? A- 1) Moderate/ severe AR with NYHA II/III/IV symptoms 2) Asymptomatic AR if a) LV dysfunction - LVID (S) > 50mm - LVID (D) > 70 mm - LVESV > 60 ml/m2 - LVEDV > 200 ml/m2 - EF < 55% - Fractional shortening < 27% b) Moderate/ severe AR along with CABG c) Acute AR Q-What is Smith criteria? A-Operate AR if: - CTR > 60% - LVH on ECG > 60 mm - Pulse pressure > 100 mm Hg Q-What is Rahimtoulla criteria (rule of 55)? A-Conserve AR if: - Age > 55 years - CTR < 55% - LVH on ECG < 55mm - LVID (S) < 55mm - EF > 50-55% Q-What are the causes of patient of severe AR with a DBP of 30-40 mm Hg? A-May be seen in: - Acute AR - Increased LVEDP - Proximal stenotic lesion (severe MS)- causing vasoconstriction Q-Discuss the comparison of Hills sign with angiographic AR. A- Hills sign Angiographic AR 20- 40 mm Hg Grade II+ AR 40- 60 mm Hg Grade III+ AR > 60 mm Hg Grade IV+ AR
- 84. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 84 Q-What is Coanda effect? A-Described by Henri Coanda (1930). Described as “when a jet stream (of air or water) comes into contact with a curved surface, it will attach itself to it & follow the curve”. OTHER VALVES Q-What tricuspid valve conditions are associated with a large RA? A- 1) TS + TR 2) Atrial fibrillation 3) Mean RAP 12 mm Hg Q-What is the significant gradient, on cath, across the TV? A-A gradient more than 5 mm Hg is significant. Q-What is the normal PV area? A-2 cm2/m2 Q-Discuss classification of PV stenosis. A- Valve area Gradient Peak systolic RV pressure Mild > 1 cm2 < 50 mm Hg < 75 mm Hg Moderate 0.5- 1 cm2 50 –80 mm Hg 75- 100 mm Hg Severe < 0.5 cm2 > 80 mm Hg > 100 mm Hg Q-What is the role of tricuspid annuloplasty in functional TR? A-It has been shown that correcting the MV lesion, without intervention on the TV, is associated in many patients with persistence or worsening of TR in the postoperative period. Hence TV annuloplasty should be contemplated if: - TR is moderate or severe - Annular dilatation is > 21 mm/m2. As in above spontaneous regression in the postoperative period is rare.
- 85. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 85 ECHOCARDIOGRAPHY IN VALVULAR HEART DISEASE MITRAL STENOSIS M Mode: Findings are 1) Due to slow closure of MV in early diastole the EF slope is markedly diminished 2) Diminished mobility causes a reduced DE amplitude 3) Thickened leaflets 4) Anterior movement of PML Discrepancy: - In patients with AS/ AR, with normal MV the EF slope is diminished- hence it is unreliable & obsolete - 20% of patients of MS will not have anterior movement of PML 2 D Echo: is the principle means of evaluating valvular pathology in MS Features are 1) Doming of AML in diastole (due to inability of valve to accommodate all the blood available for delivery into the LV) Doppler: Shows 1) Rate of decrease in diastolic flow after E point 2) Accentuation of ‘A’ wave (absent in atrial fibrillation) 3) Pressure half time (the time required for the peak gradient falls to half) for valve area. MVA= 220/ PHT 4) Valve area by continuity equation A1 x V1= A2 x V2 (A1= AV area, V1= velocity across AV, A2= MV area, V2= velocity across MV) A2= [A1 x V1]/V2 (this is provided there is no AR/MR) MITRAL REGURGITATION (Primarily by color Doppler) M MODE & 2D ECHO: Features are 1) Size of LA 2) Pulsation of LA wall 3) Size of LV 4) AV motion 5) IVS motion patterns 6) Thickening & fibrosis of MV COLOR DOPPLER: 1) Measure jet area of the maximum regurgitant jet & compare as a ratio with area of the LA 2) PISA (Proximal isovelocity surface area)- depends upon principle of flow acceleration proximal to a narrowed or regurgitant orifice.
- 86. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 86 AORTIC STENOSIS M MODE: shows 1) Thickened & immobile leaflets (M Mode for determining valvar pathology, in AS, is no longer done) 2) LV wall thickness 2 D ECHO: 1) Systolic doming (Systolic doming is the most important 2 D Echo finding of any valvar stenosis) DOPPLER 1) Pressure gradient across the AV using modified Bernoulli’s equation 2) AV area by the continuity equation AV area= [LVOT (area) x LVOT (velocity)]/ AS (velocity) 3) Measurement of ejection time AORTIC REGURGITATION M MODE: 1) Fine fluttering of AML 2) Fine fluttering of IVS (no longer performed) 2 D ECHO: 1) Reverse doming of the AML COLOR DOPPLER: 1) Size of jet 2) PISA 3) Rate of decline of the AV regurgitant velocity- diastolic decay. (the rapidity with which the aortic & LV pressures equalize is a function of the severity of AR) Q-What are the types of IVS movement on M mode? A- - Type A into LV during systole – Normal - Type B straightening of IVS in systole - Type C No movement B & C are paradoxical movements Q-How is Qp/ Qs, on echo, calculated? A- Q= Mean velocity x Time x Cross-sectional area
- 87. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 87 Q-What are the uses of TEE? A-Uses are: 1) Intraoperative: a) Off pump- for LV dysfunction b) Area free of plaques for application of cross clamp & side biting clamp c) Checking adequacy of MV/ AV repair procedures d) Completeness of deairing e) Placement of IABP f) During Batista g) TMLR 2) Diagnosis of ASD 3) Balloon guidance during intervention for BAS, dilatation of atrial baffle 4) Diagnosis of clots 5) Dissection 6) Endocarditis 7) Myocardial viability on stress echo 8)Prosthetic valve dysfunction 9) Congenital echo- especially in adults Newer uses 10) Diagnosis of aortic arch plaques as a cause for unexplained stoke 11) Catheter ablation guidance 12) 3-D echo Q-What is LA smoke? A-It is echodensites that are seen due to churning of blood in the dilated LA (due to stagnation; in a patient with MS.) Q-What is the D/D between LA smoke and LA clot? A-The position of the smoke, within the LA, constantly varies. Q-What are the contraindications to TEE? A-They are: 1) Esophageal disease 2) GI bleeding 3) Cervical spine injury
- 88. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 88 VALVULAR SURGERY GENERAL Q-Which procedures may cause injury to the 1st septal artery? A-The following may cause injury to the 1st septal artery. 1) Ross procedure 2) Morrow’s procedure (for hypertrophic subaortic stenosis) 3) Vouhe’s procedure (for hypertrophic subaortic stenosis) 4) Konno Rastan procedure 5) Infundibular resection (septal side) in TOF Q-Which procedures may damage the artery to SA node? A- 1) TCPA 2) Senning 3) Mustard 4) LA roof approach for MVR 5) Atriocavopexy for SV ASD Also in 6) Damage to artery following myocardial infarction 7) Disease of small artery- SLE, PAN Q-In which surgeries is the MPA transected? A- 1) Arterial switch 2) Extracardiac fontan 3) Krutzers modification of Fontan 4) Damus Kay Stansel procedure 5) Ross procedure 6) Anastomosis to left main 7) Norwood procedure Q-In which surgeries is the aorta transected? A- 1) Aneurysm ascending aorta- for replacement 2) Lecompte maneuver 3) Surgery for APVS 4) Arterial switch 5) Ross procedure 6) Takedown of Waterston Cooley shunt
- 89. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 89 Q-Which surgeries can be performed thru’ a left thoracotomy? A- 1) CMC 2) Pericardiectomy 3) MIDCAB 4) Potts operation (historical) 5) Benson Roe procedure (historical) Q-Which surgeries are performed thru’ a posterolateral thoracotomy? A- 1) BT shunt 2) Coarctation/ descending thoracic aortic procedures 3) PDA surgery 4) MVR (rare) Q-What are the current recommendations for adding aspirin to warfarin, in patients with prosthetic valves? A-They are:(Given by JACC, 2001) 1) TEE in a patient with mechanical valve on warfarin 2) Patient with a mechanical valve with risk factor, viz. - h/o TEE - atrial fibrillation - large LA - LA clot - > 1 mechanical prosthesis - CAD - Ball valve Q-What are the rules for choosing a valve size? A- - In the aortic position choose same size as sizer, & - In the mitral position choose one size less. Q-Does AVR for AR have better results than a MVR for MR? A-Yes, AVR for AR has better results because: 1) In MR, LV is pumping into low pressure LA & post MVR it now has to pump into the aorta 2) In MVR, when the valve is excised, a portion of the LV is excised. 3) MR/MS is associated with elevated PAP. Q-What antibiotics are used for ‘antibiotic coated’ sewing rings? A-The are coated with: 1) Minocycline 2) Rifampicin
- 90. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 90 Q-How can the outcome of a maze operation be classified? A-Using the ‘Santacruz score’ (Santacruz is a Hospital in Portugal) 0- Persistant atrial fibrillation 1- Regular with atrial fibrillation 2- Regular with RA contraction 3- Regular with LA contraction 4- Normal sinus rhythm Q-What is the most significant complication of a maze? A-An incision close to a PV may casue PV stenosis. Q-What are the indications for surgery in IE? A-Indications are: Absolute 1) CCF – Moderate/ Severe 2) Uncontrolled infection Relative 1) >10mm vegetation 2) Highly mobile vegetation 3) Embolism 4) Perivalvar extension 5) Continuous fever Q-What is the recommended duration of treatment for IE? A- If blood culture negative – 6 weeks If blood culture positive – post op 6 weeks and then till 3 subsequent blood cultures are negative Q-Describe the characteristics of native valve IE. A-They are: 1) Left> Right, 2) MV>AV 3) Regurgitant> stenotic Q-What is the commonest area of annular involvement in IE? A- 1) Aortic valve annulus - between RCC and LCC (can compress on Lt main) - between RCC and NCC (can cause heart block) 2) Mitral valve annulus – posterior - perivalvar extension is rare in pulmonary and tricuspid valves Q-When was the Medtronic Hall valve 1st implanted? A-In 1977.
- 91. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 91 Q-When was the 1st St. Jude valve implanted? A-In 1977. Q-Who invented pyrolytic carbon? A- Jack Bokros. An engineer, invented pyrolitic carbon for covering uranium pellets. It was tried by Dr. Vincent Gott. Jack Bocros then eliminated the silicone content of pyrotitic carbon & launcehed his own valve in 1996 (the Onnex valve) Q-How to prolong the life of a bioprosthetic valve? A-By: 1) Non glutaraldehyde treatment 2) Reduce BP & heart rate (anti impulse therapy) 3) Immunosupression Q-What are the ‘Ten commandments’ of prosthetic heart valves? A- (By Harken) 1) It must not propagate emboli 2) It must be chemically inert & not damage blood elements 3) It must close promptly (< 0.05 sec) 4) It must offer no resistance to physiologic flow 5) It must remain closed during the appropriate phase of cardiac cycle 6) It must have lasting physical & geometric features 7) It must be inserted in a physiologic site- generally the normal anatomic site 8) It must be capable of permanent fixations 9) It must not annoy the patient 10) It must be technically practical to insert. Q-Who started St. Jude? A-Manual Villafona in 1976. Q-What are the modifications of a St. Jude valve from the Lillehei Kalke valve? A- Lillehei Kalke valve St Jude valve All titanium Pyrolytic carbon Opening angle= 60% Opening angle= 85% Pivot mechanism- small More for systolic & diastolic washing 1st St Jude valve implanted in 1977. Q-What were the clinical trial on the lillehei Kalke valve? A-Used only in one patient who died after 24 hours. Q-Which was the Sutureless valve? A-Magovern Cromie (Ball in cage) valve. High incidence of heart block.
- 92. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 92 Q-Which was the 1st pivoting disc valve? A-The Wada Cutter valve. It was removed from market in 1972 (MV) & 1974 (AV). Q-Which was the 1st Dura mater allograft valve? A-Made by Puig et al, 1971 (Brasil). Q-How was the Medtronic Hall valve devoloped? A-A combination of the designs of Bjork Shiley & Lillehei Kaster gave rise to the Hall Kaster valve, which was later renamed as the Medtronic Hall valve. (Hall: Karl Victor Hall, Norway) Q-Who was St. Jude? A-A jewish saint. Q-What should the orientation of tilting disc valves, in the mitral position? A- Bjork: Greater orifice posteriorly Hall: Greater orifice towards IVS (to prevent possibility of hindrance to disc due to hypertrophied mural side structures.) Q-Who introduced xenografts? A-Jean Paul Binet, Jean Langlois & Alain Carpentier. Q-Who introduced Glutaraldehyde? A- Alain Carpentier. Q-Who coined the term bioprosthesis? A-Alain Carpentier (Biologic origin with Prosthetic fate) Q-Describe the care of biological valve on table? A-The following care should be taken. - do not squeeze - rinse thoroughly with saline - no penicillin antibiotics to be used topically (as it may displace the glutaraldehyde moiety) - keep valve continuously moist Q-What are the causes of early biological valve dysfunction? A-Causes are: 1) Age (children) 2) Pregnancy 3) Hypertension 4) Hyperparathyroidism Q-What is Lew’s disease? A- Degenerative calcific disease of the fibrous skeleton of the heart
- 93. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 93 Q-Who are the candidates for Ross procedure? A- 1) Patient between 10- 50 years age 2) Isolated aortic valve pathology 3) Have endocarditis limited to aortic root 4) Athlete/ young individual. Q-What are the contraindications to the Ross procedure? A- 1) Extremes of age (< 1 yr or > 70 yrs) 2) Marfans 3) PV pathology 4) Depressed LV function 5) Multivalvar disease 6) Rheumatic (as shown by Dr. Sampath Kumar, JHVD 1994) Q-Classify postoperative mediastinitis? A- Type I: presenting within 2 weeks after surgery in the absence of risk factors like 1) obesity 2) diabetes 3) immunosuppressive therapy Type II: presenting within 2- 6 weeks after surgery, in absence of risk factors Type IIIa: Type I in presence of risk factor Type IIIb: Type II in presence of risk factor Type IVa: Type I, II or III after one failed therapeutic trail Type IVb: Type I, II or III after more than one failed therapeutic trail Type V: presenting more than 6 weeks after surgery Q-What are the types of LV rupture? A-Treasures classification Type I: In the AV groove. Seen in - resection of the MV annulus during MVR - use of a large size prosthesis Type II: Base of papillary muscle. Seen in - resection of papillary muscle - decalcification - due to strut of bioprosthetic valves - deairing post MVR - adhesiolysis - site/ extension of LV vent Type III: In between above two. Seen in as Type II
- 94. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 94 Q-What is the prognosis of LV rupture? A-If intraoperative diagnosis- 50% mortality If post operative diagnosis- 100% mortality Type I mortality > Type II/ III Q-Discuss anti-thrombotic treatment post prosthetic heart valve replacement. A-(JACC 1998 recommendations) by McAnulty, Rahimtoola Warfarin (INR 2-3) Warfarin (INR 2.5-3.5) Aspirin (80-100 mg) Mechanical prosthetic valves A.First 3 months after replacement B.After 3 months 1) Aortic valve 2) Aortic valve + risk factor 3) Mitral valve 4) Mitral valve + risk factor Biological prosthetic valves A.First 3 months after replacement B.After 3 months 1) Aortic valve 2) Aortic valve + risk factor 3) Mitral valve 4) Mitral valve + risk factor + + + + + + + + + + + + + + + + + risk factor: are - atrial fibrillation - LV dysfunction - previous thromboembolism - hypercoagulable conditions INR should be maintained between 2.5 & 3.5 for aortic disk valves & Starr Edward valves. INR between 2.0- 3.0 applicable only for bileaflet valves & Medtronic Hall valves.
- 95. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 95 Q-Discuss antithrombotic therapy in patients requiring other procedures. A-Antithrombotic therapy in patients requiring non-cardiac surgery/ dental care Usual approach If patient on warfarin If patient on aspirin -stop 72 hrs before procedure -restart in afternoon on the day of procedure or after control of active bleeding -stop 1 week prior to procedure restart the day after procedure or after control of active bleeding Unusual circumstances 1.Very high risk of thrombosis if off warfarin 2.Surgery complicated by postoperative bleeding 3.very low risk for bleeding -stop warfarin 72 hours prior to procedure -start heparin when INR falls below 2 -stop heparin 6 hours prior to procedure -restart heparin within 24 h of procedure & continue until warfarin can be started & INR 2 -start heparin as soon after surgery as deemed safe & maintain PTT as 55- 7- secs until warfarin restarted & INR 2 -continue antithrombotic therapy Clinical judgement. Consider this approach if recent thromboembolism, Bjork Shiley valve or 3 risk factors (viz: atrial fibrillation, LV dysfunction, previous thromboembolism, hypercoagulable conditions & mechanical prosthesis). One risk factor is sufficient to consider heparin in patients with mechanical valve in mitral position. Heparin can be administered in outpatient’s basis before & after surgery Eg. Local skin surgery, teeth cleaning, treatment of caries. Q-What is the survival post valve replacement? A-Survival rates are better for AVR than for MVR/ DVR. 10 year survival, in general, for AVR = 65% MVR= 55% DVR= 55% -Late mortality is higher for regurgitant lesions. -Late mortality is higher for rheumatic/ ischemic valve replacement in comparison with degenerative diseases. Q-What is the mortality distribution post valve replacement? A-It is as follows (From “surgery for valves- late outcomes”-Peter Groves, Heart 2002) 60%- due to cardiac, non valve surgery related (CCF, myocardial infarction, arrhythmias) 20%- due to valve related 20%- due to non cardiac causes
- 96. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 96 Q-What are the predictors of mortality post valve replacement? A-Predictors of mortality are: 1) Age > 65 years 2) LV dysfunction 3) NYHA 4 at time of surgery 4) Coronary artery disease 5) Ventricular arrhythmias Q-Discuss ‘sudden death’ post valve replacement. A-Sudden death is defined as death within 1 hour of an event of abrupt onset & accounts for around 25% of all late deaths following valve replacements. There are 3 categories of sudden death: 1) Natural disease process: ventricular arrhythmias (AVR > MVR) 2) Related to prosthesis: Thrombosis, TEE, IE, leak, mechanical failure 3) Management failure: IC bleed due to elevated INR Q-What are the changes in PH post valve replacement? A-The most dramatic regressive changes in PH occur within the first few days after surgery & are generally complete 6 months postoperatively. Full normalization is rarely achieved. Even if the PAP’s are normal at rest, an increase with exertion will be seen suggesting residual irreversible changes. This leads to a chronic increase in afterload. Q-What are the guidelines for FU after valve surgery? A-AHA/ACC guidelines 1998 1st FU: should be clinical, ECG & X ray. Also an echo examination for documenting prosthesis function, ventricular function & PH- for future reference. Q-Which conditions are associated with ‘suboptimal’ surgical results after valve replacement? A-The results of valve replacement are suboptimal if: In AR: 1) NYHA IV symptoms 2) ESD > 55 mm In MR 1) LVESD > 45 mm Q-What are the echo predictors of ‘good outcome’ of valve surgery in AR & MR? A-They are: ESD (in mm) EF (%) FS AR 55 55 > .27 MR 45 mm 60 > .32
- 97. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 97 Q-What are the ways of in vitro testing of prosthetic valves? A-3 test systems used are: 1) Pulsatile flow (pulse duplicator) 2) Steady flow 3) Durability (accelerated wear testing) Davila introduced the design of pulse duplicator system. Gorlin introduced the “Gorlins index” for EOA in vitro. Frater introduced ‘Performance index’= EOA/ mounting diameter Superpump is a programmable & computer controlled analysis pulse duplicator system. CMC, OMC & MVR Q-Describe a brief history of mitral valve surgery? A- - Elliot Cuttler- tenotomy knife to cut the AML - Henry Souttar- first digital palpation of MV (with pt. Having symptomatic improvement) - CP Bailey- introduced a curved knife to be entered thru’ the LAA for cutting the commissures of MV - Brock- Digital fracture of commissures - Dubost- transatrial dilators - Logan & Turner- Transventricular dilators - Modification of TV dilators by- Beck, Glenn, PK Sen, Cooley, Tubbs (Tubbs introduced screws for adjustment of opening diameter) - OMC- CW Lillehei - Series of OMC- Kay et all. - MVR (mechanical valve)- Albert Starr (21st Sept, 1960) - MVR (homograft)- Senning in 1965 - MVR (bioprosthetic)- Carpentier Q-What are the specific features of anesthesia in a patient with MS? A-While administering in a patient with MS: - avoid fluid overload - avoid tachycardia. Q-What is the orientation of dilator during CMC? A- - Colley- perpendicular to the commissures - Logan- any direction Q-What was the incision taken during the first CMC? A-A ‘C’ shaped incision over the anterior chest wall
- 98. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 98 Q-If there is a confusion of 4th or 5th space during CMC, which space is preferred? A-The 5th space is preffered, as the crucial part is lifting of the LV apex. Q-When, during CMC, is the approach posterior to the phrenic nerve? A-When it is: - a posterolateral throractomy approach - redo CMC Q-What measures are to be taken if, during CMC, the LV apex pursestring tears? A-Keep finger on the tear, and attempt pursestring ↓ Pass a foley’s/ fogarty catheter into the LV and hitch it up against the tear ↓ Fibrillate the heart & suture ↓ CPB (complete or left heart only) Q-What are the outcomes of CMC in pregnancy? A-Ueland, Am J Obst Gynecol 1975 514 patients with maternal mortality= 2%, fetal mortality= 8.5% Q-Why post CMC is an open mitral commisurotomy (open heart) preferred than reCMC? A-Because: 1) Difficulty in access- no LAA, ahdsesion 2) Severe subvalve fusion (however post CMC reCMC has been a common practice & hence can be debated) Q-Where does the IAS open during opening of the LA? A-It opens at the inferior end of incision (here the IAS turns posteriorly and to the right). Q-What are the various approaches to the MV? A-The following are the approaches for the MV. 1) Paraseptal 2) Hitch pericardium after freeing SVC- Rogue 3) Freeing of Waterstons groove- Larbalestier 4) Trans RA septum- Brawley 5) Trans RA-LA (vertical incision)- Dubost 6) Retract SVC/ disconnect SVC & extend incision upwards into superior LA- Seale 7) Thru’ roof of LA- Saxena & Meyer 8) Thru’ LAA 9) Thru’ aorta- M Yacoub 10) Thru’ LV apex- Batista
- 99. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 99 Q-What instruments can be used to retract the LA? A- 1) Cooley’s retractor 2) Two right angle 3) Carpentier self retaining 4) Bhattacharya retractor 5) Bhate’s retractor 6) Neelakandan retractor Q-Does the technique of suturing affect the chances of paravalvular leak? A-Yes. The continous technique is reported to have a higher incidence of paravalvular leak. (Kirklin Ann Thorac Surg 1983.) Q-Why a MV bioprosthesis degenerates faster than AV prosthesis? A-Due to: 1) Higher pressure for closure 2) Faster closure 3) Atrial fibrillation (?) Q-What are the problems of a large LA after completing CPB? A-The problems are: 1) Deairing 2) Higher chances of thromboembolism 3) Weaning from ventilator 4) Post-operative low CoP 5) Persistence of atrial fibrillation Q-Why is valve excision started at the 12oclock position (in AML) during MVR? A-The reasons are: 1) It is the most accessible area 2) It is a safe area 3) No subvalvar structure behind it 4) This area is rarely affected by calcification 5) Provides an opportunity to protect the PML Q-What are the problem of a high profile valve in the mitral position? A- 1) LVOT obstruction 2) Hemolysis 3) Increased thromboembolism Q-Describe the intraoperative grading of commissural fusion. A- Grade I- partially fused Grade II- completely fused but fissure identified Grade III- densely fused with no delineation
- 100. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 100 Q-Who first advocated PML preservation? A-Lillehei (he plicated the PML first and then used it as a neoannulus during the MVR) Q-What are the techniques of leaflet preservation? A- 1) PML tucking- Lillehei 2) AML & PML plication- Hertzer 3) AML bulk excision- Rose 4) Splitting of the AML/PML in center- Miki 5) Splitting of the AML according to chordae & then suture that segment to the respective site on the annulus- Khonsari (modified technique: Khonsari II) Q-What are the advantages of a built in holder? A-The advantages are: 1) No chance of inserting a valve upside down 2) No damage to disc Q-What are the possibilities if post MVR a patient not coming off bypass? A-Possibilities are: 1) Poor myocardial protection- ischemia 2) Conduction block 3) Prosthesis dysfunction/ left circumflex artery injury Q-What advice should be offered, for pregnancy, post MVR? A-(It depends upon preoperative PH and LV dysfunction) If no PH/ Normal LV- can become pregnant but is advised 6- 12 months after surgery. If PH+/ LV dysfunction present: wait for 6-12 mnths & then repeat echo & advice. Q-What is the advice on ‘family planning’ post MVR? A-Avoid: 1) OCP 2) IUCD- due to increased chance of infective endocarditis/ bleeding Q-Why, in a postCMC patient, is the adhesiolysis first is started on the aorta? A-Because: 1) Aorta is posteriorly placed hence less chance of trauma 2) It is thick & easily palpable Q-Why is a normothermic release of adhesions preferred? A-For: 1) Better myocardial preservation 2) If AR is present- distension is avoided (which would result from cooling)
- 101. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 101 Q-What are the advantages of adhesiolysis? A-The advantages are: 1) Better exposure of the MV 2) Easy of checking MV competence, post OMC/ repair, from LV apex 3) Deairing 4) Defibrillating 5) Pour ice slush around the heart Q-Describe the extent of adhesiolysis? A-Adhesiolysis should be performed till beyond the AV groove. If the adhesions are not removed there will be a cephalad deviation of the mitral valve (making MV difficult to visualize). ANNULOPLASTY RINGS Q-What are the advantages of annuloplasty rings? A-The advantages are: 1) Retain shape & size of annulus 2) Keeps tension of suture lines 3) Increases leaflet coaptation 4) Prevents recurrent dilatation of annulus Q-What are the types of annuloplasty rings? A-Mainly of 2 types- rigid & flexible. (Rigid rings have been shown to interfere with the LV filling & functioning of the anterolateral segment) Ring Incomplete Complete Carpentier Edward (Baxter) Original stainless steel- now Titanium CE Physio ring Titanium + velour Dacron Size-22 to 36 (transverse diameter), 26= 3 cm2 area, 28= 4 cm2 area Duran (Medtronic) Complete flexible. Titanium core with silicone felt. Has 3 marks for reference. Seguin (St. Jude) Semiflexible with anteroposterior angulation Tailor (St. Jude) Complete flexible ring. Silicone with barium Cosgrove (Baxter) ‘C’ shaped ring, with no support for the anterior annulus Annuloflex (Sulzer Carbomedics) Complete flexible Homemade Stainless steel wire # Endoscopic placement Autologous pericardium over a titanium platform
- 102. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 102 #A No.1 stainless steel wire with 4 mm PTFE tube graft. 11 cm of this wound around a 3 cm diameter cylinder & tied- to achieve a 10 cm circumference. Post operatively 6 weeks warfarin treatment is recommended. Q-What is the concept of an ‘incomplete ring’? A-The concept is based on the fact that it is only the mural annulus that dilates & hence needs to be restored back in shape. Q-What is the concept of circular semiflexible ring? A- Anterior portion is rigid- as no change occurs in the transverse diameter during cardiac cycle Posterior portion is flexible- allows increase & decrease of the anteroposterior diameter AVR Q-What is Frater’s stitch? A-A stitch taken thru’ the center (corpora arentii) of all the 3 cusps of the AV & held up together- to determine which leaflet is redundant (used when an AV repair is planned for AR.) Q-What is the difference between an aortic & a pulmonary valvotomy? A- - In Aortic valvotomy- err on side of AS (as AR poorly tolerated) & - In Pulmonary valvotomy- err on the side of PR (as PR is well tolerated) Q-Where is the greater orifice oriented in an AVR? A- - Towards the greater curvature of aorta (advocated by Kleines)- it offers least gradient as the maximum flow is at the greater curvature & higher cerebral flow is also seen - Towards the RCC (advocated by Antunes)- maximum flow to coronaries obtained. HOMOGRAFT Q-Which is the largest homograft bank in the world? A-Cryolife, USA. Q-What factors determine the clinical results of homografts? A-The factors are: 1) Tissue viability 2) Recipient & donor age O’Brien series (JHVD 2001) showed that structural valve deterioration was;
- 103. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 103 - 47% at 15 years for those < 20 years age & - 81% at 15 years for those between 40 to 60 years of age 3) Immune response 4) Valve sizing Yankah’s series (EJCTS 2001) showed that freedom from explantation was - 48% at 15 years for undersized valves & - 92% at 15 years for oversized valves. A homograft valve of ID 3mm less than recipient should be considered as undersized 5) Implantation technique Freedom from reoperation is - 80% at 15 years for root replacement & - 72% at 15 years for subcoronary implantation Q-What is the critical period for homografts? A-5 years post implantation. Q-Who introduced homograft arterial conduits & what are they used for? A-Dubost in 1952. Present indications are: 1) Treating infected synthetic grafts of thoracic/abdominal aorta 2) Mycotic thoracic aortic aneurysm Q-What are the techniques of sterilizing a valve, for use as homograft? A-The techniques are using: 1) Viable cryopresrvation- dipping in cell culture medium, incubation in antibiotic, cryoprotectant (antifreeze) treatment & cryopreservation Historical techniques are: 2) Formaldehyde 3) Ethylene oxide 4) Chlorhexidine 5) Gamma irradiation 6) Freeze dry to -70C Q-How is viability of homograft studied? A-Viability is studied by: 1) Tritiated proline uptake for fibroblasts 2) Electron microscopy
- 104. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 104 CONGENITALACYANOTIC HEART DISEASE GENERAL Q-What are the pressures, in cardiac chambers, prior to birth? A-Pressures are (roughly, in mm Hg): RA= 10 RV=60/10 PA= 60/40 LA= 10 LV= 60/10 Aorta= 60/40 Q-What are the normal changes in PVR after birth? A-Normally the PVR drops to near normal by 2-3 weeks, after birth. However in infants with left to right shunts, it may take 6- 10 weeks to drop. In preterm babies with left to right shunt, it takes 3- 6 weeks to fall (and in these babies as the PVR regresses, CCF supervenes). Q-What is a specific feature of murmur at birth? A-The murmur of left to right shunts manifest only after regression of PH. While obstructive & regurgitant murmurs are present at birth. Q-What are the criteria for labeling a child has having heart disease? A-Nadas criteria. They are: Major Minor Systolic murmur Grade III Systolic murmur < Grade III Diastolic murmur (any grade) Abnormal BP Cyanosis Abnormal S2 CCF Abnormal X Ray Abnormal ECG The presence of 1 major or 2 minor criteria indicate the presence of a heart disease Q-What are the non-cardiac causes of CCF in child? A-They are: 1) Hypoxia 2) Hypoglycemia 3) Hypocalcemia 4) Anemia (generally precipitates CCF) Q-What are the causes of LRTI in patients with left to right shunt? A-Reasons are: 1) Increased blood flow, hence increased mucus production leading to mucus retention & subsequent infection 2) Increased flow leading to tissue edema & lymphatic stagnation
- 105. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 105 Q-What are the symptoms of increased PBF in children? A-The symptoms are: 1) Failure to thrive 2) Repeated RTI 3) Refusal for feeds 4) Suck-rest-suck cycle 5) Sweating of forehead 6) Pounding of chest noted by parents. All the above are to be considered class IV symptoms. (NYHA not applicable before 2 years) Q-What are the features of increased pulmonary blood flow? A-The features are: On Examination: - Precordial bulge - Harrison’s sulcus - LV apex - Prominent PA On ECG: - LVVO On X-ray: - Pulmonary plethora Q-What are the criterion to label a child as ‘Failure to thrive’? A-Criteria are: - Weight below 3rd percentile - < 80% of ideal weight Q-What are the signs of significant shunt, i.e., Qp/Qs >1.5/1? A-Signs are: 1) Bounding pulsations 2) hyperdynamic apex 3) Flow murmur across the MV Q-What is to be considered as ‘significant RTI’? A-> 5-episodes/ year diagnosed radiologically & requiring treatment. Q-What defines a shunt? A-A shunt is determined by: 1) Pressure difference 2) Resistance difference 3) Size of defect 4) Associated intracardiac anomalies
- 106. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 106 Q-What are the problems of a left to right shunt? A-The problems are: 1) RVVO & LVVO (leading to failure & arrhythmias) 2) Pulmonary hypertension 3) Regurgitant lesions. Q-Why is growth retarded in a left to right shunt? A-Due to: - Repeated RTI- increased catabolism - Decreased systemic output. Q-In left to right shunt, why is the PAP elevated? A-Due to: 1) Increased flow 2) Increased resistance 3) Size of defect (direct transmission) Q-What is a ‘restricted’ shunt? A-When there is a gradient across the defect in all phases of the cardiac cycle. Q-Age of onset of CCF as a clue to pathology? A-As follows: 1) < 3 days - HLHS - Severe AS/ aortic atresia - Mitral atresia 2) < 1 week - HLHS - TGA - Large VSD - Coarctation 3) < 4 weeks - TGA - Coarctation - Myocarditis - AV canal - Large PDA 4) 1-2 months - VSD - PDA - AV canal - TGA - TAPVC 5) 2- 6 months - TGA - VSD
- 107. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 107 - PDA - AV canal - Truncus - TAPVC - ALCAPA Q-What are the possible cardiac pathologies in an acyanotic newborn child who is having feeding distress? A-Possible cardiac pathologies could be: - Coarctation - PDA - Vascular rings - Large VSD - Left sided valvular lesions. Q-What are the congenital causes leading to pulmonary venous obstruction? A-They are: 1) Congenital MS 2) Cor triatriatum with PV obstruction 3) TAPVC 4) HLHS 5) Congenital AS/ coarctation aorta Q-What is a Rasmussen’s aneurysm? A-It is an aneurysm of the PA secondary to tuberculosis. Q-Ennumerate congenital heart diseases associated with absent MPA segment on X-Ray? A-An absent MPA segment, on X-ray, may be seen in: 1) Infundibular PS 2) Anteroposterior relation of great vessels 3) Pulmonary atresia Q-Which congenital heart diseases are associated with a large aorta (prominent aortic knuckle on X-Ray)? A-A large aorta maybe seen in: 1) PDA & AP window 2) TOF 3) Valvar AS 4) Coarctation (due to hypertension) Q-What is the time taken for permanent changes to occur, in the pulmonary vasculature, due to PAH? A-The time duration (on an average) is: In VSD 2 years In Large PDA 2 years In Large ASD > 30 years
- 108. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 108 [Note: Rarely an ASD may cause severe problems in infants. In these conditions an associated PV obstruction should always be ruled out.] Q-How to determine the situs? A-Situs may be ascertained by: 1) Clinically - Liver dullness on right side - Fundic bubble on left sie - Left testes is lower 2) X-ray - Trachea is to the left - Liver & fundic bubble - Brochial anatomy - Splenic flexure is to the left 3) Echo- - Crista terminalis for RA- on right sie - Rt. sided SVC/ IVC [Note: Generally abdominal situs is concordant with atrial situs] Q-Bimodal presentation is seen in which cardiac conditions? A-The conditions are: 1) Ebstein’s anomaly 2) ASD 3) Coarctation aorta 4) Pulmonary stenosis Reasons for bimodal presentations are: Ebsteins- child born with increased PVR & hypoplastic RV cyanosis. Later the PVR falls improvement in cyanosis. 3rd or 4th decade the RV fails recurrence of symptoms. ASD- 10% are symptomatic in infancy that later resolves only to become resymtomatic later. Coarctation- CCF in 1st month of life. Q-Which conditions are associated with LV dominance? A-The conditions are: 1) Tricuspid atresia 2) PA with intact IVS 3) Single ventricle 4) AV canal unbalanced to the left 5) Ebstein’s anomaly Q-Which condition has shunt at more than one level? A-AV canal.
- 109. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 109 Q-What are the causes of chest pain in children? A-Chest pain, in children, maybe seen in: 1) ALCAPA 2) Congenital AS 3) Pericarditis Q-What are the D/D of a right parasternal murmur? A-The following are associated with a right parasternal murmur. - Coronary AV fistula - Flow murmur across TV - RASOV into RA/ RV - Pulmonary AVF - Distal RPA stenosis - RCA-RA fistula D/D between the above pathologies: RASOV into RA/ RV: - Raised JVP - Wide pulse pressure - RHB+ - RV heave + Pulmonary AVF: - will have cyanosis Distal RPA stenosis: - will have loud systolic murmur & a soft diastolic murmur. Q-Which are the conditions known for suprasystemic PH? A-Conditions are: 1) PPH 2) ASD 3) MS Q-What conditions are known for suprasystemic RV pressure? A-Conditions are: 1) PPH 2) ASD 3) MS 4) Isolated severe PS Q-Which cardiac pathologies can cause stridor? A-Stridor maybe seen in: - APVS - Vascular rings - Arch aneurysm
- 110. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 110 Q-Which condition is associated with increased PAP with normal PVR/ decreased PVR? A-Peripheral pulmonary artery stenosis. Q-Define Hypertelorism? A-A defect of the anterior portion of the cranium characterized by overgrowth of the greater wing & undergrowth of the lesser wing of sphenoid. Diagnosis: Clinical- Increase in the interpupillary distance (> 42 mm) X-Ray- Distance between the 2 eyeball sockets is more than the diameter of any one eyeball. Seen commonly in: - Down’s syndrome - Noonan’s - DiGeorge’s syndrome. Q-What are the causes of ‘non surgical Heart block’ in children? A-Spontaneous heart blocks are common in: - c TGA - common AV canal Q-What are the various X-Ray patterns of Pulmonary hypertension? A-They are: - Cephalization: if post capillary PH (Eg. MS) - Centralization: if pre capillary PH - Lateralization: Westermark’s sign Q-What is Westermark’s sign? A-If due to unilateral pulmonary embolism, the ipsilateral PA is occluded, there will be oligemia on one side & increased vascularity of the other. Q-What is the X-ray differentiation between ASD, VSD & PDA? A-The conditions can be differentiated depending upon the MPA, LA & ascending aortic segments on X-Ray. MPA LA Aorta ASD + - - VSD + + - PDA + + + Q-Which conditions have left to right shunt at one level & right to left shunt at the other? A-Conditions are: 1) HLHS/ aortic atresia: L-R at ASD and R-L at PDA 2) AP window with PDA in a c/o aortic interruption
- 111. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 111 Q-What is the surgical risk in relation to PVR & SVR? A-Normal SVR=15-20 Woods & normal PVR=1-2 Woods Depending upon the PVR/ SVR ratio the risk may be determined - < 0.25 - normal - 0.25- 0.5 - mild risk - 0.5- 0.75 - moderate risk - > 0.75 - high risk - > 1 - contraindication for surgery Q-What are the types of congenital MS? A-It depends upon the level of obstruction. It could be at following levels: 1) Supravalvar: Supravalvar ring (D/D with cor triatriatum sinister) 2) Level of MV annulus & leaflets: double orifice MV 3) Level of chordea & papillary muscles: - Funnel valve - Parachute valve - Hammock valve Q-What are the components of Shone’s complex? A-It was described in 1963 & includes a constellation of 1) Supramitral ring 2) Parachute MV 3) Subaortic obstruction 4) Coarctation aorta [Note-Bolling’s postulate: The MS causes an increased PAP leading to paradoxical movement of IVS into LV, leading to LVOT obstruction.] Q-Describe ECG characteristics of important CHD’s? A- Common AV canal: 1) Prolonged PR interval 2) Axis- Left & up or indeterminate 3) Counterclockwise loop Primum ASD/ common atrium: 1) Axis- left & up or indeterminate 2) Counterclockwise loop c-TGA 1) q in right sided leads-I, AvR, V1, V4R Sinus venosus ASD-SVC type 1) Coronary sinus rhythm- p in II, III & AvF is inverted & upright in I. Q-What is the ideal age for a fetal echo? A-At 18 weeks gestation.
- 112. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 112 Q-In which conditions are all heart chambers dilated? A-The conditions are: 1) Common AV canal 2) Garbodie defect 3) RASOV into RA Q-Details about Congenital rubella syndrome? A- Caused by Toga virus. Effects mothers thru’ droplet infection Clinically characterized by fever- followed by lymphadenopathy- followed by generalized rash, starting from face. Risk of fetal infection are; During the 1st trimester- 100% During the 2nd trimester, 1st half- 40% During the 2nd trimester, 2nd half & the 3rd trimester- 0%. Features in fetus are: - General- IUFD, IUGR. - Ocular- retinopathy, cataract - Auditory- nerve deafness - CVS- PDA (in 30%), hypoplastic PA’s, valvar & supravalvar PS, branched PA stenosis, myocarditis, TOF, ASD, VSD, AS. Next baby will be immunized as mother is immunized. ASD Q-What is the natural history of ASD? A-It is as follows: < 3mm defects: mostly close by 18 months (they are mostly PFO's) 3- 5mm & 5- 8mm defects: 80% of the defects shall close (by 8 years) > 8 mm defects: have little chances of closing spontaneously The survival pattern is lesser than normal. ¼ die by 27 years ½ die by 36 years Q-What is the % distribution of various ASD’s? A-It is as follows: Os secundum= 75% Os primum= 15% Sinus venosus= 10%
- 113. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 113 Q-What are the commonest associated anomalies in ASD? A-They are: In Os secundum= MV prolapse In Os primum= MR In sinus venosus= PAPVC Q-Why in an ASD is the PA more prominent as compared to a VSD? A-In an ASD, the PVR is ‘lesser’ elevated in comparison to VSD. Post birth the PVR regresses & hence the PA thins out & becomes more susceptible to dilatation. In VSD/ PDA, the pulmonar artery wall thickness remains the same as the PVR regresses slowly & partially, hence resulting in a less complaint artery. Q-What is the natural history of ASD? A-PVR starts increasing significantly by the 3rd to 4th decade. Average life span is 50 years with an eventual death due to RV failure (Craigh- Natural history of ASD, Circulation 1968). Q-ASD on clinical examination but echo shows intact IAS- what are the possibilities? A-The possibilities are: 1) PAPVC with intact IAS 2) Fenestrated ASD 3) Sinus venosus ASD Q-Enumerate the causes of MR in ASD? A-The causes are: 1) Paradoxical IVS motion-papillary muscle dysfunction 2) Venturie effect 3) As a part of Lutembachers syndrome 4) Primum ASD Q-What are the chief complications of an ASD? A-They are: 1) Eisemengerization 2) Paradoxical embolism 3) Arrhythmias Q-When to label an interatrial defect as a PFO? A-When it is at the classical site & size is less than 3- 5mm diameter. Q-What is the significance of PFO? A-They significance is for: 1) Paradoxical embolism during pregnancy (& other DVT's) 2) Deep sea divers during decompression (embolism)
- 114. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 114 Q-What are the characteristics of familial ASD? A-They are: 1) Male= female 2) Associated with prolonged PR 3) Sudden death known Q-What are the signs of significant shunt across an ASD? A-They are: 1) If diastolic murmur across the TV- Qp/Qs > 1.5-2/ 1 2) Severity of PH is not on loudness of P2 but on the A2-P2 interval & absence of murmur across the TV Q-Which condition are characterized by the presence of a small ASD with assocaited high Qp/ Qs? A-It is seen in: 1) Sinus venosus ASD 2) PAPVC Q-Enumerate conditions characterized by cyanosis, in a patient with an ASD? A-Cyanosis in a patient with ASD may be seen in the following conditions: 1) Eisenmengerization 2) RV failure 3) Selective drainage of IVC into LA 4) Common atrium 5) TAPVC Q-In which ASD the shunt will never be R-L? A-Lutembachers. Q-How to differentiate clinically between a secundum ASD & a primum ASD? A-Primum ASD is characterized by: 1) Early age of onset of symptoms 2) Rapid progression of symptoms 3) Early onset of complications of ASD & LVF 4) Associated MR. Q-What are the clinical D/D of ASD? A-They are: 1) PAPVC with intact IAS 2) TAPVC with anemia Q-What are the ECG features of PH in an ASD? A-They are: - Tall R’ in V1 - qR in V1
- 115. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 115 Q-What is contrast echo? A-Agitated saline is injected into the antecubital vein that reaches the RA & is seen as an echo contrast. If an ASD is present, jet of blood from LA (due to left to right shunt) shall cast a negative shadow in this echobrightness of agitated saline. [Note:If injected thru’ the left basilic vein, a simultaneous diagnosis of a left SVC may also be obtained.] Q-Which is the best view to visualize ASD on echo? A-The subcostal view. Q-If which conditions are surgery not advised for an ASD? A-If 1) Qp/ Qs < 1.5/1 2) Eisenmengerization 3) Age of > 40 years (?) Q-What are the indication of cardiac cath in ASD? A-The indications are: 1) For operability 2) R/o associated coronary artery disease 3) Device closure Q-Why, in an ASD, is the shunt left to right? A-Due to: 1) RA is more complaint than LA 2) TV is larger than MV 3) RV is the volume loading ventricle Q-What are the causes of a ‘large aorta’ in a patient with an ASD? A-Possible conditions are: 1) Systemic hypertension 2) PDA 3) Associated AV disease Q-Which patients of ASD have a CTR > 65%? A-The possible reasons are: 1) Common atrium 2) AV canal 3) TAPVC 4) ASD with MS 5) CCF (4th/ 5th decade)
- 116. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 116 Q-What is the optimum timing of surgery in a person with ASD? A-It is preferred to wait till 3- 4 years of age. Surgery advised if: - Qp/ Qs> 1.5-2/1 - PVR should be less than 8 Wood/m2. Q-Can ASD surgery be performed thru’ a left thoracotomy? A-Yes, but only under circulatory arrest (as bicaval cannulation cannot be performed) Q-What is the name of the right thoracotomy incision, for ASD closure? A-Brom’s incision. Q-Why is midsternotomy preferred for ASD closure? A-Because of: 1) Familiarity 2) Easier to cross clamp & de air 3) Easier to manage surprises- Eg. Lt. SVC, MS/MR, TAPVC Q-What is a McGoon’s stitch? A-A ‘W’ horizontal mattress stitch, which is taken at the inferior angle of the ASD margin, to include a bite of the LA wall. It is taken as: - To ensure that the IVC drains into the RA - Inferior margin is thin walled. Q-Ennumerate historical techniques of closure of ASD? A-They are: 1) Well technique- Gross. 2) Button technique 3) Baileys atriocavopexy (Donut technique) 4) Pursestring technique (Sondergard) 5) Inflow occlusion. Q-How is the inflow occlusion technique performed? A-The steps are as follows: - SVC & IVC are looped - Patient is cooled to 34C - 100% oxygen & NaHCO3 is administered. - SVC/ IVC is clamped - 2-4 beats to allow the heart to empty - Aorta & MPA clamped - RA opened & ASD sutured - RA incision side clamped - SVC/IVC snuggers are released & deairing done thru’ aorta - MPA & then aorta declamped - RA incision sutured
- 117. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 117 Q-What happens to the S2 split after ASD closure? A-A wide split (due to RBBB) will persist but the fixed component disappears. Q-What are the possibilities if on opening no ASD is found? A-The possibilities to be considered are: PA soft straight back syndrome, pectus escavatum PA tense, RA dark PPH PA tense & RA pink PAPVC with intact IAS Q-In which procedures is the ASD extended? A-In, 1) MV surgery thru’ IAS 2) PAPVC with intact IAS 3) Senning’s surgery Q-What are the various materials used for ASD closure? A-They are: 1) DVD 2) Pericardium 3) PTFE 4) Direct 5) RA appendage 6) Raw silk (Solomon Victor) 7) Fascia lata Q-What is the historical importance of fascia lata? A-It was used for: 1) ASD closure 2) Manufacturing tissue valve (By Senning) Q-Is there any criteria for direct ASD closure? A-Yes. After a direct ASD closure the LA size should not get compromised. Q-What are the advantages & disadvantages of various materials used for closure of ASD? A-They are: DACRON Advantage- 1) Good handling characteristics 2) Early shunting across the patch allows the left sided chambers to adapt Disadvantage- 1) Hemolysis (if MR) 2) Clot formation on the LA side.
- 118. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 118 TREATED PERICARDIUM Advantage- 1) Good handling characteristics 2) Low chances of IE. UNTREATED PERICARDIUM Advantage- 1) As it is a live patch, higher in-growth implantation 2) Live endothelium is antithrombotic Disadvantage- 1) Handling characteristic (?) Q-Where Glutaraldehyde be obtained from in the operation theatre? A-From: - Cidex - Storing solution of bioprosthetic valves Q-In ASD closure which is the site of maximum patch giveaway? A-It is at the inferior margin, as the IAS is extremely thin here. Thus the IAS should be incised till the atrial wall. If not incised, the sutures should be taken going thru’ the RA- LA junction into the LA wall. Q-When is Dacron not used? A-In 1) ASD with MR 2) Primum ASD 3) MSD with MVR performed Q-Measures taken for an ASD operated not coming off bypass? A- Check- potassium, acidosis, temperature. Check for: 1) Poor myocardial protection- Treatment-secondary cardioplegia 2) Heart block. Treatment-pacing 3) Mixed/ poor pathology; - MV disease. Treatment- do needful - LV small. Treatment- ionotropes, fenestration Q-Prior to cannulation, in a c/o ASD, what structures can be palpated thru’ the RA wall? A-The following may be palpated: 1) TV- for TR 2) ASD- margin, size, strands 3) Coronary sinus 4) MR 5) PV’s.
- 119. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 119 LEFT SVC Q-How to clinically diagnose drainage of a left SVC into LA? A-By 1) MDM across MV 2) Soft P2 Q-What is coronary sinus rhythm? A-It maybe seen in patients with left SVC or SVC type sinus venosus ASD. Here the SA node is activated & the impulse propagates retrogradely. Hence the ‘p’ axis is leftward. Q-In which conditions is left SVC commonly seen? A-The incidence of left SVC is higher in: 1) Single ventricle 2) AV canal 3) Tricuspid atresia 4) TOF Q-What is the importance of left SVC? A-The importance lies in the following situations: 1) For a bilateral Glenn shunt 2) During a left BTS, it shall come in the way 3) Transvenous pacing from the left side will be impossible 4) Cannulation/ occlusion during CPB. 5) For retrograde cardioplegia. Q-What is the D/D of left SVC on table? A-It may be confused for the left superior PV. Q-What is a Ragib’s defect? A-A condition wherein the left SVC opens into the LA thru’ multiple openings & the coronary sinus is absent (due to absence of the roof of the coronary sinus.) VSD Q-What is the normal distribution of various types of VSD’s? A-It is as follows: Membranous= 70% Muscular= 20% Subarterial= 5% Inlet=5% Q-In which condition is a pansystolic murmur absent in a c/o VSD without PH? A-A small muscular VSD may present with an ‘ejection’ systolic murmur (wherein the defect is occluded by the contracting myocardium).
- 120. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 120 Q-Why, in a large VSD, initially there is only LVVO & no RVVO? A-With a moderate or large VSD, when the LV contracts, it pushes the blood across the VSD straight into the PA (as the RV is also contracting). The RV hence acts like a conduit. In diastole, the excess volume reaches LV from the LA leading to LVVO, while the RV receives normal volume form the RA. Q-What is the natural history of VSD closure? A-Spontaneous closure is seen in 25- 40%. 90% of those determined to close shall close by 10 years. [Note: Why 10 years? A-because the heart has grown to normal size by then.] Q-What are the ways of spontaneous closure of VSD? A-The mechanisms are: 1) Overgrowth of nearby tissue (while the VSD does not grow, hence closes) 2) Septal tricuspid leaflet 3) Aneurysm of IVS 4) RCC/ NCC prolapsing 5) Infective endocarditis. Small defects: most (80%) close on their own Moderate VSD: 50% will close or reduce in size, not requiring intervention Large VSD: rarely close Q-Which are the conditions wherein a patient with a VSD becomes symptomatic at later age? A-It maybe due to: 1) AR 2) Infective endocarditis- AR, PR, myocarditis 3) Pneumonia/ LRTI 4) Acquired heart disease Q-Generally by what time does AR develop in a patient with VSD? A-Generally by 5- 9 years. Q-In a child with Trisomy 21, what are the additional problems that complicate the heart disease? A-The associated problems are: 1) The above factors of elevated PAP due to L-R shunt 2) Multiple level shunt 3) Primary abnormality in lung (there in decreased number of alveoli & blood vessels, leading to early development of PH) 4) Due to mental retardation, there is underestimation of symptoms. 5) Due to upper respiratory abnormality that makes it more prone to infection.
- 121. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 121 Q-What is the relation between VSD & aortic size? A-‘Larger the VSD, smaller the aorta’. Q-When will one find a large aorta in a patient with VSD-PH? A-In the following conditions: 1) AR 2) Coarctation 3) PDA 4) DORV Q-How to classify VSD depending upon size? A-The VSD’s can be classified by: -With reference to aortic annulus: < 50%- small 50- 75%- moderate > 75%- large -With reference to echo: < 7 mm- small 7- 15 mm- moderate >15 mm- large Q-When is there is significant shunt across the VSD? A-If - Qp/Qs > 1.5-2/1 - LA/aorta ratio > 1.2/1 Q-Reasons why a patient with a large VSD may show spontaneous clinical improvement? A-It may be due to: 1) Development of PH 2) Spontaneous closure 3) Gasulisation. Q-Till what age is a cath not required, to determine the operability in a large VSD with PH? A-Till 1 year of age. Q-What are the complications of a VSD? A-The following complications may develop: 1) Infective endocarditis- of AV, PV, TV, RV jet 2) AR- generally between 5-9 years of age, RCC>> NCC 3) Eisenmengerization (generally in 3rd decade) 4) Gasulisation Q-What is the commonest cause of eisenmengerization in congenital heart disease? A-VSD.
- 122. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 122 Q- How to differentiate between gasulisation & TOF? A-In Gasulisation: 1) There is late onset cyanosis 2) LV is well developed 3) Malaligned VSD is absent 4) Predominantly infundibular narrowing 5) No aortic override [Note:Small VSD’s pose a threat of infective endocarditis. Risk of IE Vs morbidity/ mortality of surgery favors no intervention of small/ moderate sized VSD. But once 1 episode of IE has occurred, surgery should be performed, as chances of re IE are high.] Q-What measures may be taken if a VSD is not found during surgery? A-The techniques that maybe used are: 1) See for jet effect on the RV myocardium 2) Deliver cardioplegia & visualise VSD 3) Detach STL 4) Open aorta & see from the LV side Q-Which anaesthetic drugs worsen PH? A-The drugs are: 1) Ketamine 2) Nitrous oxide Q-What is the timing of surgery in VSD? A-There are various protocols. An acceptable protocol is mentioned below- For Large VSD’s: Infancy: No surgery if- coarctation, Swiss cheese Surgery Early (if large with uncontrolled CCF) Others by 6 months (wait for spontaneous closure) If PVR > 4 Woods/ m2, or If PVR < 4 Wood/ m2 PASP > 50% of SBP Surgery Defer surgery till 12 months Till 1 year of age, a VSD with however high the PVR is operable.
- 123. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 123 After infancy: Surgery if: - PVR < 8 Wood/ m2 - Qp/Qs > 1.5/1 - PVR/ SVR < 0.5/1 - If PVR is > 8 Wood/m2 but falls to < 7 Wood/m2 with Isoprenaline (0.01- 0.1 ug/Kg/min in PA)/ Tolazoline (1 mg/ Kg in PA) Surgery contraindicated (inoperable) if: - PVR > 8 Wood/m2 & no fall with Ispoprenaline - Qp/Qs < 1.5/1 which falls to < 1/1 after exercises For Moderate VSD’s: Symptoms present: Surgery Asymptomatic/ few symptoms: If PAP< 50 mm Hg, or If PAP > 50 mm Hg Qp/Qs < 3/1 Observe till 5 years Surgery If does not close or significant shunt- surgery For Small VSD’s: Young patient- no surgery > 10 years age- individual decision (general consensus is to leave alone) If IE develops, then medical treatment followed later by surgery or if CCF/ increase in CTR/ AR- surgery. PULMONARY HYPERTENSIVE CRISIS Q-What is definition of a pulmonary hypertensive crisis? A-It is a phenomenon seen post CPB and is characterized by a rapid rise in pulmonary arterial pressure (to suprasystemic levels) with associated systemic hypotension, hypoxia & acidosis. The mechanisms implicated are: 1) Decrease in prostacyclin/ thromboxane A2 ratio 2) Platelet activation factor 3) Endothelin release 4) Endothelial dysfunction
- 124. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 124 Q-What are the precipitating factors for pulmonary hypertensive crisis? A-They are: 1) Acidosis 2) Hypoxia 3) Hypercarbia 4) Endotracheal suctioning 5) Restlessness 6) Administration of adrenaline/ high dose of dopamine Q-What are the types of crisis? A-They are of 2 types: 1) Minor- elevation of PAP to/ less than systemic PH 2) Major- elevation of PAP to suprasystemic PH Q-How to prevent a crisis? A-The following measures maybe adopted; - Phenoxybenzamine: 1 mg/ Kg pre operatively followed post operatively by 0.5- 1 mg/Kg/ dose- 8 hrly doses for 4 weeks. - Use fentanyl instead of morphine - Keep electively ventilated for 24- 48 hrs with a PaCO2 < 30 mm Hg & PaO2 of > 100 mm Hg. Q-What is the management of a pulmonary hypertensive crisis? A-The following measures are to be taken: - Immediate paralysis with vecuronium, 100% FiO2 ventilation - Maintain PaCO2 < 30 mm Hg & PaO2 > 100 mm Hg - Fentanyl infusion - If inotrope required- use isoprenaline - NTG/ SNP/ aminophylline/ tolazoline - Prostacyclin may be used - Gradually decrease FiO2 to 50% - After 24 hours start weaning off - Newer- NO, ECMO/ LVAD - Others: a) Continuous PA perfusion during CPB b) Flap closure of VSD (controlled fenestration) c) Oral endothelin receptor antagonist- Bosentan d) Phosphodiesterase V inhibitor- Sildenefil.
- 125. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 125 PDA Q-When to term PDA? A-When the ductus arteriosus fails to close spontaneously by 3 months of age. Q-Why should even a small PDA be closed? A-Because the risk of IE is high. [Note:’PDA diagnosed, PDA should be closed’.] Q-What is the risk of IE in PDA? A-0.4/100/year. Q-Describe the timing of surgery in PDA. A-As follows: Symptomatic: Should undergo immediate closure Asymptomatic: Wait till 8 weeks, If does not close, it requires closure. (Optimum age for closure is between 6- 12 months) Inoperability- like VSD Q-What is the ‘only’ sign of communication at the great arterial level? A-A ‘continuous murmur’ is the only sign of communication at the great arterial level. Q-What is the natural history of PDA? A-It is as follows: Small- only risk of IE (which is high) Moderate & large- High risk of development of PH (1/3 rd by 30 years & 2/3 rd by 40 years) Q-What is the difference between a ductus arteriosus & other arteries? A-The ductus has the following features: 1) Spiral arrangement of muscles in the media 2) Higher content of hyaluronic acid in the media 3) Response seen to O2 & prostaglandin’s. Q-What are the anatomical types of PDA? A-They are: 1) Conical- with narrow end towards PA. 2) Tubular 3) Conical- with narrow end towards aorta (rare) Q-History of PDA surgery? A- 1937: by Streider- patient died due to gastric distension & aspiration 1939: by Gross- first successful PDA clsoure. Q-In a right aortic arch which side will the PDA be situated? A-Mainly on left: going to the left SCA or even a more distal artery.
- 126. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 126 Q-What are the advantages of reducing BP during ductus dissection? A-They are: 1) Ductus becomes less tense (less chances of tearing) 2) PA & aorta fall apart. Q-What are the ways to reduce BP, during ductus dissection? A-By administering: 1) Halothane 2) Sodium nitroprusside 3) Intranasal nifedepine (occasionally) Q-How is a PDA identified? A-A ductus maybe identified by the following points; 1) It lies just beneath the arch 2) The superior intercostals vein crosses over the aorta at the point of PDA 3) It is conical structure with the base towards aorta 4) Recurrent laryngeal nerve winds around it 5) Thrill is present over the PA. Q-How is the arch of aorta identified? A-By identifying the base of the left subclavian artery. Q-Till how much is the BP reduced, prior to clamping of ductus? A-Nearly to 60- 80 mm Hg systolic. Q-How to confirm closure of ductus, after surgery? A-It maybe confirmed by: 1) Disappearance of thrill 2) Absence of murmur over ET tube 3) Increased DBP 4) TEE Q-What are the complications of PDA surgery? A-The complications are: 1) Hemorrhage 2) Recurrent laryngeal nerve injury 3) Vagus nerve injury- gastric distension Q-What are the causes of intraoperative tear of ductus. A-Tear are commoner in: 1) Short & large ductus 2) Inflamed ductus 3) Tense ductus Q-Which is commonest site of tear? A-Mainly posteriorly.
- 127. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 127 Q-What is the management of torn ductus? A-Get blood & CPB ready- descending aortic cannulation & RVOT cannulation- on bypass- cool & achieve circulatory arrest (or trickle flow)- clamp ductus Or Clamp the ascending & descending aorta, open the pericardium & clamp the PA- fibrillate the heart- suture. Q-What are the possibilities if on thoracotomy if no ductus found? A-The possibilities are: 1) Large ductus which is confused with the arch 2) Ductus originating from behind the aorta- loop aorta, lift & visualize from behind 3) Open pericardium & visualize LPA 4) AP window. Q-What devices can be used for PDA closure? A- < 3.5 mm- coil > 5 mm- Amplatzer device 3.5- 5.5 mm- any of above Q-Describe pharmacological closure of PDA? A-It is done using NSAID’s. Indomethacin: 0.2 mg/ Kg/ dose- 12 hourly dosages x 3 Ibuprofen: 10 mg/ Kg- 1st dose 5 mg/ Kg- 2nd dose 5 mg/ Kg- 3rd dose (all at interval of 24 hours) A study from Belgium (NEJM 2000) showed equal rate of ductus closure in both the groups (Indomethacin Vs ibuprofen) with a success rate of 70%. However a significant difference in the incidence of post therapy oliguria (high for Indomethacin) AV CANAL Q-Describe the characteristic echo appearance of primum ASD? A-The MV & TV are at the same level. Q-What is the criteria to classify a interatrial setal defect intraoperatively as an ostium primum defect? A-A straight line is drawn from the coronary sinus upwards. If no part of the ASD is present anterior to the line, it is a primum ASD & similarly if no part posterior to this line, it is a secundum/ sinus venosus defect.
- 128. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 128 Q-What are the principles of ‘closure of cleft’ in AML in an AVC? A-The principles are: - Stretch the leaflets to identify the edges (recognized by chordal insertion) - Take interrupted sutures - Ensure no MS Q-Describe closure of a primum ASD? A-Start anteriorly, come thru’ the base of the AML till one reaches the inferior edge (at the level of coronary sinus) & then go along the ASD edge. Q-What is a Nuhn’s repair? A-It has been described for a complete AV canal. The sutures are taken thru’ the leaflet to the crest of the IVS & tied thus converting the entire defect into a large primum ASD & closed with a patch. COARCTATION Q-What is paradoxical hypertension & why is it termed paradoxical? A-It is termed paradoxical as post relief of coarctation the BP rises instead of falling. 2 phases are present: Early phase: Mainly systolic (within 24 hours) Due to loss of stretch on the baroreceptors of the aortic bodies/ carotid body leading to increased catecholamine release. Late phase: after 2- 4 days, lasts for 2- 4 weeks. Mainly diastolic. Associated with higher levels of rennin angiotensin, perhaps secondary response to phase I. Q-What are the problems of paradoxical hypertension? A-The problems are: 1) Bleeding 2) Mesenteric arteritis causing ischemia Q-How to prevent paradoxical hypertension? A-It can be prevented by: Preoperative: blockers Post operative: SNP, enalapril, propranolol. Q-What is the D/D of rib unilateral notching on X ray? A-They are: 1) Coarctation with involvement of Left SCA- no left sided notching 2) Coarctation with origin of right SCA distal to coarct- no right sided notching 3) Classical BT shunt.
- 129. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 129 Q-What is the D/D of bilateral rib notching? A-They are: 1) Coarctation aorta 2) Multiple neurofibromatosis. Q-What are the causes of radio-femoral delay in congenital heart disease? A-The causes are: 1) Coarctation 2) Interrupted arch Q-What are the causes of coarctation without delay? A-They are: 1) PDA 2) Well developed collaterals CORONARY Q-Classify anomalous coronary artery from aorta? A-Smith’s classification: Type I- single artery to entire heart Type II- Single artery, multiple branches resembling normal anatomy Type III- not fitting in above Q-Interventions that can be performed for anomalous termination of coronary artery? A-If symptomatic, all should be intervened as high chances of: 1) CCF 2) IE 3) Myocardial infarction 4) Rupture Management techniques inlcude: 1) Direct ligation 2) Arteriorrhaphy 3) On CPB 4) Intervention Q-What are the etiologies of aneurysm of coronary artery & discuss the management statergies of the same? A-They are: 1) Atherosclerosis 2) Infection 3) Syphilis 4) Kawasaki’s disease
- 130. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 130 Management strategies include: - Aneurysmectomy + CABG (due to increased complications of thrombosis & rupture if left alone) Q-What is Bland-White-Garland syndrome? A-It is the ‘Anomalous origin of LAD from pulmonary artery’. Its clinical features are: - Angina on crying - Myocardial infarction - MR - Endocardial fibroelastosis ECG features are: anterolateral ischemia or infarction. Treatment strategies are: - Ligate (to prevent steal) - SCA to LAD anastomosis - Aortic reimplantation Q-Should an asymptomatic coronary artery- RA/ RV fistula be closed? A-Yes, as once symptoms develop the mortality & morbidity is high. OTHER SURGICAL POINTS FOR CAHD Q-What are various devices available for intervention in CHD? A-They are: 1) Umbrella: - Rashkinds - Starskin 2) Coils: - Gianturco - Knit occluder 3) Detachable balloon 4) Amplatzer 5) Clam shell Q-What are the procedures to widen SVC? A- 1) Patch enlargement 2) Atriocavopexy 3) Warden procedure (detach SVC & resuture to RAA) Q-What are the definite indications for PV replacement? A-The indications are: 1) Hypertensive PR leading to rise in RVEDP 2) APVS (?)
- 131. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 131 Q-Is there any procedure still performed under inflow occlusion? A-Yes. Pulmonary valvotomy in a neonate is still performed in certain centers using the inflow occlusion tenchnique. Q-What are the indications for PA banding? A-The indications are: In Acyanotic: 1) VSD with infection/ CCF 2) VSD with coarctation 3) Swiss cheese septum in infant In Cyanotic: 1) TGA- in older infant for arterial switch 2) TA- Ic 3) Single ventricle.PH. Q-How does PA banding help? A-It helps by: 1) Reducing PAP- thus reducing PVR 2) Increasing SBP 3) Decreasing LVVO 4) Spontaneous closure of VSD (JACC 1999- 13/14 VSD’s closed spontaneously after PAB) Q-What are the advantage of performing a PAB thru’ a midsternotomy? A-The PA can be accessed in any relationship of great vessel . Q-What should one suspect if on sternotomy, for an interrupted arch, no thymus is found? A-Suspect DiGeorges syndrome. Q-What is the importance of DiGeorges syndrome? A-The importance is of associated; 1) Hypocalcemia- requiring treatment 2) Immunological problems. Q-What is the management of postoperative heart blocks? A-A generalized protocol is as follows; Wait for 7- 10 days with/ without steroids Evaluate for - Narrow/ broad complex - Threshold of pacing If broad complex with a high threshold for pacing- PPM If broad with good threshold- may wait for another 10 days. Narrow complex- custom to patient
- 132. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 132 INDIAN PEDIATRIC SCENERIO Q-What is the disease distribution in the pediatric population in India? A-It is as follows: 1) Infection: 30% 2) Malnutrition: 25% 3) Diarrhea: 20% 4) Others: 25% Q-What is the ‘Life expectancy’ of an individual in India? A- For male: 64 years For female: 64.5 years Q-What is the Infant mortality rate (Infant is less than1 year)? A- India: 70/ 1,000 live births Compare with US: 9/1,000 live births Afghanistan/ Angola: 170/ 1,000 live births Q-What is the current Immunization programme followed in India? A-It is as follows: Birth BCG 6 weeks (1 ½ months), 10 weeks (2 ½ months) & 14 weeks (3 ½ months) OPV + DPT 9 months: Measles 1 ½ year: OPV + DPT (Booster 1) 5 year: DT (Booster 2)
- 133. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 133 CONGENITALCYANOTIC HEART DISEASES GENERAL Q-What is the definition of complex congenital heart disease? A-A complex CHD can be defined as; “when abnormality exists at multiple levels requiring multistage procedures with an increased morbidity & mortality.” Q-What are the features of decreased pulmonary blood flow on clinical evaluation? A-The features are: History: - Cyanosis - Cyanotic spells - Squatting episodes - -ve history Examination: - Silent precordium - RV impulse ECG: - RV dominance X-ray: - Pulmonary oligemia Q-Can the age of onset of cyanosis provide a clue to a diagnosis? A-Yes. The various pathologies that have onset at a particular age are: 2) At birth - Pulmonary atresia - Aortic atresia - TAPVC - TGA - Truncus arteriosus - Taussig Bing - Hypoplastic left heart syndrome 3) 0- 7 days - Ebsteins - Tricuspid atresia- Ia/IIa - HLHS 4) > 1 week- < 1 month - TGA - TAPVC - Truncus - TOF with severe PS - DORV with severe PS - Common atrium 5) > 6 months - TOF & its variations - Eisenmengerisation
- 134. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 134 Q-What is a significant desaturation? A-A saturation of less than 95% on room air. Q-Which are the conditions associated with mild cyanosis? A-They are: 1) TAPVC 2) Ebsteins 3) Common atrium 4) Eisenmengerisation. Q-Which are the conditions known for cyanotic spells? A-They are: 1) TOF 2) DORV, VSD, PS 3) Tricuspid atresia Ib/ IIb 4) TGA, PS Q-Which are the conditions known for squatting? A-They are: 1) TOF 2) DORV, VSD, PS 3) Tricuspid atresia- Ia/Ib, IIa/IIb Q-What are the CCHD without PS but with normal PAP? A-They are: 1) single atrium 2) SVC into LA Q-Which CCHD are commonly associated with a right aortic arch? A-The following: 1) TOF with pulmonary atresia 2) Truncus Q-Which are the ‘Duct dependent circulation’? A-They are: Left to right shunt: - Pulmonary atresia with intact IVS - TGA - Tricuspid atresia Ia Right to left shunt: - HLHS - Interrupted arch - Aortic stenosis - Severe coarctation aorta.
- 135. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 135 Q-Which are the conditions associated with late onset of cyanosis? A-They are: 1) all with a well balanced shunt & RVOT obstruction 2) Eisenmengerisation Q-A single conus is seen in which conditions? A- - TGA - Truncus Q-A double conus is seen in which conditions? A- - DORV Q-Describe decision making in pulmonary atresia with intact IVS? A-Depends upon the TV annulus size. If: - TV size -4: Fontan - TV size –1 to –3: Biventricular repair. Q-Which conditions are to be considered in patients, more than 20 years of age, with cyanosis? A-They are: 1) TOF 2) CTGA, PS 3) ASD, PS 4) VSD, PS 5) TA Ib, 6) Ebstein’s. Q-What are the causes of headache in CCHD? A-Headache maybe due to: 1) Cortical venous thrombosis (due to high Hct) 2) Brain abscess 3) AV malformation with a bicuspid AV/ coarctation 4) Systemic hypertension 5) Embolization Q-Which PR is not well tolerated? A-The following PR’s are not well tolerated. - Hypertensive PR (sec to PH) - Muscle bound RV (TOF) Q-What is the ‘rough rule’ for size for pulmonary annulus? A- 1 mm/Kg body weight for the first 20 years (60% of the MPA should be the RPA & LPA)
- 136. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 136 Q-How is the actual size of pulmonary annulus calculated by? A-Using the criteria described by Rowlett, Pacifico, King, Kirklin & Moris Lev. Q-L-posed aorta is commonly seen in which conditions? A-In: 1) c-TGA 2) Taussig Bing 3) TA-III Q-When is a VSD enlarged? A-In: - DORV with restrictive VSD, when a tunnel has to constructed to the aorta - D-TGA with VSD (small) when a Rastelli is planned Q-In which CCHD is the aorta anterior to PA? A-In: 1) TOF 2) DORV 3) TGA 4) TA Q-Which conditions are commonly associated with a right aortic arch? A- 1) TOF with PA 2) Truncus 3) TOF 4) TA 5) Single ventricle 6) AP window Q-Which cyanotic heart diseases are associated with increased JVP? A-Seen in: 1) Truncus 2) Tricuspid atresia- Ic 3) TAPVC 4) Ebstein’s anomaly 5) AV canal Q-Which cyanotic heart diseases are associated with increased CTR? A-Seen in: 1) TAPVC 2) Ebstein’s 3) Single ventricle 4) Truncus 5) AV canal defect
- 137. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 137 Q-Which CCHD have absent RV inflow pulsation? A-The conditions are: 1) Tricuspid atresia 2) Ebstein’s with ASD Q-Which cyanotic heart diseases are associated with LVH? A-LVH maybe seen in: 1) TA 2) PA with intact IVS 3) AV canal 4) Ebsteins 5) Adult TOF. Q-Ennumerate the conditions which maybe associated with CCF, in patients with cyanotic heart disease of > 5-years age? A-The conditions are: 1) TOF with AR 2) TOF with IE 3) Central shunt 4) TOF with anemia 5) TOF with systemic HT 6) Ebsteins 7) Eisenmengerization Q-Which CCHD will have bounding pulsations? A-They are: 1) TOF with PA, TOF with AR 2) Truncus 3) TGA Q-What are the causes of swollen joints in cyanotics? A-It may be due to: 1) Hyperuricemia (due to increased RBC turnover) 2) Sepsis 3) Hemarthrosis Q-Which are the CCHD with split P2? A-They are: 1) TAPVC 2) Common atrium 3) Ebsteins 4) ASD with eisenmengerization
- 138. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 138 Q-Ennumerate conditions of severe cyanosis with low/ no murmur? A-The are: 1) TGA 2) Cyanotic spell Q-Which are the CCHD with a narrow pedicle on X-ray? A-Seen in: 1) Truncus 2) Aortic dilatation- AR/ PDA 3) Aortic override- PS, PA Q-Which are the CHD associated with a ‘box shaped’ heart? A-They are: 1) Ebsteins 2) TAPVC Q-What is a RV dependent coronary circulation? A-When atleast 2 major epicardial arteries (viz., LAD, left circumflex artery or RCA) are supplied entirely by the RV sinusoids. Q- On echocardiography of neonates, which structures are difficult to visualize?? A- 1) PV drainage 2) Pulmonary outflow tract obstruction due to- High PVR/PDA 3) Severity of LV outflow tract Q-Which conditions have a PA O2% > Aorta O2%? A- 1) TGA 2) Supracardiac TAPVC (if SVC blood flows preferentially across TV & IVC blood flows across ASD into LA) Q-Which conditions have an Aorta O2% > LV O2%? A- 1) c-TGA Q-Describe ‘diagnostic X-Rays’ of congenital heart disease. A-They are: 1) Ebstein’s: CTR > 60%, RAE, small MPA, narrow pedicle & oligemic lung fields 2) Valvar PS with TR: CTR > 60%, RAE, MPA full, narrow pedicle & oligemic lung fields 3) d-TGA: egg on side appearance, cardiomegaly, plethora 4) Supracardiac TAPVC: figure of 8, cardiomegaly, plethora 5) c-TGA: L posed aorta 6) TOF with APVS: dilated PA with oligemic lung fields, no LV
- 139. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 139 Q-What is the D/D between Hypertensive PR and normothermic PR? A-Hypertensive PR has an early diastolic murmur while normothermic PR has a mid diastolic murmur. Q-Which is the commonest site for formation of intracranial abscess; in cyanotics? A-The commonest site for formation of intracranial abscess is in the temporoparietal region. Q-Describe angiographic classification of PA stenosis? A-McCue’s (1965) classification- 1) MPA or proximal RPA/ LPA stenosis 2) Coarctation of PA bifurcation 3) Multiple peripheral artery stenosis (beyond pericardial reflection) 4) Combination of 1/ 2 & 3. Q-When is the thymus excised, during cardiac surgery? A-In cases of: 1) Takedown of a left BTS 2) Visualization of LPA 3) RV-PA conduit 4) Vertical vein ligation 5) As routine TOF Q-Which are the commonest adult cyanotic heart disease? A-They are: 1) TOF 2) Eisenmengerization Q-What is Taussig’s axiom? A-Cyanosis + normal sized heart + clear lung fields: the combination of the 3 is diagnostic of TOF (according to Taussig) Q-What is the cause of easy fatigability in TOF? A-It is secondary to tissue hypoxia Q-Which clicks are commonly heard in TOF? A-Mostly aortic, rarely pulmonary. Q-When is a PR significant in TOF? A-When there is: 1) Equalization of PA & RV diastolic pressure, or 2) Pulse pressure > 70% systemic SBP (in absence of AR)
- 140. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 140 Q-What is a significant gradient across the RVOT? A-When the gradient is 40 mm Hg. Q-Who coined the term pentology of Fallot? A-Rao & Anderson. Q-What is McGoon’s ratio? A-It was described in 1981 & was originally termed as the ‘Angiographic ratio’. RPA is measured at the right border of spine & the LPA before its 1st lobar artery. All the measurements are taken in systole. For ICR TOF, Ideal is > 2 & optimum is > 1.5. Q-What is the D/D of TOF.APVS clinically? A-They are: 1) Without cyanosis: - AS/AR - VSD.AR - Truncus 2) With cyanosis - TOF.pulmonary atresia with MAPCA’s - Pulmonary AVF Q-What is D/D between TOF and isolated PS? A-In a case of isolated PS: - There will be an increase in murmur with inspiration - RV heave - No sudden transition in from V1 to V2/3 Q-What is the ‘Ideal age’ for unifocalization? A-The ideal age is 3 years (as the collaterals are large enough). Q-Onwhich sided PA is osteal stenosis common? A-On the left side (due to presence of ductal tissue). Q-What is the embryological basis of conotruncal anomalies? A-Microdeletion of q11 in chromosome 22 results in abnormal development of conus. This later manifests as conotruncal anomalies. Q-What are ‘special ECG features’ of a patient with TOF with additional anomlies? A- - If counterclockwise loop- Associated AV canal - If qR in V1- c-TGA Q-What is the reason of ‘boot shaped heart’ in TOF? A-It is seen due to absence of LV density.
- 141. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 141 Q-What is the incidence of multiple VSD’s in TOF? A-About 2%. The additional VSD is mainly of inlet type (may be missed by a RVOT approach) Q-What is dosage of propranolol? A-1-4 mg/Kg/Day in 3 divided doses. Dosages as high as 20 mg/ Kg/ Day also have been tried however the complication rate is very high. During high dose regimen watch for: - Bradycardia - Increase in CTR - Decrease in EF on echo Q-How is propranolol therapy monitored clinically? A-The dosage can be increased till: - The HR falls by 25% of the basal HR - There is no bronchospasm. Q-How does propranolol help in TOF? A-It helps by: 1) Decreasing the infundibular spasm by decreasing the adrenergic drive 2) Decreasing HR & thus less chance of SVT 3) Shifts the O2 dissociation curve to right 4) Unhindered activity leading to increased SVR, hence decreased R-L shunt Q-What are the limiting factors of propranolol therapy during a spell? A- - Heart rate - Systolic BP: if SBP falls by more than 20 mm Hg of baseline, then propranolol administration has to be stopped. Q-What are the various interventions procedures that can be performed in a patient with TOF? A-They are: Pre op: 1) Coil embolization of MAPCA 2) BPV 3) Perforation/ coring of RVOT/ pulm. Atresia Post op: 1) Dilatation of BT shunt 2) Arrhythmias management 3) Management of AV block 4) Septostomy Q-Which shunt is more prone to an increased blood flow to the ipsilateral side? A-Pott’s shunt.
- 142. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 142 Q-Describe the assesment LV size in TOF? A- - Large if diameter > RV - Small if diameter < 3/4th RV - Diminutive if diameter < ½ RV (all diameters taken transversely at the end of diastolic frame) Q-What are the criteria for LV size, in TOF, contraindicating intracardiac repair? A-ICR is contraindicated if: - LVEDV < 30 ml/m2 - LVED (D) < 60% of normal for that weight - MV area < -2 Z Q-What are the causes of LV failure in TOF? A- The causes are: 1) AR 2) Systemic hypertension 3) Infective endocarditis 4) Relative anemia 5) Coronary artery disease 6) Cyanotic cardiomyopathy Q-Discuss incidence of absent ipsilateral PA’s in CHD. A-In congenital heart disease, the incidence of absent LPA is same as that of absent RPA. However in TOF, absent LPA is common but absent RPA is rare (later is seen in dextrocardia/ situs inversus). Q-What is ‘Secondary Fallot’? A-It is gasulisation of a VSD. Q-What are the causes of CCF in TOF? A-Ventricular failure, in TOF, maybe due to; 1) BTS, MAPCA, PDA LVVO LVF 2) AR, infective endocarditis, anemia, systemic HT LVF 3) Cyanotic cardiomyopathy, coronary artery disease BVF 4) TR/PR RVF Q-In which cases of TOF will the PA be full on X-ray? A-A full PA may be seen in: 1) Mild TOF 2) Post stenotic dilatation 3) Well developed 3rd chamber 4) Post BTS/ good collaterals/ PDA 5) Absent PV syndrome 6) L posed aorta
- 143. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 143 Q-What are the causes of chest pain in a patient of TOF? A-It may be due to: - RVH - Rarely coronary artery crossing between aorta & PA Q-What is the D/D of TOF? A-The various D/D of TOF are: 1) VSD, PS: - generally late (5-6 years) presentation, - mild cyanosis, - LRTI in early childhood, - LV apex 2) PS, VSD: - Harsh PS murmur with late peaking 3) DORV, VSD, PS: - on echo 4) C-TGA, VSD, PS: - Heart block - qR in V1 5) TA IIb: - No RV inflow pulsations - No R in V1, V2 Q-What is the incidence of a PV pathology in TOF? A- - Bicuspid= 60% - Tricuspid= 15% - Rest are dysplastic Q-What are the reasons for a ‘well-developed LV’ in TOF? A-They are: 1) AR 2) Good collaterals/ PDA/ shunt 3) Adult TOF 4) Common AV canal 5) VSD is restrictive Q-What are the predominant symptoms in ‘adult TOF’s’? A-They are as follows: 60%- squatters 15%- CCF 5%- cyanotic spells High incidence of systemic hypertension
- 144. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 144 Q-Why is CCF uncommon in TOF? A-CCF is uncommon in TOF due to: - RV hyperpplasia - Non restrictive VSD Q-What is the ECG characteristic of an adult TOF? A-Due to high RVEDP there is RV dilatation. This leads to tall p in II & V1. Q-What are the causes of RV failure in adult TOF? A-They are: 1) RVH 2) RCA is not meant to supply ventricle at systemic pressure 3) Hypertension 4) AR Q-What is the reason for lacy reticular pattern in TOF? A-It is seen due to the dilated bronchial arteries which supply the adjacent alveoli. They are present all over the lung, especially the lower lobe. Q-What are the cause of hemoptysis in TOF? A-They are: 1) Bronchial artery rupture 2) Polycythemia 3) Infective endocarditis leading to infarction 4) Tuberculosis Q-What is a high PAP in TOF? A-Anything that is more than normal. Q-Why is there increased bleeding tendency in TOF? A-Due to: 1) High Hct leading to relative plasma deficiency 2) Hypoxia affecting liver & platelets 3) Subclinical DIC All these factors lead to - decrease in number of platelets - decreased functioning of platelets - increased FDP - altered WBC function - decreased liver clotting factor Q-What are the reasons for high PAP in TOF? A-They are: 1) With normal PVR- peripheral pulmonary artery stenosis 2) With elevated PVR- excessive shunt (especially central shunt)
- 145. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 145 Q-What is the McGoon’s ratio accepted for an ICR TOF? A-If McGoon’s less than 0.7 then ICR TOF is contraindicated. Q-Why are adult TOF at higher risk for surgery? A-Due to: 1) RVH may lead to RV failure 2) Endocardial fibroelastosis Q-What is the mortality of ICR in adult TOF? A-Various series Have shown moratlity rates as: - Higgins (AJC, 1972)= 15% - Diettrich= 16% - Italian study in J Thorac Cardiovasc Surg 1996= 2.5% Q-What is anesthesia protocol for an ICR TOF? A- Induction with: - Ketamine (2- 10 mg/ Kg). Advantages are: a) can be given i.m. b) although it has sympathomimetic action & is expected to increase the right to left shunt but the opposite effect is seen. (always give with atropine) - midazolam (0.2- 0.3 mg/ Kg) Maintenance with: - Fentanyl & pancuronium. Q-What are the approaches for ICR.TOF & who has introduced them? A- 1) RA-PA: Hudspeth 2) RVOT (longitudinal incision): Lillehei 3) RVOT (transverse): Gerbodie 4) PA only: Sakornapant Pantpis 5) RA only: Edmunds, Saxena Q-What is the extent of a RVOT incision during ICR TOF? A- Upper margin of RVOT incision: - just below the annulus Lower margin of RVOT incison: - till the level of the aortic annulus, or - 1/3 distance from PA to apex
- 146. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 146 Q-What care should be taken while excising RVOT muscle? A- -On Septal side: take care for - can create a new VSD - damage to papillary muscle to ATL - damage to the 1st septal artery -On Parietal side: - if excess shaved, there will be no margin for suturing -On Crista: - damage to RCC -if scissor inserted across the VSD (in case of infundibular atresia- damage to AV/ VSD may get enlarged. Q-What care must be taken of ‘the hypertensive RV’ intraoperatively? A- Preop: - Administration of O2 free radicals Intra op: - Cold blood antegrade cardioplegia - Aprotinin - Warm induction - Avoid large incisions over RVOT - Avoid PR Postop: - Adequate inotropes Q-What is considered a ‘good coring’ of the RVOT? A-The following structures can be visualized after a complete coring: - complete VSD - tricuspid valve - apex of RV - pulmonary valve - AV across the VSD. Q-Discuss techniques to improve the exposure of VSD in TOF. A- In RV approach: - stay sutures over RV - turn table to left - mop beneath the LV - adequate excision of the parietal band - retractor in VSD - visualization improves with suturing - start at the anteroinferior margin
- 147. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 147 In RA approach: - stay sutures over the RA & STL - additional retractor in the TV - if required detachment of the STL Q-What are the dimensions of a RVOT patch? A-The dimensions should be such that the: - Length is 1 ½ times the incision length - Width should be 3 times more than the proposed increase in diameter Q-In a deeply cyanosed child how much Hct is generally maintained, on bypass? A-Around 45%. Lower Hct may lead to: - Capillary leak syndrome - Excessive prime requirement. Q-What is the cause of ‘low pressure’, on CPB, in TOF? A-They are: - Hemodilution - Collaterals Q-What are the management strategies for excessive LA return; in a patient with TOF? A-Management strategies includes: 1) Adjust flows, cool further 2) Search for PDA 3) Open pleura, retract lung to visualize the descending thoracic aorta- visualize any obvious collaterals & tackle Q-Discuss post ICR TOF arrhythmias. A-Using Holter monitoring, ventricular arrhythmias can be detected in 40- 50% of patients in the postoperative period. Predictors of arrhythmias are: 1) Age of surgery 2) Moderate/ severe PR 3) Ventricular dysfunction 4) Prolonged QRS interval (> 180 msec) [Note:RBBB is common after TOF surgery but complete heart block is rare.] Q-What is the incidence of complete heart block post ICR TOF? A-Less than 1%. Q-What is the incidence of RBBB +/- LAHB post ICR TOF? A-20- 25%. Q-Which heart block, post ICR TOF, has poor prognosis? A-RBBB with LAHB (there is higher chance of sudden death)
- 148. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 148 Q-What is the reason for LAHB, post ICR TOF? A-LAHD occurs if the sutures taken for VSD closure ‘lie’ towards the LV side. Q-What are the features of LAHB on ECG? A-Features are: 1) Left axis deviation 2) Counterclockwise loop 3) Prolonged QT interval 4) Small R & deep S in V5, V6. Q-What are the strategies for coronary crossing RVOT? A-The various approaches for this situation are: 1) RA-PA approach (Hudspeth) 2) Elective LIMA- LAD anastomosis (Cooley) 3) Turn the flap of anterior pulmonary artery to the ventriculotomy & suture and additional patch over this PA flap (Van Son) 4) Mobilization of the coronary artery & suture patch beneath the lifted coronary (Boncheck) 5) BT shunt Q-What measures maybe taken if there exists a significant coagulation abnormality in TOF preoperatively? A-Administer heparin for 10- 15 days (for FDP removal) Q-In, which conditions in TOF, is it difficult to go around the SVC? A-In those who have undergone a prior right BTS/ Waterston Cooley shunt. Q-Why is phenylephrine preferred on bypass, for TOF? A-It is a selective peripheral vasoconstrictor & does not affect the renal system (if not available, use adrenaline). Q-What are the causes of RV dysfunction in TOF? A-Are: 1) Pre op: - Chronic ischemia (adult TOF) - Repeated cyanotic spells 6) Post op: - CPB & cross clamp - RV incision - Damage to coronaries - PR/TR - Large adynamic patch - Residual VSD Q-Which sternotomy, in a c/o TOF, will bleed excessively? A-Post classical BTS.
- 149. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 149 Q-What are the late complications of ICR TOF? A- They are: 1) RVOT restenosis 2) PR/TR leading to RV failure 3) Arrhythmias 4) Aneurysm of RVOT patch 5) Calcification of RVOT patch (Dacron, PTFE) Q-What are the contraindications for ICR TOF? A-They are: 1) Unfavorable PA anatomy in infant 2) Multiple VSD in infant 3) Coronary artery crossing RVOT in infant 4) Hypoplastic LV (LVEDV < 30 ml/m2, MV < -2 ‘Z’, Pulmonary annulus < -7 ‘Z’) 5) Institutional criteria for performing ICR at a particular age & weight TOF PHYSIOLOGY Q-Which conditions included under Fallot’s physiology? A-The follwowing: 1) TOF, VSD, PS 2) DORV, VSD, PS 3) C TGA, VSD, PS & d TGA, VSD, PS 4) VSD, PS 5) ASD, PS 6) TA Ib/ IIb 7) Single ventricle, PS 8) AV canal, PS Q-What are the indications for creating a VSD? A-TGA with PS & intact IVS for a Rastelli. Q-How to differentiate between VSD.PS & PS.VSD? A- If the ECG axis is > 135 consider diagnosis of PS.VSD If the ECG axis is < 110 consider VSD.PS Q-What are the fallacies of McGoon/ Nakata? A-It does not take into account: - Distal PA stenosis - PA dilatation
- 150. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 150 Q-What is the definition of ‘DORV’? A-The various definitions of DORV are: 1) Anderson- 2 criteria must be fulfilled to call DORV i) > ½ circumference of each semilunar valve overlies the morphological RV ii) Persistence of a subaortic conus with loss of aorto mitral continuity. 2) Neufeld- criteria for DORV are: i) Both great arteries arise from morphological RV ii) Loss of continuity between both AV valves & semilunar valves iii) VSD may or maynot be present, & if present, then may represent the only outlet for LV iv) Valvar/ subvalvar PS may or maynot be present. 3) Lev- criteria for DORV are: i) One great artery & > ½ of other great artery arising from morphological RV ii) Loss of aortomitral or pulmonary mitral continuity 4) Van Praagh- DORV is defined as; i) Persistance of subaortic/ subpulmonic conus leading to loss of continuity with the MV. Q-What is the importance of juxta posed appendages? A-The importance lies in: 1) For association with diseases like: - TA-II - TGA - DORV, VSD, subpulmonic VSD 2) For performing procedures like: - Atrial septectomy - Contraindication to a Senning’s [Note:Left sided juxta posed appendages are more common than right sided.] Q-What is the embryology of DORV? A-It is due to abnormal development, rotation & absorption of the conal septum. Q-Discuss the embryopathology of TOF, DORV & TGA. A-Seen from above, there is a counterclockwise rotation of the aortic conus. In the various conditions, the following features are noted; - TOF- absorption of septum (in mid portion of bulboatrioventricular ledge)- responsible for aortomitral continuity - DORV- non absorption of BAL - TGA- absorption of left margin of BAL- establishment of mitralpulmonary continuity.
- 151. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 151 Q-What are the types of VSD in DORV? A- - Subaortic VSD= 70% - Subpulmonic VSD= 20% - Doubly committed VSD= 9% - Non committed VSD= 1% Q-What are the problems of c-TGA without VSD? A-The problems are: 1) Complete heart block (2% patients/ year) 2) Left AV valve (TV) regurgitation 3) Left sided ventricle (RV) failure Q-What is the segmental anatomy of c-TGA? A-It is: For situs solitus- SLL For situs inversus- IDD Q-What are the disadvantages of prostaglandin’s? A-They are: - Tachypnoea- leading to respiratory arrest - Tachycardia Q-What is the duration of prostaglandin infusion? A-It may be administered for 3 days to 2 weeks. Its efficacy is less after 2 weeks. Q-Discuss D/D of Fallot physiology on ECG? A-The following features are to be seen: TOF: QRS axis between 90- 150 If > 150: DORV, TGA -30 to -60 with LVH: Tricuspid atresia Left axis deviation with RVH: AV canal, single ventricle Right axis deviation without RVH: single ventricle SINGLE VENTRICLE Q-What pathologies are included under ‘single ventricle’? A-They are: 1) Common ventricle 2) DILV 3) HLHS 4) Tricuspid atresia
- 152. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 152 Q-What is the incidence of HLHS? A-It is the same as PDA, coarctation. (7% of CHD) Q-What are the ‘Ten commandments’ of Choussat? A-The criteria required for a candidate to be eligible for a Fontan operation were laid down by Choussat. They are: 1) Age > 4 years & < 15 years 2) Normal sinus rhythm 3) Normally draining systemic veins 4) Normal RA (complaint) 5) PA anatomy: Nakata > 250 mm2/m2 & McGoons > 1.5/1 6) No distortion of PA anatomy 7) PVR < 2-4 Wood 8) PASP < 15- 20 mm Hg 9) No left AV valve regurgitation 10) Normal LVEF [Note:These indications have undergone changes & many are no longer a contraindication for a Fontan operation] Q-What are the measures to be taken in a patient with a Glenn shunt having increased cyanosis? A-The options are: 1) Additional BTS 2) Make Glenn pulsatile by creating a right axillary artery-vein fistula 3) Investigate for presence of pulmonary AV fistula Q-What are the causes of PS with intact IVS? A-They are: 1) Congenital- 6 types: tricuspid (Williams), bicuspid, unicuspid with central opening, unicommisural, hypoplastic annulus, dysplastic. 2) Dysplastic (Noonan’s). Q-What is the worst complication of Fontan? A-The most dreaded complication after a Fontan is Protein losing enteropathy. It is associated with a high mortality. Treatment options include administration of Heparin & SOS takedown of Fontan/ conversion to 1 ½ repair.
- 153. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 153 CYANOSIS WITH PULMONARY HYPERTENSION Q-Ennumerate the cyanotic heart diseases with increased pulmonary blood flow? A-They are: 1) TAPVC 2) Truncus 3) Taussig Bing 4) TGA 5) Common atrium 6) Eisenmengerisation Q-Define the term “transposition physiology”? A-It is defined as, ‘the presence of cyanosis with increased PBF (actually is a misnomer as TGA can be present with decreased PBF)’. It includes: 1) TGA 2) TAPVC 3) Truncus arteriosus 4) Taussig Bing 5) HLHS 6) TA Ic/ IIc 7) DORV without PS 8) Single ventricle without PS Q-What are the conditions, in neonates, presenting with cyanosis and severe PH? A-The conditions are: 1) Obstructed TAPVC 2) Persistent fetal circulation Q-What is the definition of TGA? A-TGA can be defined as, “A congenital malformation characterized by origin of the great arterial trunk from inappropriate ventricles.” Term coined in 1814 by John Farre. Q-What is Hemitruncus? A-Hemitruncus is defined as, “When one PA arises from truncus & one from the RV.” There are 2 separate arterial valves. Q-What is solitary aortic trunk? A-There is complete absence of intrapericardial PA’s. The blood supply to the lungs is only from collaterals.
- 154. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 154 Q-What is Pseudotruncus? A-Pseudotruncus is a term for ‘TOF with PA’. Q-What are the primary indications for an atrial switch? A-The indications are: 1) Age (unless PAB followed by arterial switch) 2) TGA with LVOT obstruction (or perform a Rastelli) 3) AV discordance with VA concordance Q-Discuss long-term results of switch operations? A-The results of switch operations are summarized below. 10 year 15 years Mustard 85% 80% Senning 85% 80% Rastelli 60% 60% Q-What are the contraindications to Senning’s operation? A-Left juxtaposed appendages are a contraindication to Senning’s. Q-What are the contraindications to Rastelli operation? A-They are: 1) Non committed VSD 2) Straddling AV valve over VSD Q-What are the idications for a balloon atrial septostomy? A-All ASD dependent circulations with restrictive ASD are candidates for BAS. These can be divided as: Those with Left to right shunt at the ASD: 1) Aortic atresia 2) HLHS 3) Interrupted arch Those with Right to left shunt at the ASD: 1) TGA 2) TAPVC 3) TA 4) PA with intact IVS Q-Discuss the surgical technique of Blalock Hanlon atrial septectomy? A-Steps are as follows: - right anterolateral thoracotomy thru’ the 5th space - pericardium opened behind the phrenic - RPA, SVC, IVS & RPV’s freed - RPA, RSPV & RIPV looped - A long curved instrument passed behind the IVC & the RPV’s to emerge beneath the SVC - NaHCO3 administered
- 155. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 155 - RPA, RPV’s snugged & clamp (described above) applied - 2 parallel incisions on the RA & LA taken septum excised septum is further pulled into the opening & excised - clamp allowed to allow the septum to retract & fall back - suturing done - clamps & loops released Q-Can there be right vertical vein in a c/o TAPVC? A-Yes. Q-What is the site of obstruction of intracardiac TAPVC? A- 1) Esophageal hiatus 2) If it drains into the portal vein- portal vein pressure is high then drainage is impaired. Q-If prostaglandins are started to a sick neonate, with cyanosis & PH, which condition should be suspected if there is no improvement? A-TAPVC with obstruction Q-In a patient with TAPVC, how big should the opening in the posterior wall of LA be? A-As big as the mitral valve. Q-Which structure courses along the vertical vein? A-The left phrenic nerve Q-What is the D/D of TAPVC? A- D/D of unobstructed TAPVC: - In adolescents/ adults- common atrium, ASD, PAPVC - In infants- AV canal, large VSD, large PDA, truncus D/D of obstructed TAPVC: - HLHS - Severe coarctation - TGA - TA- Ia/IIa or PA Q-Which cardiac conditions may be associated with TAPVC? A-They are: 1) Truncus 2) TGA 3) AV canal 4) PDA 5) Pulmonary atresia 6) Single ventricle
- 156. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 156 Q-What are the indications for operating a patient with Ebstein’s anomaly? A-The indications can be summarized by the pneumonic ‘ABCDE” ABCDE a) A- Arrhythmias refractory to medical treatment b) B- Breathing room air O% < 80% c) C- CTR > 65% d) D- Dyspnea III, IV e) E- - Paradoxical Embolism - Echo; Tajik’s score > 2 In general the indications for surgery are: 1) Symptoms 2) Cyanosis 3) RVF 4) CTR > 65% 5) Arrhythmias 6) Paradoxical embolism Q-What is Tajik’s score? A-It is an echo based score. It is as follows: Criteria Score (total= 13) ATL tethering- severe 3 ATL immobile 2 ATL tethering- mild 1 ATL displacement 1 STL absent 1 RA > 60 mm/m2 1 TV regurgitation with prolapse 1 Functional RV < 0.35 2 RVOT aneurysmal 1 Depending upon the score the management maybe decided: < 2: conservative treatment 2-5: repair advised > 5: replacement advised Q-Describe the JACC mortality assessment for Ebsteins. A-For determining postoperative mortality. [RA + atrialized RV]/ [functional RV + LA + LA] If the above is: < 0.5= 0% mortality 0.5- 1.0= 10% mortality 1.5= 44% mortality > 1.5= 100% mortality
- 157. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 157 Q-What are the surgical options for Ebstein’s? A- In infants- Glenn followed by Fontan In teenagers- - Repair: Danielson, Quegebeur, Carpentier - Replacement: Bioprosthetic valve Q-What are the predictors determining the outcome of surgery in adult Ebstein’s? A-The predictors are: 1) NYHA class 2) Heart size 3) Presence or absence of cyanosis 4) Paroxysmal atrial tacchycardia Q-What are the complications of biventricular repair in Ebstein’s? A-They are: 1) Complete heart block 2) Persistence of SV arrhythmias 3) Residual TR 4) PV dysfunction Q-What are the problems during surgery of truncus? A-They are: 1) Cannulation & CPB 2) RV-PA conduit 3) Truncal valve- stenosis/ regurgitation- needing replacement with homograft 4) Coronary artery anomaly- damage during surgery (Mortality= 25- 75%) Q-Define eisenmengerization? A- Paul Wood has defined eisenmengerization as, “pulmonary hypertension at systemic level due to high PVR (> 800 dynes.sec.cm-5 or > 10 Wood units) with reversed/ bi- directional shunt across the VSD/ASD/PDA.” Tandon has defined eisenmengerization as, “non reactive pulmonary arterial hypertension resulting in right to left shunt at the atrial, ventricular or great arterial level.” Q-Beyond what sizes of ASD, VSD & PDA can eisenmengerization result? A- ASD: 3 cm VSD: 1.5 cm PDA: 0.7 cm
- 158. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 158 Q-What is the age of eisenmengerization in ASD, VSD & PDA? A- ASD: 35 years VSD: 22 years PDA: 19 years Q-What are the clinical feature of eisenmengerization? A-Symptoms are mainly due to hyperviscosity. They include: - visual disturbances - fatigue - headache - dizziness - hemoptysis As hemostasis is altered they are at risk of both bleeding & thrombosis Q-What are the characteristics of ‘cyanosis of eisenmengerization’? A-Cyanosis of eisenmengerization is: - Mild - Clubbing is never more than grade II. Q-What is the survival after eisenmengerization? A- 80% survive 10 years post diagnosis 77% survive for 15 years & 42% for 25 years. Q-What features, in eisenmengerization, are associated with a poor outcome? A-A poor outcome is expected if the patient has: 1) History of syncope 2) RV dysfunction 3) Low CoP 4) Severe hypoxemia Q-What precautions should be observed for patients with eisenmengerization? A-These patients should avoid: 1) Intravascular volume depletion 2) Heavy exertion 3) High altitude 4) Vasodilators 5) Pregnancy Q-Discuss management policies for eisenmengerization? A-They are: 1) IV prostacyclin (epoprosterol) 2) Phelbotomy with isovolumic replacement
- 159. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 159 PALLIATIVE SURGERY IN CYANOTIC Q-Enumerate midline palliative procedures for cyanotics? A-They are: 1) BT shunt 2) Waterston Cooley shunt 3) Gazenneiga shunt 4) Glenn shunt 5) Davidson’s shunt (direct anastomosis of MPA to aorta) 6) Brock’s procedure (infundibulectomy only thru’ a pursestring in RVOT) 7) McGoons procedure (patch widening of the MPA, RPA & LPA) Q-What are the shunts that can performed thru’ a left lateral thoracotomy? A-They are: 1) BT shunt- classical & modified 2) Potts shunt 3) Benson Roe procedure (anastomosis of LAA to vertical vein for palliation of TAPVC)- historical Q-What palliative surgeries can be performed thru’ a right thoracotomy? A-They are: 1) Right BTS 2) Blalock Hanlon atrial septectomy 3) Waterston shunt Q-Describe the chronology of ‘palliative procedures’ of CCHD. A-The following are the procedures arranged in chronological order: - Classical BTS: 1944 - Pott’s shunt: 1946 - Davidsons shunt: 1956 - Glenn shunt: 1958 - Waterston shunt: 1962 - Waterston Cooley shunt: 1966 - Gazzenega shunt: 1976 - Modified BTS: 1981 Q-Discuss important points of each shunt. A- Classical BTS: - If on right side, after transection of the Rt. SCA, it is taken out of the loop of the right recurrent laryngeal nerve & then anastamosed to RPA. - Take down: dissect posterior to SVC & loop
- 160. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 160 Modified BTS: - On right side mediastinal pleura is opened posterior to SVC & phrenic nerve - Azygous vein is ligated & divided - Takedown: On the right side: Graft generally lies just posteromedial to SVC, which is dissected, looped & ligated/ divided. On the left side: dissect beneath the arch of aorta & above the LPA or open the left pleura & dissect from the lateral aspect, then dissect for the peel over the PTFE conduit. A plane (well developed) between the peel & the conduit is isolated & graft is looped & ligated/ divided. Waterston shunt: Shunt between the posterior ascending aorta & anterior LPA thru’ a right lateral thoracotomy. - anastomosis posterior to SVC Problems of Waterston shunt; 1) size of shunt- if small then cyanosis, if large then CCF 2) distortion of RPA & preferential flow to one lung Takedown: on CPB there are 3 ways, either dissect the shunt & loop or loop RPA & LPA; - incise the native suture line followed by primary closure of the aorta & patch plasty of the RPA - open the aorta & examine from inside (Cooley) - transect aorta & repair RPA Waterston Cooley shunt: anastomosis is done between aorta & RPA, anterior to SVC Potts shunt: between descending aorta & posterior LPA Problems: are 1) increased flow- leading to CCF 2) decreased flow- leads to cyanosis 3) LPA aneurysm 4) Difficulty in takedown Takedown: There is high risk of air embolism when descending aorta is opened hence the technique followed is; - CPB- aortic or femoral arterial - Digital occlusion of the shunt from the outside for preventing pulmonary flooding & more effective cooling - Circulatory arrest- cross clamp & cardioplegia - Carotids are snared - LPA opened anteriorly & the opening of the shunt is closed with a PTFE patch.
- 161. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 161 - Flow is reinitiated & deairing done( if femoral arterial cannula then deairing is from cardioplegia needle, if aortic cannula then deairing is from the LPA- descending thoracic aorta suture line) Q-What are the indications for a BTS? A- Indications are: 2) CCHD not fit for ICR, with severe symptoms 3) TOF with pulmonary atresia 4) TOF with - Unresolved spell - Age < 6 mnths with low weight/ failure to thrive/ repeated spells - Hypoplastic PA - Underdeveloped LV (< 60% of normal) - MV annulus < -2 ‘Z’ - Institutional criteria for performing an ICR 7) TGA with PA banding for later arterial switch Q-What essential investigations are required prior to carrying out an emergency BT shunt in a child with unresolved spell? A-They are: 1) Hct (SOS blood letting to obtain Hct of around 65%) 2) Platelet function & count 3) Echo examination for - PA size, - PA confluence - Side of arch Q-What is the anesthesia protocol during BTS? A-Induction is with Ketamine (2- 10 mg/Kg). Take IV line with utmost care (no air injected). Q-Why is a modified BTS preferred, by many, on the same side as arch? A-Due to: 1) Longer length available of SCA before it branches 2) Lesser chances of damage to recurrent laryngeal nerve. Q-Damage to which artery is dangerous during dissection of SCA? A-Damage to the vertebral artery as it will cause retraction of the artery into the vertebral foramen. Q-Why “as proximal LPA” as possible for a BTS? A-The reasons are: 1) There is more equal distribution of blood flow & 2) It is easy to loop from midline (for later closure during an ICR)
- 162. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 162 Q-During a left BTS what structure may be lying in front of the LPA? A-A large lymph node Q-During a BTS how many branches of distal LPA are to be looped? A-3 (2 of upper lobe & 1 of lower lobe.) Q-Discuss strategies if LPA is not seen during BTS? A-The options are: 1) Check dissection 2) Open pericardium & anastomose to MPA 3) If large MAPCA seen entering hilum- a shunt to the MAPCA 4) Close & turn patient to opposite side Q-What are the cause of bradycardia on clamping the LPA? A-The reasons maybe: 1) RPA absent/ osteal stenosis/ hypoplastic/ non confluent 2) Isolated left lung ventilation 3) Vagus nerve included in the clamp. Q-What measures are to be taken if bradycardia occurs? A- 1) Check bilateral ventilation 2) Allow re-expansion of lung & then start 3) Check inclusion of vagus in clamp 4) Try side clamping the artery 5) BTS to upper lobar artery. Q-What is the size of Goretex to be used for a MBTS? A- 1) A Protocol by age followed at our institute is: - if < 6 mnths- 4 mm - 6mnths to 2 years- 5mm - 2 to 6 years- 6mm - > 6 years- 8mm 2) Protocol by weight (at JJH) - < 7 Kg- 4mm - 7 to 12 Kg- 5mm - 12- 20 Kg- 6mm - > 20 kg- 8mm 3) Graft size by body weight & BSA (Miki, Ueda) Diameter of graft = 1.88 (body weight) + 1.8 = 0.87 (BSA) + 5.3 [Note:However the decision for the size of Goretex is ultimately based on the size of the SCA]
- 163. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 163 Q-What is the concept of Qb/Qs? A- (Qb- flow thru’ shunt, Qs= systemic blood flow) Ideal Qb/Qs [by Miki, Ueda (Ann Thorac Surg 1987)] is 30- 40%. Ideal Qb index is= 1.6- 2.4 litres/ min/ m2. Q-What care should be taken with Gore-Tex? A-The following precautions should be followed. 1) Cut with a sharp knife 2) Do not crush 3) Avoid multiple punctures. Q-What are the alternatives if Gore-Tex is not available for a BTS? A-The options are: - Classical BTS - Use maternal saphenous vein - Use Dacron Q-What are Gore-Tex sutures? A-They are hygroscopic & hence clog the needle holes Q-What is the management of an “on table” cyanotic spell? A-Clamp the descending thoracic aorta (acts like “squatting”). Q-Discuss intraoperative techniques to ensure patency of graft? A-The following techniques should be followed: - Taking all sutures under vision - All sutures inside-out on the artery - Lie & length of graft should be appropriate. Q-What is the technique of air removal after a modified BTS? A-The clamps over distal PA & distal SCA are released - followed by proximal PA & the proximal SCA clamps (never needle puncture Goretex as it will lose its electronegativity). Q-What are the signs of good shunt functioning? A-They are: a) Graft related- - sweating - thrill over PA b) Hemodynamics related- - improvement in O% - fall in DBP
- 164. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 164 Q-What are the reasons for an absent thrill post BTS? A-Reasons are: 1) High Hct 2) Low BP 3) Small SCA (ligate distal SCA) 4) Blocked shunt During redo BTS: - 1st perform SCA anastomosis & then PA anastomosis - ensure adequate heparinization - heel first - inside out sutures over the artery Q-What are the changes occurring after a BT shunt? A-They are: 1) Symptomatic improvement 2) PA- - PA size grows (by 25%)# - Increase in annular size (due to increased pressure on the sinus of valsalva) # #-all within the first 6 months 3) LV develops- normalizes 4) Infundibular obstruction worsens 5) Hct decreases & coagulation profile normalizes 6) Collaterals close Q-What should not occur post BTS? A-The following should not occur: - cyanotic spells & - CCF Q-How long does Hct take to normalize post BTS? A-Around 15 days. Q-What is the incidence of systemicopulmonary shunt causing irreversible increase in PVR? A-It is as follows: - BT shunt: Rare, < 10% incidence at 5 years post op - Central shunt: Nearly 30% incidence at 5 years post op. Q-What are the advantage of a modified BTS over a classical BT shunt? A-Advantages of modified BTS are: 1) Decrease chances of distortion of- PA & SCA 2) Less dissection 3) Blood supply to arm is maintained
- 165. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 165 Q-Is there any difference in the incidence of CCF in modified BTS and classical BTS? A-Both have the same incidence; as the flow limiting factor is the subclavian artery. Q-What are the e/o previous BTS on X-ray? A-Any of the following may be present. Evidence of thoracotomy: - rib crowding - synostosis/ callous formation - subperiosteal resection Evidence of dissection: - elevation of dome of diaphragm Evidence of functioning shunt: - normalization of pulmonary vasculature - MPA prominent - LV developed Q-What is the indication for repeat BT shunt? A-A blocked shunt Q-Why a repeat BTS is not performed on the same side? A-Because increased adhesions will be present & hence a higher tendency for bleeding. Q-What are the possible reasons for a BT shunted patient devoloping symptoms later? A-The possibilities are: 1) Patient has outgrown shunt 2) Shunt is blocked, due to - thrombosis - neointimal hyperplasia - infective endocarditis 3) PA distortion 4) Intracardiac cause- AR/ PR Q-Why are the symptoms more severe (in comparison to preoperative) if a BTS gets blocked? A-Because - Infundibular obstruction has become worse - Collaterals have closed Q-What are the ways of closure of BT shunt, during an intracardiac repair? A-Options are: 1) Dissect on inner side of arch & loop 2) On CPB, open MPA & suture opening from the inside 3) Ligate SCA
- 166. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 166 Q-What is the disadvantage of a BTS performed thru’ a thoracotomy? A-Due to a thoracotomy there is increased collateral formation. These may interfere during and post intracardiac repair if a Fontan operation has been performed.
- 167. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 167 CARDIAC CATHETERIZATION Q-What is conversion factor of mm of Hg? A-1 mm Hg= 1.36 cm H2O= 133 Pascals= 1334 dyne.cm-2. Q-What are the normal pressures, in various chambers, during cath? A- (all in mm Hg) RA a= 6 v= 5 mean= 3 LA a= 10 v= 12 mean= 8 PA S= 25 D= 9 Mean= 8 Aorta S= 130 D= 70 Mean= 85 RV S= 25 D= 4 LV S= 130 D= 8 Q-Who performed the first right heart catheter? A-Forsmann (German who directed urological catheter into his own RA) Q-Who performed the first left heart catheter? A-Zimmerman (1947) Q-What is the D/D of catheter in RA? A-The possibilities are: 1) Constrictive pericarditis 2) Tricuspid atresia 3) Ebstein’s anomaly Q-What is the D/D of a RA-RV-aorta catheter? A-The possibilities are: - TOF - DORV - D TGA - Proximal AP window Q-When on cath is a ventricle anterior? A-A catheter is in the anterior ventricle when it lies just behind the sternum & no portion of the cardiac silhouette is in front of it.
- 168. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 168 Q-Describe diagnosis based on ‘desaturation at a chamber level’? A-In a patient undergoing cardiac cath if there is: Level Diagnosis -Desaturation at ventricular level: TOF -Desaturation at atrial level: TOF with ASD with high RVEDP -Desaturation at PV level: lung pathology, Pulmonary AV fistula -All chambers have the same saturation: TAPVC -LVOT saturation is more than aorta: TGA, Taussig Bing anomaly Q-What are the requirements to call pressure in RV & LV as equal? A-If the pressures are measured simultaneously, they should be equal. If they are measured by the ‘pull back’ technique, the difference should be within 10 mm Hg. Q-What are the indications for cath in a neonate? A-The indications are: 1) TOF with PA 2) PA with intact IVS 3) Evaluation of PV drainage. Q-What are the angiographic features of PA hypertension? A-They are: 1) Increased background haze 2) Arborization 3) Withertree appearance Q-A LV angiography in, PA view, is for what pathology? A-AV canal defect. Q-What are the cath techniques for calculating LV/ RV volumes? A-There are 3 systems, viz., 1) Simpson rule 2) 2 chamber method 3) Area length method Q-What is the Simpson rule? A-It is for calculating the RV volume. The RV image, in AP & Lateral view, is divided into even number of segments (1,2….10) of width ‘h’ as In AP= X0, X1, X2……X10 In Lateral= Y0, Y1, Y2…..Y10 Volume of segment 0= /3 x X0 x Y0 x h Sum total of all the segments will give the RV volume
- 169. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 169 Q-What is the 2 chamber method? A-For calculating RV volume. RV shoot in lateral view is taken. Volume of infundibulum (cylinder)= r2h Volume of body (ellipsoid)= 4/3 r2 (LL/2) r= radius of ellipsoid LL= largest length RV volume= sum of infundibular & body volumes Q-What is the Area-length method? A-For calculating the LV volume. Volume= 4/3 x r(AP) x r(lat) x (LL/2) r(AP)= radius in AP view r(Lat)= radius in lateral view Q-What are normal RV & LV volumes? A-They are: Normal LVEDV (in ml)= 72.5 x BSA Normal RVEDV (in ml)= 75.1 x BSA Q-What is the normal position of IVS? A-Normally is LAO 60 but in c-TGA is anteroposterior. [Note:One cannot determine the shunt direction on a ventricular shoot, as the force of injection is very powerful.] Q-Onplain fluoroscopy how will one determine that the catheter is in LV & not in RV? A-In lateral view the catheter will overlap the spine. Q-What are the catheters for PA? A-They are: 1) Berman (balloon tipped catheter) 2) Grollman PA seeking catheter Q-What are the views taken during cath, for TOF? A-The views are: - For LPA- LAO - For RPA- RAO - RVOT- RAO - Coronary- LAO caudal - Lateral view for- IVS, infundibulum, relation of great vessels, coronary crossing RVOT. Q-Howmuch contrast is normally injected? A-5 cc/ Kg.
- 170. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 170 Q-Which catheters are used for cardiac cath in TOF? A-Venous catheters- Berman (Balloon tipped), NIH Arterial- Pigtail 6F= 2mm diameter, 7F= 2.3 mm diameter Q-Describe specific cath findings in TOF? A-The specific findings are: Oximetry- there is a step down of oxygen saturation at ventricular level & further step- down at the ventriculoaortic level. Pressure- There is equalization of peak systolic pressures of LV & RV with a gradient across the RVOT. Q-What are the indications for cath in TOF? A-Cath is performed in TOF for: 1) PA anatomy 2) MAPCAS 3) Coronary crossing RVOT 4) Additional VSD Q-What are the indications for LV angiography in TOF? A-They are: 1) Additional VSD 2) LV function (performed in adults) 3) Aortic override 4) Aortomitral continuity Q-What are the possibilities of a catheter not entering PA in a TOF? A-The possibilities are: 8) Severe PS 9) Pulmonary atresia 10) Posteriorly placed PA Q-In TOF, why RVOT shoot is performed in RAO? A-Because 1) The overlapping spine is taken away from the RVOT 2) Parietal & septal bands are well seen Q-Which is the view for estimating PA ratio’s? A-LAO cranial. Both the PA’s and the descending aorta are well seen in this view. Q-What is the use of lateral view in TOF? A-It is to visualize the RVOT & IVS [Note: The PA cannot be seen well in the lateral view. The RPA will be seen as a coin & the LPA as a comma.]
- 171. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 171 Q-How to determine the extent of aortic override on cath? A- - In lateral X-ray (LAO): a line is drawn from the center of aorta & if it falls - On IVS- 50% override - On left side- < 50% override - On right side- > 50% override Q-What is a significant MAPCA on cath? A-If the MAPCA is: - > 2.5- 3 mm, - Has the same pressure as the aorta - Supplies a significant portion of the lung. Q-What are the complications of cath in TOF? A-They are: 1) Vascular injury, hemorrhage & hypothermia 2) Induce hypoxic spell 3) Arrhythmia- late RV failure 4) Infective endocarditis Q-Can PA angiography be done by PV route? A-Yes, by PV wedging & then injecting the contrast.
- 172. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 172 CORONARY Q-Describe drug treatment post CABG. A-Mnemonic for drug treatment post CABG. ABCDE A- Antianginal & Aspirin B- β blockers & blood pressure controlling C- Cholesterol & cigarettes D- Diet & Diabetes E- Education & Exercises Hence the drugs that are generally started are: - Aspirin +/- clopidogrel - Lipid lowering- if LDL > 130 without diet or > 100 with diet - ACE inhibitors if CHF, LV dysfunction (EF < 40%), hypertension, diabetes - β blockers Q-What are the accepted serum lipid values under the NCEP guidelines? A-The values are: - LDL < 100 mg/L - TG< 150 mg/L - Total cholesterol < 200 mg/ dl - HDL > 50 mg/ dl Q-What are angina equivalents are? A-They are: 1) Dyspnea 2) Fatigue 3) Faintness 4) Erructations Q-Briefly describe the profile of coronary artery disease in Indians? A-In Indians; - CAD is 7 times more common than Chinese - First myocardial infarction is 5 years earlier than west - 2 times more incidence of triple vessel disease Prevalence of CAD is: 96.7/ 1000 persons. (Krishnaswami, Chennai, IHJ 2002) WHO prediction is that by 2010, 60% of the coronary artery disease patients will be from India Reasons implicated for above are: 1) Faulty diet 2) Higher incidence of diabetes & higher prevalence of insulin resistance patterns 3) High lipoprotein A levels- which in turn lead to high LDL, low HDL & higher triglycerides
- 173. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 173 4) Barker’s hypothesis- states that the basic problem lies with the malnourished mother, which leads to stress on the fetus. This causes over stimulation of neurohumoral responses thus giving rise to diabetes, hypercholesterolemia etc. Q-What is the critical area for maintenance of coronary blood flow? A-75% Q-Is there a circadian variation for myocardial infarction? A-Yes. Maximum myocardial infarctions are seen between 9-11 AM. Reason:Believed to be due to increased BP & altered platelet activity. Q-What is preoperative optimization of status in a patient for CABG? A-It includes: 1) Stoppage of smoking, if not completely, atleast till 1 week prior to surgery 2) Maximal treatment for angina 3) Treatment of hypertension/ diabetes/ renal insufficiency/ COPD Q-What are the nomenclatures in coronary angiography? A-They are: CASS- coronary artery surgery study TIMI- thrombolysis in myocardial infarction BARI- bypass angioplasty revascularization investigation Q-Describe TIMI flow. A-There are 4 grades of TIMI flow. They are: Grade III- prompt antegrade flow with rapid filling Grade II- slowed filling but complete vessel opacified Grade I- small amount of flow but incomplete opacification of distal vessel Grade 0- No contrast flow Q-Who performed the 1st coronary angiography? A-Mason Sones (in 1962) Q-Who performed the 1st angioplasty? A-Andrea Gruntezig (in 1977) Q-What are the catheters for CAG? A-They are: 1) Judkins (separate for right & left coronary) 2) Amplatz (separate for right & left coronary) 3) Multipurpose (same for both) Q-Which is the single best view for coronaries in CAG? A-RAO caudal
- 174. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 174 Q-Why are multiple views taken for the same vessel? A-It is for visualization of eccentric plaques. Q-Which plaques are more prone to rupture? A-Eccentric plaques are more prone to rupture than concentric plaques. Q-What angiographic findings are present in a left main osteal stenosis? A-The following findings may be present: 1) No reflux 2) Eccentric reflux 3) ECG changes/ patient complaining of angina 4) Ventricularization of tracing. Q-What is the % of dominance of coronary artery circulation & discuss criteria for dominance? A- 75% are RCA dominant: PDA from RCA & a branch beyond to LV 10% are co-dominant: PDA from RCA but no branch beyond to LV 15% are LCA dominant: PDA from LCA Q-What is the origin of SA nodal artery? A-It can be varying. In 55% it is from RCA while in 45% it is from left circumflex artery. It is never from left main or LAD. Q-How is LV function classified? A- > 40% Fair 25- 40% Moderate < 25% Low Q-What are the AHA guidelines for CAG? A-They are: 1) Male: > 35 years age 2) female: post menopausal or > 35 years with risk factors 3) chest pain 4) e/o ischemia 5) previous coronary artery disease Q-Which is the commonest congenital coronary anomaly? A-ALCAPA Q-Which is the commonest coronary anomaly in adults? A-Origin of left circumflex artery from right sinus or RCA.
- 175. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 175 Q-In a patient requiring CABG + MVR, which should be performed first? A-CABG first, because; 1) Delivery & even distribution of cardioplegia possible 2) No need to lift the heart for OM’s, which may lead to a tear in the AV groove (if a prior MVR has been performed) Q-What is Anrep effect? A-It is also called homeometric auto regulation. It is a positive inotropic effect following abrupt elevation of systolic aortic pressure. Q-Which is the most susceptible portion to ischemia & what is its significance? A-The subendocardial region is most susceptible to ischemia. It is so because it receives its blood supply only during diastole. In systole the intramyocardial vessels are squeezed & hence get shut. The outer shell of LV & the entire RV (later due to lesser compressive force) maintain the blood supply during systole too. Hence the endocardial blood flow depends upon Dp- diastolic pressure & Dt- diastolic time Additionally, prolonged CPB impairs the subendocardial microcirculation because all the pump oxygenator systems produce particulate emboli, which preferentially go to the subendocardium. Also, in a fibrillating arrested heart, the subendocardium suffers maximum ischemia. Q-Which is the inotrope of choice post CABG? A-It is dobutamine because it is a: 1) Good inotrope 2) Decreases SVR (hence decreasing afterload & increased diastolic filling) 3) Does not cause vasospasm Q-Why is SNP not preferred after CABG? A-Because SNP may cause, 1) Coronary steal syndrome 2) Side effects of cyanide/ thiocynate Q-What are the unchallenged indication of CABG? A-They are: 1) Left main > 50% 2) Triple vessel disease (each more than 70%) Q-What are the indications for CABG? A-AHA 1999 guidelines are as follows: A)In symptomatic or mild angina Class I: 1) Significant left main disease 2) Left main equivalent ( 70% proximal LAD & left circumflex artery)
- 176. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 176 3) Triple vessel disease (survival benefit is better in patients with abnormal LV function) Class IIa: 1) Proximal LAD with 1 or 2 vessel disease Class IIb 1) 1 or 2 vessel disease not involving proximal LAD B)In stable angina Class I: 1) Significant left main disease 2) Left main equivalent ( 70% proximal LAD & left circumflex artery) 3) Triple vessel disease (survival benefit is better in patients with LVEF < 50%) 4) 2 vessel disease with significant proximal LAD disease & either - EF < 50% or - Demonstrable ischemia on non invasive testing 5) 1 or 2 vessel disease without significant proximal LAD disease but large area of viable myocardium & high risk criteria on non invasive testing 6) Disabling angina despite maximal medical treatment, when surgery can be performed with acceptable risk Class IIa: 1) Proximal LAD with single vessel disease 2)1 or 2 vessel disease without significant involvement of proximal LAD, but with moderate area of viable myocardium & demonstrable ischemia on noninvasive testing Class III: 1) 1-2 vessel disease without proximal LAD involvement in patients with mild symptoms, unlikely to be due to myocardial ischemia or not received adequate trial of medical treatment & a) Have a small area of viable myocardium or b) No demonstrable ischemia on noninvasive testing 2) Borderline stenoses (50-60%) in location other than left main & no demonstrable ischemia on non invasive testing 3) Insignificant (<50%) stenoses C) In unstable angina/ non q wave myocardial infarction Class I: 1) Significant left main disease 2) Left main equivalent ( 70% proximal LAD & left circumflex artery) 3) Ongoing ischemia not responsive to maximal non surgical treatment. Class IIa: 1) Proximal LAD disease with 1-2 vessel disease Class IIb: 1) 1 or 2 vessel disease not involving proximal LAD D) In ST elevation (q wave) myocardial infarction: Class I: None
- 177. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 177 Class IIa: 1) Ongoing ischemia/ infarction not responsive to maximal non-surgical treatment ClassIIb: 1) Progressive LV pump failure with coronary stenosis compromising viable myocardium outside the initial infarct area 2) Primary reperfusion in the early hours (6-12 hours) of an evolving ST segment elevation myocardial infarction Class III: 1) Primary reperfusion late (> 12 hours) in evolving ST segment increasing myocardial infarction without ongoing ischemia E) In poor LV function Class I: 1) Significant left main disease 2) Left main equivalent ( 70% proximal LAD & left circumflex artery) 3) Proximal LAD with 2 or 3 vessel disease Class IIa: 1) Poor LV function with significant viable, non contracting revascularizable myocardium without any of the aforementioned anatomic patterns Class III: 1) Poor LV function without e/o intermittent ischemia & without e/o significant revascularizable myocardium. F) In life threatening ventricular arrhythmias Class I: 1) Significant left main disease 2) Triple vessel disease Class IIa: 1) Bypassable 1 or 2 vessel disease causing life threatening ventricular arrhythmias 2) Proximal LAD disease with 1 or 2 vessel disease Class III: 1) Ventricular tachycardia with scar & no e/o ischemia G) After failed PTCA Class I: 1) Ongoing ischemia or threatened occlusion 2) Hemodynamic compromise Class IIa: 1) Foreign body in crucial anatomic position 2) Hemodynamic compromise in patients with impairment of coagulation system & without previous sternotomy Class III: 1) Absence of ischemia 2) Inability to revascularize owing to target anatomy or no reflow state
- 178. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 178 H) With previous CABG Class I: 1) Disabling angina despite maximal noninvasive treatment Class IIa: 1) Bypassable distal vessel with a large area of threatened myocardium on noninvasive testing Class IIb: 1) Ischemia in non LAD distribution with patent internal mammary artery to LAD graft and without aggressive attempt at medical treatment &/or percutaneous revascularization Q-What are dilated coronary arteries a feature of? A-Of: 1) SVAS 2) HOCM 3) Coronary A-V fistula Q-Which are the various arterial grafts used for CABG? A-The can be classified as: 1) Somatic - Internal mammary artery - IEA - Subscapular artery 2) Splanchinic - GEA - Inferior mesenteric artery - Splenic artery 3) Limb - Radial - Ulnar [Note:Other grafts that can be used are: - Veins - Permaflow (PTFE) - Bovine carotid - Bovine internal mammary artery] Q-What are the advantage of the internal mammary artery? A-Internal mammary artery is: 1) Pedicled 2) Has less muscle, hence less prone to spasm 3) Endothelium releases prostacyclin, hence less atherogenic 4) Artery size is similar to the size of the coronary artery 5) Ability to alter flow according to the need of the myocardium 6) It reaches all coronaries
- 179. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 179 Q-Which is the most vulnerable period for a ventricular fibrillation? A-In the period post myocardial infarction the heart is most vulnerable for VF. Occurs if an ectopic occurs in the midportion of ‘T’ wave (as some portion of the ventricular myocardium is depolarized & some incompletely or completely repolarized.) Q-What are the branches of internal mammary artery? A-The branches are: 1) Pericardiophrenic artery 2) Anterior intercostals arteries: 4- 10 in number 3) Sternal branches: 4- 10 in number 4) Perforating branches: 3- 6 in number 5) The artery terminates by: - bifurcating (in 93%) into - superior epigastric - musculophrenic artery - trifurcating (in 7%) - superior epigastric - musculophrenic artery - diaphragmatic branch Q-How to test adequacy of internal mammary artery flow on table? A-Flow should be more than 90 ml/ min. Q-What measures are to be taken if the internal mammary artery does not have a good flow? A-The possibilities and the subsequent action are: 1) In spasm- instill papaverin in surrounding tissues 2) Check entire length for occlusion & test luminal patency with metal dilator 3) Check for perforators (especially 2,3 & 4th, which may be large & steal blood) 4) Check for pericardiophrenic artery Q-What are the complications of internal mammary artery harvesting? A-The complications are: 1) Injury to the phrenic nerve 2) Deep dull retrosternal pain# 3) Rarely breast necrosis (# it is believed to be due to cautery burning of the anterior intercostals arteries which conduct the heat to the nerves in the intercostals spaces, causing neuralgia. Hence some advice to use clips on either side & cut in between) Q-What are the contraindications for harvesting internal mammary artery? A-They are: For unilateral IMA harvesting: 1) Definitive: subclavian artery stenosis 2) Relative: emergency CABG [to a) save time, b) inability to perfuse ima graft, c) adverse effect due to use of postoperative vasoconstrictors]
- 180. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 180 For bilateral IMA harvesting: (all relative contraindication) 1) COPD 2) Diabetes 3) Old age Q-What is coronary artery steal syndrome? A-When blood is taken away by 2nd, 3rd, & 4th perforating branches and pericardiophrenic artery. Q-What are the advantages of radial artery? A-They are: 1) Good length 2) Adequate caliber 3) Good handling characteristics 4) It is even normally subjected to systemic pressure (cf with reversed saphenous vein graft) Q-How is the aorta, during CABG, exmained for plaques? A-By: 1) Palpation 2) If adventitia is adherent to media or inflamed, there are high chances of plaque 3) Epiaortic doppler/ TEE Q-What are the step to be taken if ascending aorta is atherosclerosed? A-The following can be done. 1) Use only internal mammary artery & use a LIMA-RIMA/ Radial Y 2) Graft to right subclavian artery 3) If aorta is being clamped, clamp the carotid before aortic clamping & declamping Q-Why during CABG an ‘inside out suturing technique on coronary’ is preferred? A-Because: 1) Any intimal disruption or plaque will be plastered to the vessel wall 2) Graft patency is ensured Q-What actions are to be taken if post onbypass CABG patient is not coming off bypass? A-Firstly check the following: - K+ - Temperature - Acidosis -if possible check PCWP & cardiac index & accordingly - inotropes +/- vasodilators - amrinone/ milrinone - IABP
- 181. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 181 Q-What are the patency rates of radial artery? A-The patency rates are: Tatoulis: 1 ½ -year patency of 90% Acar: 5-year patency of 83%. Q-Is the degree of coronary artery stenosis related to patency rates of grafts? A-Yes. If coronary artery stenosis > 70%- 1 year patency is 95% If coronary artery stenosis < 70%- 1 year patency is 75% Q-Technique of ‘on table’ dilatation of the radial artery? A-Diltiazam 5 mg or Papaverine 20 mg added to 20 ml warm normal saline/ heparinised blood is used for dilatation. The dilatation should be at a pressure less than the systemic. Q-What are the indications for coronary endartrectomy? A-A coronary endarterctomy is performed in a severely & diffusely diseased artery with distal portion unsuitable for grafting. Q-What are the contraindications for a coronary endartrectomy? A-They are: 1) Aneurysmal coronary artery 2) < 2 mm diameter coronary artery 3) Small non dominant vessel 4) Non viable myocardium Q-Why is myocardial infarction common following coronary endartrectomy? A- Probably due to: 1) Dissection of blood outside the remaining plaque leading to luminal occlusion 2) Occlusion of branched coronary artery 3) Thrombosis of artery due to raw surface Q-What are contraindications for a redo-CABG? A-They are: 1) Irradiation of anterior mediastinum 2) Lack of conduits. BATISTA Q-When was Batista procedure first described? A-In 1996. It is also called as partial left ventriculectomy. Q-What is the concept of the Batista operation? A-It is based on the Laplace’s law, wherein the radius & thickness of the wall determine the stress on the wall. Decreasing the radius- concept of Batista operation Increasing the thickness- concept of Cardiomyoplasty
- 182. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 182 Q-In how low EF can a Batista be performed? A-As low as 5 %. Q-Who are the candidates for the Batista procedure? A-Those with dilated cardiomyopathy (secondary to idiopathic/ ischemic/ rheumatic causes) with LVED (D) > 70 mm. Original procedure was performed on beating heart. Now is performed on an arrested heart. Q-What are the steps of the Batista procedure? A- Intraoperative TEE is a must for: LVID, imterpapillary muscle distance, EF, MR Procedure includes - Resection of LV wall - AML & PML are stitched in the center using a 4/0 prolene stitch (Alferi & Fucci stitch) to prevent MR - Annuloplasty ring implanted Q-What is the difference between Batista & aneurysmectomy? A-In Batista, viable but overdistended muscle tissue is excised while in an aneurysmectomy the scar is removed. Q-What is described as the ‘medical’ Batista procedure? A-The use of Carvedilol. Q-What is Myosplint? A-It a concept described by McCarthy. It involves reducing the dilated LV cavity (along the outflow tract) into 2 parts. This results in the formation of 2 cylinders, of lesser diameter, hence lesser tension on the wall. Q-What is an Acorn wrap? A-The ventricles are wrapped in an elastic bag, which prevents over distension of the ventricle & additionally the elastic recoil aids in contraction. Q-Describe the uses of skeletal muscle in cardiac surgery? A-The following are the uses of skeletal muscles. 1) Skeletal cardiomyoplasty - posterior wrap: Carpentier - Anterior wrap: Magovern 2) Skeletal muscle ventricle 3) Diastolic counterpulsation by placing in - ascending aorta - descending aorta
- 183. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 183 IABP Q-Who introduced IABP? A- Concept was by Moulopolous & Clinical application was by Kantrowitz. Q-What is the Shuttle gas used for IABP? A-Either of the following is used. 1) Helium- preferred as it has a low viscosity, enabling rapid inflation & deflation 2) CO2- it is highly viscous but has a better safety margin than helium (as it dissolves rapidly) Q-What is the site of insertion of IABP by the percutaneous technique? A-Femoral artery: - The stronger pulse side, - It should be free from PVD - Free from scarring Always below the inguinal ligament, as manual hemostasis is extremely difficult above the ligament. Q-What are the other sites of insertion of IABP? A-They are: 1) Aortic pursestring 2) Axillary- to make patient ambulatory ( as a bridge to transplant) 3) Iliac 4) Abdominal aorta 5) PA (for PA counterpulsation) Q-What is the action of IABP? A-It has 2 folds action, viz.: 1) Inflation during diastole causing augmentation of diastolic pressure (at dicrotic notch) 2) Deflation just prior to systole allowing distal runoff, hence deceasing the afterload. Q-What are the criteria for IABP insertion? A-They are: 1) CoP < 1.8 litres/ min/ m2 2) SBP < 90 mm Hg 3) Mean BP < 60 mm Hg 4) LAP > 20 mm Hg 5) Urine output < 20 ml/ hour 6) SVR > 2100 dynes.sec.cm-5
- 184. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 184 Q-What is the anticoagulation policy with an IABP in situ? A-Either of the two: 1) Heparin to keep APTT 1.5 to 2 times or ACT between 200 – 250 sec 2) LMW Dextran 40- max 10 ml/ Kg/ day Q-What are the contraindications for IABP? A-The contraindications can be classified an absolute & relative. Absolute 1) AR 2) Dissection Relative 1) Liver dysfunction 2) Renal dysfunction 3) Sepsis 4) Children Q-What are the problems of IABP in children & discuss the methods to counteract them? A-The are summarized in the table below. Problem Counteraction 1 Vascular access Intraop thru’ the aortic cannulation site (neonates & infants) 2 Increased elasticity of the aorta Not found to be a significant problem 3 High heart rate Cooling of the patient in the ICU, to decrease HR has been found effective 4 Balloon size Available 5 Absence of coronary artery disease - Q-How to wean a patient ‘off’ IABP? A-The augmentation is reduced gradually to 1:4 & 50% balloon inflation. Later the patient is kept for 1/2 hour on flutter mode and then is the balloon removed. Q-What is the technique of removal of IABP? A-After removal apply immediate manual pressure for atleast 30 minutes & then a sandbag for 8 hours ‘or’ perform a surgical closure of the arteriotomy Q-What is a Double balloon catheter? A-It has a smaller distal balloon (which inflates slightly earlier than the upper main balloon) for more effective augmentation. Q-What is the ‘Fail-safe’ mechanism of IABP? A-In case the IABP develops a problem; the balloon will stop in the ‘deflated’ position.
- 185. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 185 Q-What measures are to be taken if, while on IABP, limb ischemia develops? A-The options are: 1) Remove & insert on the opposite side 2) Femorofemoral cross over graft Q-Can IABP be used as PA balloon counterpulsation? A-Yes. It can be used in RV failure. The criteria are: - CVP/ RAP > 25mm Hg - LAP < 15 mm Hg - SBP < 90 mm Hg - Cardiac index < 1.8 L/min/m2 Above all in the presence of a competent tricuspid valve TMLR Q-Where has the concept of TMLR originated? A- - Vineberg: direct implantation of internal mammary artery in myocardium - PK Sen: needle acupuncture of heart - Baffi: implatation of T tubes with long limb into LV Q-What are the indications of TMLR? A-They are: 1) Distal coronary artery disease 2) Diffuse coronary artery disease 3) No conduits 4) As hybrid procedure Q-What are the various routes for TMLR? A- 1) Thoracotomy 2) Thoracoscopy 3) Percutaneous Q-Describe the procedure of TMLR? A-It is as follows: - 1 mm holes at distance of 1 cm - Administered at peak of ‘R’ as there is no electrical activity & the heart is distended - TEE for bubble formation in LV cavity, marking the end point - Application of digital pressure to control bleeding
- 186. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 186 Q-What are the prerequisites for TMLR? A-They are: 1) Presence of viable myocardium 2) TEE Q-What are the mechanism of action of TMLR? A-TMLR is believed to benefit patient by: 1) Direct blood flow thru’ the channels created 2) Neovascularization due to inflammation 3) Denervation- leading to relief of angina. Q-What are the shortcomings of TMLR? A-They cannot be done on the IVS & diaphragmatic wall (later only via percutaneous route) Q-What are the complications of TMLR? A-They are: 1) Bleeding 2) MR 3) Arrhythmias Q-What are the contraindication for TMLR? A-They are: 1) LV aneurysm 2) Bleeding diathesis 3) Ventricular arrhythmias
- 187. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 187 CONSTRICTIVE PERICARDITIS & TUMORS CONSTRICTIVE PERICARDITIS Q-What is the etiology of constrictive pericarditis? A-The possible causes are: 1) Idiopathic 2) Tuberculosis 3) Dressler’s syndrome 4) Radiation 5) Uremia 6) Drug induced- procainamide/ hydralazine 7) Post operative (especially if Betadine washes used- Miller & Mansoor, Ann Thorac Surg 1982, showed a 20 times higher incidence of postoperative constrictive pericarditis with betadine washes) [Note:All conditions causing acute pericarditis can cause subsequent constrictive pericarditis except rheumatic carditis.] Q-What are the cath signs of constrictive pericarditis & discuss its D/D with restrictive cardiomyopathy. A-The cath signs of constrictive pericarditis are: 1) RA mean pressure > 10 mm Hg - Mild: 10- 15 mm Hg - Moderate: 15- 20 mm Hg - Severe: > 20 mm Hg 2) Equalization of diastolic pressures in all the 4 chambers (within 5 mm Hg) [in restrictive cardiomyopathy the LVEDP (PCWP) is > 5 mm Hg higher than the RVEDP] 3) RVEDP > 1/3rd RVESP [in restrictive cardiomyopathy RVEDP < 1/3rd RVESP] 4) Positive square root sign 5) Positive Kussmauls sign 6) Thickness of pericardium on fluoroscopy > 5 mm 7) Fluid challenge (500- 1000 ml of normal saline over 6-8 minutes) will lead to persistent elevation in CVP 8) Endocardial biopsy [in restrictive cardiomyopathy will show an infiltrative pathology] 9) Pulmonary hypertension will be negative [in restrictive cardiomyopathy will be positive] 10) RV angiography will show blunting of apex (Ballet Dancers shoe)
- 188. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 188 Q-Discuss echocardiography D/D between restriction and constriction. A-The differences observed are: Restrictive Constrictive 1) Septal bounce - + 2) LV thickness + - 3) EF decreased normal 4) Early diastolic decreased normal filling 5) Changes with - + respiration Q-What are the types of pericardiectomy? A-Pericardiectomy maybe classified as: Radical: pericardium is removed from all surfaces of the heart & over intrapericardial major vessels Adequate/ total/ extensive: Pericardium over the RV & LV (including anterolateral & diaphragmatic surfaces) removed but RA, PV’s & cavae are left alone Partial: leave the diaphragmatic wall & anterolateral wall. CARDIAC TUMORS Q-Describe Echo classification of LA myxomas? A-Charuzi’s classification. Class I- small tumor that prolapses thru’ the MV Class II- small, non-prolapsing tumor Class III- large tumor prolapsing thru’ the MV Class IV- large tumor without prolapse Q-What is a tumor plop A-A heart sound typically heard after S2. It probably represents the tumor striking the myocardium during rapid diastolic filling phase Q-What is the commonest tumor of the heart? A-Myxoma Q-Describe myxomas? A-Origin- mesenchymal cells. Seen commonly in females in the 3rd, 4th of 5th decade. Consists of the classic triad of: 1) Constitutional symptoms (fever, malaise, arthralgia, myalgia, weight loss) 2) Hemodynamic problems (like MS) 3) Embolization Myxoma diagnosed is an indication for surgical excision (due to high chances of embolization)
- 189. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 189 Q-What is the commonest site for myxomas? A-LA> RA> RV > LV > valves. Q-What is the recurrence rate after excision of myxoma? A-The incidence of recurrence is 1-5% (within 2 ½ years). It is believed to be due to: 1) Inadequate resection 2) Spillage & implantation 3) Multicentricity Rate of re-recurrence is nearly 25% Q-What is the commonest tumor of heart in a child? A-Rhabdomyosarcoma Q-Which is the commonest cardiac malignancy? A- 1) Secondaries form lung/ breast 2) Primary: Angiosarcoma
- 190. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 190 AORTA, LUNG & MEDIASTINUM ANEURYSM Q-What are the current recommendations, for surgery, on patient with aneurysm aorta? A-They are: 1) All symptomatic 2) Asymptomatic if - > Twice the size of normal contagious aorta - > 5 cm diameter for ascending aorta, > 5 cm for arch, > 6 cm for descending aorta - Documented enlargement of the aneurysm - Progressive AR in c/o an ascending aortic aneurysm Q-Describe the classification systems for dissection of aorta. A-The various systems are: 1) Debakey- Type I, II, IIA & IIIb 2) Stanford- A & B (given by Daily et al) 3) Applebaum- ascending & descending 4) Meng- Anterior & posterior Q-What is etiology of ascending/ arch aortic aneurysm? A-They are: 1) Marfans, Ehler Danlos (leading to cystic medial necrosis) 2) Syphilis 3) Arteriosclerosis 4) Chronic dissection 5) Mycotic aneurysm 6) Arteritis Q-What is the etiology of descending thoracic aortic aneurysm? A-They are: 1) Atherosclerosis 2) Same as above [Note:Clot formation in an aneurysm confers no benefit or protection against rupture.] ASOV Q-What is the etiology of ASOV? A-The causes maybe: 1) Syphilis 2) Medial necrosis 3) Atherosclerosis 4) Rarely endocarditis Q-What is the advantage of a bicameral approach for RASOV? A-A missed VSD will be detected.
- 191. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 191 PULMONARY Q-What is the normal relation of the domes of the diaphragm to each other? A-In: 95%: right side is high 4%: Equal 1%: left side is high Q-Discuss on table ‘feasibility’ of going ahead with a pneumonectomy. A-Assess in the following way: 1) Preoperative PFT valves 2) Clamp the pulmonary artery - if hypotension, bradycardia: indicates RV failure - Decrease in O% < 95% Then the patient will not withstand pneumonectomy 3) Needle proximal to he clamp & measure the PAP. If PAP > 30 mm Hg, impending RVF. Q-Which segments of the lung are prone to herniation A- UL: Anterior segment LL: Superior, medial & posterior Q-What is the division of zones of lung on a X-Ray? A-The zones are: Till 2nd rib (anteriorly)- upper zone 2nd to 4th - middle below 4th - lower zone Q-What is the importance of zones? A-It gives: 1) Idea about lobe 2) Idea about lesion, Eg: TB- generally upper, hydatid- generally middle, Bronchiectasis- generally lower Q-Who described segmental anatomy of lung? A-Boyden. Q-What is the D/D of air cyst on X ray? A-It is as follows: If hairline thickness: pneumatocele If increased thickness: Simple lung cyst, TB, malignancy
- 192. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 192 Q-What is the D/D of a cavity on CT scan? A-Depends upon wall thickness. If the thickness is: < 1mm- pneumatocele 1-3 mm- abscess > 3mm- TB/ malignancy Q-What is the D/D of lung cyst in infant/ children? A-They are: 1) Congenital lobar emphysema 2) Congenital lung cyst (generally lower lobe) 3) Congenital cystic adenomatoid malformation 4) Sequestration cysts 5) Pneumatocele Q-What is the commonest cause of pneumatocele in children A-A resolving pneumonia. Q-What is the commonest cause of multiple pneumatoceles in neonates? A-Seen in neonatal staphylococcal pneumonia. Q-What measures are to be taken, if on single lung ventilation, the PO2 falls? A-The normally the set parameters during one lung ventilation are: 1) FiO2= 100% 2) Tidal volume= 12- 15 ml/ Kg 3) High respiratory rate 4) PEEP If the PO2 falls (critical level is 65 mm Hg, which is the shoulder of the O2- dissociation curve), the measures to be taken are: 1) Check above adjustments of ventilation 2) Intermittent inflation of the clamped lung 3) Partial inflation with CPAP 4) Clamp PA 5) Use of perflourocarbons, to increase the O2 carrying capacity of blood 6) Abandon procedure Q-What are the indications for extraperiosteal rib resection? A-They are: 1) Tuberculosis 2) Malignancy 3) Cervical rib Q-Define Emphysema? A-Abnormal dilatation of air spaces distal to the terminal non respiratory bronchiole with destructive changes of the alveolar wall.
- 193. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 193 Q-Define Bulla? A-A large emphysematous air cavity > 2.5 cm in diameter. Q-What are the diagnostic criteria for emphysema on X-Ray? A-Consider emphysema if the following features are present: 1) > 8 intercostal spaces are seen 2) if a vertical line is drawn from the highest point of the diaphragm dome to a line joining the ipsilateral costophrenic & cardiophrenic angle, is < 1.5 cm (in adult) Q-What are the indications for surgery for Bulla? A-They are: 1) Spontaneous pneumothorax 2) Giant bulla (> 30% of the hemithorax) Q-What does popcorn calcification on X Ray suggest? A-Indicative of hamartoma Q-Surgery is the first choice of management in which lung condition? A-In 1) Aspergilloma 2) Hydatid cyst 3) Tumor Q-Medical management is the first choice of management in which lung conditions? A-In 1) Lung abscesses 2) Bronchiectasis Q-What are the indications for an urgent thoracotomy post trauma? A-Indications are 1) Initial ICD > 1500 ml blood 2) > 200 ml/ hour blood in ICD for 4 hours 3) Tamponade 4) Need for direct cardiac massage 5) Massive clot collected in the thorax 6) Known injury to; - esophagus - heart - great vessels - diaphragm 7) Significant chest wall defect 8) Massive air leak s/o tracheal/ bronchial rent
- 194. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 194 Q-What are the accessory muscles of respiration? A-The accessory muscles of respiration are: 1) Sternomastoid & trapezius 2) Scalenus anticus 3) Pectoralis major 4) Alae nasi 5) Latissimus dorsi & intercostals muscles (causing intercostals retraction) [Note:The above muscles are arranged in the order in which they are generally recruited] Q-Who introduced double lumen tubes A-Bjork & Carlens. Q-What is the difference between Carlen & Robertshaw tubes? A-Carlen’s tube has a carinal hook. Q-Who introduced the Univent tube A-Inoue. Q-What are the causes of pneumothorax A-The are: 1) Primary- bleb 2) Secondary- to a) COPD b) Cystic fibrosis c) Congenital d) Pneumonia e) Endobronchial block f) Tuberculosis 3) Traumatic 4) Iatrogenic 5) Therapeutic Q-What are the types of high frequency ventilation A-3 types 1) High frequency positive ventilation 2) High frequency jet ventilation 3) High frequency oscillation Q-What are the types of Jet ventilation A-2 types 1) Injector jet ventilation (uses a large TV of 500- 1500 ml at a slow rate of 10-30 breaths/ min) 2) High frequency jet ventilation (injects a small TV of 50- 250ml at a high rate of 60- 600 breaths/ min)
- 195. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 195 Q-What are the uses of jet ventilation A-It is used during: 1) Bronchoscopic procedure 2) Airway surgery. Q-Discuss incidence & types of Bronchopleural fistula A- Incidence is 1- 4% of pneumonectomy/ lobectomy (4% for stapled closure Vs 12% for manual closure) Types of bronchopleural fistula are: - Early (1-2 days to 7 days): generally due to poor surgical technique - 8-10th day to < 2 weeks: due to failure of healing or occasionally empyma - > 2 weeks: infection/ empyma Q-What is Occult bronchopleural fistula? A-There is no expectoration of pleural fluid A fall in the pleural fluid level of > 1.5 cm should arouse suspicion. Theories implicated for same are: 1) Subconscious swallowing of fluid 2) Absorption of the fluid by the parietal pleura due to increased intrathoracic pressure Q-What are the factors favoring development of bronchopleural fistula? A-The factors are: Local factors; 1) Long stump (leading to accumulation of secretions) 2) Poor bronchial blood supply 3) Technique of closure (stapled Vs non stapled) 4) Failure to provide tissue cover of irradiated or diseased bronchus 5) Sepsis General factors; 1) Underlying disease 2) Nutrition Q-Discuss strategy for treatment of bronchopleural fistula. A-The treatment consists of: Nutrition/ proteins + correction of anemia + Antibiotics +/ - Surgical closure
- 196. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 196 Q-What are the ways of closure of bronchopleural fistula? A-They are: 1) Resuture proximally, preferably using staples & cover the suture line with muscle/ pericardial/ omental flap 2) Use fibrin glue for small leak 3) Transsternal transpericardial approach 4) Right posterior approach for left main bronchus 5) Completion pneumonectomy 6) All of the above +/- thoracoplasty Q-Discuss Mediastinal tracheostomy. A- Indication: If resection of the larynx & trachea is being performed for cure or palliation Procedure: 1) Pull the trachea to surface ‘or’ 2) Create a complex skin tube to trachea However 1) & 2) are prone to failure due to separation of suture lines, sepsis & osteomyelitis of sternum. Hence the technique now preferred is: 3) Removal of head of clavicles, upper portion of sternum & medial ends of 1st & 2nd ribs and then constructing an extrapleural skin conduit to the tracheal stump. Q-What are the indications of VATS A-They are: Diagnostic: - tissue diagnostic: pleural, pulmonary, Mediastinal - indeterminate pleural effusion Therapeutic: - Pleuropulmonary: control effusion, empyma drainage, bullous disease - Esophageal: myotomy, cysts, antireflux surgery - Mediastinal: thymectomy, cysts, masses - Cardiac: internal mammary artery- coronary artery anastomosis - Others: sympathectomy, paravertebral abscess Q-What is the basic setup for VATS? A-VATS requires: 1) General anesthesia 2) Double lumen ET 3) A standby open thoracotomy tray 4) Thoracoscope (10mm preferred) 5) 2 high resolution monitors 6) 2 to 5 port accesses 7) Videoscope instruments 8) Endoscopic staplers 9) Adequate suction & smoke evacuation system
- 197. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 197 Q-Define Thoracoplasty A-The operative removal of the skeletal support of the portion of the chest Q-What are the types of Thoracoplasty A- 1) Conventional: Alexander’s thoracoplasty Originally 3 stage. Now 1 stage surgery is performed. Excise 7 ribs (generally leaving the 1st rib) & allow the scapula to fall inside 2) Bjórks osteoplastic thoracoplasty 3) Sawamura modified thoarcoplasty: debride empyma cavity, close bpf & perform subperiosteal rib stripping. Now place ICD in empyma cavity & close allowing the periosteum & muscles to fall onto the obliterated cavity 4) Plombage thoracoplasty (obsolete)- using paraffin, Lucite spheres, fiberglass 5) Schede’s thoracoplasty Q-Which is the commonest pulmonary disease due to a fungus? A-Aspergillosis. Q-What are the types of lesions seen in aspergillosis A-They maybe: 1) Allergic 2) Local- simple/ complex 3) Systemic/ invasive Q-What is an Aspergilloma A-It is a sphere consisting of hyphae + inflammatory cells + fibrin + epithelial cell debris. It is highly friable Q-What is the source of infection? A-Is by inhalation (present on damp bread) Q-Can other fungi cause aspergilloma A-Yes. Rarely Nocardia Q-What are the underlying lung disorders causing formation of aspergilloma? A- 1) TB 2) Bronchogenic Ca 3) Lung cyst 4) Brochiectasis Q-Discuss diagnosis of aspergillosis. A-Diagnosis of aspergilloma is on - sputum/ bronchoalveolar lavage- stain & culture - X-ray: Halo sign Crescent sign with movement of ball on posture
- 198. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 198 Q-What is the medical treatment of aspergillosis? A-It consists of: -Amphotericin B (1- 1.5 mg/ Kg/ Day) Indicated in: - poor surgical candidates - invasive aspergillosis - empyma Q-Discuss bedside PFT’s? A-They include: 1) Portable spirometer 2) Peak flow meter (normal is 450- 750 L/min) 3) Schnider test: at 1 foot distance a burning candle is kept & the person is asked to blow it with the mouth completely open 4) Breath holding time (< 45 sec is significant) TUBERCULOSIS Q-What is burden of TB in India? A-In India: - More than 40% of the population is infected with the TB bacilli - 2 million cases of TB/ year - 500,000 deaths from TB/ year - Each untreated patient infects 10-15 person/ year Q-What is the technique of sputum collection? A- - 5-10 ml of deep respiratory expectorate specimen with no nasal secretions or saliva x 3 days - If no sputum produced then nebulization with hypertonic saline - Still no sputum obtained then brochoscopic collection of specimen - In children or rarely in adults, who are unable to bring out sputum, gastric lavage Q-What are the culture media for TB? A- 1) Egg based - Lowenstein Jensen - ATS media 2) Agar based - middlebrook media 7 H 10 - middlebrook media 7 H 11 3) Liquid media 4) Selective media (LJ graft)
- 199. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 199 Q-Discuss BACTEC. A-it is liquid middlebrook 7H12 + 14C labeled palmitic acid for radiometric detection of growth. 0.5 ml of specimen is inoculated into BACTEC 12B bottle. When the organisms grow, the 14C is released into the headspace of the bottle, which is detected by a sensor. Q-What are the staining techniques for TB bacilli? A-At least 105 organisms/ ml should be present. Techniques are: - Carbol Fuschin- ZN staining, Kiryoun - Auramine dye Q-Discuss Mantoux test. A- 0.1 ml of PPD is injected intradermally on the ventral aspect of the forearm using a 26/ 27 no. needle, with the bevel facing upwards. A weal of 6- 10 mm diameter is made. Test reading: 48- 72 hours later & it depends upon the presence or absence of induration, on touch, and the diameter is measured (and not on visual erythema) Q-What is the molecular detection of TB. A-By nucleic acid amplification method, viz., 1) Amplified mycobacterium tuberculosis test (MTD) 2) Amplicor M. tuberculosis test Q-Discuss the current management strategy of TB. A-DOTS (Directly Observed Treatment Shortcourse) Category Criteria Initial Therapy Continual Therapy Category I (all new severe) -new smear +ve PTB -New smear –ve PTB with Xray e/o extensive destruction -extrapulmonary TB 2 x H3R3Z3E3 4 x H3R3 Category II -relapse -failure -discontinuation 2 x H3R3Z3E3S3 + 1 x H3R3Z3E3 5H3R3E3 Category III -milder PTB -other extrapulmonary TB 2 x H3R3Z3 4 x H3R3 [Note:Intrapulmonary cases (under DOTS) also include: 1) Pleural effusion 2) Hilar/ mediastinal lymphadenopathy 3) Pericardial involvement 4) Meningeal 5) Spinal.
- 200. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 200 Q-What are included under ‘mediastinal TB’ in the DOTS regimen? A- 1) Pleural effusion 2) Hilar/ mediastinal lymphadenopathy 3) Pericardial involvement Dosages of the drugs are: Drug Drug Dosage in DOTS Thrice a week (mg/Kg) Dosage in per day regimen (Mg/ Kg) H Isoniazid 10 5 R Rifampicin 10 10 Z Pyrazinamide 35 25 E Ethambutol 30 15 S Sterptomycin 15 15 Q-Discuss anti-TB treatment in special conditions? A- Pregnancy: All drugs may be administered except streptomycin Lactation: All drugs may be administered Liver failure: Drugs not to be administered, in the order of significance are; - Pyrazinamide - Isoniazid - Rifampicin Renal failure: Drugs not to be administered, in the order of significance are; - Streptomycin - Ethambutol Q-What are the chief side-effects of the antitubercular drugs A-They are: Isoniazid Hepatitis Neuritis Rifampicin Hepatitis Pyrazinamide Hepatic failure Hyperuricemia Ethambutol Optic neuritis Renal toxicity Streptomycin Renal failure Ototoxicity
- 201. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 201 Q-What is the management policy if there is drug induced hepatitis? A- Stop all drugs Let hepatic failure resolve Start all (if mild hepatitis) Do not include pyrazinamide/ isoniazid Q-Which anti tubercular drugs are bacteriostatic & which are bacteriocidal A- Bacterostatic drugs are: 1) Isoniazid 2) Ethambutol Bacterocidal drugs are: 1) Rifampicin 2) Pyrazinamide 3) Streptomycin Q-What are the newer antitubercular drugs? A-They include: 1) Flouroquinozoles - Ofloxacin - Sparfloxacin - Ciprofloxacin 2) Aminoglycosides - Amikacin - Kanamycin - Kapriomycin - Rheomycin 3) beta lactams - Clavulanic acid + amoxycillin - Sulbactum 4) pyridine analogues - Ethionamide - Prothionamide 5) Cytokines - IL 2 - IL 10 - IL 12 6) Macrolides - Azithromicin - Erythromycin - Raxithromicin - Clarithromicin 7) Clofazime
- 202. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 202 Q-What is the source of TB pericarditis A-It could be from: 1) Adjacent structures 2) Lymphogenous 3) Hematogenous Q-What is the incidence of TB pericarditis? A-1% of all TB [Note:There is a high incidence of coexistent pleural effusion] Q-Discuss the diagnosis of TB pericarditis. A- Signs: effusion, muffled heart sounds, rub In large effusions there will an area of dullness at the angle of left scapula. Ewart’s sign: tubular breathing at the angle of the left scapula (due to compression of the underlying lung) ADA levels: Generally seen 100 IU/L Vs 20 IU/L (Abnormal Vs normal) If it is > 40 IU/ L- it has a sensitivity & specificity of 93% & 97% Q-What are the signs of active pulmonary TB on a CT scan A-They are: - Tree in bud appearance - Cavity with fungal ball - Pleural effusion - Granuloma Q-What are the signs of active TB on X Ray A-They are: 1) Cavity with or without fungal ball (generally in the posterior segment of upper lobe or superior segment of lower lobe) 2) Lymph nodes (especially in children) 3) Hydropneumothorax 4) Spontaneous pneumothorax 5) Consolidation 6) Military pattern OTHER MEDIASTINAL Q-What is the staging of Corrosive ingestion A-(Endoscopic staging) Stage 1: Mucosal hyperemia Stage 2a: Superficial ulcers Stage 2b: Deep ulcers Stage 3: Necrosis Stage 4: Stage 3 + systemic metabolic derangements
- 203. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 203 Q-Discuss the management of corrosive ingestion. A- Stage 1 & Stage 2 conservative in form of: - NBM - Parentral nutrition or nasoduodenal or feeding jejunostomy Patient can start eating in- Stage 1= day 0 Stage 2a= day 25 Stage 2b= day 35 Stage 3 (if luminal continuity present)= day 45 - Antibiotics - Corticosteroids (role is debated) - Repeat endoscopy after 4 weeks & assess. The options are- 1) Dilatation 2) Surgery required response may be a) good response b) dilatation not possible c) 50% recurrence within 1 year wait for another 8 weeks (total for 12 weeks post injury) Excision & colonic transposition via a thoracotomy (as excessive periesophgeal scarring shall not permit a transhiatal procedure) Stage 3 & 4 require surgery -extent of damage to stomach is assessed thru’ a laparotomy & - if stomach is viable: jejunostomy performed - if stomach necrosis: transhiatal esophgectomy + cervicostomy & jejunostomy + drainage of mediastinal space. -both followed 12 weeks later with colonic transposition Q-What are the various fundoplication procedures? A-They may be classified as complete & incomplete. Complete: 1) Nissen’s fundoplication 2) Rosetti modification 3) Donahue modification Incomplete: 1) Belsey Mark IV 2) Toupet partial plication 3) Watson partial plication 4) Lind partial plication.
- 204. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 204 Q-What is Heimlich maneuver A-A technique of applying sudden thrust of pressure over the upper abdomen (& stomach) & lower thorax, leading to increase in the intraesophageal & intrathoracic pressure & thus ejection of a blunt esophageal or tracheal foreign body Q-Classify esophageal atresia? A-Classification by Gross. Type I: only esophageal atresia Type II: esophageal atresia with proximal tracheoesophageal fistula Type III: esophageal atresia with distal tracheoesophageal fistula Type IV: esophageal atresia with proximal & distal tracheoesophageal fistula Type V: only tracheoesophageal fistula Q-What are most frequent complications after correction of esophageal atresia? A- 1) hypertrophic subpyloric stenosis 2) gastroesophageal reflux 3) tracheomalacia Q-What is the Cervicothoracic sign A-When a mass in the thorax is extending above & crossing the clavicle. If the superior margin is well defined then it belongs to the anterior mediastinum & if the superior margin is ill defined then it belongs to the posterior mediastinum. Q-What are the types of thymectomies? A- 2) Simple thymectomy 3) Masaoka’s extended radical thymectomy 4) Jaretzki’s thymectomy Q-What are the approaches for thymectomy? A-Thymectomy maybe performed by any of these approaches. - Midsternotomy: partial & complete - transcervical - VATS
- 205. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 205 TRAUMA & CPR TRAUMA Q-Which is the commonest site of aortic injury after blunt trauma? A- 1) Isthumus (90- 95%), or 2) Just above aortic annulus Q-What are the X-ray finding of above? A-The findings are: 1) Widening of the mediastinum, i.e., figure of 8 or width mediastinum/ width chest wall ratio > 0.25. 2) Right deviation of trachea or of nasogastric tube 3) Presence of fluid level in left pleura Q-In which conditions, despite the need of an immediate surgery for aortic injury, surgery may be deferred? A-If it is associated with: 1) Severe head injury 2) Burns 3) Sepsis CARDIOPULMONARY RESUSCITATION Q-Describe ideal chest compression. A-Ideal chest compression should be; - with a board underneath the chest - 100 times high impulse compression/ minute (AHA recommendations) Q-What are the theories behind “chest compression”? A-Chest compression is believed to benefit by: 1) Cardiac pump mechanism: due to cardiac compression 2) Thoracic pump mechanism: due to increased intrathoracic pressure there is cardiac output generated Q-What are the other techniques of chest massage? A-Chest massage maybe given using: 1) Pneumatic vest 2) Interposed abdominal compression (functions like IABP) 3) Active chest compression & decompression with a custom hand held suction device 4) Open heart massage
- 206. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 206 Q-What is the commonest cause of death, post CPR, that is missed? A- 1) Ischemic bowel 2) Pulmonary embolism Q-Discuss controversy in CPR? A- 1) NaHCO3: it is believed that NaHCO3 administration is of no benefit, but only increases problems due to - Shift of O2 dissociation curve to left - Hyperosmilarity - Hypernatremia - Paradoxical acidosis by increased CO2 2) Calcium: excess can cause altered metabolism Q-Which is the most specific indicator of successful endotracheal ventilation? A-ETCO2 (100% specific)
- 207. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 207 X-RAYS Q-What are features of Right Atrium enlargement? A- - > 5.5 cm from midline - > 1 vertebrae from midline - > ½ vertebrae from the lateral sternal border - Ratio of RA to mediastinal height > 50% Q-What are features of Left atrial enlargement? A- - Enlargement of LAA (straightening of the left heart border) - Double atrial shadow - Widening of the carinal angle - Posterior displacement of the esophagus Q-What are features of Aneurysmal LA? A- - Right CTR > 60% - Carinal angle > 120 - Left bronchus/ trachea < 0.4 - LA inferior border touches the diaphragm - LA size (AP) > 65 mm (echo) - LA volume > 1 litre (echo) Q-What are the features of Pulmonary arterial hypertension? A- - Dilatation of the MPA, LPA & RPA (RPA > 10- 15mm in males & > 9- 14mm in females), prominent MPA conus - RPA to its first lobar branch (if > 6:1- indicated increased flow, if > 7: 1- indicates severe PH with obliterative changes) - Arterial- bronchiolar ratio > 1.2/ 1 - Perivascular cuffing - Withertree appearance - Increased background haze Q-What are the features of Eisenmengerization? A- - Peripheral pruning: no markings in lateral 1/3rd while less in middle 1/3 rd) - Lack of arborization - Dilated PA till inner 1/3rd
- 208. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 208 Q-Discuss features of pulmonary venous hypertension. A-Depending upon the severity of venous hypertension, the various features are: LAP=13- 17 mm Hg: - cephalization of PV’s (antlers sign or the inverted moustache sign) - upper lobar vein > 3 mm in the 1st ICS LAP=18- 25 mm Hg: Interstitial edema in form of - Kerley’s B lines (interlobar lymphatics) - Kerleys C lines (in center of lung fields) LAP >25 mm Hg: - alveolar edema - hazy fluffy infiltrates Hemosiderosis Q-Describe features of LV enlargement? A- - On frontal X Ray: apex is below the diaphragm & forming an obtuse marginal - On lateral X ray: Hoffman Reigler sign: posterior wall of silhoute projects beyond the IVC - Supporting: e/o LAE & pulmonary venous hypertension Q-What are the features of RV enlargement? A- - Frontal X Ray: apex is upturned & forming an acute angle - On Lateral X Ray: if the anterior cardiac border is in contact with > ½ of the sternum - Supporting: e/o PA dilatation Q-What is the feature of biventricular enlargement? A- - LV on frontal X Ray & RV on lateral view. Features are as described above. Q-What are the features of constrictive pericarditis? A- - Frontal X Ray: penicilling of the heart border - Lateral X Ray: summation of calcification (predominantly over the RV)
- 209. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 209 VASCULAR VASCULAR CASE EXMINATION PROFORMA: INSPECTION 1) Color 2) Signs of ischemia - Decrease in amount of hair & thin hair - Loss of subcutenous fat - Shininess of skin - Trophic changes in nail- brittle & transverse ridges - Ulceration of skin 3) Beurgers postural test- The angle at which the limb becomes pale & vein empty is called the Beurgers angle. If it is < 30°, it indicates severe ischemia. Now if the foot is lowered, a cyanotic hue will form within 2- 3 minutes. 4) Capillary filling time- elevate the limb & then lower and ask the patient to sit up. In a normal person there is no pallor. In a person with severe ischemia; the capillary filling will take more than 30 sec. 5) Gangrene PALPATION 1) Palpate all peripheral pulsations. 2) Skin temperature. 3) Capillary filling- decreased in ischemia, increased in AV fistula (Harvey’s sign) 4) Fuschig’s test- Cross the legs→ seen for limb movement of crossed leg with pulsations. If pronounced- popliteal artery aneurysm & if absent- normally seen or absent pulsations. 5) For upper limb: - Adson’s test (& reverse Adson’s test- believed by some to be more specific than Adson’s test) - Roos test - Costoclavicular compression test - Hyperabduction test - Arm claudication Q-What is Brown’s vasomotor index? A-It is an index used for determining the role of sympathectomy. Technique: Nerve block with a local anesthetic & then the following is calculated. (Rise of skin temperature- Rise of mouth temperature)/ Rise of mouth temperature If > 3.5- sympathectomy is beneficial. Q-What are the signs of DVT? A-Signs of DVT are: 1) Homans sign- pain on forced passive dorsiflexion 2) Moses sign- tenderness on calf compression side to side. 3) Bancrofts sign- tenderness on anteroposterior compression 4) Lowenberg sign- pain after inflation of cuff around the calf to 80 mm Hg.
- 210. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 210 Q-What are the clinical categories of acute limb ischemia? A-The categories are: Sensory loss Muscle weakness Doppler Arterial Venous Viable nil nil + + Threatened Marginally Minimal (toes) nil - + Threatened Immediately More than toes, rest pain Mild to moderate - + Irreversible Anaesthetic Major tissue loss - - Q-What are the clinical categories of chronic limb ischemia? A-The categories are: (Fontaine’s classification) Fontaine’s grade Catego ry Clinical Objective criteria 1 0 Asymptomatic Normal treadmill test# 2 1 Mild Can complete treadmill AP after exercise> 50 mm Hg But 25 mm Hg less than SBP 2 Mod claudication 3 Severe claudication Cannot complete treadmill. AP after exercise < 50 mm Hg 3 4 Ischemic rest pain Resting AP< 40 mm Hg TP < 30 mm Hg 4 5 Minor tissue loss Resting AP< 40 mm Hg TP< 40 mm Hg 6 Major tissue loss #- For 5 min at 2 mph at 12° incline AP- Ankle pressure TP- Toe pressure Q-Describe the tests for thoracic outlet syndrome. A- 1) Adson’s test/ scalene test: Technique: deep breath, hold, extend the neck fully & turn the face to the same side obliteration or diminution of pulse. Mechanism: tightening of the anterior & middle scalene muscles leads to a decrease in the interscalene space & this magnifies the preexisting compression on the subclavian artery or brachial plexus. 2) Costoclavicular test/ military position test Technique: The shoulder is drawn downward & backwards change in radial pulse & symptoms. Mechanism: Narrowing of the costoclavicular space by approximation of the clavicle against the 1st rib.
- 211. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 211 3) Hyperabduction test Technique: Arm in hyperabduction to 180. Mechanism: The components of the neurovascular bundle are pulled around the pectoralis minor tendon, coracoid process & head of humerus. Any other obstruction will cause further pressure on the bundle. 4) Roos test Technique: The arm is raised to 90 position with the limb externally rotated out producing appearance of symptoms. 5) Arm claudication test Technique: Arm is raised to horizontal position & elbow is flexed to 90, the hands are exercised leading to appearance of symptoms. Q-What is the significance of Ankle brachial index (ABI)? A-Normally the SBP of the ankle is higher by 12-24 mm Hg as compared to brachial. Hence the normal ABI of a resting patient in supine position is 1.1 (lowest normal= 0.92) BHJ, 1973, described the following findings of significance: -Calf brachial index values of: < 70% indicate complete block < 40% indicate severe ischemia, with resultant rest pain -Thigh/ brachial index (cuff around thigh) values of: > 120% No significant aortoiliac block 80- 120% Significant aortoiliac block < 80% Complete iliac block Q-Describe the classification of prosthetic graft infection. A-The various classifications are: 1) Depending upon time of appearance after implantation Early- < 4 mnths Late- > 4 mnths 2) Relation to extent of wound infection (Szilagyi’s classification) Grade I- cellulites of wound Grade II- Infection of subcutaneous tissue Grade III- Infection of the vascular prosthesis 3) Depending upon the extent of peripheral (P) graft involvement (Bunt’s classification) P0- Infection of cavitary graft- interposition P1- Infection of graft whose entire course is not cavitary- axillofemoral, femorofemoral P2- Involvement of extracavitary portion of the graft with an intracavitory origin- aortofemoral P3- Infection of a prosthetic patch angioplasty- carotid endartrectomy
- 212. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 212 Q-What are the advantages of insitu SVG? A-The advantages are: 1) Large diameter to proximal artery 2) If tributaries, the vein can be used as a - bifurcated graft - double length graft 3) Intact vasavasorum (but as both ends are transected, the most important vasae are destroyed) 4) Increased production of prostacyclin (this factor has a definite advantage in below knee anastomosis) 5) Can use small diameter SVG (2.5- 4mm) which otherwise would not have been used. Q-Describe the important steps of ‘insitu SVG’? A-The important steps are as follows: - Remove valvar obstruction - Control tributaries ( by- the null flow technique of using Doppler probe or – intraop phlebography) - Mobilze ends for construction of anastomosis Q-What is the minimum time required for collaterals to develop angiographically after an acute arterial occlusion? A-6 hours Q-Why do collaterals open in ischemia? A-Ischemia causes local acidosis causing release of substance P. This in turn leads to the opening up of collaterals. Q-What are the modifications of PTFE? A-They are: 1) Goretex (thin walled) 2) Stretch PTFE 3) Impraflo (thick walled with coil support) 4) Carboflo (carbon coated) 5) Tapering grafts Q-What is Dacron? A-Polyethylene terephthate. Q-What is Weslowski unit A-Described by Weslowski from NewYork. It is the amount of water that can pass thru’1 cm2 area of a graft material, at 120 mm Hg, in 1 minute. Ideal implant porosity - < 50 WU Ideal ingrowth porosity- 4,000- 5,000 WU
- 213. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 213 Q-Classify aortoarteritis? A-The various classifications are: 1) Modified Nasu classification Type I- aortic arch & its branches Type II- descending thoracic aorta & its branches Type III- abdominal aorta & its branches Type IV- Extensive involvement of aorta & its branches Type V- Ascending aorta only Type VI- Branches of aorta only 2) Radiological classification Type I- Occlusive Type II- Constrictive Type III- diffuse irregularity Type IV- diffuse dilatation Type V- Aneurysmal Type VI- combination of above Q-What are the indications for lumbar sympathectomy A-The indications are: 1) Causalgia 2) Severe rest pain with poor response to analgesics & revascularization is not possible 3) Reflex sympathetic dystrophy 4) Beurgers disease 5) Hyperhydrosis Q-What are the causes of unequal carotid pulsations? A-Unequal carotid pulsations maybe seen in: 1) Supravalvar AS 2) Carotid artery stenosis Q-Describe the pathogenesis of atherosclerosis A-Response to injury theory (Ross 1973) There is cellular injury leading to dysfunction. This causes a change in the endothelial permeability, adhesive characteristic & abnormal growth responses. There is interaction of endothelium & smooth muscle cells with monocytes/ platelets/ T lymphocytes, which leads to fibroproliferative changes & eventually plaque formation. Q-What are the stages of atherosclerosis A- 3 categories of atherosclerosis are: Category 1: Fatty streak Category 2: fibrofatty lesion Category 3: Fibrous plaque
- 214. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 214 AHA staging (1995) Type I: Increase in number of intimal macrophages & lipid accumulation Type II: Fatty streak Type III: Type II + extracellular lipid pools Type IV: Atheroma (Type II + well defined collection of extracellular lipid in intima) Type V: formation of new fibrous connective tissue Type VI: complicated lesions, in form of; - surface defects (ulceration) - hematoma (hemorrhage) - thrombus Q-What are the criteria for diagnosis of TAO A-Criteria by Mill’s & Porter Major: 1) Distal ischemia < 45 years age 2) Tobacco abuse 3) Undiseased artery proximal to popliteal or brachial artery Minor: 1) Migratory superficial phlebitis 2) Raynauds phenomenon 3) Upper extremity involvement Q-What are the angiographic features of TAO A-They are: 1) Involvement of small & medium sized arteries a) Digital arteries b) Palmar, plantar, tibial, peroneal, radial, ulnar 2) Segmental occlusive arteries 3) There is more severe disease distally 4) Normal proximal arteries 5) Extensive collaterals around the occlusion (cork screw collaterals) Q-What are Windkessel arteries A-In the distal portion of the aorta & large arteries, the velocity of blood is greater in systole than in diastole. As these arteries are elastic, the forward flow is continuous because of the recoil during diastole, of the vessel walls, that have been stretched in systole. This is the Windkessel effect & the arteries called Windkessel arteries. Q-How is muscle power graded? A-Described by Robert Lovett in 1932 Grade 0: No power Grade 1: flicker of contraction Grade 2: movement with gravity eliminated Grade 3: movement against resistance, with gravity eliminated Grade 4: movement against resistance & also gravity Grade 5: normal power
- 215. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 215 DRUGS & FIRST’S DRUGS Adenosine Q-How is adenosine obtained? A-It is obtained by hydrolysis of c- AMP. Q-What are the types & actions of adenosine receptors? A-They are of 3 types A1- on myocytes: decrease the rate of depolarization A2a- in CNS: induce sleep A2b- on vascular endothelium: decrease platelet adherence & cause coronary vasodilatation A3- on mast cells: stabilize the cell membrane Q-What is the dose of adenosine A- 0.1- 0.2 mg/ Kg (max 12 mg) Q-What is the half life of adenosine? A-½ life is < 5 seconds. Q-What are the uses of adenosine. A-They are: 1) In CPB- immediately after cross clamping & during reperfusion 2) Correction of arrhythmias 3) Induce sleep (term ‘fatigue factor’) 4) For refractory PH Q-What drugs affect action of adenosine? Action is potentiated by dipyridamole Action inhibited by caffeine & aminophylline Q-What are its side effects? A-They are: 1) Headache & flushing 2) Arrhythmias Q-What are the contraindication for adenosine? A-Heart block & bradyarrhytmias Q-What is the antidote for adenosine? A-Aminophylline
- 216. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 216 Heparin Q-Who discovered heparin? A-McLean in 1916. Q-What is the mechanism of action of heparin? A-It requires the presence of antithrombin III for its action. Heparin binds to AT III brining about a conformational change converting AT III from a slow progressive thrombin inhibitor to a very rapid inhibitor. [Note:Only 1/3rd of the administered dosed of heparin binds to AT & this fraction is responsible for most of its anticoagulant effects.] Mechanism of action is as follows: 1) The heparin- AT III complex inactivates a number of coagulation enzymes; including Thrombin factor IIa, Xa, Ixa, XIa & XIIa. The major effects are due to inhibition of IIa & Xa. 2) Binds to heparin cofactor II & catalyses inactivation of IIa. 3) Binds to platelets- contributing to the hemorrhagic effects of heparin. XIIa ← AT III- heparin complex ↓ XIa ← AT III- heparin complex ↓ IXa ← AT III- heparin complex ↓ Xa ← AT III- heparin complex ↓ IIa ← AT III- heparin complex ↓ Fibrinogen → Fibrin - molecular size= 3.000 to 30,000 daltons (approx.=15,000 daltons) (- Mol wt. of LMWH= 5000 daltons_ Q-How is heparin cleared from the body & discuss the half life of heparin? A-High molecular weight moieties are cleared more rapidly than the low molecular weight moieties. Heparin is cleared by 2 mechanisms: 1) Rapid- binding to the endothelial cell receptors and macrophages, where it is depolymerised 2) Slower- renal. This makes the anticoagulant response to heparin non linear at therapeutic doses, with both the duration and intensity of the effect rising disproportionately with increasing doses. Thus the biological ½ life increases from 30 minutes with IV bolus of 25 IU/ Kg to 60 minutes with IV bolus of 100 IU/ Kg & to 150 minutes with a bolus of 400 IU/Kg.
- 217. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 217 Q-What conditions effect the action of heparin? A-Heparin action is potentiated in cirrhosis & action is depressed in pulmonary embolism. Q-What is 1 IU heparin? A-I IU of heparin is the amount of heparin that is required to maintain the fluidity of 1 ml of citrated sheep blood for 1 hour, at 37º C, with calcification. Q-What are the side effects of heparin? A-They are: 1) It decreases the SVR by decreasing the amount of ionized calcium. 2) DIC 3) Osteopenia 4) Heparin induced thrombocytopenia & heparin resistance Q-Discuss the protocol for management of a patient with post CPB non-surgical bleeding. A-Check for & correct: 1) Heparin- residual/ rebound 2) Platelet number & function 3) Coagulation factors 4) Activation of fibrinolytic system 5) Hypothermia & 6) Hypocalcemia. Q-What is the definition of heparin induced thrombocytopenia? A-Heparin induced thrombocytopenia is diagnosed if in a patient receiving heparin treatment: 1) The platelet count drops by 50% of the pretreatment levels, or 2) The platelet count drops to < 1 lac/ mm3 Q-What are the advantage of LMWH over unfractionated heparin? A-They are: 1) Due to low molecular weight, higher bioavailability by s.c. route, hence OD dosage suffices - bioavailability of LMWH (s.c. route)= 100% - bioavailability of unfractionated heparin (s.c. route)= 30% 2) Due to increased bioavailability, clinical effect is predictable & hence no need for repeated APTT monitoring 3) Lesser rate of thrombocytopenia, osteopenia & hemorrhagic side effects. Q-What are the disadvantage of LMWH? A-They are: 1) Lower antithrombotic properties 2) No drug to reverse its effect
- 218. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 218 Q-Enumerate heparin substitutes. A-They are: 1) LMWH 2) Medium MWH 3) High MWH 4) Dermatans (Danaparoid) 5) Heparans 6) Heparinoids (Lomoparon) 7) Murine polysaccharides Q-Which conditions can cause Heparin resistance? A-Heparin resistance maybe seen in: 1) AT III deficiency- congenital/ acquired 2) Prolonged administration- in unstable angina/ IABP 3) Septicemia 4) Pregnancy 5) NTG treatment Q-What is the management of heparin resistance? A-Any of the following measures (or combination) maybe adopted: 1) Administering higher dose of heparin (up to 1000 IU/ Kg) 2) Accepting a lower ACT (up to 420 sec) 3) Administering 2-3 unit FFP or AT III concentrate 4) Using hirudin/ danapariod. Nitric oxide Q-What is the source of NO? A- Endogenous- negligible Exogenous- from fossil, grains, NO donors (SNP, NTG etc) [Note:Nitric oxide is termed as “The winner & killer drug” (as high doses may cause fatal vasospasm)] Q-What is the half-life of NO? A-< 1 minute Q-Discuss NO delivery system. A-Special features of NO delivery are: - Special ventilators with 2 posts allowing NO & O2 mixture to occur only at the mouth of the endotracheal tube (If it comes in contact with O2, form NO2, which is toxic.) - Exhaust should be outside the building - Multiple NO sensors in the ICU.
- 219. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 219 Q-What is the problem of overdosage of NO? A-No has affinity for hemoglobin. It combines to hemoglobin to form methhemoglobin. A methhemoglobin level of up to 15% is acceptable. If it rises above 20- 25%, it may lead to acidosis. Warfarin Q-What does warfarin stand for? A-Wisconsin Alumini Research Foundation coumaRIN It is a 4-hydroxy coumarin derivative & was introduced as a rodenticide. Q-Discuss warfarin metabolism. A-It is metabolized in the liver (by enzyme cytochrome P 450) & excreted in bile It has a ½ life of 25- 60 hours (action lasts for 2 –5 days) Q-Discuss drug interactions with warfarin. A- Drugs that potentiate action of warfarin (increasing INR) are: 1) By inhibiting metabolism (Cytochrome P 450 inhibitors) - cimetidine - metronidazole - omeprazole - amiodarone 2) Preventing formation of active form of Vit K - 3rd generation cephalosporins - ciprofloxacin 3) Decreasing availability of Vit K - diet 4) By direct anticoagulat action - aspirin - dipyridamole Drugs that decrease action of warfarin (decrease INR) are: 1) By decreasing absorption of warfarin - sucralfate - cholestyramine 2) By increasing warfarin metabolism - gardinal - eptoin - alcohol - rifampicin 3) By decreasing GI uptake of warfarin - dairy products - fruits - tea/ coffee - raddish/ onion/ potato
- 220. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 220 FIRST’S IN HISTORY Q-Who performed the 1st heart surgery? A-Ludwig Rehn, 1896 Frankfurt Q-Who described ‘inflow occlusion’? A-Lewis & Varco Q-Who performed the 1st open heart operation? A-John Gibbon, 2nd Sept 1952 Q-Who introduced the concept of hypothermia? A-Bigelow (1950) Q-Who introduced topical hypothermia? A-Normal Schumway (1959) Q-Who introduced hypothermia with inflow occlusion? A-Lewis, Tauffic & Varco. Q-Who introduced hypothermia in CPB? A-Sealy Q-Who introduced hemodilution during CPB? A-Zuhdi, Gott & Lillehei Q-Who introduced cardioplegia? A-Melrose (1955, used 200 meq/ litre potassium)- abandoned due to high failure rate. Q-Who reintroduced potassium cardioplegia? A-Gay & Ebert (1973, 30 meq/ litre potassium) Q-Who introduced cold blood cardioplegia? A-Follette. Q-Who described the first oxygenator? A-Gibbon (1953, screen oxygenator). Q-Who performed the first successful surgery using an oxygenator? A-Kirklin (1955 on screen oxygenator) Q-Who introduced the bubble oxygenator? A-DeWall & Lillehei (1955) Q-Who introduced the concept of hypothermic circulatory arrest? A-Charles Drew
- 221. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 221 Q-Who performed the first clinical application of deep hypothermic circulatory arrest? A-Randall Griepp. Q-Who introduced Retrograde cardioplegia? A-Zuhdi & Gott. Q-Who introduced the TransRA technique of retrograde cardioplegia? A-Buckberg. Q-Who performed the first direct coronary sinus cannulation for retrograde cardioplegia? A-Menache. Q-Who described retrograde cerebral perfusion? A-Ueda & Miki. Q-Who described total body retrograde perfusion? A-Yasuarra (1994). Q-Who performed the 1st pericardiectomy? A-Ludwig Rehn. Q-Who performed the 1st ASD closure? A-Lewis & Varco (using inflow occlusion) Q-Who performed the 1st ASD closure on pump? A-Gibbon (1953) Q-Who performed the 1st PDA surgery? A-Streider (1937- but patient died of abdominal distension & aspiration). Q Who performed the 1st ‘successful’ PDA closure? A-Gross (1939). Q-Who performed 1st Pneumonectomy? A-Nissen. Q-Who introduced the prosthetic grafts for vascular procedures? A-The first material to be introduced was Viniyon by Voorhes in 1952 (Viniyon was the material used for making parachute) PTFE- Edwards (1957) Dacron- DeBakey (1960) ePTFE- Sayer & El Gore Q- Who performed the 1st cardiac transplant? A-Christian Bernard (3rd December, 1967).
- 222. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 222 Q- Who performed the 1st pediatric cardiac transplant? A- Kantrowitz (1967). Q- Who performed the 1st ‘successful’ pediatric cardiac transplant? A-Bailey (1967). Q- Who performed 1st heart lung transplant? A-Reitz (1981). Q- Who performed 1st lung transplant? A-Cooper (1984). Q- Who performed the 1st reversed saphenous vein graft for peripheral vascular disease? A-Kunlin. Q- Who performed the 1st ‘insitu’ saphenous vein grafting? A-KV Hall (later the technique was popularized by Leather). Q- Who performed 1st elective cardiac fibrillation? A-Ake Senning. Q-Who introduced DC defibrillator? A-Berkovit’s. Q-Who performed the 1st clinical application of internal defibrillator? A-Harken. Q-Who introduced the concept of counterpulsation? A-Moulopolous. Q-Who coined the term ‘counterpulsation’? A-Harken. Q-Who performed the 1st clinical use of counterpulsation? A-Kantrowitz. Q-Who performed the 1st surgery of coronary artery to RA fistula? A-Bjork & Crafoord (ligation in 1947).
- 223. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 223 Q-Who described the various cardiac pathologies? A-The underlying table summarizes the above: Etiology 1st description 1st surgery ASD Leonardo da Vinci Lewis & Varco by inflow occlusion Gibbon on CPB VSD Roger Lillehei on cross circulation Kirklin on CPB TOF Nicholas Steno Etiene Louis Arthur Fallot Lillehei on cross circulation Lillehei on CPB PDA Galen Leo Botali Gross (division & suturing) Coarctation Morgagni Craaford Angina Heberden various INDIAN SCENARIO Q-Who performed the 1st open-heart surgery in India? A-Dastoor. Q-Who performed the 1st single vessel bypass in India? A-KM Cherian (1975). Q-Who performed the 1st triple vessel bypass in India? A-KR Shetty (1975). Q-Who performed the 1st VSD closure in India? A-Gopinath. Q-What are the instruments introduced by an Indian? A-They are: 1) Kole’s cardioplegia chamber 2) Pandey Joshi oxygenator (bubble type) 3) Lillehei- Kalke valve (precursor of St. Jude) Q-Who performed 1st CMC in India? A-PK Sen. Q-Who performed 1st ASD with inflow occlusion in India? A-PK Sen. Q-Who performed 1st heart transplant in human in India? A-PK Sen.
- 224. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 224 INSTRUMENTS PLASTIC PERIPHERAL ARTERIAL CANNULA *This is a plastic arterial cannula for peripheral arterial cannulation for the purpose of CPB. This cannula (peripheral arterial cannulation) is used for: Unchallenged indications are: 1) Ascending aortic aneurysm surgery 2) TOF ICR with previous Potts shunt 3) AP window 4) Dissection Stanford Type I Also used for 5) Emergency bypass 6) Right thoracotomy approach open heart surgery 7) Redo surgery 8) Port access surgery 9) CPB for constrictive pericarditis. Advantages are: 1) Single cast 2) Beveled 3) Only the tip is narrow Disadvantages are: 1) Resistance to flow due to small inner diameter ratio as compared to outer diameter. 2) Can get kinked 3) No markings present 4) Can come out Q-Is there a ‘complete’ metallic cannula for same purpose? A-Described by Solomon Victor. Has the advantage of reusability & optimization of inner diameter: outer diameter ratio. Q-Why iliac cannulation is preferred over femoral? A-Because: 1) Iliac artery is larger hence larger cannula can be inserted 2) Lesser chances of infection & lymphorrhea COOLEY’S CLAMP *This is a Cooley’s vascular clamp
- 225. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 225 Instrument is used for 1) Waterston Cooley shunt 2) Proximal anastomosis construction on aorta, during a CABG. 3) Aortic cannulation 4) BT shunt 5) PDA surgery (division & suturing) 6) Peripheral vascular surgery 7) Right atrial appendage cannulation 8) Ligation of left atrial appendage Q-Why are there marks on the inner aspect of the clamp? A-These marks are made at a distance of 4 mm, to indicate the limit of anastomosis during a Waterston Cooley shunt DEBAKEY CLAMP *This is a DeBakey vascular clamp made out of stainless steel. Advantage of this clamp A-are 1) Atraumatic 2) Doesn’t come in way of surgery It is used for A- 1) Peripheral vascular surgery 2) Cross clamping aorta in pediatric patient 3) Clamp PDA (larger size clamp) 4) Clamping aorta in thoracic & abdominal aortic procedure (larger sized clamps) Q-Why is a ‘crest’ present beyond the jaws of the clamp? A-The crest is present for accommodating arterial wall, to avoid puckering. SATINSKY CLAMP Specific uses are: 1) Side biting of aorta for proximal anastomoses during CABG 2) Clamping LAA during CMC 3) During Waldhausen’s repair for coarctation 4) Rest like Cooley’s clamp BAILEYS RIB APPROXIMATOR Used for approximation of ribs post thoracotomy.
- 226. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 226 AORTIC CROSS CLAMP *This is an aortic cross clamp used for cross clamping the aorta during an open-heart procedure Q-Which surgeries, on CPB, can be performed without aortic cross clamping? A-They are: 1) CABG on fibrillating arrest or CABG on CPB with aid of stabilizer 2) Right sided surgeries (on TV/ PV) Q-What are the other ways of cross-clamping aorta? A-By using endoluminal balloon occlusion for: 1) Port access surgery 2) Atherosclerotic aorta Q-Which conditions require ‘early’ clamping of aorta? A-are 1) AR 2) AP window 3) Truncus arteriosus 4) Myxoma Q-What are the complications of cross-clamping aorta? A-They are: 1) Clamp MPA 2) Dislodgement of plaque 3) Can clamp tip of arterial cannula 4) Clamp may be applied partially Q-What are the disadvantage of a cross-clamp? A-The disadvantage is that it can come in the way of surgery. Q-Why is the flow reduced during declamping of aorta? A-The flow is reduced as the aortic cusps are open & on release of the clamp, the gush may distend the LV (even before the cusps can close). CAVOATERIAL CANNULA *This is a single cast, wire reinforced 2-stage venous drainage cannula, also called as the cavoatrial cannula, used for the purpose of caval drainage on CPB & has an obturator inside. Used for 1) Aortic valve surgeries 2) Ascending aortic surgeries 3) CABG 4) LV aneurysm surgery 5) Rarely MVR with a large LA
- 227. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 227 Disadvantages are: 1) Causes early rewarming of the heart 2) The SVC may get tented (& hamper venous drainage) during positioning for OM grafts 3) Right sided procedures cannot be performed 4) May cause incompetence of the NCC & hinder in delivery of cardioplegia Q-What are the types of cannulae (cavoatrial) tips available? A-They maybe one of the following type: 1) Basket tip 2) Bullet tip 3) Swirl tip *RETROGRADE CARDIOPLEGIA CANNULA This is a self-retaining retrograde cardioplegia cannula Q-When is a retrograde cannula termed ‘self retaining’? A-When there is no separate port for balloon inflation. Q-How does one know that the balloon is in the coronary sinus? A-The following will indicate that the balloon is in the coronary sinus. 1) Balloon is felt in the coronary sinus 2) Dark blood in the cannula as compared to SVC & IVC 3) If a pressure line is connected, it will show ventricular tracings Q-Who described insertion techniques of a retrograde cardioplegia cannula? A- Direct coronary sinus: Menasche Trans RA: Buckberg Q-What is the site of insertion, over RA, of the cannula? A-A point, at the junction of cephalad 2/3rd & caudad 1/3rd, on a line joining the RAA to the lateral aspect of IVS. Q-What should be the relation of the retrograde cardioplegia cannula to the 2-stage cannula? A-It should be anterior to the 2-stage cannula. Q-What is the technique of insertion of the cannula? A-Classically cannula is placed in the left hand & is guided by the right hand. Generally the opposite is practiced.
- 228. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 228 Q-What are the options available if the retrograde cardioplegia cannula is not entering the coronary sinus, with a cavoatrial cannula in situ and the patient on CPB? A-The options available are: 1) Go off bypass, insert two caval cannulae, snug the cavae, on bypass, open the RA & then undervision insert the cannula in the coronary sinus. 2) Push the 2 stage cannula completely into the IVC, loop the IVC, occluded the SVC, open RA & insert the cardioplegia cannula into the coronary sinus, close RA, and release caval snares & withdraw the 2 stage cannula back into the RA. Q-What are the disadvantage of retrograde cardioplegia? A-They are: 1) It may not perfuse the RV (if the anterior cardiac veins are draining directly into the RA) or also if the retrograde cardioplegia cannula is inserted to much inside 2) Impaired perfusion of the IVS 3) Complications due to insertion, viz. - hematoma at the site of coronary sinus - coronary sinus rupture - RV rupture Q-What is the disadvantage of combined antegrade & retrograde cardioplegia? A-Myocardial edema Q-What are the advantages of retrograde cardioplegia during a CABG operation? A-They are: 1) Subendocardial perfusion 2) Even distribution in case of diffuse coronary artery disease 3) Washes out air & debris 4) By avoiding direct osteal cannulation, late osteal stenosis may be avoided Q-Discuss monitoring of retrograde cardioplegia delivery? A- 1) Maximum pressure of delivery is 30 mm Hg 2) Blood will be seen emerging from the coronary ostia 3) TOPS (fine needle probes to monitor PO2 in tissues) Q-Which is the manual inflatable retrograde cardioplegia cannula? A-It is termed as the Gundry’s silicone retrograde cardioplegia cannula. Q-What is the rate of delivery of retrograde cardioplegia? A-Is 100- 500 ml/min/m2 at 25 mm Hg.
- 229. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 229 IVC MIXTER *This an IVC mixter used for going around the IVC for the purpose of looping it. It is also used for dissection & looping the aorta. Q-What are the complications of looping IVC? A-The possible complications are: 1) Damage to RIPV 2) Damage to IVC MIXTER Used for 1) Looping vessels like - SVC - PDA - Vertical vein - Peripheral vascular structures 2) OMC- for hooking the subvalve 3) Clamping the RCA at the initiation of cardioplegia delivery ti prevent air from entering the RCA 4) Deairing the aorta, from the LV, at the start of the repeat cardioplegia Q-Discuss management of SVC tear during its looping. A-Insert aortic cannula & be on suction bypass Or IVC cannulation & partial CPB (with SVC cannula connected & clamped) Or IVC & Innominate vein cannulation & full CPB AORTIC CANNULA *This is a short/ long tipped curved, 2 cast, vented/non vented, wire/ non wire reinforced aortic cannula, made of PVC, used for cannulation of the ascending aorta during an open heart surgery. It can also be used rarely for 1) Proximal arch cannulation 2) Venous cannula Sizes available in adults are: 20, 22 & 24 F. Advantage of metal tipped cannula are 1) Maximum optimization of inner diameter/ outer diameter ratio 2) Has a hub for retaining it in position 3) Has a fixed distance from hob to tip of metal, hence less chances of branch cannulation.
- 230. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 230 Disadvantage of the cannula are: 1) Maximum RBC damage 2) Formation of air vaccoules at the sides of the jet emerging from the tip 3) Non wire reinforced, hence can get kinked/ clamped Q-What is double arterial cannulation? A-In cases of large descending thoracic aortic aneurysm, 2 cannula, one each in the axillary artery & the femoral artery are inserted. Q-What is the Chaukar-Pandey shunt? A-It is a shunt inserted between the subclavian artery & the left CCA, for arch surgeries, for maintained cerebral perfusion with the arch clamped. Q-What is ‘Scouring’? A-A partial thickness incision made over the aorta with a knife (15 no.) for the purpose of cannulation. Q-What is the size of the cannula used normally? A-It depends on only one factor- the flow required. Q-What is the maximum resistance permissible? A-Immediately after insertion of aortic cannula, around 180 mm Hg. ( 60 mm Hg of tubing & 120 mm Hg of aorta.) Q-What is the D/D of ‘no blood’ in the aortic cannula post insertion? A-They are: 1) Partial thickness puncture (dissection) 2) Tip abutting aortic wall inside- turn the cannula & pulsatile blood should flow Q-What signs will indicate dissection secondary to aortic cannulation? A-They are: 1) No flow in the cannula 2) Non pulsatile flow in cannula 3) Increase in size of hematoma 4) Decrease venous return (if on bypass) Q-Discuss management of dissection secondary to aortic cannulation. A-Terminate bypass & perform a femoral arterial cannulation & aortic cannulation. Assess extent of dissection by TEE & perform corrective procedure Q-What are the disadvantages of small tip cannula? A-They are: 1) May cause partial thickness puncture in the aortic wall 2) Causes increased turbulence & vacoulations
- 231. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 231 METAL TIPPED VENOUS CANNULA *This is a long/ short, curved, metal tipped, 2 cast, wire reinforced pacifico venous drainage cannula for selective caval cannulation Q-What are the unchallenged indications for selective SVC cannulation? A-The unchallenged indications for selective SVC cannulation are: 1) Senning’s 2) Mustard 3) Transplant 4) TCPC Q-What does ‘dlp’ stand for? A- d- David l- Linda p- Philip they are children of J Davies. Q-What is the classical technique of caval cannulation? A-The SVC cannula goes from the IVC pursestring & the IVC cannula from the SVC pursestring (both pursestring’s are taken over the RA & straight venous cannulae are used). PLASTIC STRAIGHT VENOUS CANNULA *This is a plastic tipped straight; non wire reinforced venous cannula, made of PVC, for cannulation of iliac/ femoral vein for the purpose of CPB. Q-Which side is preferred for the cannulation? A-The right side is preferred as: 1) the left sided common iliac vein is crossed by the iliac artery 2) the left common iliac vein is more angulated Q-What are the indications of iliac vein cannulation? A-The indications are: 1) Emergency surgery 2) Redo surgery 3) Portaccess surgery 4) Large arch aneurysm (where the caval visualization is impossible) Q-What are the possible complications of Iliac vein cannulation? A-They are: 1) Lymphorrhea (more common with femoral exposure) 2) Infection
- 232. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 232 ANTEGRADE AORTIC ROOT CARDIOPLEGIA CANNULA *This is an antegrade aortic root cardioplegia cannula with a flange (for fixing it in position) & with/ without a vent line. It is used for 1) Delivery of cardioplegia 2) Deairing 3) Venting the LV, transaorta, during - CPB - Retrograde cardioplegia delivery Also rarely used for 4) Pulmonary artery perfusion for - pulmonoplegia (transplant) - in patients with L-R shunts with severe PH (for PA perfusion during CPB) Q-How is air removed prior to delivery of second cardioplegia? A-As follows: - clamp RCA - make aortic valve incompetent transiently, if possible - clamp the vent arm of cannula after air flows out Q-What are the steps of deairing the heart? A- De-air LA (if LA open) followed by LV apex from aortic vent (+/- aspirate the apex) Patient is give a Head low position & patient shaken side to side over the table suction is attached to the aortic vent & de airing confirmed on TEE (ideal) CPB flows are dropped & clamp is partially removed followed by normal flows Transiently reapply clamp & massage to de-air & then remove clamp, bring the table to normal position Q-What measures may be taken if the coronary arteries contain air? A-The following measures maybe adopted: 1) Administration of higher pressure cardioplegia 2) Administration of retrograde cardioplegia 3) Milking of the arteries 4) Stab the coronary with fine needle
- 233. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 233 OXYGENATOR & RESERVOIR Q-How can reservoir overflow be prevented in a patient with a large heart? A-Either or combination of the following maybe adopted. 1) Increase flow 2) Decrease venous return 3) Vasodilators 4) Diuretics 5) Ultrafilteration 6) Use a 2nd reservoir Prevention is by using minimum prime. Q-Discuss the characteristics of routinely used oxygenator/ reservoirs. A- Prime Blood flow rates (litres/ min) Minimum operating level Reservoir capacity Affinity NT 270 ml 1- 7 200 ml 4 litres Minimax plus 150 ml 0.5- 2.3 150 ml 2 litres Capiox SX 10 135 ml 0.5- 4 100 ml 3 litres Safe Micro 52 ml 0- 800 ml 25 ml 400 ml ARTERIAL FILTER Filter size: 25- 40 um Produces a gradient of 30 mm Hg with a flow of 7 litres/ min & requires a priming of 200 ml. TUBB’S DILATOR *This is a transventricular dilator called as the Tubb’s dilator, made of stainless steel & is used during a CMC Q-How is a dilator checked prior to using? A-The dilator should: 1) Open against resistance 2) Open smoothly 3) Close completely 4) Its blade should not rotate Q-Describe the maintainence of dilators. A-By: 1) Oiling the screw 2) Immediately post procedure, flush the proximal portion with saline/ hydrogen peroxide & let the effluent escape from the distal portion
- 234. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 234 Q-What are various ways of using Tubb’s dilator? A-Depends upon which direction are the blades opened. - Logan: open dilator in any direction - Cooley: open dilator perpendicular to the commissure Q-Discuss modifications of MV dilators over time. A- Original transventricular dilator: Logan & Turnur. Modifications introduced by: - PK Sen - Cooley - Beck - Glenn - Tubb Q-What modification did Tubb introduce in the dilator? A-He introduced a screw to enable a predetermined opening distance of the dilator. Q-What complications may occur secondary to using a Tubb’s dilator? A-The following are the potential complications. 1) Avulsion of LV pursestring due to dilator getting stuck in it 2) Dilator stuck in open position 3) Tip getting disengaged & remaining in the LA/ LV 4) Tearing of leaflet resulting in an acute MR. Q-What MR is acceptable after CMC? A-Grade I MR. Q-What is unacceptable MR after CMC? A-The following MR is unacceptable: 1) Grade II or more 2) MR with unrelieved MS 3) MR due to tear in leaflet/ rupture chordae 4) Associated with a high preoperative PH Q-How is pursestring taken for a small LAA? A-The pursestring should be over the posterior aspect of LA; extending over the PV’s. Q-How can CPB be established, if required, during CMC? A-Depending upon the emergency either thru’ same incision or thru’ a midsternotomy. Ways of going on to CPB are thru’ the same incision are via: 1) RVOT & femoral artery 2) RA & femoral artery (cut the pericardium perpendicular to the incision to expose RA) Dissect between the PA & aorta for cross clamping & cardioplegia pursestring & delivery)
- 235. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 235 Q-Which ‘pliable’ MS is difficult to open during CMC? A-Eccentric MS. VSD RETRACTOR It is used for: 1) Retracting the posterior margin of VSD (RA approach) to visualize the superior margin 2) Retracting the anterosuperior margin of VSD (RV approach) to visualize the posteroinferior margin 3) Aortic valve surgery 4) MV surgery- to lift the AML to see underneath the valve STERNOTOMY SAW Q-What are the various instruments available for sternotomy? A-They are: 1) Oscillating saw 2) Labsche 3) Gigli saw 4) Saurebroch’s sternal cutter 5) Stout scissors (in neonates & infants) FOGARTY CATHETER Q-Enumerate historical techniques of embolectomy? A-They are: 1) Milk the artery to the arteriotomy (Lahey’s technique) 2) Pass a catheter & flush the artery 3) Pass a catheter, apply suction to it & withdraw. Q-What are the general specifications of Fogarty? A-Balloon capacity is 2 ml. Length is 80 cm 3 markings at 70, 60 & 50 cm. Q-What is Sheiley’s embolectomy catheter? A-It has 2 balloons. One is at the regular place while the other is near the site of inflation, to gauge the extent of inflation of the inner balloon. Q-What are the modifications of Fogarty? A-They are: 1) Fogarty with side holes 2) Fogarty with ribbed balloon (for increased strength)
- 236. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 236 Q-What is the use of stylus in the Fogarty catheter? A-If a firm clot, it will not permit the Fogarty to pass thru’ without a stylus (beyond the clot). Q-What are the other uses of Fogarty? A-They are: 1) Lung occlusion technique 2) PDA occlusion for closure on CPB 3) Pulmonary embolectomy Q-What complications can result due to overdistension of the balloon? A- 1) Intimal tear 2) Plaque disruption Q-When should catheter passage be stopped? A-Till no more clots retrieved. Q-What are ‘non-balloon’ embolectomy catheters? A-Are: 1) Adherent clot catheter 2) Graft thrombectomy catheter. LINE CLAMP Used for: 1) Clamping the aortic cannula post insertion for - Deairing - Checking pulsatile flow - Color of blood 2) Clamping the venous cannula just prior to going on bypass & also when on bypass with single cannula in situ. LANGENBECK RIGHT ANGLED RETRACTOR Used for: 1) Retracting lower & upper edges of incision prior to sternotomy 2) Retracting inferior angle of RVOT incision for VSD closure 3) 2 for retracting LA during MV procedures 4) Retracting anterior lip of aorta during VAR 5) Retract RA 6) Retract sternum to check for wire bleeders/ internal mammary artery bed post harvesting
- 237. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 237 Q-What are the techniques for retracting right atrium? A-They are: 1) Stay sutures 2) Right angled retractors 3) Kirklin retractors. SPONGE HOLDING FORCEPS Used for: 1) Painting & draping 2) LA clot removal 3) As an aid in internal mammary artery dissection TUFFIER RIB RETRACTOR For spreading ribs after thoracotomy DUVAL’S LUNG HOLDING FORCEPS For holding lung parenchyma during various lung procedures D/D with Freidrich’s lung holding forcep. STABILIZERS Q-What are the techniques of stabilization? A- 1) Pharmacological – using Esmolol 2) Mechanical-are a) Suction: Octopus (Medtronic), X pose (Guidant) b) Compression: CTS (Baxter) c) Calafiore tapes Q-What are the types of mechanical stabilizers? A-The maybe classified as: 1) Hand held 2) Table mounted 3) Retractor mounted Q-What is the dosage of esmolol? A-Loading= 0.5 mg/ Kg over 2- 4 minutes Maintenance= 0.05 mg/ Kg/ min. ½ life= 9 minutes
- 238. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 238 OCTOPUS STABILIZER (presently available Octopus IV) *This is an Octopus stabilizer for stabilization of a portion of the ventricle, on a beating heart, during an off pump CABG. It has 3 parts: 1) Foot plate 2) Stabilizing system 3) Locking system Q-How much suction is applied? A-300 psi. Q-What is the advantage of suction stabilization device? A-There is no compression on the heart. Q-What are the disadvantages of suction stabilizer? A-They are: 1) May cause damage to epicardium & myocardium (suction injury) 2) Produce arrhythmogenic areas 3) Damage to vennules 4) Cost. INTRACORONARY SHUNTS This is an intracoronary shunt & is used during an off pump CABG to maintain distal perfusion of the coronary, during the procedure. Q-What are the advantages of shunt? A-They are: 1) Tapering end- provides easy insertion 2) Bulbous end- prevents slipping out & prevents leak 3) Transparent- allows to see blood flowing 4) Avoids taking of the posterior wall at the angles in small coronaries Q-What are the sizes available? A-From 1mm to 3.5 mm. Q-What are the disadvantage of shunt? A-They are: 1) Provide inadequate flow if a small shunt is used 2) Plaque dislodgement during insertion 3) Sutures may go thru’ the shunt MIST BLOWER *This is a mist blower & is used to aid visualization during OPCAB.
- 239. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 239 It has an added advantage of opening up the angles for increased ease of suturing. Q-What is the gas used? A- 1) O2- cheap & easily available 2) CO2- preferred as less chances of embolism AORTIC PUNCH *This is a plastic/ metal aortic punch used for punching holes in the ascending aorta for the purpose of proximal anastomosis, after having side-clamped & stabbed the artery. Q-What sizes are available? A-4, 4.5 & 5 mm. Q-What are the uses of the aortic punch? A-They are: 1) Proximal anastomosis in a CABG 2) ASD/ VSD patch septostomy 3) Bentall’s procedure- to punch holes in the graft Q-What sizes are used for proximal anastomoses over the aorta? A-Generally for radial artery- 4 or 4.5 mm For reversed Saphenous vein graft- 4.5 or 5 mm. HANCOCK II VALVE It is a porcine aortic valve. Designs, over time, are: 1) Hancock standard 2) Hancock modified orifice 3) Hancock II 4) Hancock Mosaic Q-Who is Hancock? A-Warren Hancock, Vice President of Edwards laboratories. He left it & established his own company & released the Hancock valve. Q-Which chief surgeons use Hancock tissue valve? A- - Tirone David - Brian Barret Boyes Q-Which chief surgeons use Carpentier Edward valve? A- 1) Delos Cosgrove
- 240. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 240 Q-Discuss design of Hancock valve. A- 1) Stent: - Flexible (decrease stress on valve tissue) - Made of acetal homopolymer 2) Supraaanular design- 21mm can be used in 19 mm Gradient of Hancock II in aortic position 21mm has 12 mm Hg Material used: - Stent: Acetal homopolymer with polyester fabric - Radioopaque rings with eyelets- made of Haynes alloy - Tissue treatment with sodium dodecyl sulfate surfactant (T6) - Physiologic fixation Sizes available are: Aortic- 21 to 29 mm. Maximum ventricular protrusion of 16 mm Mitral- 25 to 33 mm, with ventricular protrusion of < 16 mm till 29 mm size & is 17 & 17.7 mm respectively for 31 & 33 mm size. MOSAIC: Material used - Stent: acetal homopolymer & polyester fabric - Radioopaque eyelets of Haynes 25 alloy - Anticalcification- alpha amino oleic acid (AOA) Sizes available are: Aortic- 19 to 29 mm Mitral- 25 to 33 mm Q-What is physiological fixation? A-Equal pressure of 40 mm Hg is applied to the inflow & outflow portion simultaneously. This technique preserves the anatomy of sinuses of valsalva & the angle of attachment of leaflets. Q-What is the advantage of AOA treatment? A-When a tissue valve is fixed with glutaraldehyde it results in free aldehyde formation. Calcium ions bind to this free aldehydes and cause calcification. AOA binds & blocks the free aldehydes & thereby inhibiting calcification.
- 241. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 241 SURGEONS & THEIR ACHIEVEMENTS Rene Favalaro (1923- 2000) - 1st documented aortocoronary bypass using an autologous saphenous vein on 9th May 1967 - CABG in patient with acute myocardial infarction - CABG along with AVR - Wrote book with > 20 1st technical contributions to the field of cardiac surgery - Developed retractor for harvesting internal mammary artery - Established Favalaro foundation in Argentina Charles Theodor Dotter - 1st peripheral angioplasty - Developed flow directed balloon catheter - Percutaneous arterial stenting - Won nobel prize Brom - 3 patch technique for supravalvar AS - Trouser patch for mustard operation - Brom’s incision- Rt. Thoracotomy for ASD Aldo Casteneda (1930- till date) - Chief of children hospital Boston - > 400 scientific articles & books - Concept of correcting cardiac anomalies at an early age for TOF, AV canal, TGA - Norwood worked under him & described the Norwood operation for HLHS - Developed needle holder & vascular clamps - Studied effect of CPB on blood elements & heart lung transplantation in primates Alfred Blalock (1899- 1964) Baltimore - 1st BT shunt on 29th Nov, 1944, assisted by Longmire - Blalock Hanlon atrial septectomy - Blalock loop - 1st thymectomy - First PDA ligation - In personal life was plaqued by illnesses: septicemia with osteomyelitis of sternum, nephrectomy with permanent ulnar nerve palsy, pulmonary TB Sir Magdi Yacoub - Extensive work on homografts - AV repair techniques - Proposed PA banding to train the LV for arterial switch - VSD with AR- closure of VSD from aorta while plicating the AV with the same Sutures - MVR thru’ aorta
- 242. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 242 Clarence Walton Lillehei - Father of modern cardiac surgery - From University of Minnesota, Medical Center, Variety Heart Hospital, Minneapolis - Described hypothermia with inflow occlusion (with Lewis) - Azygous flow principle - Cross circulation (maternal) - Autologous oxygenation - Infusion of oxygenated blood only during CPB (but the reservoir would empty & gas emboli) - Biological oxygenation (using Baboon lung) - Bubble oxygenator (along with DeWall) - 1st open heart surgery & also 1st to perform OMC, AVR, TOF ICR, TAPVC, TGA - Proposed PML preservation - Developed 3 valves: -Lillehei Kaster valve- pivoting disc valve -Lilehei Kalke valve- bileaflet valve with a 60 opening angle (only one human implantation done & patient died within 24 hours) -Lillehei Naqib valve- Toroidal disc valve (disc with central hole) - First to describe external cardiac pacing [Note:Indians trained under Lillehei are - Dr. Gopinath & Dr. Kalke] - Lillehei suffered from a left parotid malignancy for which 2 surgeries were performed (radical resection with radical neck dissection & mediastinal dissection) Wills Potts - Described Pott’s shunt - Described the various types of vascular rings & slings Denton Cooley - Founded Texas Heart Institute - Cooley’s clamp - Cooley’s retractor for LA - Concept of stone heart - Waterston Cooley shunt - Cooley’s vascular graft - 1st heart transplant in US - 1st artificial heart - 1st aortic aneurysm surgery - 1st LV aneurysm surgery on arrested heart - LV apicoaortic conduit - Developed Cooley Cutter valve
- 243. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 243 Ake Senning (1915- 2000) - He joined work with Crafoord - Developed one of the first pump oxygenators & used on patient with LA myxoma - Described the Atrial switch procedure - 1st use of elective fibrillation of heart during surgery - Implanted the first implantable pacemaker in a 43 year old man of Stoke Adams syndrome (the man now 84 is still alive after changing 26 pacemakers) - Introduced fascia lata for trileaflet valve & also implanted the 1st mitral homograft in mitral position - Worked with Gruntezig towards the 1st transluminal coronary angioplasty - > 350 publications Vincent Gott - Gott shunt (between LV apex & descending thoracic aorta) - Gott Dagget valve (bileaflet valve) - Work on biocompatibility studies for valves Charles Dubost - Developed the vertical RA-LA incision for MV exposure - Transatrial MV dilators - Endocardial resection with atrioventricular valve replacement for endomyocardial fibrosis - 1st abdominal aortic aneurysm resection Donald Ross - 1st aortic homograft - Pulmonary autograft in aortic position - Described the various types of sinus venosus defects Alain Carpentier (1933- till date) - Discovered glutaraldehyde, - Coined the term bioprosthesis (Phd thesis in 1975) - Describe dynamic cardiomyoplasty - 1st bioprosthetic valve implantation - Reconstruction surgeries of valves - Technique for complete AV canal correction - Surgical technique for Ebsteins - Introduced radial artery as conduit for CABG - 1st cardiomyoplasty - 1st videoassisted open heart - 1st computer assisted open heart Clarence Crafoord - 1st surgery for coarctation aorta- resection with end to end anastomosis - Developed ventilators - Co-developer of heart lung machine (along with Bjork, Senning)
- 244. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 244 PK Sen (1915- 1982) - Born Calcutta, MBBS from GSMC (KEM) - Dept. of CTS at KEM is by his name - Founder of CTS in India as a speciality - 1st CMC in India - 1st ASD with inflow occlusion in India - Work on Transmyocardial accupuncure (forerunner of TMLR) - Cardiac transplant in canine - 1st heart transplant in human in India & 6th in the world (1968) - Described a technique for arch replacement - Extensive work on aortoarteritis - Married Marie Barnes, had no children - Received Padma Bhusan Alexis Carrel (French Born) - Vascular suturing techniques - Sutured homologous free carotid artery between the aorta & coronary (canine) - Interposed vein bypass of arterial tree - Nobel Prize in 1912 - After a dispute left Rockefeller university & returned to France - In France he was accused of being Nazi collaborator (in 1943) - Died in 1944 Robert Gross - 1st successful PDA surgery (performed division & suturing) - Interposed Dacron graft for coarctation aorta - Atrial well technique for ASD closure - 1st pediatric pneumonectomy - 1st surgery for double aortic arch - Classification of esophageal atresia - Described various vascular rings & slings - 1st congenital diaphragmatic hernia surgery - 1st AP septal defect surgery (direct ligation) McGoon - McGoon’s ratio - Classification of MAPCA’s - McGoons surgery (of MPA widening as first stage for TOF correction) - 2 patch technique for supravalvar AS - McGoon’s stitch at inferior angle of ASD
- 245. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 245 Micheal Debakey - Born Louisianna, New Orleans - Established MASH units - Invention of roller pump - Development of double velour Dacron - 1st carotid endartrectomy - 1st use of LVAD - Classification system for aortic dissection - DeBakey clamp - Debakey-Surgitool valve - CTS center at Baylor college named after him. Christian Neethling Bernard (1922- 2001) - 1st cardiac transplant on 3d Decrease 1967 at the Groote Shruur Hospital, Cape Town. Performed on 54 year old Louis Washkansky who received heart of 18 year old Dennis (accident victim) & the patient lived for 18 days 2nd patient, in 1968, lived for 1 ½ years - Devised piggy back operation - Developed Bernard Shrire valve - 1st prosthetic replacement of TV for ebsteins - Described surgery for TGA in 1962 (involved connecting the PV’s to TV via a Teflon tube graft) - 1st use of DHCA for aortic operations (?) -Father was preacher & mother organist -3 marriages (last wife 40 years young to him) -Retired in 1983 due to disabling rheumatoid arthritis -Had 2 regrets in life: 1) endorsing an antiaging cream (which turned to be bogus) 2) apartheid
- 246. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 246 MUST KNOW JOURNALS CMC 1) CMC- early results with long term follow up in 3724 patients; Stanley John. Circulation 1983 A study from 1956 to 1980 of 3724 patients. Mean age= 27 years (youngest 6 yrs) Immediate Mortality= 1.5%. Incidence of MR requiring surgery immediately after CMC= 0.3%. Survival: 84% on 24 yr FU. Peak time of restenosis=12 yrs 2) Schoevaedts, JTCVS 1981 The 10th post op year is the critical period when the need for reoperation is highest, irrespective of whether procedure is open or closed. 3) CMC for mitral restenosis-113 patients experience. RK Suri, JTCVS 1996. 10-year experience. Mean interval between 1st & 2nd surgery= 9.4 yrs Hospital mortality <3% Post op Grade I MR= 16% Post op significant MR (requiring Sx)= 2% Restenosis rate at 5 year= 8.4/ 1000 pt/ year & at 10 year= 20/ 1000 pt/ year. 4)Burden of RF & congenital heart disease in India Padmavati, IHJ 2002 Indian population= 1,027 million 34.3% are below 15 years 65% below 40 years Congenital heart disease: Incidence of 4- 12/1000 live births Hence 1,12,000 are added to the congenital heart disease number every year in the Indian population RHD: 5 lac children (5- 15 years) have RHD. 14 lac is the total prevalence of RHD in India with 50,000 cases of RHD being added per year. 0.2- 0.7/ 1000/ year children get RF. OMC 1) Plea for an early open mitral commissurotomy; Frank Spencer, AHJ 1978 Appealed for an early OMC in patients with - fewer symptoms - valve area between 1.3- 1.5 cm2 as it may prevent progressive fibrosis which may eventually require a prosthetic valve.
- 247. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 247 2) Factors affecting MV reoperation in 317 survivors after MV reconstruction J Fernandez, ATS 1992 The factors are - young age - rheumatic heart disease - mixed mitral pathology 3) OMC- 14- 18 year follow up clinical study J Herrera, ATS 1993 159 patients of OMC Freedom form reoperation was 92% at 15 years & 88% at 18 years. 4) Mitral commissurotomy- a technique outdated. Long term FU over a period of 35 years Christian Detter, ATS 1999 183 patients (143 CMC, 40 OMC) Reoperation rate in both groups= 15.7 ± 7 years Survival at 10, 20 & 30 years for CMC is 89%, 68% & 49% respectively and for OMC at 92%, 67% & 46% respectively. Valve related morbidity & mortality was 2.1% patient year in CMC & 1.1% patient year in OMC. Long term survival same in both groups however the reoperation related mortality decreases in the OMC group. Hence OMC is procedure of choice. 5) Open mitral commisurotomy the current era- Indications, technique & results. Choudhary SK, Sampath Kumar, ATS 2003. VALVE REPLACEMENT 1) 20 year experience with the Medtronic Hall valve Eric Butchart, JTCVS 2001 1981 valves implanted in 1720 patients. 42% AVR, 45% MVR, 13% DVR Mortality: Early 4.2% for AVR, 7% for MVR, 12% for DVR. Late valve related deaths: 0.8%/ year for AVR, 0.9%/ year for MVR & 1.1%/ year for DVR Long-term survival was 10 years 15 years AVR 64% 45% MVR 58% 36% DVR 47% 30%
- 248. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 248 Freedom for all valve related complications 10 years 15 years AVR 72% 60% MVR 61% 50% DVR 61% 52% 2) 18 year FU with Hancock II bioprosthesis Juan Legarra, JHVD 1999 279 Hancock II bioprosthesis implanted 48% AVR, 44% MVR, 8% DVR Acturial freedom from explantation is: 10 years 18 years AVR 73 16% MVR 77% 38% DVR 72% 24% - The Hancock II is more durable in the aortic position, especially in the elderly. 3) Late results of valve replacement with Hancock II- 20 years Tirone David, JTCVS 2001 1128 valves 50% AVR, 30% MVR, 20% DVR 15 year survival of AVR= 47%, MVR= 30%. Freedom from reoperation (of the same valve) at 15 years for AVR= 77%, MVR= 69%. 4) Long term (29) year results of reconstructive surgery in RHD- MR Alain Carpentier, Circulation 2001 951 patients, mean age= 26 years 95% had annuloplasty ring &/ or shortening of chordae, leaflet enlargement with autologous pericardium, commissurotomy. Mortality= 2% Mean FU= 12 years Freedom from reoperation was At 10 years= 82%, & At 20 years= 55% 5) AV repair using cusp extension in children with rheumatic AR Kalangos, JTCVS 1999 41 children mean age 12 years with rheumatic AR requiring surgery 3 year FU Post Op AR: Grade 0=27, Grade I= 14 No reoperation for AR. No AS produced (PSG < 10 mm Hg)
- 249. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 249 6) Treatment of endocarditis with valve replacement: the question of tissue vs mechanical valve. Marc Moon, Norman Shumway. ATS 2001 306 patients of left sided IE (209- native, 97- prosthetic) Valve sued- mechanical in 65, bioprosthetic in 226 & homograft in 20. Operative mortality= 18% (independent of the valve type) Long-term survival was better for native valve endocarditis Vs prosthetic valve endocarditis. (44% Vs 16% at 20 years) Long-term freedom from reoperation: < 60 years age, at 15 years postop for biologic valve was 51% at 10 years and 19% at 15 years. > 60 years- same for biologic & mechanical (84% vs. 74% at 15 years) Conclusion: Mechanical valves are most suitable for younger patients with native valve endocarditis however tissue valves are acceptable for those more than 60 years of age with native prosthetic valve endocarditis. 7) Late results of valve sparing operation in patients with aneurysm of ascending aorta & root. Magdi Yacoub, JTCVS 1998 158 patients 50% had Marfan’s. 30 day mortality= 4.6%. Need for reoperation was 3% at 1 year & 11% at 10 years. FU: No AR-64%, mild to moderate AR=33%, Severe AR= 3%. 8) AVR- comparison of late survival between autografts & homografts Christopher Knott-Craigh, ATS 2000. 238 patients late survival at 10 years was - 77% for autograft - 67% for homograft Freedom from reoperation (degeneration/ infective endocarditis) at 10 years was - 88% for autografts - 72% for homografts Conclusion: Autografts & homografts have comparable late survival. The incidence of calve degeneration is low, for both, till 8 years at which point there may be a trend towards an advantage for autografts over homografts. 9) Fate of AV disease after MV intervention Sampath Kumar, JTCVS 2001 284 patients of MV surgery with mild AV disease conserved AV disease conserved was AS with mean gradient < 25 mm Hg or AR Grade I or II. 2- 18 year FU. Patients with mild AR - at 5 years- no increase in AR - at 10 years- 3% developed significant AR
- 250. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 250 - at 15 years- 13% developed significant AR Patients with mild AS - at 5 years- 25% developed significant AS - at 10 years- 39% developed significant AS - at 15 years- 54% developed significant AS 10) Severe AS with severe LV dysfunction- result of AVR Jamil Tajik, Circulation 2000 52 patients all with EF <35% mean transvalvar gradient < 30 mm Hg. Operative mortality= 21% (predictors being age & small aortic prosthesis) 62% survival at 3 years. Post op 75% had an increase in EF by 10% 11) TV valve replacement- UK heart valve registry midterm results comparing mechanical Vs biological prostheses; C Ranatunga, ATS 1998 425 patients 53% received bioprosthesis, 47% received mechanical FU= 4 years Survival was 73% at 1 year, 60% at 5 year, 43% at 10 year. 30 day mortality= 15- 18%. There was no difference in early mortality & also no difference in 1, 5 & 10 year survival. Freedom from redo operations at 10 years was 97% & was same for both the groups. Trend analysis has identified that surgeons in UK are opting for mechanical valves in TV position. 12) TVR with bioprostheses- long-term results & causes of valve dysfunction. K Nakano, ATS 2001 18 year experience with 98 bioprosthesis (Carpentier Edward, Hancock pericardial) Age= 52 ± 13 years Freedom from SVD was: - 98% at 5 years - 96% at 10 years - 96% at 18 years Duration between TVR & re-TVR (12 patients) = 8 years 13) 25 year experience with mitral & aortic valve replacement for RHD in 456 patients; Stanley John, ATS 2000. 456 patients of DVR. Mean age= 32 years 90% MVR & 73% AVR using Starr Edward valve Early mortality= 8%
- 251. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 251 Actuarial survival was - 85.6% at 10 years & - 82% at 24 years (mentioned in the article is- “it is not what you do, it is how you do it”) 14) Long term results of triple valve surgery, Micheal Carrier, ATS 2002 Survival was - 80% at 1 year - 75% at 5 years - 41% at 10 years 15) Current recommendations for adding aspirin to warfarin in patients with prosthetic heart valves, JACC 2001 i- patients with mechanical valves who suffer TEE despite adequate anticoagulation ii- those with ball in cage valve iii- patients with mechanical valves with additional risk factors like - h/o TEE - af - large LA (> 60 mm) - CAD - Ball valve - > 1 mechanical prosthesis or a mechanical prosthesis in mitral position TOF 1) TOF- What surgery at what age M Pozzi, EJCTS 2001 Study duration: Between 1993- 1998. Mean age: 16 mnths, mean wt.= 8.8 (75% of pts < 6 mnths) Hospital mortality= 0%. Rhythm- nsr=100%, RBBB= 21% Conclusion- A primary repair of TOF can be performed at any age. 2) Pulmonary artery (Nakata) index Seisuke Nakata, JTCVS 1984 Described an angiographic method of estimation of PA size in 4 group of patients, viz: -Normal -TOF -Rastelli -Fontan Method: Diameter of right & left pulmonary artery just prior to the 1st lobar branches, taken in systole & diastole (as there is a 20% difference in the sizes in the 2 phases) PA index= [RPA area + LPA area] BSA in mm2m2 Normal index= 330 ± 30mm2m2
- 252. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 252 Other ratio’s available are: 1) McGoon’s: [RPA + LPA diameter] diameter of aorta at level of diaphragm All taken in systole. 2) Muraoka’s index: Ratio of PA annulus to aortic annulus. (the diameter of the MPA & ascending aorta vary depending upon the extent of valvar & supravalvar stenosis, hence are not considered for estimation of ratio) 3) Late PV replacement after ICR TOF Dannielson, JTCVS 2001 42 pts with pulmonary valve replacement at mean age of 22 years & mean interval of 10 years. Post PVR: 5 year survival= 95% 10 year survival= 76% Freedom from rePVR was 93% and 70% at 5 & 10 years The significant risk factor for rePVR was young age at time of PVR Lessons learnt: 1) Operate on asymptomatic TOF’s in deterioration of PR 2) Correct all concomitant lesions 3) Insert largest size PV (atleast or more than 25 mm) 4) Secondary Fallot Circulation 1956, Gasul 5% of patients of VSD develop a RV infundibular hypertrophy which causes protection of the pulmonary circulation- secondary Fallot 5) Long term results after early primary repair of TOF. Richard Jonas, JTCVS 2001 57 patients, mean age= 8 mnths, mean wt.= 6.5 Kg All under DHCA, transventricular approach. VSD closed with interrupted sutures 50% had a transannular pericardial patch. FU= 23.5 yrs. Results: - 86% survival at 20 years (no difference whether patch used or not) - Freedom from reintervention at 5 years= 93% and at 20 years= 79% - Commonest cause of reoperation was RVOT stenosis (Vs PR as stated by most of other studies) 6) A 26 years experience with surgical management of TOF- risk analysis for mortality or late intervention Christopher Knot-Craigh, ATS 1998 294 patients, mean FU of 10.6 years All < 12 mnths age, operative mortality for primary repair= 2% and for staged repair= 11.8%.
- 253. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 253 Risk factors for hospital death are: - hypothermic circulatory arrest - pulmonary artery patch plasty - earlier year of reoperation (before 1990) - closure of PFO Freedom from reintervention for RVOT at 20 years is: 85% for TOF with PS and 43% for TOF with pulmonary atresia. Findings: - Incidence of redo surgery is lower in younger age group - Incidence of arrhythmias is lower in the early age group - No effect of age of surgery on the mortality - Do not close PFO if operating at an early age 7) TOF- surgical management individualized to the patient. Fraser, Cooley, ATS 2001 144 patients, 94 underwent primary ICR, 39 were post BTS Conclusion: - Symptomatic patients in spell or those less than 4 Kg should undergo palliative BTS followed by ICR between 6- 12 mnths age - Patients with pulmonary atresia should undergo BTS followed by definitive repair between 6- 12 mnths age - All patients should undergo complete repair after 6 mnths age 8) Reconstruction of the pulmonary outflow tract without a prosthetic conduit. Yves Lecompte, JTCVS 1982 - The PA is delivered in front of the aorta - extensive widening of VROT by resection of the infundibular septum - PA is sutured to the RVOT with an anterior valved pericardial patch 9) TOF in adults. Stanley John, American J Medicine 1979 147 patients, all > 18 years. Most frequent symptom was dyspnea 6% had cyanotic spells, 60% squatters, 16% had CCF, 10% had systemic HT, CTR > 55%= 25%. CCF commonly seen due to- AR, systemic HT, IE, relative anemia CTR > 55% is uncommon in children but present in significant number in adults 10) Results of ICR TOF in adults ATS 1996 (from Italy) 40 pts over 20 years, mean age at surgery= 30 years Hospital mortality= 2.5% Reoperation rate of 8% at an interval of 1-2 years post ICR, for residual VSD. Conclusion: - post operative problem same as young patient
- 254. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 254 - Arrhythmias: 40% of adult patients Vs 10- 20% in young patients, with a definite increased risk of sudden death BT SHUNT 1) Modified BT shunt. Marc DeLeval, JTCVS 1981. 99 patients between 1975- 1979 at the Great Ormond Street Hospital 1st 13 using woven Dacron and 2nd 86 using Teflon. Overall failure arte= 8.1% 2) Classic BTS-upper limb complications. Lodge, JTCVS 1983 28 pts of classic BTS BAPI(op) BAPI (normal) ratio calculated BAPI (op)=Brachial artery pressure index on operated side BAPI (nor)= Brachial artery pressure index on normal side Findings: Pre op BAPI= 0.99 Immediate post op= 0.4 3 weeks post op= 0.7 Follow up=0.7 Exercise resulted in an increase in BAPI No limb ischemia 3) Effect of BTS- modified & classical on the pulmonary arterial tree F. Godart, ATS 1998 78 patients, mean age 20 months, mean wt.= 8 Kg FU angio done at 90mnths for classic shunt, & 40 mnths for modified BTS. McGoon ratio evaluated which showed 1) Comparable increase in size of RPA LPA (by 25%) for 5 & 6 mm size 2) Both RPA & LPA increase in similar manner & amount 3) No increase in size with 4 mm shunt 4) Increased rate of tenting & stenosis with MBTS 4) BTS in neonates. Amruta institute, IJCTS 2001 20 infants, mean age= 82 days, mean wt.= 3.2 Kg 3.5- 4mm shunt used in all Rate of shunt blocking= 10% Mortality= 10% 5) BTS causing growth of contra lateral PA. Jehangiri, ATS 1999 Showed equal growth of both the branched PA’s with a modified BTS (either side)
- 255. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 255 GLENN 1) Bi-directional Glenn- physiology. Freedom, ATS 1998 Showed that a BDG does not cause an increased growth of the PA’s. Thus if a BDG is performed as a stage to Fontan, for hypoplastic PA’s, it has no benefit. 30% devolop significant systemic venous to pulmonary venous collaterals. AV CANAL 1) Operation for partial AV septal defect-a 40 year review. G Dannilson, JTCVS 2000. 334 patients, Average age= 8 years. Conclusion: - all with closure of cleft & operated below 20 years had better survival - Survival at 30 yrs= 85%, at 40 yrs= 76% - 11% incidence of redosurgery, at a mean interval of 17 yrs. - Arrhythmias were more common in pts with late surgery & cleft left open. 2) Surgical repair of complete AV septal defects. Fred Crawford, ATS 2001 172 pts, mean age=10 mnths, mean wt=6 Kg 82% had Downs’s syndrome Single patch closure in all Early mortality=5% Complete heart block=3% FU: 7% had MR requiring surgery (most due to opening of the cleft)- hence advisable to close the cleft over pericardial pledgets Freedom from reoperation at 5 yrs= 95%, 10 yrs= 88% 3) AV valve function after single patch repair of complete AV septal defect in infancy: how early should repair be attempted. V Mohan Reddy, JTCVS 1998 72 infants, median age= 3.9 months. Cleft closed either completely or partially. 1 death No relation of age on death, left AV valve regurgitation & reoperation. ASD VSD 1) Incidence of atrial flutter fibrillations in adults with ASD before & after surgery ATS 1999 24 hours holter monitoring Incidence of atrial flutter is reduced after surgery but no significant change in fibrillation. Hence for patients with atrial fibrillation, an additional maze procedure should be considered
- 256. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 256 2) Double patch closure of VSD in patients with elevated PVR William Novick, ATS 1998. 18 patients A fenestration was made into the patch and was covered by a smaller patch with a hinge mechanism, with the opening directed into the LV, towards the apex. PASP PVR Preop 105 11.4 wood Postop 42 O% 89% 98% -no hospital mortality -echo showed no shunting across the flap -the technique provides a mean of maintaining systemic CoP during pulmonary hypertensive crisis & preventing RVVO 3) Multiple VSD’s- how and when should they be repaired F Seddio, Mohan Reddy. JTCVS 1999 45 patients with multiple VSD’s (more than or equal to 2) 1 early death All RA approach. Maneuvers to aid in visualization or identify VSD are: 1) Incision of trabecular musculature 2) Division of moderator band 3) Open aorta- pass suture from LV to right & see full extent of VSD Other techniques for closure for multiple VSD are: 1) Place a single large patch over the entire area of the IVS (Cherian et al) 2) Pass oversized patch thru’ the defect into the LV & suture the knots on the side of RV 3) For anterior muscular VSD- directly suture posterior edge of VSD to the RV free wall 4) Biologic glue for small VSD 4) Coarctation with VSD- should we perform a single stage repair Y Isomatsu, JTCVS 2001 79 patients, all less than 3 months Mean age= 28 days, mean wt.= 3.2 Kg Only 2 stage repair performed Stage 1: subclavian flap angioplasty wit PAB (19mm + body weight) Stage 2: closure of VSD with debanding Mortality= 8% Survival= 92% at 10 years 8% recoarctation, all dealt with balloon dilatation 5) New strategy for VSD with coarctation. JACC 1999 Use of absorbable polidioxone 5mm bands for PAB 11 infants operated at mean age of 10 days with PAB & aortic reconstruction.
- 257. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 257 Results: 6 mnths FU, all 11 VSD’s had closed or became hemodynamically insignificant. Need for debanding & reconstruction of PA is avoided. 6) Coexistent MV disease with left to right shunt at the atrial level Stanley John, JTCVS 1970 Lutembachers, in 1916, described ASD with MS. MS is considered to be congenital, & the increased LAP (due to MS) is believed to lead to opening of the PFO, & hence ASD. In this article, S John emphasis that the MS is acquired. Also suggests the inclusion of MR under the spectrum, of Lutembachers. 7) PA banding Albus, Trussler, Izukawa. JTCVS 1988. Gave the formula for PAB for 3 groups of patient. Group I- 20mm + 1mm/ kg body weight Group II/III- 24 mm + 1mm/ Kg body weight All the banding performed using a 4mm wide band. -also mentioned in the discussion of the article is an alternative technique, suggested by Harold King: which is as follows. < 3 mnths/ < 4 Kg weight: use 6 no. Hegars > 3 mnths/ > 4 Kg weight: use 7 no. Hegars A band is placed around the PA & the Hegars is placed over the PA (along the length). The band is tightened over the Hegars & the PA occluding the PA completely and then the Hegars is slid out. OTHERS 1) Negative reexploration for cardiac postoperative bleeding- can it be therapeutic? Pelletier MP. ATS 1998. 5 patients with negative reexploration, the fibrinolytic activity of systemic blood Vs mediastinal blood was compared. -revealed marked increase in the fibrinolyic activity of mediastinal blood ( fibrinogen, FDP, plasminogen activator inhibitor) which may play a role in lysis of freshly thrombosed capillary ends. Hence removal of clots reduces the fibrinolysis allowing bleeding end capillaries & small vessels to thrombose. 2) Continuos perfusion of PA’s during total CPB favorably affects levels of circulating adhesion molecule & lung function. Suzuki, JTCVS 2000. 14 patients of SBPpa/ SBPao > 0.5, mean age of 6 mnths. Systemic perfusion at 150 ml/ kg/ min & PA perfusion at 30 ml/ Kg/ min (using a needle in MPA & a LV vent) Analysis of circulating intracellular adhesion molecule, soluble granular membrane protein 140, sialyl Lewisx, duration of mechanical ventilation- all showed that continous lung perfusion avoids ischemia & reperfusion injury.
- 258. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 258 3) Distribution of cerebral blood flow during antegrade & retrograde perfusion. M Katz, ATS 1999 Rabbit model & analysis of capillary filling, using Tc99m scan, score of 0 to 5 allotted (no flow to 100% flow) 4 groups studied & following findings noted Group Score warm antegrade 3.7 warm retrograde 0 cold antegrade 4.6 cold retrograde 0.5 Thus in RCP, there is very poor flow thru’ the capillaries, possible because of - venoarterial shunt - venovenous shunt Thus RCP possibly helps by - backwash of particulate debris - generalized cooling 4) IABP in children M Pozzi, ATS 1999 14 patients. Age- 7 days to 13 years. Site of insertion in smaller children- from aortic pursestring site. Rest femoral route. Results: 71% could be weaned off. Problems & solution: 1) Difficult in cannulation- use aortic pursestring 2) Increased elasticity- not true 3) Increased heart rate- if increased HR & balloon not able to deliver then cool patient to 34C which decreases the heart rate & allows augmentation 4) No coronary artery disease 5) Children have additional RV/ pulmonary arterial disease- thus ECMO is better. 5) Rupture/ dissection rates for thoracic aorta- predictors based on size. Ryan Connecticut, ATS 2002 721 pts over 9 years follow up. Risk of rupture 1) If > 6cm, 4 times more risk of rupture 2) If it is in the descending or thoracoabdominal aorta 3) Males had lower incidence % rate/ year of complication: < 5cm- 2%/ year 5-6 cm- 3%/ year >6cm- 7%/year
- 259. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 259 6) Surgical treatment of dilated ascending aorta- when & how Randall Griepp. ATS 1999 Indication for surgery: Emergency- 1) Dissection 2) Rupture 3) Intramural hemtoma 4) Destruction of aortic annulus by bacterial endocarditis Elective: 1) 5 cm diameter in degenerative disease 2) 4.3 diameter in Marfans 3) > 4.5 cm of found at the time of valve replacement 497 pts., Mortality= 4%. Single predictor of mortality was age (> 60 yrs= 7% mortality Vs < 60 yrs= 0.8% mortality) 7) Natural history of descending thoracic & thoracoabdominal aneurysm Randall Griepp, ATS 1999 165 pts. Increased risk of rupture: - age - COPD - Uncharacteristic continued pain 20% incidence of rupture. 8)Aortic aneurysm operation: past, present & future Denton Cooley. ATS 1999 9) Prediction of thoracic aortic aneurysm- validation of formula describing growth Shimada, ATS 1999 Linear expansion rate (mean 2.6mm/ year) Increase in aortic diameter < 40mm= 2 mm/year 40-49= 2.3 mm/year 50-59= 3.6 mm/year > 60= 5.6 mm/ year Yale formula underestimated growth by 0.8 mm Mt. Sinai formula overestimated growth 1.5cm Osaka formula overestimated growth by 0.2 mm 10) Sinus of valsalva- aneurysm or rupture, management & outcome. Denton Cooley, ATS 1999 129 pts.
- 260. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 260 Unruptured aneurysm: highest of RCC NCC LCC Ruptured aneurysm: Commonest of RCC (max in RV & then in RA) NCC (max in RA & then in RV) LCC Survival- unruptured: not known natural history Ruptured: survival of 3.9 years, hence surgery is a must 11) Prevention of spinal cord injury during thoracic & thoracoabdominal aortic repair. T. Wada, ATS 2001 Measure CSF pressure, SEP, Spinal cord perfusion pressure (SCPP= Mean aortic pressure- CSF pressure) 82 pts if SCPP < 40 mm Hg, then - increase mean distal aortic pressure (increasing flow to the distal aorta) - decrease CSF pressure (by withdrawing CSF) - change in operative technique- so as to begin perfusion to intercostals - reattach ICA graft CSF pressure should be < 10 mm Hg & mean distal aortic pressure > 60 mm Hg 12) Aortic root replacement in 271 Marfans patients- 24 year experience Vincent Gott, ATS 2002 Result: Actuarial freedom at 20 years from Thromboembolism= 93% Endocarditis= 90% Incidence of reoperation on residual aorta = 74% 13) PTFE for infrainguinal bypass Capetown, Surgery 1999 (from year book of vascular surgery 2000) 5 yr patency for above knee= 68% below knee= 76% 14) Dorsalis pedis artery bypass J Vasc Surgery 1999 (from year book of vascular surgery 2000) Primary patency (using RSVG) 1 yr= 80% 5 yr= 60% 15) Myth of insitu graft superiority Eur J Vasc Endovasc Surg, 1999 (from year book of vascular surgery 2000) 500 pts of insitu & 955 pts of RSVG 2 year patency rates were similar for both the group
- 261. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 261 16) Operative risk & results of LV aneurysm Tirone David, ATS 1992 365 pts 281- linear repair, 38 Dor’s repair 1 month mortality= 7% Predictors of immediate mortality are - age > 60 yrs - EF < 20% - Previous CABG - NYHA IV - No angina Predictors of late death are - left main - CCF - EF < 20% There was no difference in mortality between the 2 types of procedure, except in patients with EF < 20% 17) LV aneurysm repair Girinath, IHJ 2001 95 pts 67 linear, 28 Dor’s Mortality of 10% for linear repair VS 0% for Dor’s. NYHA comparison similar for both Lesser use of IABP in Dor’s 18) Circulatory arrest under moderate hypothermia Tirone David, ATS 1998 Generally patient cooled to < 18C but problems are: - increased time for cooling & rewarming - coagulopathy 104 patients, cooled to 22- 28C with retrograde cerebroplegia. Early mortality= 7.7% Mortality & stoke rate same as in < 18C group. Predictors of stroke were: 1) Laminated thrombi in ascending aorta & arch 2) Total arch replacement 3) Peripheral vascular disease 4) Circulatory arrest time > 30 minutes
- 262. AGT’s Notes compiled by Dr. Pawan Kumar AGT’s Notes Compiled by Dr. Pawan Kumar 262 19) Changes in QRS voltage in cardiac tamponade & effusion and its reversibility JACC 2001 Mechanism for low voltage in tamponade is ?. Reasons implicated are: - due to increased distance from body source - due to decrease in heart size & volume (definition of low voltage- maximum QRS of < 0.5 mV in limb leads) Results: - Low QRS is s/o tamponade & not diagnostic (53%) - no significance in effusion - low QRS persists for about a week even after pericardiocentesis & the returns to normal voltage. 20) Long term follow-up after coarctation surgery Am J Card 2002 274 pts with > 50 yr follow up. Immediate mortality = 7% 81% alive at >50 years. Commonest cause of mortality was coronary artery disease Highest survival with - age of surgery between 1-5 years - absence of hypertension at time of surgery






