Approach to lymphadenitis pmm
- 1. A p p r o a c h t o G ra n u l o m a t o u s Ly m p h A d e n i t i s ( G L A ) PA R T H I V M E H TA A H M E D A B A D
- 4. Granulomatous Lymph Adenitis (GLA) • Granulomatous Lymph Adenitis is a reactive phenomenon of lymph nodes that displays a distinctive pattern of chronic inflammation and histiocytes. • It is caused by a heterogeneous collection of diseases, including reactive, infectious and malignant etiologies. GLA – Parthiv Mehta 20180805 MEHSANA
- 5. Granulomatous Lymph Adenitis (GLA) •Histologically, granulomatous lymphadenitis (i.e. granulomas) be divided into 3 distinct –Based on the type of inflammation present (acute v/s chronic), and –whether or not necrosis accompanies the inflammation GLA – Parthiv Mehta 20180805 MEHSANA
- 6. Granulomatous Lymph Adenitis (GLA) GLA – Parthiv Mehta 20180805 MEHSANA
- 7. Approach
- 8. Approach GLA – Parthiv Mehta 20180805 MEHSANA
- 9. Granulomatous Lymph Adenitis (GLA) GLA – Parthiv Mehta 20180805 MEHSANA
- 10. Granulomatous Lymph Adenitis (GLA) • The common causes of GLA are • (A) Infective agents like mycobacteria, fungi, parasites, etc. and • (B) Non-infective etiologies like Sarcoidosis, Foreign bodies, Wegener’s granulomatosis, Crohn’s disease, etc. In addition, • (C) Certain neoplasms are also known to be associated with a granulomatous response in the parenchyma e.g. Hodgkin’s disease • Approach to Differential diagnosis and management demand a skillful interpretation of clinical findings and histology. GLA – Parthiv Mehta 20180805 MEHSANA
- 11. Approach GLA – Parthiv Mehta 20180805 MEHSANA
- 12. GLA - Etiology • Acute v/s Chronic • Caseating v/s Non-caseating • Infective v/s Non-infective • Neoplastic v/s Non-neoplastic
- 13. Granulomatous Lymph Adenitis (GLA) Noninfectious GLA 1) Sarcoidosis lymphadenitis 2) Sarcoid-like lymphadenitis 3)Berylliosis Infectious GLA A. Suppurative 1) Tularemia lymphadenitis 2) Cat scratch lymphadenitis 3) Yersinia lymphadenitis 4) Lymphogranuloma venereum 5) Fungal infection B. Non-suppurative 1) Tuberculous Lymphadenitis 2) Atypical Mycobacterial infection 3) BCG-Lymphadenitis 4) Toxoplasma Lymphadenitis 5) Leprosy 6) Syphilis 7) Brucellosis 8) Fungal infection (Cryptococcus, Histoplasma, Coccidioidomycosis, Pneumocystis) GLA – Parthiv Mehta 20180805 MEHSANA
- 14. Approach GLA – Parthiv Mehta 20180805 MEHSANA
- 15. Approach 01 HISTORY & CLINICAL EXAMIATION E X T R E M E LY I M P O R TA N T, A N D C A N , I N FA C T, O F F E R C R I T I C A L D I A G N O S T I C C L U E S
- 16. History and Clinical Examination • Factors that can assist in identifying the etiology of lymphadenopathy include – Age of patient, – Duration of lymphadenopathy, – Exposures, – Associated symptoms, and – Location (localized vs. generalized). – Time course of enlargement, – Tenderness to palpation, – Recent infections, recent immunizations, and medications. GLA – Parthiv Mehta 20180805 MEHSANA
- 17. History and Clinical Examination • History of exposure to infection or infectious agents is a particularly helpful clue. • History of animal exposure helps to suspect. • Has the patient travelled and possibly been exposed to area specific infectious agents? • Mycoses (fungal infections) are endemic in many parts of the world, Koch’s is most likely in family contacts. GLA – Parthiv Mehta 20180805 MEHSANA
- 18. History and Clinical Examination • Some granulomatous diseases have a particular predilection for affecting certain body sites. Eosinophilic Granuloma –––– Bone Wegener’s Granulomatosis –– Face Giant Cell Granuloma –––––– Oral Cavity Granuloma Annulare ––––––– Skin Various Infectious Agents –––– CNS GLA – Parthiv Mehta 20180805 MEHSANA
- 19. Clue - 1 : Site of Lymph nodes GLA – Parthiv Mehta 20180805 MEHSANA
- 20. Clue - 1 : Site of Lymph nodes GLA – Parthiv Mehta 20180805 MEHSANA
