Awake intubation
- 1. AWAKE INTUBATION PREPARATION AND BLOCKS ZIKRULLAH
- 2. BACKGROUND • First awake intubation was performed by Dr. Macewend in 1880 without topical or regional blocks , sedatives, analgesics.
- 3. When do we need Awake Intubation?? • History of the patient and Airway assessment is suggestive of a -Difficult mask ventilation. -Difficult conventional Laryngoscopy and Intubation. • In such circumstances, awake intubation becomes the most prudent and secure option to maintain the patency of Airway. 3
- 4. DIFFICULT AIRWAY GENERAL ANESTHESIA +/- PARALYSIS RECOGNIZED PROPER PREPARATION ASA DIFFICULT AIRWAY ALGORITHM UNRECOGNIZED AWAKE INTUBATION CHOICES SUCCEED FAIL SURGICAL AIRWAY MASK VENTILATION NO YES EMERGENCY PATHWAY NON -EMERGENCY PATHWAY LMA COMBITUBE TTJV INTUBATION CHOICES INTUBATION CHOICES SURGICAL AIRWAY SUCCEED FAIL CONFIRM ANESTHESIA WITH MASK VENTILATION AWAKEN SURGICAL AIRWAY EXTUBATE OVER JET STYLET REGIONAL ANESTHESIA CANCEL CASE REGROUP Intubation choices include use of different laryngoscope blades, LMA as an intubation conduit (with or without fiberoptic guidance), fiberoptic intubation, intubating stylet or tube changer, light wand, retrograde intubation, and blind oral or nasal intubation. * * * AWAKEN DIFFICULT AIRWAY GENERAL ANESTHESIA +/- PARALYSIS RECOGNIZED PROPER PREPARATION ASA DIFFICULT AIRWAY ALGORITHM UNRECOGNIZED AWAKE INTUBATION CHOICES SUCCEED FAIL SURGICAL AIRWAY MASK VENTILATION NO YES EMERGENCY PATHWAY NON -EMERGENCY PATHWAY LMA COMBITUBE TTJV INTUBATION CHOICES INTUBATION CHOICES SURGICAL AIRWAY SUCCEED FAIL CONFIRM ANESTHESIA WITH MASK VENTILATION AWAKEN SURGICAL AIRWAY EXTUBATE OVER JET STYLET REGIONAL ANESTHESIA CANCEL CASE REGROUP Intubation choices include use of different laryngoscope blades, LMA as an intubation conduit (with or without fiberoptic guidance), fiberoptic intubation, intubating stylet or tube changer, light wand, retrograde intubation, and blind oral or nasal intubation. * * * AWAKEN
- 5. WHY AWAKE INTUBATION IN Pt. WITH DA ??? 1. The natural airway is preserved 2. Spontaneous breathing is maintained 3. A patient who is awake and well topicalized is easier to intubate 4. The patient can still protect his or her airway from aspiration. 5. Patients are able to monitor their own neurologic symptoms (for example, the patient with potential cervical pathology).
- 6. INDICATIONS FOR AWAKE INTUBATION 1. Previous history of difficult intubation. 2. Anticipated difficult airway (assessed on physical examination) . 3. Trauma to the following: Face Upper airway Cervical spine 4. Anticipated difficult mask ventilation 5. Severe risk of aspiration 6. Respiratory failure 7. Severe hemodynamic instability 6
- 7. Elements of Awake Intubation(AI) Element Underlying Concept or Action Explanation Patients understand Safety Desiccation Dry the Airway Dilatation Prepare the Nose Tropicalization Obtund Reflexes Sedation Maintain the patient’s airway control Procrastination AI Cannot and Should not be RUSHED
- 8. THE PREOPERATIVE VISIT A. REVIEWING OLD CHARTS Focus on four important features: • Degree of difficulty of the endotracheal intubation • Positioning of the patient during laryngoscopy • Equipment used • Whether the technique that was used previously is familiar
- 9. B. PREPARATION OF THE PATIENT • A detailed explanation of the technique is provided, and questions are answered. • Reason should be explained to the patient, emphasizing that this is done for the patient's safety. • The patient is informed of what he or she can do to assist in a smooth intubation.
