Anesthetic management in Pediatric Neuromuscular disorders
- 1. Anesthetic Management of Pediatric Neuromuscular disorders DR GHULAM MOHAMMED MIR Assistant Consultant Anesthesiology , King Fahad medical City , Riyadh KSA
- 2. Neuromuscular Disease Neuromuscular disorders consist of conditions affecting: nerves: any or all components of the nerves, thereby producing sensory, motor, and autonomic dysfunction neuromuscular junction muscle: proximal and/or distal muscles
- 3. Cerebral palsy Originates from a non-progressive neurological insult sustained perinatally or before 2 yrs of age Predominantly affects the motor system, and the resultant spasticity and hypertonicity are progressive Infants generally have very low birth weight
- 4. Cerebral palsy Spastic: Lesion in cerebrum. Includes quadriplegia, diplegia, hemiplegia. Dyskinetic: Lesion in basal ganglia. Ataxic: Lesion in cerebellum includes tremor, loss of balance, and speech. Mixed: Includes spasticity and athetoid movements.
- 5. Cerebral palsy – preoperative Gastroesophageal: Reflux Impaired ability to handle pharyngeal secretions Increased salivation Respiratory Recurrent pneumonia (chronic aspiration and inability to cough) Reactive airway disease is common Neurological Seizures are present in roughly 30% - anticonvulsants. Musculo-skeletal Poor nutrition, contractures, fragile bones
- 6. Cerebral palsy – intraoperative Lower inhalational M.A.C., sensitivity to agents . Temperature:Hypothermia risk (↓ body fat, ↓ temp regulation) Poor bone quality – disuse osteoporosis, osteopenia, nutrition .
- 7. Peri-operative management Premedication includes sedatives, antiacids ,anticonvulsants,anticholinergicsand antidepressants and anti emetics. Have primary care taker during induction. Vascular access may be difficult. Careful positioning. Latex allergy has been reported Intra-operative hypothermia
- 8. Airway maintenance Excessive ,secretions and or a history of gastro-oesophageal reflux is a concern. Tracheal tube size selection should be based on their age as this usually provides the most appropriate fit.
- 9. DRUG RESPONSES Resistance to non-depolarising muscle relaxants. Reduced MAC relative to normal controls. Elevated pain threshold, decreased central pain perception
- 10. 1. Emergence from anesthesia may be delayed : Hypothermia Residual volatile anaesthetic agents Irritability on emergence from anaesthesia is common Pain Urinary retention. Unfamiliar environment.
- 11. POST JUNCTIONAL NEUROMUSCULAR DISEASE Muscular Dystrophy Myotonias Congenital myotonias Mitochondrial myopathies Channelopathies
- 12. Muscular Dystrophy Duchenne Muscular Dystrophy Becker’s Muscular Dystrophy
- 13. Muscular Dystrophy 1. Duchenne muscular dystrophy (DMD) Most common childhood dystrophy with incidence of 1: 3500 male live births. Abnormal or absent dystrophin that leads to necrosis , degeneration and regeneration. A positive family history (90%) Delayed motor milestones, late walkers, difficul ,Paraspinal weakness(kyphoscoliosis), respiratory weakness , degenerative changes in cardiac muscle causes conduction defects and cardiac failure.Also gastric hypomotility and also delayed gastric emptying, and a hypertrophied tongue.
- 14. Pre-operative Assessment ECG: RVS , tall R waves and inverted T waves . Echocardiogram : Ventricular Systolic dysfunction progress to DCM. Chest X-ray , Pulmonary function test (Decreased VC )and blood gases (hypoxemia and Carbon-dioxide retention) Elevated CK levels.
- 15. Anesthetic Considerations Suxamethonium is contraindicated (implicated in intra-operative cardiac arrests secondary to rhabdomyolysis and hyperkalemia). This anaesthetic-induced Rhabdomyolisis (AIR) is unrelated to malignant hyperthermi (Ensure a “ trigger-free anaesthetic” and “clean” anaesthesia machine). TIVA .
