Antiemetics and prokinetics classification with mechansim
- 1. ANTIEMETICS and PROKINETICS Prepared by : SONAL VIJAY PANDE M.Pharm Department : Pharmacology
- 2. NAUSEA : Non observable subjective feeling of having an urge to vomit. EMESIS : ACUTE EMESIS: occurs within mins. And resolves within 24 hrs. DELAYED EMESIS: occurs after 2-3 days BREAKTHROUGH EMESIS: emesis occurring after the prophylactic antiemetic treatment.
- 3. Nausea and vomiting may be manifestations of many conditions and may occur due to stimulation of vomiting center that respond to inputs from: •Chemoreceptor trigger zone (CTZ) stimulation •Disturbance of vestibular system •Higher cortical centers stimulation (CNS) •The periphery (Pharynx, GIT)via sensory nerves
- 4. 1. Chemoreceptor trigger zone (CTZ) stimulation: • The fourth ventricle of the brain hosts the vomiting centre called the chemoreceptor trigger zone (CTZ). • It is also called the area postrema. When the CTZ is stimulated, vomiting may occur. • CTZ is physiologically outside BBB. • CTZ Contains opioid receptors, D2 receptors & 5 HT3 receptors, Substance P stimulated by: Drugs (opioids, general anesthetics), Chemicals and toxins in blood, CSF. Radiation.
- 5. 2.Disturbance of vestibular system • GIT irritation, myocardial infarction, renal or biliary stones. 3. Disturbance of vestibular system • By motion sickness 4. Higher cortical centers stimulation: • Emotional factors, nauseating smells or sights.
- 6. CHEMICAL TRANSMITTER AND RECEPTOR INVOVLED IN VOMMITNG : • Ach (Muscarinic receptors) • Dopamine (D2) • Histamine (Histaminergic receptors H1) • Serotonin (5 -HT3) • Substance P (Neurokinin receptors, NK1) • Opioid (Opioid receptors)
- 7. ETIOLOGY
- 10. CLASSIFICATION RECEPTOR ANTAGONISTS • Anticholinergics : Hyoscine, Dicyclomine • H1 antihistaminics : Promethazine , Diphenhydramine, Dimenhydrinate, Doxylamine, Meclozine (Meclizine), Cinnarizine • Neuroleptics(D2 blockers) : Chlorpromazine, Triflupromazine, Prochlorperazine, Haloperidol, etc. • 5-HT3 antagonists : Ondansetron, Granisetron, Palonosetron, Ramosetron • NK1 receptor antagonists : Aprepitant, Fosaprepitant Prokinetics : Metoclopramide, Domperidone ADJUVANT ANTIEMETICS : Dexamethasone, Benzodiazepines, Dronabinol, Nabilone
- 11. RECEPTOR ANTAGONIST 1) H1 RECEPTOR ANTAGONISTS • Cinnarizine, cyclizine and promethazine: They are effective against nausea and vomiting arising from many causes, including motion sickness and the presence of irritants in the stomach. None is very effective against substances that act directly on the CTZ
- 12. CYCLAZINE: Dose 50mg/ml injection 50mg tablet
- 13. • Promethazine It is used for morning sickness of pregnancy (on the rare occasions when this is so severe that drug treatment is justified), and has been used by NASA to treat space motion sickness. chief unwanted effects : Drowsiness and sedation DOSE:6.25mg/5ml
- 14. • Betahistine: It has complicated effects on histamine action, antagonising H3 receptors but having a weak agonist activity on H1 receptors. It is used to control the nausea and vertigo associated with Menière’s disease Dose: 16mg/tab
- 15. 2) MUSCARINIC RECEPTOR ANTAGONISTS • Hyoscine (scopolamine) It is employed principally for prophylaxis and treatment of motion sickness, and may be administered orally or as a transdermal patch. most common unwanted effects : Dry mouth and blurred vision, Drowsiness also occurs, The drug has less sedative action than the antihistamines because of poor central nervous system penetration.
- 16. Dose: 0.4-0.6 mg p.o 30min before journey.
- 17. 3) 5-HT3 RECEPTOR ANTAGONISTS Granisetron, ondansetron and palonosetron These are of particular value in preventing and treating the vomiting and, to a lesser extent the nausea, commonly encountered postoperatively as well as that caused by radiation therapy or administration of cytotoxic drugs such as cisplatin. The primary site of action of these drugs is the CTZ.