- 10. PREMEDICATION • Alleviate anxiety • Provide a clear and dry airway • Protect against the risk of aspiration • Enable adequate topicalization of the airway
- 11. A. SEDATIVES/HYPNOTICS • 1. BENZODIAZEPINES • Excellent anxiolytics, amnestics, sedatives, and hypnotics. • MIDAZOLAM • Dosages : 0.07 -0.15 mg/kg i.m. • 0.01 – 0.1 mg/kg i.v. • decrease the dose (∼30%) if narcotics or other central nervous system depressants are administered concomitantly.
- 12. • 2. OPIOIDS • Sedatives • Antitussive properties depress laryngeal reflexes further • Alter the respiratory pattern to a slower and deeper rhythm. • FENTANYL: 1 to 2 μg/kg i.v. • onset in about 2 to 3 minutes • Transmucosally, the onset of effect is 5 to 15 minutes, with peak analgesia within 20 to 30 minutes • SUFENTANIL: 1 μg/kg i.v. onset in 1 to 3 minutes
- 13. • 3. INTRAVENOUS HYPNOTICS • DEXMEDETOMIDINE: • Highly specific α2-adrenoreceptor agonist • Sedative, analgesic, without a change in ventilatory status • Dose :1 μg/kg IV over 10 minutes • :infusion of 0.2 to 0.7 μg/kg/hr • PROPOFOL • Sedating dosage : 0.25 mg/kg IV • Excellent sedative with a smooth plane achieved • Good acceptance by patients • Amnesia, adequate anxiolysis, and beneficial antiemetic properties.
- 14. B. ASPIRATION PROPHYLAXIS • patients with full stomach (e.g., trauma victims) or be obese with DA • H2-RECEPTOR ANTAGONISTS • Cimetidine and Ranitidine • Selective and competitive antagonists that block secretion ofH+ • Ranitidine : 0.25-1.0 mg/kg i.v • Cimetidine : 5-10 mg /kg PO • METOCLOPRAMIDE • Dopamine antagonist • Doses are 0.15 to 0.3 mg/kg IV. • For complete aspiration prophylaxis, a combination of nonparticulate antacid, H2-receptor blocking agent, and metoclopramide may be used.
- 15. • C. ANTISIALOGOGUES • Secretions obscure the view • Prevents the local anesthetics from reaching intended areas, • Administered approximately 1.5 hours prior to the application of local anesthetics • Atropine: • Dosage : 0.01-0.02 mg/kg i.v. • : 0.02 mg/kg i.m. • Glycopyrrolate : • Dose: 0.005-0.01 mg/kg • Onset in 1 to 2 minutes • 20 min. before intubation
- 16. D. Nasal mucosal vasoconstrictors • Patient requires awake nasal intubation, adequate anesthesia of this area, along with vasoconstriction, is essential • Agents commonly used are 4% cocaine and 2% lidocaine with 1% phenylephrine • Adequate anesthesia and vasoconstriction can be achieved in 10 to 15 minutes • Nasal decongestants 0.025% to 0.05% oxymetazoline hydrochloride nasal solution sprayed twice in each nostril
- 17. PREOPERATIVE PREPARATIONS • 1. STAFF • One additional individual to serve as an assistant in DA management. • Preferred whenever possible is a second anesthesiologist who can assist in the monitoring and ventilation of the patient • 2. MONITORS • During AI, the routine use of ECG, noninvasive BP monitor, pulse oximetry, capnography, and a precordial stethoscope is required as part of standard basic intraoperative monitoring
- 18. • 3. SUPPLEMENTAL OXYGEN • Supplemental oxygen (O2) should be considered during the entire process of DA management • In addition to the standard methods there are nonconventional methods for increasing the fractional concentration of o2in inspired gas (fio2): • suction port of the FOB, • Atomizer during topicalization, or • Elective transtracheal jet ventilation (TTJV)
- 19. 4 . AIRWAY EQUIPMENT • Suggested Contents of the Portable Unit for Difficult Airway Management : • 1. Rigid laryngoscope blades • 2. Endotracheal tubes of assorted sizes. • 3. Endotracheal tube guides. • 4. Fiberoptic intubation equipment. • 5. Retrograde intubation equipment. • 6. At least one device for emergency nonsurgical airway ventilation. • 7. Equipment suitable for emergency surgical airway access • 8. An exhaled CO2 detector. • 9. Pulse oximetry unit. • 10. Portable O2 tank.