- 21. Clue - 1 : Site of Lymph nodes GLA – Parthiv Mehta 20180805 MEHSANA
- 22. Clue - 1 : Site of Lymph nodes GLA – Parthiv Mehta 20180805 MEHSANA
- 23. Clue - 2: Character and size of Lymph nodes •Warmth, overlying erythema, tenderness, mobility, fluctuance and consistency. •A painless, hard, irregular mass or a firm, rubbery lesion that is immobile or fixed may represent a malignancy, although in general, qualitative characteristics are unable to reliably predict malignancy. •Shotty lymphadenopathy is the presence of multiple small lymph nodes that feel like “buck shots” under the skin. This usually implies reactive lymphadenopathy from viral infection. •Painful or tender lymphadenopathy is nonspecific and may represent possible inflammation caused by infection, but it can also be the result of hemorrhage
- 24. Approach 01 History & Clinical Examination • Q.1 – Is that a Lymph node? –Enlarged parotid –Thyroglossal cyst –Abscess –Branchial cyst GLA – Parthiv Mehta 20180805 MEHSANA
- 25. Approach 01 History & Clinical Examination • Q. 2 Is it Acute of Chronic? • Q.3 Localized or generalized?? • Q.4 Are there associated systemic / localizing symptoms / signs??? • Q.5 What is the character? –Tender / nontender –Mobile & Separate / Fixed & matted –Firm & rubbery / Painless & stone hard GLA – Parthiv Mehta 20180805 MEHSANA
- 26. Approach 01 History & Clinical Examination • Q.6. Are there usual epidemiological clues? –Exposure to TB –Sexual exposure –Travel –Exposure to bird droppings –Exposure to cats GLA – Parthiv Mehta 20180805 MEHSANA
- 27. Approach 02 INVESTIGATIONS J U D I C I O U S U S E C A N A D D T O C O N F I D E N C E , C O S T E F F E C T I V E N E S S A N D L E A D T O P R O G N O S T I C A T I O N
- 28. Investigation - Approach • If history and physical examination findings suggest a benign or self-limited process, reassurance can be provided and follow-up arranged if lymphadenopathy persists. • Findings suggestive of infectious or autoimmune etiologies may require specific testing and treatment as indicated. • If malignancy is considered unlikely based on history and physical examination, localized lymphadenopathy can be observed for four weeks. • Generalized lymphadenopathy should prompt routine laboratory testing and testing for
- 29. Laboratory Diagnosis • Usually, routine laboratory tests are nondiagnostic; cultures of blood, skin lesions or lymph nodes are frequently negative. • If there is suspicion of an infectious agent, there are specific serologic studies that can confirm the diagnosis. • Polymerase chain reaction (PCR) and antibody titre also are very helpful. • Direct and indirect fluorescence antibody tests are also available and have good sensitivities. • FNAC and/or Biopsy are a must to establish cause GLA – Parthiv Mehta 20180805 MEHSANA
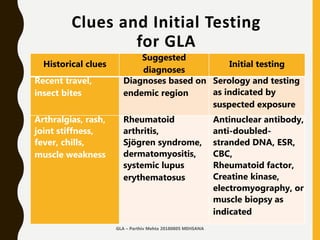
- 30. Clues and Initial Testing for GLA Historical clues Suggested diagnoses Initial testing Fever, night sweats, weight loss, Node located in supraclavicular, popliteal, or iliac region, Bruising, Splenomegaly Leukemia, Lymphoma, Solid tumor Metastasis CBC, ESR Imaging - USG or CT may be considered Biopsy- Nodal or Bone Marrow Fever, chills, malaise, sore throat, nausea, vomiting, diarrhea; No other red flag symptoms Bacterial or viral pharyngitis, Hepatitis, Influenza, Mononucleosis, Tuberculosis (if exposed), Rubella Limited illnesses may not require any additional testing; (depending on clinical assessment, consider CBC, LFT, cultures, and disease- specific serologies as needed)
- 31. Clues and Initial Testing for GLA Historical clues Suggested diagnoses Initial testing High-risk sexual behavior Chancroid, HIV infection, Lympho-granuloma Venereum, Syphilis HIV-1/HIV-2 immunoassay, Culture of lesions, Nucleic acid amplification for chlamydia, Migration inhibitory factor Test GLA – Parthiv Mehta 20180805 MEHSANA