- 18. They may be given orally or by injection (sometimes helpful if nausea is already present). Unwanted effects : such as headache and gastrointestinal upsets are relatively uncommon. Ondansetron dose: 4mg each ampule. 4-8mg tablet, 4mg/5ml oral solution Granisetron dose: 1mg IV
- 19. 4) DOPAMINE ANTAGONISTS Antipsychotic phenothiazines, such as chlorpromazine, perphenazine, prochlorperazine and trifluoperazine commonly used for treating the more severe nausea and vomiting associated with cancer, radiation therapy, cytotoxic drugs, opioids, anaesthetics and other drugs. administered orally, intravenously or by suppository. act mainly as antagonists of the dopamine D2 receptors in the CTZ but they also block histamine and muscarinic receptors. Common
- 20. Unwanted effects : sedation (especially chlorpromazine), hypotension and extrapyramidal symptoms including dystonias and tardive dyskinesia. Other antipsychotic drugs, such as haloperidol, the related compound droperidol and levomepromazine also act as D2 antagonists in the CTZ and can be used for acute chemotherapy-induced emesis Chlorpromazine dose: p.o.:10-25mg 4-6hrs IV/IM:25-50 mg 4-6hrs
- 21. 5) NK1 RECEPTOR ANTAGONISTS Substance P causes vomiting when injected intravenously and is released by gastrointestinal vagal afferent nerves as well as in the vomiting centre itself. Aprepitant: It blocks substance P (NK1) receptors in the CTZ and vomiting centre. given orally, and is effective in controlling the late phase of emesis caused by cytotoxic drugs, with few significant unwanted effects. Fosaprepitant It is a prodrug of aprepitant, which is administered intravenously.
- 23. ADJUVANT ANTIEMETICS The synthetic cannabinol (nabilone) : found to decrease vomiting caused by agents that stimulate the CTZ, and is sometimes effective where other drugs have failed. The antiemetic effect is antagonised by naloxone, which implies that opioid receptors may be important in the mechanism of action. Given orally; it is well absorbed from the gastrointestinal tract and is metabolised in many tissues. Plasma half-life -120 min, metabolites are excreted in the urine and faeces.
- 24. Unwanted effects are common : especially drowsiness, dizziness and dry mouth. Mood changes and postural hypotension are also fairly frequent. Some patients experience hallucinations and psychotic reactions, resembling the effect of other cannabinoids .
- 25. High-dose glucocorticoids (dexamethasone): can also control emesis, especially when this is caused by cytotoxic drugs. The mechanism of action is not clear. Dexamethasone can be used alone but is frequently deployed in combination with a phenothiazine, ondansetron or aprepitant. MAIN SIDE EFFECTS: drowsiness and antiparasympathetic effects (hyoscine, nabilone > cinnarizine) dystonic reactions (metoclopramide) general CNS disturbances (nabilone) headache, gastrointestinal tract upsets (ondansetron).
- 26. CONDITION DRUGS Motion sickness Hyoscine , cyclizine , Promethazine , Cinnarizine Vomiting due to cytotoxic drugs Ondansetron + Dexamethsone + aprepitant 2. Metoclopramide + dexamethasone + diphenhydramine + lorazepam Vomiting due to other drugs Chlorpromazine , Metoclopramide Postoperative vomiting Ondansetron , Metoclopramide Vomiting in Pregnancy Doxylamine , Dicyclomine , pyridoxine , cyclizine , meclizine , Metoclopramide
- 27. CLINICAL USE OF ANTIEMETIC DRUGS Histamine H1 receptor antagonists :- • cyclizine: motion sickness • cinnarizine: motion sickness, vestibular disorders (e.g. Menière’s disease) • promethazine: severe morning sickness of pregnancy. Muscarinic receptor antagonists: – • hyoscine: motion sickness.
- 28. Dopamine D2 receptor antagonists: – • phenothiazines (e.g. prochlorperazine): vomiting caused by uraemia, radiation, viral gastroenteritis, severe morning sickness of pregnancy • metoclopramide: vomiting caused by uraemia, radiation, gastrointestinal disorders, cytotoxic drugs • domperidone is less liable to cause CNS side effects as it penetrates the blood– brain barrier poorly. 5-Hydroxytryptamine 5-HT3 receptor antagonists (e.g. ondansetron): cytotoxic drugs or radiation, postoperative vomiting. • Cannabinoids (e.g. nabilone): - cytotoxic drugs
- 30. PROKINETICS
- 31. PROKINETICS • These are drugs which promote gastrointestinal transit and speed gastric emptying by enhancing coordinated propulsive motility. • This excludes traditional cholinomimetics and anti-ChEs which produce tonic and largely uncoordinated contraction. • Prokinetic drugs increase the movement of ingested material through the GI tract • PROKINETICS DRUGS : Metoclopramide, Domperidone, Cisapride, Mosapride, Itopride
- 32. Metoclopramide • Metoclopramide is a D2 receptor antagonist, closely related to the phenothiazine group, that acts centrally on the CTZ and also has a peripheral action on the gastrointestinal tract itself, increasing the motility of the oesophagus, stomach and intestine. • This not only adds to the antiemetic effect, but explains its use in the treatment of gastro-oesophageal reflux and hepatic and biliary disorders.