- 20. TOPICALIZATION • A. LIDOCAINE • Available in various preparations including aqueous (1%, 2%, and 4%) and viscous (1%) solutions, ointment (1%), and aerosol preparation • Xylocaine 10% metered-dose oral spray (astra) delivers 10 mg per spray and rapidly anesthetizes the upper airway. • B. BENZOCAINE • Benzocaine is available for use as 10%, 15%, and 20% solutions
- 21. • C. COCAINE • Local anesthesia and vasoconstriction when applied topically • Available as 4% and 10% solutions, for topical application. • The 10% solution is not used because of a very high incidence of toxic effects. • The maximum dose should not exceed 200 mg or 1 mg/kg. • Cocaine should be used with caution in patients with known hypersensitivity, coronary artery disease, hypertension, pseudocholinesterase deficiency, preeclampsia or hyperthyroidism as well as in children, elderly patients, and patients receiving monoamine oxidase inhibitors
- 22. • E. Application Techniques • 1. ATOMIZERS • Tetracaine : 0.3% to 0.5% with epinephrine 1:200,000 maximum 4 to 7 mL, • Lidocaine :4% maximum 10 mL, • placed in an atomizer , connected to the oxygen tank (flow, 8 to 10 L/min), and sprayed in the oropharynx for 10-second periods with 20- second rest intervals for about 20 minutes
- 24. • 2. NEBULIZERS • The ultrasonic nebulizer utilizes 5 mL of 4% lidocaine to be nebulized with O2 (6 to 8 L/min). • The size of the droplet depends on the flow of O2 and the type of nebulizer. • With O2 flow less than 6 L/min, droplet sizes of 30 to 60 μm can be achieved, coating the mucosa up to the trachea. • Other less commonly used techniques for topical anesthesia include lozenges (amethocaine lozenges 60 mg) and gargle with 4% lidocaine gel.
- 25. • NERVE BLOCKS
- 26. SENSORY NERVE SUPPLY 0F AIRWAY
- 27. • A. NASAL CAVITY AND NASOPHARYNX • The majority of the innervation is derived from two sources: the sphenopalatine ganglion and the anterior ethmoidal nerve. • Located in the pterygopalatine fossa posterior to the middle turbinate. • The greater and lesser palatine nerves, provide sensory innervation to the nasal turbinates and to two thirds of the posterior nasal septum
- 28. SPHENOPALATINE NERVE BLOCK: NASAL APPROACH • Long cotton-tipped applicators soaked in either 4% cocaine or 4% lidocaine with epinephrine 1:200,000 applied over the mucosal surface overlying the ganglion • The applicator should be angled at approximately 45-degree angle to the hard palate until the upper posterior wall of the nasopharynx (sphenoid bone) is reached. • The applicators are then left in place for approximately 5 to 10 minutes
- 30. • ANTERIOR ETHMOIDAL NERVE BLOCK • The anterior ethmoidal nerve is blocked by the insertion of a long cotton-tipped applicator, soaked in either 4% cocaine or 4% lidocaine with epinephrine 1:200,000, that is placed parallel to the dorsal surface of the nose until it meets the anterior surface of the cribriform plate . • The applicator is held in position for 5 to 10 minutes.
- 31. B. OROPHARYNX • The somatic and visceral afferent fibers of the oropharynx are supplied by a plexus derived from the vagus, facial, and glossopharyngeal nerves (GPN). • GPN supplies sensory innervation to the posterior third of the tongue (lingual branch), vallecula, anterior surface of the epiglottis, posterior and lateral walls of the pharynx, and the tonsillar pillars.