- 32. Clues and Initial Testing for GLA Historical clues Suggested diagnoses Initial testing Animal or food contact Cats Cat-scratch disease (Bartonella) Serology and PCR Toxoplasmosis Serology Rabbits, or sheep or cattle wool, hair, or hides Anthrax Per CDC guidelines Brucellosis Serology and PCR Tularemia Blood culture and serology Undercooked meat Anthrax Per CDC guidelines Brucellosis Serology and PCR Toxoplasmosis Serology
- 33. Clues and Initial Testing for GLA Historical clues Suggested diagnoses Initial testing Recent travel, insect bites Diagnoses based on endemic region Serology and testing as indicated by suspected exposure Arthralgias, rash, joint stiffness, fever, chills, muscle weakness Rheumatoid arthritis, Sjögren syndrome, dermatomyositis, systemic lupus erythematosus Antinuclear antibody, anti-doubled- stranded DNA, ESR, CBC, Rheumatoid factor, Creatine kinase, electromyography, or muscle biopsy as indicated GLA – Parthiv Mehta 20180805 MEHSANA
- 34. Histopathological Diagnosis • Direct approach –Needle –True cut – Core Needle Biopsy –Excision GLA – Parthiv Mehta 20180805 MEHSANA
- 35. FNAC in Diagnosis of GLA • Easy to perform • Trained Physician / Pathologist / Radiologist can do it • Diagnostic yield approximately 60% –More so in Lymphoma / Malignancy –Cervical lymph nodes Fine needle aspiration cytology (FNAC) in the diagnosis of granulomatous lymphadenitis UMJ. 2006 Jan; 75(1): 59–64 Evaluation of fine needle aspiration cytology of lymph nodes in KMC, Teaching hospital. KUMJ. 2009 Apr-Jun;7(26):139-42. GLA – Parthiv Mehta 20180805 MEHSANA
- 36. FNAC in Diagnosis of GLA Choice of node • Largest node • Avoid inguinal & axillary • Supra clavicular-highest diagnostic yield • Complications GLA – Parthiv Mehta 20180805 MEHSANA
- 37. Excision Biopsy in Diagnosis of GLA • Incisional –External approach • Laparoscopic –Thoracoscopic –Mediastinoscopic –Laparoscopic Larger tissue.. All possible investigations GLA – Parthiv Mehta 20180805 MEHSANA
- 38. Histological Diagnosis of GLA • The histologic identification of granulomatous inflammation is a helpful predictor of diagnostic etiology. • Histologic patterns (foreign-body, necrotizing, non-necrotizing, suppurative, and a diffuse histiocytic reaction) can narrow the clinical differential diagnosis. • A definitive diagnosis can often be made with the aid of ancillary testing (special stains and or molecular diagnostics). • An open clinical dialogue between the clinician and the pathologist allows for appropriate use of ancillary laboratory techniques and ultimately accurate and effective patient care.GLA – Parthiv Mehta 20180805 MEHSANA
- 39. Histological Diagnosis of GLA • 23% of diagnoses could not identify the specific etiology via H&E stain at the time of biopsy. • Etiology identification improved to 90.8% with clinical features, radiographic findings, and improved laboratory methodologies, including molecular techniques, culture, IHC profiles, and serologic values. S. Mukhopadhyay, et al. Pulmonary necrotizing granulomas of unknown cause: Chest, 144 (3) (2013), pp. 813-824 GLA – Parthiv Mehta 20180805 MEHSANA
- 40. Radiodiagnosis • USG - Surface –Must –Defines structure –Helps identify site –Precision GLA – Parthiv Mehta 20180805 MEHSANA
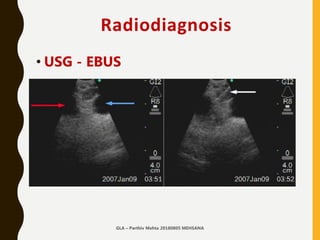
- 41. Radiodiagnosis • USG - EBUS –Must –Defines structure –Helps identify site –Precision GLA – Parthiv Mehta 20180805 MEHSANA
- 42. Radiodiagnosis • X-ray Chest –Hilar Adenopathy –Progress / Resolution –Thoracic structures –Associated Pulmonary Infiltrates –Associated Pleural Pathology GLA – Parthiv Mehta 20180805 MEHSANA
- 43. Radiodiagnosis CT Scan • Lymph nodes • Probable structure • Vascularity • Associated thoracic pathology • Likely approach • Likely diagnosis clue - PET CT GLA – Parthiv Mehta 20180805 MEHSANA