![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 6
Q-What is the auscultatory triangle?
A-Is formed by:
- Lower margin of trapezius
- Vertebra
- Upper border of latissimus dorsi
Q-What is the meaning of term ‘Diaphragm’?
A-In greek; ‘Dia’ means thru’ & ‘phragma’ means partition.
Q-What is the meaning of term ‘Coarctation’?
A-In Latin coarctere means to contract.
Q-What is the importance of angle of Louis?
A-It corresponds to:
- The level of 4th vertebra
- Tracheal bifurcation
- Arch of aorta traverses the thorax from right to left in a posterolateral direction
- Site of 2nd ICS
Q-What is the nerve supply of the diaphragm?
A-The diaphragm is supplied by the phrenic nerves.
[Note:If quadriplegia also involves the diaphragm, it is termed as Pentaplegia.]
Q-When does the heart starts beating in an embryo?
A-22 days.
Q-Why is LA O2% 99% and not 100%?
A-Due to drainage into the PV & LA of the:
- Bronchial veins
- Thebesian veins](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-6-320.jpg)
![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 7
PHYSIOLOGY
Q-What is Ohms law?
A-Current= (potential difference)/ (resistance)
Q-What is Poiseulle’s law?
A-Flow is directly proportional to the 4th power of radius & inversely proportional to the
length of narrowing.
Hence,
Pressure= flow x impedance
Systemic BP= systemic flow (CoP) x SVR
SVR in Wood units
1 wood= 80 dynes.sec.cm-5
Q-What are the phases of a cardiac electrical cycle?
A-
Phase 0: rapid depolarization- due to influx of Na+
Phase I: initial repolarization- influx of Cl-
Phase II: plateau- balance of K+ outflow with Ca2+ inflow
Phase III: late repolarization- continuing K+ efflux
Phase IV: resting phase
Q-Describe ECG correlation with phase of electrical cycle.
A-is
Phase 0 & I- QRS complex
Phase II- ST segment
Phase III- T wave
Q-What is the rate of normal coronary blood flow?
A-It is 70- 90 ml/100 gm of myocardium/ min
Q-What is the rate of myocardial oxygen extraction?
A-
Normal myocardium- 75% extracted
Stressed myocardium- 100% extracted
Normally other organs- 25% extracted
[Note: Significance of above:Unlike other organs the myocardium cannot extract more
oxygen when required. It requires an increase in blood flow.]
Q-How is Ejection fraction calculated?
A-Ratio of stroke volume to end diastolic volume
[(EDV-ESV)/EDV] x 100
Normally 67 8%.
Q-Is normal endothelium negatively charged
A-Yes.](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-7-320.jpg)