- 16. Anesthetic Considerations(contd.) Anticipate Difficult Airway. Minimise Cardiac and Respiratory Depression. Drugs should be short-acting and rapidly metabolised .Increase sensitivity to non- depolarising muscle relaxants. Close post-operative monitoring is needed, and ventilation is often indicated .
- 17. Becker’s Muscular dystrophy Second most common form of dystrophy, occurring in 1:30000 live male births . Dystrophin is abnormal, but still partly functional.The dystrophy is much milder with a slower onset. can develop severe cardiac manifestations. Symptoms start at around 11 years .
- 18. Anesthetic Considerations ECG/echocardiogram: Dilated cardiomyopathy often presents before skeletal muscle symptoms, and arrhythmias can also occur. CK level elevation will be less marked than DMD : 50 - 100 times. Respiratory: Optimise chest infections, and assess function, (deterioration may occur as a result of scoliosis, muscle weakness and aspiration pneumonia. Post-operative ventilatory assistance may be necessary.
- 19. Myotonias MYOTONIC DYSTROPHY (STEINER’S DISEASE) AND CONGENITAL MYOTONIC DYSTROPHY Gene mutations in various channels involved in skeletal muscle excitation-contraction coupling and sarcolemmal excitability. Normal dystrophin and stable sarcolemma No increased risk of developing MH .
- 20. Myotonias (contd.) Bulbar weakness leads to recurrent aspiration pneumonia.Involvement of the intercostal muscles and diaphragm lead to poor cough and chronic alveolar hypoventilation, necessitating postoperative ventilation. Swallowing and feeding difficulties due to severe dysphagia(nutritional status assessment and support necessary.
- 21. Anesthetic considerations : Sedatives pre-operatively can alleviate fear and anxiety in an aggressive child prone to myotonic episodes, but has the risk of serious respiratory depression. Temperomandibular joint contractures might limit mouthopening and make direct laryngoscopy difficult. Neither muscle relaxants nor regional anaesthesia prevent or reverse myotonic contractions .
- 22. Anesthetic considerations(contd.) Depolarising muscle relaxants and cholinesterase inhibitors exacerbate myotonia . Succinylcholine has resulted in fatal rhabdomyolysis with hyperkalaemia. Postoperative cardiac, respiratory and apnoeic complications can be dramatic. Prevent peri-operative hypothermia and pain to limit myotonia
- 23. Mitochondrial and Metabolic Myopathies Heterogeneous group of disorders is now the commonest cause of muscle weakness in children with an incidence of 1 in 4 000. Electron transport chain (ETC) function results in decreased ATP production, and an increased production of free radicals. The acidosis and excess free radicals further damage the mitochondria.
- 24. Mitochondrial and Metabolic Myopathies Mitochondrial DNA mutations include:- MELAS: mitochondrial encephalopathy, lactate acidosis MERRF: myoclonic epilepsy with red fibres syndrome. • The severest forms can present in the neonatal period with profound weakness, liver and renal failure, and substantial neurological impairment
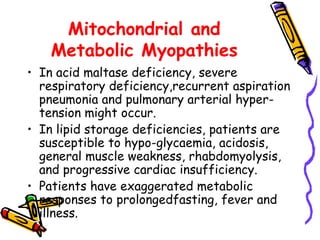
- 25. Mitochondrial and Metabolic Myopathies In acid maltase deficiency, severe respiratory deficiency,recurrent aspiration pneumonia and pulmonary arterial hyper-tension might occur. In lipid storage deficiencies, patients are susceptible to hypo-glycaemia, acidosis, general muscle weakness, rhabdomyolysis, and progressive cardiac insufficiency. Patients have exaggerated metabolic responses to prolongedfasting, fever and illness.
- 26. Mitochondrial and Metabolic Myopathies The patient is typically a floppy infant, a poor feeder with small stature, displays developmental delay, is hypotonic or hypoglycaemic, with or without positive family history. ECG and Echo might reveal cardiomyopathy or conduction deficits, and ventricular dilatation can compress the airway.