- 44. Approach 02 Investigations 1.CBC with differential…. –Atypical lymphocytosis –Eosinophilia –Pancytopenia 2. Biochemistry –Serum Uric Acid –Serum Kidney, Liver functions GLA – Parthiv Mehta 20180805 MEHSANA
- 45. Approach 02 Investigations Localized Adenopathy 1. Throat culture 2. Urethral/cervical swabs 3. Blood culture 4. USG / CT Scan 5. Biopsy 6. Bone Marrow biopsy GLA – Parthiv Mehta 20180805 MEHSANA
- 46. Approach 02 Investigations Generalised Adenopathy 1. Heterophile test (For IM due to EBV) 2. VDRL 3. Antibody titer of viruses, fungi, toxoplasmosis 4. Anti nuclear antibodies 5. Rheumatoid factor GLA – Parthiv Mehta 20180805 MEHSANA
- 47. Approach 02 Investigations Hilar Adenopathy 1.Mantoux test 2.Chest X-RAY, CT 3.ACE determination 4.Bronchoscopy - EBUS 5.Mediastinoscopy GLA – Parthiv Mehta 20180805 MEHSANA
- 48. Approach 03 DECISION MAKING and GUIDANCE W E L L I N F O R M E D P H Y S I C I A N I S T H E B E S T P E R S O N T O H E L P
- 49. Decision Making
- 50. Decision Making GLA – Parthiv Mehta 20180805 MEHSANA
- 51. Decision Making - 01
- 52. Decision Making - 02
- 53. Decision Making - 03
- 54. Guidance - Initial Management • Patients worry about the cause of their abnormal lymph nodes. • To adequately address their fears, the physician should ask the patient about his or her concerns and respond to questions about specific diagnoses. • When biopsy is deferred, the physician should explain to the patient the rationale for waiting. • Patients should be cautioned to remain alert for the reappearance of the nodes because lymphomatous nodes have been known to temporarily regress. GLA – Parthiv Mehta 20180805 MEHSANA
- 55. Approach Final Comment L E T U S M A K E L I F E S I M P L E
- 56. Tb or no TB?
- 57. Tb or no TB? GLA – Parthiv Mehta 20180805 MEHSANA
- 58. Tb or no TB? • In countries with high incidence of TB, TB is considered firstly in differential diagnosis of granulomatous diseases. • Detailed analysis and physical examinations should be done in differential diagnosis of granulomatous diseases, and TB must be excluded. GLA – Parthiv Mehta 20180805 MEHSANA
- 59. Tb or not TB? • Organisms are easily detectable by proper staining, immuno-histochemical and molecular biological methods such as PCR • Accurate pathological and microbiological diagnosis can lead to precise treatment. MDR / XDR TB must be excluded.GLA – Parthiv Mehta 20180805 MEHSANA
- 60. Let us make it simple.. Clinical Recommendation Evidence rating USG should be used as the initial imaging modality for children up to 14 years presenting with a neck mass with or without fever. C CT Scan should be used as the initial imaging modality for children older than 14 years and adults presenting with solitary or multiple neck masses. C Corticosteroids should be avoided until a definitive diagnosis of lymphadenopathy is made because they could potentially mask or delay histologic diagnosis of leukemia or lymphoma. C FNAC may be used to differentiate malignant from reactive lymphadenopathy. C AJFP. 2016 Dec 1;94(11):896-903.GLA – Parthiv Mehta 20180805 MEHSANA
- 61. Let us make it simple… • In most patients, lymphadenopathy has a readily diagnosable infectious cause. • A diagnosis of less obvious causes can often be made after considering the patient's age, the duration of the lymphadenopathy and whether localizing signs or symptoms, constitutional signs or epidemiologic clues are present. • When the cause of the lymphadenopathy remains unexplained, a three- to four-week observation period is appropriate when the clinical setting indicates a high probability of benign disease.GLA – Parthiv Mehta 20180805 MEHSANA
- 62. Let us make it simple… GLA
- 63. Arise, Awake.. Stop Not Till the Goal is Reached..