![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 12
OCCUPATION
For:
1) Respiratory ailments.
2) Sedentary lifestyle- higher chances of coronary artery disease.
RELIGION
For:
If a bioprosthetic valve is being planned then
- In a Muslim- a porcine valve may not be preffered, &
- In a Hindu- a bovine valve may not be preffered.
RESIDENCE
For:
1) Higher attitude patients have a higher tendency for Secundum ASD’s & also
earlier development of PH in the same.
2) Higher attitude patients have a higher tendency for PDA
3) People from tropical areas (Eg: Kerala) have a higher incidence of
endomyocardial fibrosis.
4) Aortoarteritis is more common in south India
5) Hydatid cyst is commoner in Punjab & Madurai.
DYSPNEA
Definition: Abnormally uncomfortable awareness of ones own breathing.
Divided into 4 grades, similar to NYHA classification.
NYHA classification: The New York Heart Association: has 4 components, viz;
Dyspnea, palpitations, fatigue & angina.
Presently followed is the 7th edition of NYHA (laid down in 1994.)
NYHA I: In a patient with heart disease with no limitation of physical activity. Ordinary
physical activity does not cause dyspnea, palpitations, fatigue or angina.
NYHA II: In a patient with heart disease with mild limitation of physical activity.
Comfortable at rest but ordinary physical activity causes dyspnea, palpitations, fatigue or
angina.
NYHA III: In a patient with heart disease with moderate limitation of physical activity.
Comfortable at rest but less than ordinary physical activity causes dyspnea, palpitations,
fatigue or angina.
NYHA IV: In a patient with heart disease with marked limitation of physical activity.
Symptoms are present at rest & increase on exertion.
[Note:PND is not included in the NYHA classification.]](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-12-320.jpg)
![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 13
Q-Is there any classification besides NYHA?
A-The following are the classification systems:
1- Canadian cardiovascular society classification CSS - only angina (of)
2- Specific activity scale (of Goldman)- most specific- calculation of metabolic
equivalents (1 MET= 2.5 ml/ Kg/ min)
Dyspnea is cardinal manifestation of LV failure. The increase in severity is in the
following order:
Dyspnea on exertion → PND → Orthopnoea → Dyspnea at rest → pulmonary edema.
Orthopnoea:
In the recumbent position there is decreased pooling in the lower limbs & abdomen →
blood is displaced from extrathoracic compartment to thoracic compartment →
Failure of LV to pump blood →
Increased pulmonary venous congestion & capillary pressure →
Interstitial edema → leading too:
1) Decrease in lung compliance +
2) Increase in airway pressure +
3) Ventilation perfusion mismatch.
→ all leading to dyspnea.
It occurs rapidly, within1-2 minutes of lying down & is relieved on sitting.
Cough accompanies due to increased pulmonary congestion.
A non-productive cough present in CCF is considered as “ dyspnea equivalent” and in
recumbency is considered as “ Orthopnea equivalent”
Trepopnea:
Orthopnea limited to one lateral position. ? due to distortion of great vessels.
Platypnea:
Dyspnea relieved on lying down. Reasons are not known.
Paroxysmal nocturnal dyspnea:
The patient awakes suddenly with a feeling of severe anxiety & breathlessness.
Associated bronchospasm (due to edema of bronchial mucosa) may be present.
[Note:Also called as cardiac asthma due to associated wheeze.]
It receives a longer time to get relieved. Reasons for PND are:
1) Slow absorption of extracellular fluid from the dependent areas & resultant
increase in blood volume
2) Elevation of diaphragm
3) Decrease LV adrenergic support during sleep
4) Depression of respiratory center during sleep
5) Transient nocturnal arrhythmias.](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-13-320.jpg)