- 27. Anesthetic Considerations Evaluate pre-operative cardiac and respiratory status. Total AV block requires pacing . Evaluate metabolic status: glucose, lactate, liver enzymes and serum creatinine. Overnight fasting can cause hypoglycaemia, dehydration and mild metabolic acidosis. Maintain intravenous infusion containing glucose and electrolyte pre-operatively, avoid lactate-containing fluids.
- 28. Anesthetic Considerations(contd.) Increased sensitivity to sedatives, barbiturates, and propofol.Variable sensitivity to nondepolarising muscle relaxants. Avoid succinylcholine.
- 29. Anesthetic Considerations(contd.) Inhalation or total intravenous anaesthesia Propofol, which is a lipid carrierconsisting of long–chain fatty acids, may have an adverse effect on fatty acid oxidation and impair mitochondrial respiratory chainfunction, and therefore put patients with mitochondrial disorders and carnitine deficiency syndromes at risk for a clinical scenario similar to propofol infusion syndrome (PRIS).
- 30. Anesthetic Considerations Alternative intravenous anaesthetics that are under investigation include ketamine, etomidate, and dexmedetomidine. Many clinicians now consider sevoflurane as the agent of choice in these patients, how ever some respiratory chain disorders are more sensitive to inhaled agents and require lower MAC.
- 31. Anesthetic Considerations (contd.) Pain management is essential, as the response to pain may heighten the risk of lactic acidosis from depletion of energy stores and increased oxygen demand. Prevent hypothermia
- 32. Channelopathies Disturbance in the transfer of ions across the sarcolemma. 1. Familial periodic paralysis : A. Hyperkalemic Perodic Paralysis. B. Hypokalemic Periodic Paralysis. 2. Ligand Gated Calcium Channelopathy. Malignant Hyperthermia
- 33. Familial periodic paralysis Hyperkalaemic: Early onset, sometimes in infancy (autosomal dominant). Periodic paralysis is marked by brief episodes of flaccid weakness, which occur variably and resolve spontaneously. Respiratory and cranial muscles are typically spared. Genetic mutation that affects sodium channels causes sustained sodium currents which don’t allow the formation of action potentials during these brief attacks.
- 34. Familial periodic paralysis ECG signs of hyperkalemia, also ectopic beats or paroxysmal. Preo-perative management consists of potassium-free dextrose-containing solutions .Avoid cold, hyperkalaemia and carbohydrate depletion. Succinylcholine is contra-indicated.
- 35. Familial periodic paralysis Hypokalemic : Most common type, onset during dolescence ,Results from a mutation in a calcium channel. Attacks can be severe, resulting in respiratory compromise and cardiac disturbances . Triggers are strenuous exercise, high carbohydrate intake, lowserum potassium, mental stress, cold, trauma and infection. Maintain normal serum potassium, glucose and acid bases Status peri-operatively. .
- 36. Familial periodic paralysis .Adequate premedication needed to avoid stress. Maintain normothermia. .Avoid overeating the day before surgery. Avoid intravenous fluids with dextrose and sodium .
- 37. Ligand-gated calcium Channelopathy Malignant hyperthermia : Occult myopathy unmasked by triggers such as depolarising muscle relaxants and inhalation anaesthetics . Abnormalities in intracellular calcium homeostasis result in muscle rigidity, increased metabolism, rhabdomyolysis,hyperkalaemia, acidosis and cardiac arrest or death if untreated.
- 38. Ligand-gated calcium Channelopathy Multiple mutations in the ryanodine receptor (RYR1) . When exposed to “triggering” anaesthetic agents, this abnormal calcium release causes sustained muscle contraction and rhabdomyolysis .
- 39. Malignant hyperthermia Definite association with MH in CCD, King-Denboroughsyndrome and Evans myopathy. In vitro caffeine-halothane contracture tests are recommendedm to assess MH susceptibility, particular in cases with a strong family history. This test is 97 - 99% sensitive, but only 80 -90% specific.