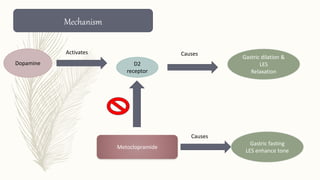
- 33. Dopamine D2 receptor Gastric dilation & LES Relaxation Metoclopramide Gastric fasting LES enhance tone Mechanism Activates Causes Causes
- 34. Metoclopramide Activates 5HT4 RECEPTOR At prejunctional ACh release Promotes Contractile activity (increase gastric motility ) Response 5HT4 agonism
- 35. • As metoclopramide also blocks dopamine receptors elsewhere in the central nervous system, it produces a number of unwanted effects : disorders of movement (more common in children and young adults), fatigue, motor restlessness, spasmodic torticollis (involuntary twisting of the neck) and occulogyric crises (involuntary upward eye movements). • It stimulates prolactin release, causing galactorrhoea and disorders of menstruation. • Dose :5-10 mg Injection 10mg tablet
- 36. ACTIONS: 1)GIT: Metoclopramide has more prominent effect on upper G.I.T. • increases gastric peristalsis • relaxing the pylorus and the first part of duodenu • speeds gastric emptying, especially if it was slow. 2) CNS : Metoclopramide is an effective antiemetic; acting on the CTZ, blocks apomorphine induced vomiting. The gastrokinetic action may contribute to the antiemetic effect.
- 37. Pharmacokinetics : Rapidly absorbed orally, enters brain, crosses placenta and is secreted in milk. • It is partly conjugated in liver and excreted in urine within 24 hours; • t½ is 3– 6 hours. • Orally it acts in ½–1 hr, but within 10 min after i.m. and 2 min after i.v. injection. Action lasts for 4–6 hours.
- 38. Interactions : • It hastens the absorption of many drugs, e.g. aspirin, diazepam, etc. by facilitating gastric emptying. • Bioavailability of cimetidine is also reduced. • By blocking DA receptors in basal ganglia, it abolishes the therapeutic effect of levodopa. • Adverse effects • Sedation, dizziness, loose stools, • Long-term use can cause parkinsonism, but it should not be used to augment lactation. • No harmful effects are known when used during pregnancy. • Though the amount secreted in milk is small, but suckling infant may develop loose motions, dystonia, myoclonus.
- 39. Uses : Antiemetic: an effective and popular drug for many types of vomiting— postoperative, drug induced, disease associated (especially migraine), radiation sickness, etc, but is less effective in motion sickness Gastrokinetic: To accelerate gastric emptying Dyspepsia and other functional G.I. disorders Gastroesophageal reflux disease (GERD)
- 40. Domperidone : • It is a similar drug often used to treat vomiting due to cytotoxic therapy as well as gastrointestinal symptoms. • does not readily penetrate the blood–brain barrier less prone to producing central side effects. • Pharmacokinetics : • Domperidone: absorbed- orally • bioavailability is only ~15% • biotransformed and metabolites - excreted in urine. • Plasma t½ is 7.5 hr. • Dose: 10mg,30mg tablets • 1mg/ml syrup.
- 41. Cisapride : This benzamide derivative is a prokinetic with little antiemetic property, because it lacks D2 receptor antagonism. Dose:10mg tablet
- 42. Itopride: Another substituted benzamide as a prokinetic drug. It has D2 antidopaminergic and anti-ChE (ACh potentiating) activity, but very low affinity for 5-HT4 receptor. Thus, the basis of prokinetic action may be different from that of cisapride and mosapride. Dose:50mg tablet
- 43. Mosapride : A subsequently introduced congener of cisapride with similar gastrokinetic and LES tonic action due to 5-HT4 agonistic (major) and 5-HT3 antagonistic (minor) action in the myenteric plexus. Dose: 5mg tablet
- 44. References Tripathi KD. Essentials of medical pharmacology. JP Medical Ltd; 2013 Sep 30.chp:47 .pg 661.
- 45. Thank you