![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 21
Q-What are the causes of peripheral cyanosis?
A-Causes of peripheral cyanosis are:
1) Cold/ vasoconstriction
2) Shock
3) Increased viscosity of blood
Q-What are the causes for mixed cyanosis?
A-Causes are-
1) Acute LVF
2) Severe MS (incipient pulmonary edema & vasoconstriction)
Q-What are the abnormal pigments that can produce cyanosis like picture?
A-They are:
Methhemoglobin, sulphhemoglobin etc.
Q-Discuss ‘differential cyanosis’?
A-It is seen in-
1) Only of lower limbs with/ without left upper limb in
- PDA with PH with Rt. To Lt. Shunt. With preductal coarctation
- Severe coarctation
2) Only upper limbs in
- PDA with PH with rt. to lt. Shunt along with TGA
- Coarctation with TGA
Q-What is the D/D between central cyanosis & peripheral cyanosis?
A-In central cyanosis there is:
1) Good peripheral warmth
2) Clubbing
Q-Which are the conditions were cyanosis cannot occur?
A-Cyanosis cannot occur in:
1) Severe anemia (Hb< 5 gm%),
2) Carbon monoxide poisoning
[Note:In Indians cyanosis is apparent when the O% is < 85%. When < 65%, intense
cyanosis.]
Q-In which conditions a patient may appear blue but there is no cyanosis?
A-The conditions are:
1) Sulphhemoglobinemia/ methhemoglobinemia
2) Silver poisoning
3) Aniline dye workers
4) Extreme cold environment](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-21-320.jpg)