- 40. MH” Triggering Agents Potent Volatile Anesthetic Agents: Halothane Isoflurane Sevoflurane Desflurane Succinylcholine
- 41. Signs of Malignant Hyperthermia Increased ETCO2 CO2 absorber may quickly turn purple(explain) Truncal or total body rigidity Masseter spasm or trismus Tachycardia/Tachypnea Acidosis Increased temperature
- 42. Signs of Malignant Hyperthermia …continued Sudden/Unexpected Cardiac arrest in young patients Trismus or masseter muscle spasm following uscle inhalation induction and succinylcholine is associated with an approximately 50% incidence of MH diagnosed by contracture testing. The classic signs of MH are tachycardia, rapid rise in end tidal carbon dioxide , muscle rigidity, fever, acidosis , elevated potassium, arrhythmias, myoglobinuria and elevated resting creatine kinase.
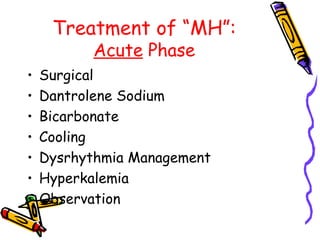
- 43. Treatment of “MH”: Acute Phase Surgical Dantrolene Sodium Bicarbonate Cooling Dysrhythmia Management Hyperkalemia Observation
- 44. Acute Phase Management : Halt surgery as quickly as is conveniently possible. Dantrolene Sodium 2.5 mg/kg rapidly IV through large-bore IV, if possible Dissolve the 20 mg in each vial with at least 60 ml sterile, preservative-free water for injection. Repeat until signs of MH are reversed. Sometimes more than 10 mg/kg (up to 30 mg/kg) is necessary.
- 45. Acute Phase Management: Bicarbonate 1-2 mEq/kg if blood gas values are not yet available. Lavage open body cavities, stomach, bladder, or rectum. Apply ice to skin surface. Infuse cold saline intravenously. Dysrhythmia Management: Usually respond to treatment of acidosis and hyperkalemia and or Use standard drug therapy .
- 46. Acute Phase Management: Hyperkalemia Management ; Hyperventilation, Bicarbonate, glucose/insulin, calcium. Bicarbonate 1-2 mEq/kg IV. 10 units regular insulin IV and 50 ml 50% glucose. Calcium chloride 10 mg/kg or calcium gluconate 10-50 mg/kg for life-threatening hyperkalemia. Check glucose levels hourly
- 47. Acute Phase Management Follow ETCO2, electrolytes, blood gases, CK, core temperature, urine output and color, coagulation studies. Venous blood gas (e.g., femoral vein) values may document hypermetabolism better than arterial values. Central venous or PA monitoring as needed and record minute ventilation. Place Foley catheter and monitor urine output.
- 48. Treatment of “MH”: Post Acute Phase Observe patient in ICU for at least 24 hours. Dantrolene 1mg/kg q 4-6hrs or 0.25 mg/kg/hr gtt for at least 24 hours. labs and VS as during acute phase management urine myoglobin Counsel patient and family regarding MH and further precautions
- 49. conclusion When the specific diagnosis is known, it would be appropriate to choose a TIVA technique for the child with muscular dystrophy, and an inhaled agent for the child with mitochondrial myopathy. The risk of rhabdomyolysis or malignant hyperthermia when using inhalational anaesthesia is 1,09%and a total intravenous technique may be used in all children with undiagnosed myopathy
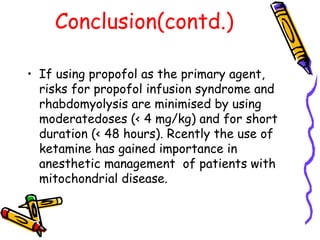
- 50. Conclusion(contd.) If using propofol as the primary agent, risks for propofol infusion syndrome and rhabdomyolysis are minimised by using moderatedoses (< 4 mg/kg) and for short duration (< 48 hours). Rcently the use of ketamine has gained importance in anesthetic management of patients with mitochondrial disease.
- 51. QUESTIONS and COMMENTS