- 32. • 2. GLOSSOPHARYNGEAL NERVE BLOCK • The oropharynx is topicalized • patient is placed in the sitting position and asked to protrude the tongue anteriorly • displaces the tongue medially, forming a gutter or trough • The gutter ends in a cul-de-sac formed by the base of the palatoglossal arch • A 25-gauge spinal needle is inserted at the base of the cul-de- sac and advanced 0.25 to 0.5 cm • Two milliliters of 1% to 2% lidocaine is injected, and the procedure is repeated on the other side
- 33. • COMPLICATIONS: headache,pharyngeal abcess,hematoma,paralysis of pharyngeal muscles with airway obstruction
- 34. . LARYNX • The SLN supplies sensory innervation to the base of the tongue, vallecula, epiglottis, aryepiglottic folds, arytenoids, and down to but excluding the vocal cords. • The SLN originates as a branch of the vagus nerve, lying deep to the carotid artery. It then travels anteriorly and at the level of the cornu of the hyoid bone branches
- 35. • Position And Landmarks • The patient is placed in the supine position, head slightly extended. • The cornu of the hyoid bone lies beneath the angle of the mandible and anterior to the carotid artery • The superior cornu of the thyroid cartilage can be recognized by palpating the thyroid notch and tracing the upper edge of the thyroid cartilage posteriorly.
- 36. EXTERNAL APPROACH: • The patient is placed supine with the neck extended. • The hyoid bone is displaced laterally toward the side to be blocked, • 25-gauge, 2.5-cm needle is walked off the greater cornu of the hyoid bone inferiorly and advanced 2 to 3 mm. As the needle passes through the thyrohyoid membrane, a slight loss of resistance is felt, and 3 mL of 1% lignocaine solution is injected superficial and deep to this structure. The block is then repeated on the opposite side. 36
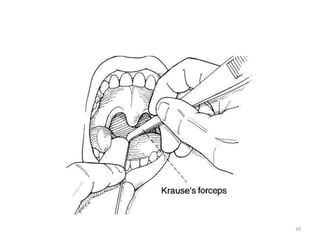
- 38. INTERNAL APPROACH: PYRIFORM FOSSA • Patient is asked to open the mouth widely, and the tongue is grasped using a guaze pad or tongue blade. • A right angle forcep (e.g., Jackson-Krause) is covered with anesthetic-soaked guaze and is slid over the lateral posterior curvature of tongue and down into the pyriform sinuses bilaterally. • Cotton swabs are held in place for 5 minutes. 38
- 39. 39
- 40. D. TRACHEA AND VOCAL CORDS Translaryngeal block Patient selection – A translaryngeal block results in anesthesia of the trachea below the vocal cords. – However, injection of local anesthetic usually stimulates the cough reflex, and this block should be avoided in patients in whom coughing is undesirable. Drug – 3-4 ml of 4% lidocaine 40
- 41. – Patient lies supine with neck slightly extended – Cricothyroid memb. is identified.
- 42. Position – A 22 gauge or smaller needle is inserted into midline until air can be freely aspirated . – 3ml of LA is injected rapidly – Needle should be removed rapidly since the pt usually coughs vigorously. – This helps in spreading the LA under the vocal cord thus causing rapid anaesthesia of trachea &carina.
- 44. 44
- 45. Potential problem – Coughing – Bleeding from thyroid gland & its blood vessel. – Tracheal injury. – Subcutaneous emphysema.
- 46. SPRAY AS YOU GO TECHNIQUE • Noninvasive and involves injecting local anesthetics through the suction port of the FOB. • It requires attaching a triple stopcock to the proximal portion of the suction port in order to connect oxygen tubing to flow at 2 to 4 L/min. • Under direct vision through the bronchoscope, targeted areas are sprayed with aliquots of 0.2 to 1.0 mL of 2% to 4% lidocaine. The physician then waits 30 to 60 seconds before advancing to deeper structures and repeating the maneuver. 46
- 47. LABAT TECHNIQUE • Method of anesthetizing the vocal cords and trachea. • This technique requires a laryngeal mirror, a head lamp, and a Labat needle. • Sitting position, mouth wide open, the tongue is pulled outward. 47
- 48. • In a right hand–dominant physician the left hand holds the laryngeal mirror over the oropharynx in order to identify the vocal cords. The right hand then holds the Labat needle and syringe and drips local anesthetic (4 mL of 2% lidocaine) over the vocal cords.
- 49. The most difficult part of Awake intubation is – the decision to do it. THANKS