![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 25
H/O RHEUMATIC FEVER
-Ask for h/o sore throat followed by fleeting arthritis.
Definition: It is an acute non-suppurative immune mediated inflammatory disease,
usually in children, that follows a few weeks after an attack of pharyngitis; caused by
group A hemolytic streptococci.
Q-What are the reasons for increased prevalence in developing nations?
A-The exact reasons are not known. It is believed to be due to:
- Increased urbanization (due to increased droplet infection),
- Overcrowding ( ” ).
[Note:There is no proof to suggest that nutritional factor has a role in RF.]
Q-Discuss the etiopathogenesis of RF.
A-The causative agent is group A hemolytic streptococci however in 1/3rd of the
patients there is no h/o sore throat nor blood culture yield e/o streptococcal infection.
Pathogenesis is not known & is believed to be an immune reaction to bacterial allergy or
an autoimmunity.
Q-Describe Aschoff bodies.
A-Aschoff bodies have the following features:
- May be seen if there is cardiac involvement secondary to RF
- Seen in the myocardium & endocardium (rarely over the valves)
- Most frequently seen in the; IVS & posterior surface of LV/ LA.
- They are discrete lesions, < 1mm diameter, formed by a collection of round cells,
fibroblasts & MN giant cells, surrounded by a zone of PMN cells & lymphocytes.
- Particularly situated around small blood vessels.
Q-What are the clinical features of RF?
A-The clinical features of rheumatic fever are:
- symptoms begin usually 2-3 weeks after an episode of acute pharyngitis.
-fever (is always present, except in chorea)
-fever lasts for 2-3 weeks.
-Other features that may follow are:
1) Arthritis: It is a fleeting arthritis affecting large joints with no residual deficit.
Generally affected joints are:
- Knee
- Ankle
- Elbow
- Wrist
Each joint remains inflamed for 1-7 days & complete episode lasts for 3 weeks.](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-25-320.jpg)

![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 27
Myocarditis-
- Important feature of myocarditis is progressive dilatation of LA & LV.
Pericarditis- 2 types
- Acute fibrinous
- Effusion
(pericarditis is associated with severe forms of carditis.)
Q-What is the incidence of CCF in patients with rheumatic carditis?
A-CCF occurs in 10% of patients with rheumatic carditis.
[Note:Prolongation of PR interval is temporary but may persist for months (reason is not
known)]
[Note:Rheumatic fever may lick the joints but certainly bites the heart.]
[Note:Rheumatic fever mainly affects the left side of the heart (reason unknown)]
Q-Discuss Jones criteria.
A-
Original criteria were described by T. Duckett Jones in 1944.
Currently the 4th edition (updated in 1992) of Jones criteria is accepted.
The criteria is as follows:
Major Minor
Carditis Clinical-
- Fever
- Arthralgia
- H/o rheumatic fever/RHD
Polyarthritis Investigations-
- Presence of acute phase
reactants (CRP, ESR, leucocytosis)
- PR interval prolongation
Subcutaneous nodules
Erythema marginatum
Chorea
+
E/o of streptococcal infection, in form of
- ASLO +ve, or
- + ve throat culture, or
- h/o scarlet fever.
The diagnosis of rheumatic fever, by modified Jones criteria, is by
- 2 major criteria + e/o streptococcal infection, or
- 1 major & 2 minor criteria + e/o streptococcal infection.
If there is no supporting e/o streptococcal infection then a diagnosis of rheumatic fever
should not be accepted, except in 2 conditions:
- only signs of chorea, or
- only signs of carditis.](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-27-320.jpg)
![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 28
(This is because the infection may have occurred few months back & hence the antibody
titres may have returned too normal.)
[Note:In India polyarthralgia is included as major criteria (in 1994 by Padmavati &
Khanna)]
Q-What is average duration of rheumatic fever?
A-The average duration of an attack of rheumatic fever is 3 months. In cases of carditis, it
may continue for nearly 6 months.
Q-Discuss ASLO.
A-Described by Todd in 1932.
Normal levels are upto 333 Todd units- in children &
Upto 250 Todd units in adults.
Most specific test for rheumatic fever is AntiDNAase antibody levels.
Normal levels are upto 240 Todd units- in children &
Upto 120 Todd units in adults.
Q-What is the D/D of streptococcal pharyngitis?
A-
- viral: characterized by more malaise & rhinitis.
- Other bacterial.
Q-What is the risk of recurrence of RF?
A-Risk of recurrence of rheumatic fever is 65% & subsequently the risk decreases with
time.
Q-What are the WHO recommendations for rheumatic fever?
A-The WHO recommendations are to treat all sore throat as due to group A hemolytic
streptococci unless proved otherwise. The prophylaxis is:
Single injection of 12 lac units Benzathine penicillin (if wt. > 27 Kg) &
Single injection of 6 lac units Benzathine penicillin (if wt. < 27 Kg)
Or
Oral Erythromycin 20 mg/Kg/day for 10 days.
Q-Discuss the treatment of rheumatic fever.
A-Treatment of rheumatic carditis is 3 fold:
1) Treatment of CCF- bed rest, salt restriction, digoxin, diuretics
2) Treatment of Carditis- Aspirin- 100 mg/kg/day in 8-10 divided doses for 1 month
if symptoms persist after few days of starting aspirin add Prednisolone 1-2 mg/ Kg/
day & reduce aspirin.
3) Treatment of rheumatic fever.
Q-What is the incidence of valvular affection of RHD?
A-The incidence of valvular affection of RHD:
MV- 70-80%, MV + AV- 20- 25%,
Only AV- 5- 8%, TV- 30- 50% (autopsy)](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-28-320.jpg)


![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 31
FAMILY HISTORY
Significance of family history is for
- Coronary artery disease
- Congenital heart disease,
- Consanguineous marriage,
- Age of the parent; at time of birth of child (patient).
Q-Discuss the importance of family history for congenital heart disease?
A-(From an article by Nora & Nora, Circulation 1978)
The % risk of an offspring having a CHD if the parent has the disease:
Disease % in offspring if father is % in offspring if mother is
affected affected
Congenital AS 3% 13%
ASD 1.5% 4.5%
AV canal 1% 14%
Tetrology of Fallot 1.5% 2.5%
VSD 2% 10%
PDA 2.5% 4%
The % of risk of a baby being affected if a sibling is affected:
Disease % in 1st sibling % in 2nd sibling
ASD 3% 8%
Tetrology of Fallot 3% 8%
VSD 3% 10%
PDA 3% 10%
[Note:If a parent & sibling, both are involved then the risk of another sibling having the
heart disease is very high.]
Q-What is the importance of consanguineous marriage?
A-The importance lies for autosomal dominant & recessive conditions.
For autosomal dominant conditions like:
- Holt Oram syndrome
- Noonans syndrome
- Williams syndrome
- Marfans syndrome.
For autosomal recessive conditions like:
- Ellis Van Creveld syndrome,
- Kartegners syndrome
Q-What is the significance of age of parents?
A-The significance of age is as follows:
- Increased paternal age: Higher incidence of Noonan’s
- Increased maternal age: Higher incidence of Down’s syndrome](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-31-320.jpg)




![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 36
3) Volume:
High volume in-
- AR, MR, PDA, VSD
- High output states- fever, anemia, pregnancy, Beri beri, thyrotoxicosis
- Increased stroke volume- complete heart block
Low volume in-
- LVOT obstruction
- Myocardial cause
- Pericardial
Varying volume in:
- Pulsus alterans- sinus rhythm of alternating beats of varying volume- seen in LVF
4) Character:
Normal pulse has
a- anacrotic wave
t- tidal wave
n- dicrotic notch
d- dicrotic wave
Q-What are various types of pulses?
A-
a) Anacrotic pulse- slow rising well sustained- seen in AS
b) Dicrotic pulse- 2 beats palpable; the percussion wave & the dicrotic wave- seen in
fever, CCF
c) Pulsus besferiens- 2 betas palpable in systole, rapidly rising pulse; the anacrotic
wave & the tidal wave- seen in AS with AR, idiopathic hypertrophic subaortic stenosis.
d) Pulsus parvus et tardus- slow rising & slow falling- seen in AS
e) Pulsus alterans- alternate strong & weak pulsations- seen in LVF
f) Pulsus bigeminus- regularly irregular with high volume- seen in unifocal ectopics.
g) Pulsus paradoxus- Normally the systolic BP falls by 10 mm Hg during inspiration.
This phenomenon is seen due to:
i. Increased venous return to the right heart & pooling in
the PV circulation decreased return to LA/LV
decreased CoP.
ii. Movement of the IVS to the left due to RV filling
decreased LV filling.
When the SBP falls more than 10 mm Hg, in inspiration, it is termed as pulsus paradoxus.
It is a misnomer, as it is nothing but exaggeration of the normal.
(*The paradox is that while the heart sound is heard, the pulse may not be felt)
Q-What are causes of pulsus paradoxus?
A-Causes are:
1) Cardiac- tamponade, constrictive pericarditis.
2) Pulmonary- Asthma, emphysema
3) SVC obstruction
[Note:Reverse pulsus paradoxus- It is seen in patients with CPAP, on ventilator]](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-36-320.jpg)
![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 37
h) Waterhammer pulse- rapid upstroke & rapid downstroke, characteristic rapidly
rising & rapidly falling pulse with high volume.
Causes:I) High output states- fever, anemia, pregnancy, Beri beri, thyrotoxicosis
II) Cardiac- AR, RSOV, PDA, AP window
5) Radioradial, radiofemoral delay & apex pulse deficit
Q-When can radiofemoral delay be appreciated?
A-If more than 40 millisec difference is present.
Q-What are the reasons of radioradial delay?
A-They are:
- SVAS,
- Coarctation aorta with involvement of SCA or with origin of the right SCA distal
to the coarct segment
- BT shunt- classic or rarely modified
Q-What is the normal time delay between the apex beat & a peripheral pulse?
A-The time difference normally between apex beat & a peripheral pulse is:
- Carotid artery= 30 millisec
- Brachial artery= 60 millisec
- Femoral artery= 75 millisec
- Radial artery= 80 millisec
JUGULAR VENOUS PULSE
Q-Why is JVP seen in the internal jugular vein?
A-It is easier to recognize pulsations in the EJV than IJV but still the EJV is not used as
an indicator of RA pressure due to:
1) Presence of valves in EJV
2) EJV passes thru’ more fascial planes & may be affected by extrinsic compression.
3) IJV is in a straight line with RA.
Q-Describe the technique of measurement of JVP?
A-Patient is kept in reclining position (at 45) & the neck is supported to relax neck
muscles (especially the sternomastoid) normally 5-9 cm of H2O from the mid RA or
0-4 cm from the sternal angle of Louis (center of RA lies ≈ 5 cm below the sternal angle).
[Note:In a healthy individual, at an angle of 45, the mean level is invisible. However the
a & v waves will be visible just above the clavicle (sternal angle).]
Q-How to differentiate JVP with carotid pulse?
A-The JVP is characterized by:
- postural variation,
- decrease in impulses with inspiration &
- not palpable impulse/ pulse.](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-37-320.jpg)

![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 39
BLOOD PRESSURE
Q-Describe the ‘cuff’ that is used to measure the BP.
A:
Name- Riva Rocci cuff
Optimum length of cuff- 2/3rd the circumference of the limb wih the center of the cuff
overlying the artery
Optimum width of cuff- 20% more than the diameter of the limb.
Normal width of cuff in adults is 12 cm for upper limb & 15 cm for lower limb
(if the width is narrower, a higher pressure will be recorded)
Q-How is lower limb BP measured?
A-For measurement of lower limb BP the patient lies prone & a 18 cm cuff is applied
above the level of the knee. Auscultation is carried out in the popliteal fossa.
Q-What are phases of Korotkoffs sound?
A-(from Hutchisons manual)
There are 5 phases:
1st phase- peak systolic pressure,
2nd & 3rd phase- due to turbulent blood flow thru’ a partially occluded artery.
4th phase- muffling of sound, & is 7-10 mm Hg above the true DBP.
5th phase- absent sound- true DBP.
Q-When is Korotkoff’s 4th phase used for measuring DBP?
A-In physiological conditions like pregnancy & pathological conditions like AR, PDA
and RASOV.
Q-What are the values of ‘normal’ BP in children?
A-A rough formula is as follows:
SBP= 90 + (age in years x 5)/ 2
DBP= 60 ± 20 m Hg
[Note:Normally the right UL BP is slightly higher than the left UL.]
Q-What conditions are associated with an abnormally high right UL BP?
A-The following conditions are associated with a abnormally high right uppel limb BP:
1) Interrupted arch
2) Supravalvar AS
3) Coarctation involving the left SCA.
Q-Does gravity affect BP?
A-For a distance above or below the level of the heart, subtract or add 0.77 mm Hg/cm.
Q-What is Ossler’s sign?
A-Ossler’s sign is pseudohypertension that is seen in Moenckbergs degeneration, where
the artery is sclerotic. Thus even with a lower systemic BP, the recording obtained is high
as the cuff is unable to occlude the artery (as it would normally do on inflation.)](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-39-320.jpg)



![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 43
8) Corigan’s sign- dancing carotids
9) Quinke’s sign- pulsatile capillary filling of nail bed on application of pressure over
the nails.
10) Waterhammer pulse- brisk upstroke, brisk downstroke with high volume, felt even
thru’ a less sensitive area like palm.
11) Locomotor brachials.
12) Mayne’s sign- < in DBP by > 15 mm Hg when BP is measured with arm hanging &
later with arm raised.
13) Austin Flint murmur- is due to:
a. Regurgitant jet hitting AML,
b. The coming together of 2 jets, ie, AR jet & The LA to LV jet, to
create turbulence,
c. Increased LVEDP
[Note:Even in severe AR an Austin Flint murmur may not be heard due to calcific AML
or an eccentric jet.]
14) Rosenbach sign- liver pulsations,
15) Gerhardt’s sign- splenic pulsations,
16) Duroziez murmur- on ausculatation over femoral artery, with pressure a systiloc
murmur heard distally & a diastolic murmur proximally
17) Lincoln sign- toe movements with cardiac contraction,
18) Traube’s sign- pistol shot femorals,
19) Shiley’s sign- Pulsating cervix.
MARFAN’S SYNDROME
Described in 1896 by Antine Marfan.
65-70% are by genetic transmission (caused due to mutation of the FBN1 gene on
chromosome 15.)
Q-What are the organ systems affected & diagnosis in Marfans?
A-The organ systems affected are CVS, Occular, pulmonary, skeletal & skin.
Diagnostic criteria laid down by Ghent:
1) Skeletal:
Major-
- Pectus escavatum/ carinatum
- Upper segment/ lower segment< 0.8
- Arm span/ height > 1.05
- Walker Murdoch sign (wrist sign)- little finger can go across the opposite wrist
and touch the thumb
- Steinberg sign (thumb sign)- thumb flexed and if it protrudes out of the medial
aspect of the hand, sign is +ve
- Metacarpal index> 8.4 (radiological length of 2,3,4 & 5 metacarpal added &
indexed to the added central diameter of the above metacarpals)
- Scoliosis
- Angle of elbow> 160º.](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-43-320.jpg)






![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 50
TRACHEAL TUG (OLIVER’S SIGN)
Technique- Raise the chin of the patient→ apply firm pressure on both the sides of
cricoid cartilage with one hand (thumb & index finger) or 2 hands → a downward tug is
felt by the fingers with each heart beat. It is seen in- arch aneurysms & mediastinal
masses
DIASTOLIC SHOCK:
It is palpable 2nd heart sound.
THRILL:
It is a palpable murmur & feels like the purring of a cat.
[Note:Diastolic thrills are better felt than systolic.]
[Note:Thrill is present in stenotic lesions & absent in regurgitant (as the turbulence
produced by low flow is coarse).]
PERCUSSION
The finger should be placed along the length of the ICS. The static finger is the
pleximeter while the striking finger the flexiform.
Left border:
Technique: start from the 4th or 5th ICS in midaxillary line & come medially. The left
heart border should coincide with the apex.
If outside apex- consider pericardial effusion.
Upper border: for 2nd & 3rd space paramedially on the left side.
If dullness is present in the left 2nd / 3rd ICS anteriorly, the possibilities are-
- Pericardial effusion
- Aneurysm aorta
- Dilated PA
- L posed aorta
- Ductal ampulla aneurysm
Right heart border:
Technique: percuss in the midclavicular line till liver dullness → come one space
higher→ percuss medially till sternum.
Normally Rt. HB should be retrosternal. If dullness present, it may suggest:
- pericardial effusion
- right atrial enlrgement
- aneurysm ascending aorta
- dextrocardia](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-50-320.jpg)

![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 52
Q-What are the causes for a soft 1st heart sound?
A-
1) Poor conduction of sound- thick chest wall, emphysema, pleural & pericardial
effusions.
2) MR, TR
3) Calcific MS
4) Long PR interval
[Note:S 1 is normally single & heard all over the precordium]
Q-What is the cause of a ‘reverse split’ of 1st heart sound?
A-Due to:
1) MS
2) LA myxoma
Q-Normally why does the MV close earlier than the TV?
A-Due to septal activation being from left to right.
SECOND HEART SOUND:
Normally A2 is audible in all areas while P2 is audible only in the pulmonary area & for
a short distance from the left sternal border.
Q-What is the normal splitting of S 2?
A-Normal spitting of the 2nd heart sound is:
During inspiration= 0.06 sec
During expiration= 0.02 sec
Q-When is P2 considered loud?
A-P2 is loud if:
- it is heard at the apex
- same or louder than A2 in the pulmonary area.
Q-When is A2 considered loud?
A-A2 is loud if:
- it is louder than P2 in the pulmonary area.
Q-What are the causes of a widely split S2?
A-The causes are:
-Electrical-
- RBBB
-Mechanical-
- ASD
- VSD
- PS
- RVF
- MR
- TAPVC](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-52-320.jpg)

![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 54
Q-What causes appearance of the 3rd & 4th heart sounds?
A-The 3rd & the 4th heart sound are due to abnormal filling patterns in the ventricles.
LVS3- during early rapid filling
LVS4- during atrial systole
FOURTH HEART SOUND:
*It represents a decreased compliance/ increased stiffness of the LV/RV.
*It is best heard with the bell of the stethescope with the patient in the left lateral
position.
MURMUR
Q-Describe the grading of murmur.
A-Grading of murmur was described by Levine & freeman in 1933.
I- III: are without thrill
IV- VI: are with thrill
Grade I: very faint murmur
Grade II: faint but easily audible
Grade III: loud without thrill
Grade IV: loud with thrill
Grade V: Louder, heard else where, with the side of the stethoscope placed sideways
Grade VI: Heard with the stethoscope lifted away from the chest wall.
[Note:Earlier the systolic murmurs were divided into 6 grades & the diastolic murmurs
into 4 grades]
Q-Which systolic murmurs are significant?
A-All systolic murmurs ≥ grade III are hemodynamically significant.
Q-Discuss murmurs in child.
A-Diastolic murmurs are always organic.
Systolic murmurs:
- Pansystolic- always organic; due to VSD, MR, TR
- Ejection systolic- organic if has associated
a. Symptoms
b. Cardiomegaly
c. > grade III
d. associated ejection click
Q-Describe the D/D between hypertensive PR Vs Normotensive PR.
A-
Hypertensive PR Normotensive PR
Murmur Decresendo Cresendo decresendo
P2 loud soft
RVH + -
Etiology All conditions with
increased PAP
APVS, post IE PV,
idiopathic dilatation of
PA, RVOT patch](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-54-320.jpg)


![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 57
13) Avoid alpha agonist
14) Avoid SNP (cyanide toxicity to fetus)
15) Administer tocolytics
Maternal mortality= 3%
Fetal mortality= 19%
Q-Can LMWH be administered in pregnancy?
A-No, as it crosses the placental barrier.
Q-What are normal blood volumes?
A-
Children= 85 ml/ Kg
Adults= 65 ml/ Kg
Q-How to calculate the amount of autologous blood to be removed?
A-
Volume to be removed= {Total bld volume x (Initial Hct- Desired Hct)}/ mean Hct
Q-How to calculate the amount of blood to be added?
A-
Volume of blood = [(Bv + Pv) x Desired Hct – Bv x Hct of patient]/ Hct donor blood
to be added (ml)
Bv= blood volume of patient
Pv= priming volume
Q-What is the height difference between the patient & the reservoir, during CPB?
A-It should be 25- 30 inches.
Q-What are the ways of confirming cardioplegia delivery?
A-Indicators of cardioplegia delivery are:
1) Aortic root distension
2) Heart stopping immediately
3) Generalized cooling of the myocardium
4) Coronary veins become bright red & distended
5) Blood returning from opposite coronary ostia if direct coronary injection being
given
Q-When does the myocardial activity continue even after delivery of cardioplegia?
A-The possibilities are:
1) Partially applied aortic clamp
2) AR
3) Incomplete venous drainage
4) K+ not added](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-57-320.jpg)



![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 61
Q-What actions are to be taken if air has entered thru’ the arterial line?
A-The following actions are to be taken.
- Cooling of patient & administration of 100% oxygen
- Head low
- Increase depth of anesthesia with thiopentone
- Administer mannitol & corticosteroids
- Retrograde cerebral perfusion
Q-What are the problems of venting thru’ the aorta?
A-The problems are:
1) Faster rewarming (as blood passes thru’ the entire left side of heart)
2) LV distension possibility
3) Has to be stopped during cardioplegia
Q-When is definite indication of venting the PA?
A-RA myxoma.
Q-Enumerate techniques for achieving ‘pulsatile flow’ during CPB?
A-Techniques are:
1) Additional pump after oxygenator
2) IABP
3) After removal of cross clamp allowing the beating heart to be partially full
4) Changing revolution of pump constantly
[Note:Historical technique- Cross circulation]
Q-What are the various anomalies of coronary sinus?
A-They are:
1) Absent coronary sinus (left SVC into LA- Ragib’s defect)
2) Hypoplastic coronary sinus- some veins opening directly into RA
3) Atretic coronary sinus
4) Dilated coronary sinus
- without L-R shunt: Lt. SVC into coronary sinus
- with L-R shunt: intracardiac TAPVC
5) Unroofed coronary sinus
Q-Describe St. Thomas hospital cardioplegia solution.
A-
First described by Mark Brainbridge & Hearse.
St. Thomas I in 1975 & St. Thomas II in 1981.
(St. Thomas Hospital is in London.)](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-61-320.jpg)





![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 67
Q-Describe Protamine administration protocol post CPB.
A-As follows:
-2-3 mg protamine per 100 U heparin administered
-Check ACT, if within 10 secs of post incision baseline ACT, there is no coagulopathy.
If more than 10 secs- suggests coagulopathy- add 25 mg more protamine
-Add 20 mg protamine for each 500 ml of heparinised pump blood.
-No protamine is required to cover cell saver blood.
Q-Is there any rate & site prefernce for protamine administration?
A-Recommended is a maximum of 5 mg/ min (in an adult) of protamine.
No difference has been noted on the site of administration, i.e., left or right
“It is the rate of administration & not the the site of administration”
Wakefield (Surgery, 1996) demonstrated a significant drop in the BP, HR & CoP with a
rapid administration of protamine to reverse heparin.
Q-What are the reasons for heparin rebound?
A-2 reasons are implicated
1) Release of heparin bound to plasma proteins
2) Release of heparin bound to endothelium
Maximum is within 1-3 hours, can appear as late as 6 hours.
It should be suspected if signs of bleeding appear after a period of dryness in the
operating field.
Q-Can LMWH be used for conducting CPB?
A-Yes. Disadvantages of LMWH for conducting CPB are:
- No effective dosage known
- Inadequate reversal with protamine
Q-Describe the protocol followed for using LMWH for CPB.
A-Anticoagulation protocol with LMWH is as follows (A. Carpentier)
- LMWH- 75 mg/ m2- IV bolus
(Additional 10 mg for every unit of blood added to the prime)
- If expected CPB < 60 minutes- monitor ACT
- If expected CPB > 60 minutes- monitor anti Xa activity
- If Anti Xa activity is > 1 IU/ml the proceed with aortic cannulation
- Repeat Anti Xa activity 1 hourly & if it is < 1.4 IU/ml, add 40 mg/m2 of LMWH
every 1 hour
Results with the above policy:
1) Protamine reversal was partial
2) Postoperative bleeding was more with LMWH
3) No effect on decreasing the requirements of blood or blood products (due to CPB
induced coagulopathy)
[Note:LMWH is used only if unfractionated heparin is contraindicated]](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-67-320.jpg)



![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 71
VALVUHAR HEART DISEASE
GENERAL
Q-What are the echo predictors of embolism in a patient with infective endocarditis?
A-(By JACC, 2001) Increased chances are if it is:
- a mobile vegetation
- > 10 mm vegetation (if > 15 mm vegetation then chance of embolisation is 80%)
Q-What are type of prosthetic valve endocarditis?
A-
- Early; within 60 days
- Late; after 60 days
Risk of prosthetic valve endocarditis is greatest within the first 6 months after surgery,
especially the first 6 weeks.
< 12 months- organism is usually staph aureus
> 12 months- organism is usually streptococcus
Q-What is the difference between prosthetic valve endocarditis & native valve
endocarditis?
A-NVE is largely confined to leaflet. In PVE, the infection commonly extends beyond
the valve ring, into the annulus & para annular tissue.
Q-Discuss the burden of rheumatic fever & CHD in Indians?
A-Padmavati, IHJ 2002
Total population of India= 1,027 million
34% are below 15 years
CHD: 4- 12/ 1000 live births
1,12,000 are added to CHD total every year
RHD: 5 lac children (< 15 yrs) have RHD
14 lac of total population have RHD
0.09% of the population has RHD
50,000 are added every year to the total.
Q-What is the pattern of rheumatic fever in Indians?
A-IHJ 2002, Chandigarh.
The following manifestation pattern is seen during the 1st & 2nd attacks of rheumatic
fever.
Symptom Incidence during 1st attack Incidence during 2nd attack
Fever 75% 70%
Arthritis 60% 60%
Arhtralgia 40% 20%
Carditis 22% 70%
Chorea 16% 10%
[Note:Incidence of anaphylaxis to penidura: 0.8- 4/ 10,000 courses of penidura.]](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-71-320.jpg)



![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 75
Q-What are commissural leaflets?
A-Sometimes accessory leaflet tissue is present at the commissures of MV, termed as
commissural leaflets. It is functionless.
Q-When to term as pulmonary hypertension?
A-When
Mean PAP> 20 mm Hg
Peak SPAP > 30 mm Hg
Q-What cardiac conditions are associated with a high risk of mortality in pregnancy?
A-There is increased risk of mortality if:
A-if following heart diseases present
1) Eisenmengerization
2) LVEF < 20%
3) Marfan’s with ascending aorta > 40 mm diameter
Q-What is dilated coronary sinus a feature of?
A-
1) CCF
2) Intracardiac TAPVC
3) Left SVC into coronary sinus
MITRAL STENOSIS
Etiology:
1) RHD
2) Congenital
3) Lutembachers
4) Endomyocardial fibrosis
5) Hurlers syndrome ( 1 iduronidase deficiency)
Signs:
- Pulsus parvus
- Tapping apex
- Diastolic shock
- Diastolic thrill
- Heart sounds- Loud S1, Loud P2, OS- may/ may not be present
- Murmur- middiastolic murmur with a presystolic accentuation heard over
the apex, radiating to the axilla, best heard with the bell of the stethoscope,
with the patient in left lateral position & breath held in expiration &
increased on clinching the fists.
[Note:The sign of severity of MS is the S2- OS interval (shorter the interval, more severe
is the stenosis)]](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-75-320.jpg)


![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 78
Q-How is size of inoue balloon, for BMV, calculated?
A-Size of balloon= {height (cm)/ 10} + 10
Q-During BMV why a pigtail is kept in the aorta?
A-To avoid damage to the NCC during septal puncture.
MITRAL REGURGITATION
Etiology:
Organic-
1) RHD
2) Mitral valve prolapse
3) Infective endocarditis
4) Papillary muscle dysfunction
5) Endomyocardial fibrosis
6) Collagen disorder- Marfans, SLE
7) Ruptured chordae- secondary to infection & trauma
8) Congenital
9) Os primum defect
10) Methysergide therapy
Functional-
1) AV disease
2) Systemic hypertension
3) Cardiomyopathy
4) Ischemia
Signs:
- Waterhammer pulse
- Apex- hyperdynamic
- Systolic murmur
- Heart sounds: S1 soft, P2 loud, widening of A2- P2 split (due to early
closure of MV), LVS3/S4 may be present
- Murmur- A pansystolic blowing murmur, best heard at apex, radiating to
axilla & back (thru’AML) or Lt. Parasternal region (thru’ PML), with
patient in left lateral position, with diaphragm of stethoscope, exercising
(clinching fists), no relation of respiration, flow murmur across MV.
[Note:The sign of severity of MR is the presence of LVS3]
Q-What is Carvallo’s sign?
A-It is to differentiate between TR Vs MR. With inspiration if the loudness of murmur, it
is a TR murmur.
Q-Which MV disease is associated with a midsystolic murmur?
A-MV prolapse.](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-78-320.jpg)
![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 79
Q-What are the reasons for a normal CT ratio in a patient with MR?
A-Reasons are:
- Acute MR (infective endocarditis, post MI MR, trauma, post
BMV/OMC/CMV)
Q-What are the reasons for silent MR?
A-Reasons are:
- Paravalvar leak
- Post myocardial infarction MR
- Obesity
- Emphysematous chest
AORTIC STENOSIS
Etiology:
1) Valvar
- rheumatic
- congenital
- atherosclerotic
- degenerative
2) Subvalvar
- idiopathic subaortic stenosis
- HOCM
3) Supraaortic
- diffuse hypoplastic
- hourglass
- membrane shelf
Signs:
- pulsus parvus et tardus
- heaving apex
- systolic thrill over the aortic area & carotids
- Heart sounds- S1 normal, S2: soft A2 with narrow A2- P2 split, LVS3/ S4
may be present, ejection click may be present.
- Murmur- Harsh ejection systolic murmur, cresendo decresendo in nature,
heard best over the aortic area & apex, radiating to carotids, heard best
with the diaphragm of the stethoscope with the patient sitting & leaning
forward & breath held in expiration.
Findings of severe AS are:
- increased harshness of murmur
- late peaking of murmur
- soft S2
- pulsus parvus et tardus
[Note:The sign of severity of AS is the late peaking of murmur]](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-79-320.jpg)


![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 82
diaphragm of the stethoscope with the patient sitting, leaning forward &
breath held in expiration.
- Austin Flint murmur may be present
- Murmur of functional AS may be present (with/ without a thrill)- this is
the only functional murmur that may be present with a thrill.
[Note:The sign of severity of AR is the length of murmur]
Q-What does the site of murmur of AR suggest?
A-If heard best in:
- Erbs area- there is no dilatation of the aortic root- rheumatic
- Aortic area- there is dilatation of the aortic root- Marfans (connective
tissue)
Q-Describe the clinical detection of acute AR.
A-Acute AR is suggested by the presence of:
- acute onset of symptoms
- soft S1- due to closure of MV even before the onset of ventricular systole,
due to acute LVVO.
- Absence of peripheral signs of AR
(If there is echo e/o MV preclosure, then the prognosis is grave, unless
immediate surgical intervention is done)
Q-What is the importance of Austin Flint murmur?
A-Its presence suggests that at least moderate AR is present.
Q-What are the causes of Austin Flint murmur?
A-Reasons advocated are:
- AR jet hitting upon the AML hence producing vibrations
- AR jet hitting the jet coming from LA to LV.
Q-Why is the AR murmur never more than Grade III?
A-As it is high pitched (& hence there is no thrill too).
Q-Discuss Syphilitic AR.
A-It has the following features:
- minimum 9 years post primary syphilis
- congenital syphilis is very rarely affects the AV
- often associated with coronary osteal narrowing- angina, importance is for
impaired cardioplegia delivery
Q-Describe the criteria for dilated aortic root.
A-
- Displacement of coronary ostia > 20 mm from the annulus
- Diameter of annulus > 1.5 times normal (in Marfans > 1.34 times; operate)](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-82-320.jpg)


![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 85
ECHOCARDIOGRAPHY IN VALVULAR HEART DISEASE
MITRAL STENOSIS
M Mode: Findings are
1) Due to slow closure of MV in early diastole the EF slope is markedly diminished
2) Diminished mobility causes a reduced DE amplitude
3) Thickened leaflets
4) Anterior movement of PML
Discrepancy:
- In patients with AS/ AR, with normal MV the EF slope is diminished-
hence it is unreliable & obsolete
- 20% of patients of MS will not have anterior movement of PML
2 D Echo: is the principle means of evaluating valvular pathology in MS
Features are
1) Doming of AML in diastole (due to inability of valve to accommodate all the
blood available for delivery into the LV)
Doppler: Shows
1) Rate of decrease in diastolic flow after E point
2) Accentuation of ‘A’ wave (absent in atrial fibrillation)
3) Pressure half time (the time required for the peak gradient falls to half) for valve
area.
MVA= 220/ PHT
4) Valve area by continuity equation
A1 x V1= A2 x V2 (A1= AV area, V1= velocity across AV, A2= MV area, V2=
velocity across MV)
A2= [A1 x V1]/V2
(this is provided there is no AR/MR)
MITRAL REGURGITATION
(Primarily by color Doppler)
M MODE & 2D ECHO:
Features are
1) Size of LA
2) Pulsation of LA wall
3) Size of LV
4) AV motion
5) IVS motion patterns
6) Thickening & fibrosis of MV
COLOR DOPPLER:
1) Measure jet area of the maximum regurgitant jet & compare as a ratio with area of
the LA
2) PISA (Proximal isovelocity surface area)- depends upon principle of flow
acceleration proximal to a narrowed or regurgitant orifice.](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-85-320.jpg)
![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 86
AORTIC STENOSIS
M MODE: shows
1) Thickened & immobile leaflets
(M Mode for determining valvar pathology, in AS, is no longer done)
2) LV wall thickness
2 D ECHO:
1) Systolic doming
(Systolic doming is the most important 2 D Echo finding of any valvar stenosis)
DOPPLER
1) Pressure gradient across the AV using modified Bernoulli’s equation
2) AV area by the continuity equation
AV area= [LVOT (area) x LVOT (velocity)]/ AS (velocity)
3) Measurement of ejection time
AORTIC REGURGITATION
M MODE:
1) Fine fluttering of AML
2) Fine fluttering of IVS
(no longer performed)
2 D ECHO:
1) Reverse doming of the AML
COLOR DOPPLER:
1) Size of jet
2) PISA
3) Rate of decline of the AV regurgitant velocity- diastolic decay. (the rapidity with
which the aortic & LV pressures equalize is a function of the severity of AR)
Q-What are the types of IVS movement on M mode?
A-
- Type A into LV during systole – Normal
- Type B straightening of IVS in systole
- Type C No movement
B & C are paradoxical movements
Q-How is Qp/ Qs, on echo, calculated?
A-
Q= Mean velocity x Time x Cross-sectional area](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-86-320.jpg)





















![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 108
[Note: Rarely an ASD may cause severe problems in infants. In these conditions an
associated PV obstruction should always be ruled out.]
Q-How to determine the situs?
A-Situs may be ascertained by:
1) Clinically
- Liver dullness on right side
- Fundic bubble on left sie
- Left testes is lower
2) X-ray
- Trachea is to the left
- Liver & fundic bubble
- Brochial anatomy
- Splenic flexure is to the left
3) Echo-
- Crista terminalis for RA- on right sie
- Rt. sided SVC/ IVC
[Note: Generally abdominal situs is concordant with atrial situs]
Q-Bimodal presentation is seen in which cardiac conditions?
A-The conditions are:
1) Ebstein’s anomaly
2) ASD
3) Coarctation aorta
4) Pulmonary stenosis
Reasons for bimodal presentations are:
Ebsteins- child born with increased PVR & hypoplastic RV cyanosis. Later the PVR
falls improvement in cyanosis. 3rd or 4th decade the RV fails recurrence of
symptoms.
ASD- 10% are symptomatic in infancy that later resolves only to become resymtomatic
later.
Coarctation- CCF in 1st month of life.
Q-Which conditions are associated with LV dominance?
A-The conditions are:
1) Tricuspid atresia
2) PA with intact IVS
3) Single ventricle
4) AV canal unbalanced to the left
5) Ebstein’s anomaly
Q-Which condition has shunt at more than one level?
A-AV canal.](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-108-320.jpg)


![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 111
Q-What is the surgical risk in relation to PVR & SVR?
A-Normal SVR=15-20 Woods & normal PVR=1-2 Woods
Depending upon the PVR/ SVR ratio the risk may be determined
- < 0.25 - normal
- 0.25- 0.5 - mild risk
- 0.5- 0.75 - moderate risk
- > 0.75 - high risk
- > 1 - contraindication for surgery
Q-What are the types of congenital MS?
A-It depends upon the level of obstruction. It could be at following levels:
1) Supravalvar: Supravalvar ring (D/D with cor triatriatum sinister)
2) Level of MV annulus & leaflets: double orifice MV
3) Level of chordea & papillary muscles:
- Funnel valve
- Parachute valve
- Hammock valve
Q-What are the components of Shone’s complex?
A-It was described in 1963 & includes a constellation of
1) Supramitral ring
2) Parachute MV
3) Subaortic obstruction
4) Coarctation aorta
[Note-Bolling’s postulate: The MS causes an increased PAP leading to paradoxical
movement of IVS into LV, leading to LVOT obstruction.]
Q-Describe ECG characteristics of important CHD’s?
A-
Common AV canal:
1) Prolonged PR interval
2) Axis- Left & up or indeterminate
3) Counterclockwise loop
Primum ASD/ common atrium:
1) Axis- left & up or indeterminate
2) Counterclockwise loop
c-TGA
1) q in right sided leads-I, AvR, V1, V4R
Sinus venosus ASD-SVC type
1) Coronary sinus rhythm- p in II, III & AvF is inverted & upright in I.
Q-What is the ideal age for a fetal echo?
A-At 18 weeks gestation.](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-111-320.jpg)



![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 115
Q-What is contrast echo?
A-Agitated saline is injected into the antecubital vein that reaches the RA & is seen as an
echo contrast. If an ASD is present, jet of blood from LA (due to left to right shunt) shall
cast a negative shadow in this echobrightness of agitated saline.
[Note:If injected thru’ the left basilic vein, a simultaneous diagnosis of a left SVC may
also be obtained.]
Q-Which is the best view to visualize ASD on echo?
A-The subcostal view.
Q-If which conditions are surgery not advised for an ASD?
A-If
1) Qp/ Qs < 1.5/1
2) Eisenmengerization
3) Age of > 40 years (?)
Q-What are the indication of cardiac cath in ASD?
A-The indications are:
1) For operability
2) R/o associated coronary artery disease
3) Device closure
Q-Why, in an ASD, is the shunt left to right?
A-Due to:
1) RA is more complaint than LA
2) TV is larger than MV
3) RV is the volume loading ventricle
Q-What are the causes of a ‘large aorta’ in a patient with an ASD?
A-Possible conditions are:
1) Systemic hypertension
2) PDA
3) Associated AV disease
Q-Which patients of ASD have a CTR > 65%?
A-The possible reasons are:
1) Common atrium
2) AV canal
3) TAPVC
4) ASD with MS
5) CCF (4th/ 5th decade)](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-115-320.jpg)




![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 120
Q-Why, in a large VSD, initially there is only LVVO & no RVVO?
A-With a moderate or large VSD, when the LV contracts, it pushes the blood across the
VSD straight into the PA (as the RV is also contracting). The RV hence acts like a
conduit. In diastole, the excess volume reaches LV from the LA leading to LVVO, while
the RV receives normal volume form the RA.
Q-What is the natural history of VSD closure?
A-Spontaneous closure is seen in 25- 40%.
90% of those determined to close shall close by 10 years.
[Note: Why 10 years? A-because the heart has grown to normal size by then.]
Q-What are the ways of spontaneous closure of VSD?
A-The mechanisms are:
1) Overgrowth of nearby tissue (while the VSD does not grow, hence closes)
2) Septal tricuspid leaflet
3) Aneurysm of IVS
4) RCC/ NCC prolapsing
5) Infective endocarditis.
Small defects: most (80%) close on their own
Moderate VSD: 50% will close or reduce in size, not requiring intervention
Large VSD: rarely close
Q-Which are the conditions wherein a patient with a VSD becomes symptomatic at later
age?
A-It maybe due to:
1) AR
2) Infective endocarditis- AR, PR, myocarditis
3) Pneumonia/ LRTI
4) Acquired heart disease
Q-Generally by what time does AR develop in a patient with VSD?
A-Generally by 5- 9 years.
Q-In a child with Trisomy 21, what are the additional problems that complicate the heart
disease?
A-The associated problems are:
1) The above factors of elevated PAP due to L-R shunt
2) Multiple level shunt
3) Primary abnormality in lung (there in decreased number of alveoli & blood
vessels, leading to early development of PH)
4) Due to mental retardation, there is underestimation of symptoms.
5) Due to upper respiratory abnormality that makes it more prone to infection.](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-120-320.jpg)

![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 122
Q- How to differentiate between gasulisation & TOF?
A-In Gasulisation:
1) There is late onset cyanosis
2) LV is well developed
3) Malaligned VSD is absent
4) Predominantly infundibular narrowing
5) No aortic override
[Note:Small VSD’s pose a threat of infective endocarditis. Risk of IE Vs morbidity/
mortality of surgery favors no intervention of small/ moderate sized VSD. But once 1
episode of IE has occurred, surgery should be performed, as chances of re IE are high.]
Q-What measures may be taken if a VSD is not found during surgery?
A-The techniques that maybe used are:
1) See for jet effect on the RV myocardium
2) Deliver cardioplegia & visualise VSD
3) Detach STL
4) Open aorta & see from the LV side
Q-Which anaesthetic drugs worsen PH?
A-The drugs are:
1) Ketamine
2) Nitrous oxide
Q-What is the timing of surgery in VSD?
A-There are various protocols.
An acceptable protocol is mentioned below-
For Large VSD’s:
Infancy: No surgery if- coarctation, Swiss cheese
Surgery
Early (if large with uncontrolled CCF) Others by 6 months (wait for spontaneous
closure)
If PVR > 4 Woods/ m2, or If PVR < 4 Wood/ m2
PASP > 50% of SBP
Surgery Defer surgery till 12 months
Till 1 year of age, a VSD with however high the PVR is operable.](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-122-320.jpg)


![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 125
PDA
Q-When to term PDA?
A-When the ductus arteriosus fails to close spontaneously by 3 months of age.
Q-Why should even a small PDA be closed?
A-Because the risk of IE is high.
[Note:’PDA diagnosed, PDA should be closed’.]
Q-What is the risk of IE in PDA?
A-0.4/100/year.
Q-Describe the timing of surgery in PDA.
A-As follows:
Symptomatic: Should undergo immediate closure
Asymptomatic: Wait till 8 weeks, If does not close, it requires closure. (Optimum age for
closure is between 6- 12 months)
Inoperability- like VSD
Q-What is the ‘only’ sign of communication at the great arterial level?
A-A ‘continuous murmur’ is the only sign of communication at the great arterial level.
Q-What is the natural history of PDA?
A-It is as follows:
Small- only risk of IE (which is high)
Moderate & large- High risk of development of PH (1/3 rd by 30 years & 2/3 rd by 40
years)
Q-What is the difference between a ductus arteriosus & other arteries?
A-The ductus has the following features:
1) Spiral arrangement of muscles in the media
2) Higher content of hyaluronic acid in the media
3) Response seen to O2 & prostaglandin’s.
Q-What are the anatomical types of PDA?
A-They are:
1) Conical- with narrow end towards PA.
2) Tubular
3) Conical- with narrow end towards aorta (rare)
Q-History of PDA surgery?
A-
1937: by Streider- patient died due to gastric distension & aspiration
1939: by Gross- first successful PDA clsoure.
Q-In a right aortic arch which side will the PDA be situated?
A-Mainly on left: going to the left SCA or even a more distal artery.](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-125-320.jpg)





















![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 147
In RA approach:
- stay sutures over the RA & STL
- additional retractor in the TV
- if required detachment of the STL
Q-What are the dimensions of a RVOT patch?
A-The dimensions should be such that the:
- Length is 1 ½ times the incision length
- Width should be 3 times more than the proposed increase in diameter
Q-In a deeply cyanosed child how much Hct is generally maintained, on bypass?
A-Around 45%.
Lower Hct may lead to:
- Capillary leak syndrome
- Excessive prime requirement.
Q-What is the cause of ‘low pressure’, on CPB, in TOF?
A-They are:
- Hemodilution
- Collaterals
Q-What are the management strategies for excessive LA return; in a patient with TOF?
A-Management strategies includes:
1) Adjust flows, cool further
2) Search for PDA
3) Open pleura, retract lung to visualize the descending thoracic aorta- visualize any
obvious collaterals & tackle
Q-Discuss post ICR TOF arrhythmias.
A-Using Holter monitoring, ventricular arrhythmias can be detected in 40- 50% of
patients in the postoperative period.
Predictors of arrhythmias are:
1) Age of surgery
2) Moderate/ severe PR
3) Ventricular dysfunction
4) Prolonged QRS interval (> 180 msec)
[Note:RBBB is common after TOF surgery but complete heart block is rare.]
Q-What is the incidence of complete heart block post ICR TOF?
A-Less than 1%.
Q-What is the incidence of RBBB +/- LAHB post ICR TOF?
A-20- 25%.
Q-Which heart block, post ICR TOF, has poor prognosis?
A-RBBB with LAHB (there is higher chance of sudden death)](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-147-320.jpg)


![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 150
Q-What is the definition of ‘DORV’?
A-The various definitions of DORV are:
1) Anderson- 2 criteria must be fulfilled to call DORV
i) > ½ circumference of each semilunar valve overlies the morphological
RV
ii) Persistence of a subaortic conus with loss of aorto mitral continuity.
2) Neufeld- criteria for DORV are:
i) Both great arteries arise from morphological RV
ii) Loss of continuity between both AV valves & semilunar valves
iii) VSD may or maynot be present, & if present, then may represent the
only outlet for LV
iv) Valvar/ subvalvar PS may or maynot be present.
3) Lev- criteria for DORV are:
i) One great artery & > ½ of other great artery arising from
morphological RV
ii) Loss of aortomitral or pulmonary mitral continuity
4) Van Praagh- DORV is defined as;
i) Persistance of subaortic/ subpulmonic conus leading to loss of
continuity with the MV.
Q-What is the importance of juxta posed appendages?
A-The importance lies in:
1) For association with diseases like:
- TA-II
- TGA
- DORV, VSD, subpulmonic VSD
2) For performing procedures like:
- Atrial septectomy
- Contraindication to a Senning’s
[Note:Left sided juxta posed appendages are more common than right sided.]
Q-What is the embryology of DORV?
A-It is due to abnormal development, rotation & absorption of the conal septum.
Q-Discuss the embryopathology of TOF, DORV & TGA.
A-Seen from above, there is a counterclockwise rotation of the aortic conus.
In the various conditions, the following features are noted;
- TOF- absorption of septum (in mid portion of bulboatrioventricular
ledge)- responsible for aortomitral continuity
- DORV- non absorption of BAL
- TGA- absorption of left margin of BAL- establishment of
mitralpulmonary continuity.](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-150-320.jpg)

![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 152
Q-What is the incidence of HLHS?
A-It is the same as PDA, coarctation. (7% of CHD)
Q-What are the ‘Ten commandments’ of Choussat?
A-The criteria required for a candidate to be eligible for a Fontan operation were laid
down by Choussat. They are:
1) Age > 4 years & < 15 years
2) Normal sinus rhythm
3) Normally draining systemic veins
4) Normal RA (complaint)
5) PA anatomy: Nakata > 250 mm2/m2 & McGoons > 1.5/1
6) No distortion of PA anatomy
7) PVR < 2-4 Wood
8) PASP < 15- 20 mm Hg
9) No left AV valve regurgitation
10) Normal LVEF
[Note:These indications have undergone changes & many are no longer a
contraindication for a Fontan operation]
Q-What are the measures to be taken in a patient with a Glenn shunt having increased
cyanosis?
A-The options are:
1) Additional BTS
2) Make Glenn pulsatile by creating a right axillary artery-vein fistula
3) Investigate for presence of pulmonary AV fistula
Q-What are the causes of PS with intact IVS?
A-They are:
1) Congenital- 6 types: tricuspid (Williams), bicuspid, unicuspid with central
opening, unicommisural, hypoplastic annulus, dysplastic.
2) Dysplastic (Noonan’s).
Q-What is the worst complication of Fontan?
A-The most dreaded complication after a Fontan is Protein losing enteropathy.
It is associated with a high mortality.
Treatment options include administration of Heparin & SOS takedown of Fontan/
conversion to 1 ½ repair.](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-152-320.jpg)



![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 156
Q-What are the indications for operating a patient with Ebstein’s anomaly?
A-The indications can be summarized by the pneumonic ‘ABCDE”
ABCDE
a) A- Arrhythmias refractory to medical treatment
b) B- Breathing room air O% < 80%
c) C- CTR > 65%
d) D- Dyspnea III, IV
e) E-
- Paradoxical Embolism
- Echo; Tajik’s score > 2
In general the indications for surgery are:
1) Symptoms
2) Cyanosis
3) RVF
4) CTR > 65%
5) Arrhythmias
6) Paradoxical embolism
Q-What is Tajik’s score?
A-It is an echo based score. It is as follows:
Criteria Score (total= 13)
ATL tethering- severe 3
ATL immobile 2
ATL tethering- mild 1
ATL displacement 1
STL absent 1
RA > 60 mm/m2 1
TV regurgitation with prolapse 1
Functional RV < 0.35 2
RVOT aneurysmal 1
Depending upon the score the management maybe decided:
< 2: conservative treatment
2-5: repair advised
> 5: replacement advised
Q-Describe the JACC mortality assessment for Ebsteins.
A-For determining postoperative mortality.
[RA + atrialized RV]/ [functional RV + LA + LA]
If the above is:
< 0.5= 0% mortality
0.5- 1.0= 10% mortality
1.5= 44% mortality
> 1.5= 100% mortality](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-156-320.jpg)





![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 162
Q-During a left BTS what structure may be lying in front of the LPA?
A-A large lymph node
Q-During a BTS how many branches of distal LPA are to be looped?
A-3 (2 of upper lobe & 1 of lower lobe.)
Q-Discuss strategies if LPA is not seen during BTS?
A-The options are:
1) Check dissection
2) Open pericardium & anastomose to MPA
3) If large MAPCA seen entering hilum- a shunt to the MAPCA
4) Close & turn patient to opposite side
Q-What are the cause of bradycardia on clamping the LPA?
A-The reasons maybe:
1) RPA absent/ osteal stenosis/ hypoplastic/ non confluent
2) Isolated left lung ventilation
3) Vagus nerve included in the clamp.
Q-What measures are to be taken if bradycardia occurs?
A-
1) Check bilateral ventilation
2) Allow re-expansion of lung & then start
3) Check inclusion of vagus in clamp
4) Try side clamping the artery
5) BTS to upper lobar artery.
Q-What is the size of Goretex to be used for a MBTS?
A-
1) A Protocol by age followed at our institute is:
- if < 6 mnths- 4 mm
- 6mnths to 2 years- 5mm
- 2 to 6 years- 6mm
- > 6 years- 8mm
2) Protocol by weight (at JJH)
- < 7 Kg- 4mm
- 7 to 12 Kg- 5mm
- 12- 20 Kg- 6mm
- > 20 kg- 8mm
3) Graft size by body weight & BSA (Miki, Ueda)
Diameter of graft = 1.88 (body weight) + 1.8
= 0.87 (BSA) + 5.3
[Note:However the decision for the size of Goretex is ultimately based on the size of
the SCA]](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-162-320.jpg)
![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 163
Q-What is the concept of Qb/Qs?
A-
(Qb- flow thru’ shunt, Qs= systemic blood flow)
Ideal Qb/Qs [by Miki, Ueda (Ann Thorac Surg 1987)] is 30- 40%.
Ideal Qb index is= 1.6- 2.4 litres/ min/ m2.
Q-What care should be taken with Gore-Tex?
A-The following precautions should be followed.
1) Cut with a sharp knife
2) Do not crush
3) Avoid multiple punctures.
Q-What are the alternatives if Gore-Tex is not available for a BTS?
A-The options are:
- Classical BTS
- Use maternal saphenous vein
- Use Dacron
Q-What are Gore-Tex sutures?
A-They are hygroscopic & hence clog the needle holes
Q-What is the management of an “on table” cyanotic spell?
A-Clamp the descending thoracic aorta (acts like “squatting”).
Q-Discuss intraoperative techniques to ensure patency of graft?
A-The following techniques should be followed:
- Taking all sutures under vision
- All sutures inside-out on the artery
- Lie & length of graft should be appropriate.
Q-What is the technique of air removal after a modified BTS?
A-The clamps over distal PA & distal SCA are released - followed by proximal PA & the
proximal SCA clamps (never needle puncture Goretex as it will lose its
electronegativity).
Q-What are the signs of good shunt functioning?
A-They are:
a) Graft related-
- sweating
- thrill over PA
b) Hemodynamics related-
- improvement in O%
- fall in DBP](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-163-320.jpg)





![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 169
Q-What is the 2 chamber method?
A-For calculating RV volume.
RV shoot in lateral view is taken.
Volume of infundibulum (cylinder)= r2h
Volume of body (ellipsoid)= 4/3 r2 (LL/2)
r= radius of ellipsoid
LL= largest length
RV volume= sum of infundibular & body volumes
Q-What is the Area-length method?
A-For calculating the LV volume.
Volume= 4/3 x r(AP) x r(lat) x (LL/2)
r(AP)= radius in AP view
r(Lat)= radius in lateral view
Q-What are normal RV & LV volumes?
A-They are:
Normal LVEDV (in ml)= 72.5 x BSA
Normal RVEDV (in ml)= 75.1 x BSA
Q-What is the normal position of IVS?
A-Normally is LAO 60 but in c-TGA is anteroposterior.
[Note:One cannot determine the shunt direction on a ventricular shoot, as the force of
injection is very powerful.]
Q-Onplain fluoroscopy how will one determine that the catheter is in LV & not in RV?
A-In lateral view the catheter will overlap the spine.
Q-What are the catheters for PA?
A-They are:
1) Berman (balloon tipped catheter)
2) Grollman PA seeking catheter
Q-What are the views taken during cath, for TOF?
A-The views are:
- For LPA- LAO
- For RPA- RAO
- RVOT- RAO
- Coronary- LAO caudal
- Lateral view for- IVS, infundibulum, relation of great vessels, coronary crossing
RVOT.
Q-Howmuch contrast is normally injected?
A-5 cc/ Kg.](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-169-320.jpg)
![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 170
Q-Which catheters are used for cardiac cath in TOF?
A-Venous catheters- Berman (Balloon tipped), NIH
Arterial- Pigtail
6F= 2mm diameter, 7F= 2.3 mm diameter
Q-Describe specific cath findings in TOF?
A-The specific findings are:
Oximetry- there is a step down of oxygen saturation at ventricular level & further step-
down at the ventriculoaortic level.
Pressure- There is equalization of peak systolic pressures of LV & RV with a gradient
across the RVOT.
Q-What are the indications for cath in TOF?
A-Cath is performed in TOF for:
1) PA anatomy
2) MAPCAS
3) Coronary crossing RVOT
4) Additional VSD
Q-What are the indications for LV angiography in TOF?
A-They are:
1) Additional VSD
2) LV function (performed in adults)
3) Aortic override
4) Aortomitral continuity
Q-What are the possibilities of a catheter not entering PA in a TOF?
A-The possibilities are:
8) Severe PS
9) Pulmonary atresia
10) Posteriorly placed PA
Q-In TOF, why RVOT shoot is performed in RAO?
A-Because
1) The overlapping spine is taken away from the RVOT
2) Parietal & septal bands are well seen
Q-Which is the view for estimating PA ratio’s?
A-LAO cranial. Both the PA’s and the descending aorta are well seen in this view.
Q-What is the use of lateral view in TOF?
A-It is to visualize the RVOT & IVS
[Note: The PA cannot be seen well in the lateral view. The RPA will be seen as a coin &
the LPA as a comma.]](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-170-320.jpg)







![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 178
H) With previous CABG
Class I:
1) Disabling angina despite maximal noninvasive treatment
Class IIa:
1) Bypassable distal vessel with a large area of threatened myocardium on
noninvasive testing
Class IIb:
1) Ischemia in non LAD distribution with patent internal mammary artery to LAD
graft and without aggressive attempt at medical treatment &/or percutaneous
revascularization
Q-What are dilated coronary arteries a feature of?
A-Of:
1) SVAS
2) HOCM
3) Coronary A-V fistula
Q-Which are the various arterial grafts used for CABG?
A-The can be classified as:
1) Somatic
- Internal mammary artery
- IEA
- Subscapular artery
2) Splanchinic
- GEA
- Inferior mesenteric artery
- Splenic artery
3) Limb
- Radial
- Ulnar
[Note:Other grafts that can be used are:
- Veins
- Permaflow (PTFE)
- Bovine carotid
- Bovine internal mammary artery]
Q-What are the advantage of the internal mammary artery?
A-Internal mammary artery is:
1) Pedicled
2) Has less muscle, hence less prone to spasm
3) Endothelium releases prostacyclin, hence less atherogenic
4) Artery size is similar to the size of the coronary artery
5) Ability to alter flow according to the need of the myocardium
6) It reaches all coronaries](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-178-320.jpg)
![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 179
Q-Which is the most vulnerable period for a ventricular fibrillation?
A-In the period post myocardial infarction the heart is most vulnerable for VF. Occurs if
an ectopic occurs in the midportion of ‘T’ wave (as some portion of the ventricular
myocardium is depolarized & some incompletely or completely repolarized.)
Q-What are the branches of internal mammary artery?
A-The branches are:
1) Pericardiophrenic artery
2) Anterior intercostals arteries: 4- 10 in number
3) Sternal branches: 4- 10 in number
4) Perforating branches: 3- 6 in number
5) The artery terminates by:
- bifurcating (in 93%) into
- superior epigastric
- musculophrenic artery
- trifurcating (in 7%)
- superior epigastric
- musculophrenic artery
- diaphragmatic branch
Q-How to test adequacy of internal mammary artery flow on table?
A-Flow should be more than 90 ml/ min.
Q-What measures are to be taken if the internal mammary artery does not have a good
flow?
A-The possibilities and the subsequent action are:
1) In spasm- instill papaverin in surrounding tissues
2) Check entire length for occlusion & test luminal patency with metal dilator
3) Check for perforators (especially 2,3 & 4th, which may be large & steal blood)
4) Check for pericardiophrenic artery
Q-What are the complications of internal mammary artery harvesting?
A-The complications are:
1) Injury to the phrenic nerve
2) Deep dull retrosternal pain#
3) Rarely breast necrosis
(# it is believed to be due to cautery burning of the anterior intercostals arteries which
conduct the heat to the nerves in the intercostals spaces, causing neuralgia. Hence
some advice to use clips on either side & cut in between)
Q-What are the contraindications for harvesting internal mammary artery?
A-They are:
For unilateral IMA harvesting:
1) Definitive: subclavian artery stenosis
2) Relative: emergency CABG [to a) save time, b) inability to perfuse ima graft, c)
adverse effect due to use of postoperative vasoconstrictors]](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-179-320.jpg)







![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 187
CONSTRICTIVE PERICARDITIS & TUMORS
CONSTRICTIVE PERICARDITIS
Q-What is the etiology of constrictive pericarditis?
A-The possible causes are:
1) Idiopathic
2) Tuberculosis
3) Dressler’s syndrome
4) Radiation
5) Uremia
6) Drug induced- procainamide/ hydralazine
7) Post operative (especially if Betadine washes used- Miller & Mansoor, Ann
Thorac Surg 1982, showed a 20 times higher incidence of postoperative
constrictive pericarditis with betadine washes)
[Note:All conditions causing acute pericarditis can cause subsequent constrictive
pericarditis except rheumatic carditis.]
Q-What are the cath signs of constrictive pericarditis & discuss its D/D with restrictive
cardiomyopathy.
A-The cath signs of constrictive pericarditis are:
1) RA mean pressure > 10 mm Hg
- Mild: 10- 15 mm Hg
- Moderate: 15- 20 mm Hg
- Severe: > 20 mm Hg
2) Equalization of diastolic pressures in all the 4 chambers (within 5 mm Hg)
[in restrictive cardiomyopathy the LVEDP (PCWP) is > 5 mm Hg higher than the
RVEDP]
3) RVEDP > 1/3rd RVESP
[in restrictive cardiomyopathy RVEDP < 1/3rd RVESP]
4) Positive square root sign
5) Positive Kussmauls sign
6) Thickness of pericardium on fluoroscopy > 5 mm
7) Fluid challenge (500- 1000 ml of normal saline over 6-8 minutes) will lead to
persistent elevation in CVP
8) Endocardial biopsy
[in restrictive cardiomyopathy will show an infiltrative pathology]
9) Pulmonary hypertension will be negative
[in restrictive cardiomyopathy will be positive]
10) RV angiography will show blunting of apex (Ballet Dancers shoe)](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-187-320.jpg)


![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 190
AORTA, LUNG & MEDIASTINUM
ANEURYSM
Q-What are the current recommendations, for surgery, on patient with aneurysm aorta?
A-They are:
1) All symptomatic
2) Asymptomatic if
- > Twice the size of normal contagious aorta
- > 5 cm diameter for ascending aorta, > 5 cm for arch, > 6 cm for
descending aorta
- Documented enlargement of the aneurysm
- Progressive AR in c/o an ascending aortic aneurysm
Q-Describe the classification systems for dissection of aorta.
A-The various systems are:
1) Debakey- Type I, II, IIA & IIIb
2) Stanford- A & B (given by Daily et al)
3) Applebaum- ascending & descending
4) Meng- Anterior & posterior
Q-What is etiology of ascending/ arch aortic aneurysm?
A-They are:
1) Marfans, Ehler Danlos (leading to cystic medial necrosis)
2) Syphilis
3) Arteriosclerosis
4) Chronic dissection
5) Mycotic aneurysm
6) Arteritis
Q-What is the etiology of descending thoracic aortic aneurysm?
A-They are:
1) Atherosclerosis
2) Same as above
[Note:Clot formation in an aneurysm confers no benefit or protection against rupture.]
ASOV
Q-What is the etiology of ASOV?
A-The causes maybe:
1) Syphilis
2) Medial necrosis
3) Atherosclerosis
4) Rarely endocarditis
Q-What is the advantage of a bicameral approach for RASOV?
A-A missed VSD will be detected.](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-190-320.jpg)



![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 194
Q-What are the accessory muscles of respiration?
A-The accessory muscles of respiration are:
1) Sternomastoid & trapezius
2) Scalenus anticus
3) Pectoralis major
4) Alae nasi
5) Latissimus dorsi & intercostals muscles (causing intercostals retraction)
[Note:The above muscles are arranged in the order in which they are generally
recruited]
Q-Who introduced double lumen tubes
A-Bjork & Carlens.
Q-What is the difference between Carlen & Robertshaw tubes?
A-Carlen’s tube has a carinal hook.
Q-Who introduced the Univent tube
A-Inoue.
Q-What are the causes of pneumothorax
A-The are:
1) Primary- bleb
2) Secondary- to
a) COPD
b) Cystic fibrosis
c) Congenital
d) Pneumonia
e) Endobronchial block
f) Tuberculosis
3) Traumatic
4) Iatrogenic
5) Therapeutic
Q-What are the types of high frequency ventilation
A-3 types
1) High frequency positive ventilation
2) High frequency jet ventilation
3) High frequency oscillation
Q-What are the types of Jet ventilation
A-2 types
1) Injector jet ventilation (uses a large TV of 500- 1500 ml at a slow rate of 10-30
breaths/ min)
2) High frequency jet ventilation (injects a small TV of 50- 250ml at a high rate of
60- 600 breaths/ min)](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-194-320.jpg)







![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 202
Q-What is the source of TB pericarditis
A-It could be from:
1) Adjacent structures
2) Lymphogenous
3) Hematogenous
Q-What is the incidence of TB pericarditis?
A-1% of all TB
[Note:There is a high incidence of coexistent pleural effusion]
Q-Discuss the diagnosis of TB pericarditis.
A-
Signs: effusion, muffled heart sounds, rub
In large effusions there will an area of dullness at the angle of left scapula.
Ewart’s sign: tubular breathing at the angle of the left scapula (due to compression of the
underlying lung)
ADA levels: Generally seen 100 IU/L Vs 20 IU/L (Abnormal Vs normal)
If it is > 40 IU/ L- it has a sensitivity & specificity of 93% & 97%
Q-What are the signs of active pulmonary TB on a CT scan
A-They are:
- Tree in bud appearance
- Cavity with fungal ball
- Pleural effusion
- Granuloma
Q-What are the signs of active TB on X Ray
A-They are:
1) Cavity with or without fungal ball (generally in the posterior segment of upper
lobe or superior segment of lower lobe)
2) Lymph nodes (especially in children)
3) Hydropneumothorax
4) Spontaneous pneumothorax
5) Consolidation
6) Military pattern
OTHER MEDIASTINAL
Q-What is the staging of Corrosive ingestion
A-(Endoscopic staging)
Stage 1: Mucosal hyperemia
Stage 2a: Superficial ulcers
Stage 2b: Deep ulcers
Stage 3: Necrosis
Stage 4: Stage 3 + systemic metabolic derangements](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-202-320.jpg)



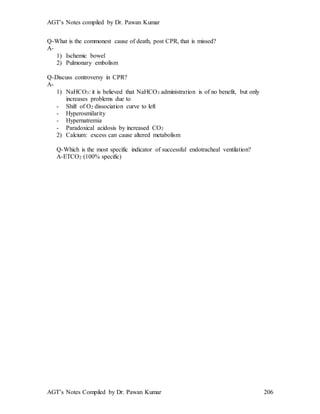









![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 216
Heparin
Q-Who discovered heparin?
A-McLean in 1916.
Q-What is the mechanism of action of heparin?
A-It requires the presence of antithrombin III for its action.
Heparin binds to AT III brining about a conformational change converting AT III
from a slow progressive thrombin inhibitor to a very rapid inhibitor.
[Note:Only 1/3rd of the administered dosed of heparin binds to AT & this fraction is
responsible for most of its anticoagulant effects.]
Mechanism of action is as follows:
1) The heparin- AT III complex inactivates a number of coagulation enzymes;
including Thrombin factor IIa, Xa, Ixa, XIa & XIIa. The major effects are due to
inhibition of IIa & Xa.
2) Binds to heparin cofactor II & catalyses inactivation of IIa.
3) Binds to platelets- contributing to the hemorrhagic effects of heparin.
XIIa ← AT III- heparin complex
↓
XIa ← AT III- heparin complex
↓
IXa ← AT III- heparin complex
↓
Xa ← AT III- heparin complex
↓
IIa ← AT III- heparin complex
↓
Fibrinogen → Fibrin
- molecular size= 3.000 to 30,000 daltons (approx.=15,000 daltons)
(- Mol wt. of LMWH= 5000 daltons_
Q-How is heparin cleared from the body & discuss the half life of heparin?
A-High molecular weight moieties are cleared more rapidly than the low molecular
weight moieties.
Heparin is cleared by 2 mechanisms:
1) Rapid- binding to the endothelial cell receptors and macrophages, where it is
depolymerised
2) Slower- renal.
This makes the anticoagulant response to heparin non linear at therapeutic doses, with
both the duration and intensity of the effect rising disproportionately with increasing
doses.
Thus the biological ½ life increases from
30 minutes with IV bolus of 25 IU/ Kg
to
60 minutes with IV bolus of 100 IU/ Kg &
to
150 minutes with a bolus of 400 IU/Kg.](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-216-320.jpg)

![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 218
Q-Enumerate heparin substitutes.
A-They are:
1) LMWH
2) Medium MWH
3) High MWH
4) Dermatans (Danaparoid)
5) Heparans
6) Heparinoids (Lomoparon)
7) Murine polysaccharides
Q-Which conditions can cause Heparin resistance?
A-Heparin resistance maybe seen in:
1) AT III deficiency- congenital/ acquired
2) Prolonged administration- in unstable angina/ IABP
3) Septicemia
4) Pregnancy
5) NTG treatment
Q-What is the management of heparin resistance?
A-Any of the following measures (or combination) maybe adopted:
1) Administering higher dose of heparin (up to 1000 IU/ Kg)
2) Accepting a lower ACT (up to 420 sec)
3) Administering 2-3 unit FFP or AT III concentrate
4) Using hirudin/ danapariod.
Nitric oxide
Q-What is the source of NO?
A-
Endogenous- negligible
Exogenous- from fossil, grains, NO donors (SNP, NTG etc)
[Note:Nitric oxide is termed as “The winner & killer drug” (as high doses may cause fatal
vasospasm)]
Q-What is the half-life of NO?
A-< 1 minute
Q-Discuss NO delivery system.
A-Special features of NO delivery are:
- Special ventilators with 2 posts allowing NO & O2 mixture to occur only at the
mouth of the endotracheal tube (If it comes in contact with O2, form NO2, which
is toxic.)
- Exhaust should be outside the building
- Multiple NO sensors in the ICU.](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-218-320.jpg)























![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 242
Clarence Walton Lillehei
- Father of modern cardiac surgery
- From University of Minnesota, Medical Center, Variety Heart Hospital,
Minneapolis
- Described hypothermia with inflow occlusion (with Lewis)
- Azygous flow principle
- Cross circulation (maternal)
- Autologous oxygenation
- Infusion of oxygenated blood only during CPB (but the reservoir would empty &
gas emboli)
- Biological oxygenation (using Baboon lung)
- Bubble oxygenator (along with DeWall)
- 1st open heart surgery & also 1st to perform OMC, AVR, TOF ICR, TAPVC,
TGA
- Proposed PML preservation
- Developed 3 valves:
-Lillehei Kaster valve- pivoting disc valve
-Lilehei Kalke valve- bileaflet valve with a 60 opening angle (only one
human implantation done & patient died within 24 hours)
-Lillehei Naqib valve- Toroidal disc valve (disc with central hole)
- First to describe external cardiac pacing
[Note:Indians trained under Lillehei are
- Dr. Gopinath & Dr. Kalke]
- Lillehei suffered from a left parotid malignancy for which 2 surgeries were
performed (radical resection with radical neck dissection & mediastinal
dissection)
Wills Potts
- Described Pott’s shunt
- Described the various types of vascular rings & slings
Denton Cooley
- Founded Texas Heart Institute
- Cooley’s clamp
- Cooley’s retractor for LA
- Concept of stone heart
- Waterston Cooley shunt
- Cooley’s vascular graft
- 1st heart transplant in US
- 1st artificial heart
- 1st aortic aneurysm surgery
- 1st LV aneurysm surgery on arrested heart
- LV apicoaortic conduit
- Developed Cooley Cutter valve](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-242-320.jpg)








![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 251
Actuarial survival was
- 85.6% at 10 years &
- 82% at 24 years
(mentioned in the article is- “it is not what you do, it is how you do it”)
14) Long term results of triple valve surgery,
Micheal Carrier, ATS 2002
Survival was
- 80% at 1 year
- 75% at 5 years
- 41% at 10 years
15) Current recommendations for adding aspirin to warfarin in patients with prosthetic
heart valves,
JACC 2001
i- patients with mechanical valves who suffer TEE despite adequate
anticoagulation
ii- those with ball in cage valve
iii- patients with mechanical valves with additional risk factors like
- h/o TEE
- af
- large LA (> 60 mm)
- CAD
- Ball valve
- > 1 mechanical prosthesis or a mechanical prosthesis in mitral position
TOF
1) TOF- What surgery at what age
M Pozzi, EJCTS 2001
Study duration: Between 1993- 1998.
Mean age: 16 mnths, mean wt.= 8.8
(75% of pts < 6 mnths)
Hospital mortality= 0%.
Rhythm- nsr=100%, RBBB= 21%
Conclusion- A primary repair of TOF can be performed at any age.
2) Pulmonary artery (Nakata) index
Seisuke Nakata, JTCVS 1984
Described an angiographic method of estimation of PA size in 4 group of patients, viz:
-Normal -TOF
-Rastelli -Fontan
Method: Diameter of right & left pulmonary artery just prior to the 1st lobar branches,
taken in systole & diastole (as there is a 20% difference in the sizes in the 2 phases)
PA index= [RPA area + LPA area] BSA in mm2m2
Normal index= 330 ± 30mm2m2](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-251-320.jpg)
![AGT’s Notes compiled by Dr. Pawan Kumar
AGT’s Notes Compiled by Dr. Pawan Kumar 252
Other ratio’s available are:
1) McGoon’s: [RPA + LPA diameter] diameter of aorta at level of
diaphragm
All taken in systole.
2) Muraoka’s index: Ratio of PA annulus to aortic annulus.
(the diameter of the MPA & ascending aorta vary depending upon the extent
of valvar & supravalvar stenosis, hence are not considered for estimation of
ratio)
3) Late PV replacement after ICR TOF
Dannielson, JTCVS 2001
42 pts with pulmonary valve replacement at mean age of 22 years & mean interval of 10
years. Post PVR:
5 year survival= 95%
10 year survival= 76%
Freedom from rePVR was
93% and 70% at 5 & 10 years
The significant risk factor for rePVR was young age at time of PVR
Lessons learnt:
1) Operate on asymptomatic TOF’s in deterioration of PR
2) Correct all concomitant lesions
3) Insert largest size PV (atleast or more than 25 mm)
4) Secondary Fallot
Circulation 1956, Gasul
5% of patients of VSD develop a RV infundibular hypertrophy which causes protection
of the pulmonary circulation- secondary Fallot
5) Long term results after early primary repair of TOF.
Richard Jonas, JTCVS 2001
57 patients, mean age= 8 mnths, mean wt.= 6.5 Kg
All under DHCA, transventricular approach. VSD closed with interrupted sutures
50% had a transannular pericardial patch.
FU= 23.5 yrs.
Results:
- 86% survival at 20 years (no difference whether patch used or not)
- Freedom from reintervention at 5 years= 93% and at 20 years= 79%
- Commonest cause of reoperation was RVOT stenosis (Vs PR as stated by most of
other studies)
6) A 26 years experience with surgical management of TOF- risk analysis for mortality or
late intervention
Christopher Knot-Craigh, ATS 1998
294 patients, mean FU of 10.6 years
All < 12 mnths age, operative mortality for primary repair= 2% and for staged repair=
11.8%.](https://image.slidesharecdn.com/agtnotes-200308161818/85/AGT-notes-252-320.jpg)









