Brain tumours part 1
- 1. Presentor- Dr.Vrishit Saraswat Moderator- Dr. Dharm raj Meena
- 2. all or none law is applied
- 5. Relative prevalence of brain tumors in children. Metastases, anaplastic astrocytoma, and glioblastoma multiforme are rare. Pilocytic astrocytoma and PNETs are more common compared to adults
- 7. AT/RT = atypical teratoid/rhabdoid tumor; DIG/DIA = desmoplastic infantile ganglioglioma or astrocytoma; DNET = dysembryoplastic neuroepithelial tumor; N/A = central nervous system tumor not assigned a grade by the World Health Organization; PNET = primitive neuroectodermal tumor; PPTID = pineal parenchymal tumor of intermediate differentiation; PTPR=papillary tumor of the pineal region. Tumors of Neuroepithelial Tissue ASTROCYTIC OTHER NEUROEPITHELIAL Pilocytic astrocytoma I Astroblastoma N/A Pilomyxoid astrocytoma II Chordoid glioma of third ventricle II Subependymal giant cell astrocytoma I Angiocentric glioma (ANET) I Pleomorphic xanthoastrocytoma II Diffuse astrocytoma II NEURONAL, MIXED GLIONEURONAL Anaplastic astrocytoma III Gangliocytoma I Glioblastoma multiforme IV Ganglioglioma I Gliosarcoma IV DIG/DIA I Gliomatosis cerebri III DNET I Central neurocytoma II OLIGODENDROGLIAL Extraventricular neurocytoma II Oligodendroglioma II Cerebellar liponeurocytoma II Anaplastic oligodendroglioma III Paraganglioma (spinal cord) I Oligoastrocytoma II-III Papillary glioneural tumor I Rosette-forming glioneuronal tumor I EPENDYMAL Subependymoma I PINEAL REGION Myxopapillary ependymoma I Pineocytoma I Ependymoma II PPTID II-III Anaplastic ependymoma III Pineoblastoma IV PTPR II-III CHOROID PLEXUS Choroid plexus papilloma I EMBRYONAL Atypical choroid plexus papilloma II Medulloblastoma IV Choroid plexus carcinoma III PNET IV AT/RT IV
- 8. Cellular constituents of the neuropil include astrocytes, oligodendrocytes, neurons, microglia, choroid plexus, and ependymal cells.
- 9. Astrocytomas are the largest group of primary brain tumors. More than half are AA (WHO grade III), GBM (grade IV). Astrocytoma (grade II), pilocytic astrocytoma (grade I) account for about 1/3 of all cases
- 10. N/A = central nervous system tumor not assigned a grade by the World Health Organization. Table adapted from Louis DN et al: World Health Organization Classification of Tumours of the Central Nervous System. 4th ed. Lyon, France: IARC Press, 2007. Meningeal Tumors MENINGOTHELIAL NONMENINGOTHELIAL MESENCHYMAL Meningioma I Lipoma I Atypical meningioma II Liposarcoma N/A Anaplastic/malignant meningioma III Chondroma I Chondrosarcoma N/A OTHER RELATED Osteoma N/A Hemangioblastoma I Osteosarcoma N/A Osteochondroma N/A PRIMARY MELANOCYTIC Hemangioma I Diffuse melanocytosis N/A Hemangiopericytoma II-III Melanocytoma N/A Malignant melanoma N/A Meningeal melanomatosis N/A
- 11. MPNST = malignant peripheral nerve sheath tumor; N/A = central nervous system tumor not assigned a grade by the World Health Organization. Table adapted from Louis DN et al: World Health Organization Classification of Tumours of the Central Nervous System. 4th ed. Lyon, France: IARC Press, 2007. Other Tumors CRANIAL & SPINAL NERVE TUMORS SELLAR REGION TUMORS Schwannoma I Craniopharyngioma I Neurofibroma I Adamantinomatous MPNST II-IV Papillary Granular cell tumor of neurohypophysis I GERM CELL TUMORS Pituicytoma I Germinoma II Spindle cell oncocytoma of adenohypophysis I Embryonal carcinoma N/A Yolk sac tumor N/A LYMPHOMA/HEMATOPOIETIC Mixed germ cell tumor N/A Malignant lymphoma N/A Teratoma N/A Plasmacytoma N/A Mature teratoma Leukemia/granulocytic sarcoma N/A Immature teratoma Teratoma with malignant degeneration
- 13. Tumor spread Intra- versus Extraaxial
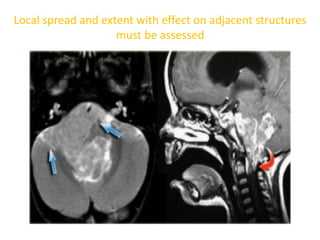
- 15. Local spread and extent with effect on adjacent structures must be assessed
- 16. Midline crossing • Glioblastoma multiforme (GBM) • Radiation necrosis • Meningioma • Lymphoma • Epidermoid cysts • MS
- 17. Multifocal disease • Multiple tumors in the brain usually indicate metastatic disease • Primary brain tumors are typically seen in a single region, but some brain tumors like Lymphomas Multicentric glioblastomas Gliomatosis cerebri • Multifocal as a result of seeding metastases: this can occur in Medulloblastomas (PNET-MB) Ependymomas Gbms Oligodendrogliomas • Multiple brain tumors can be seen in phacomatoses
- 18. Cortical based tumors • Most intra-axial tumors are located in the white matter. Some tumors, however, spread to or are located in the gray matter. The differential diagnosis for these cortical based tumors includes Oligodendroglioma Ganglioglioma Dysembryoplastic Neuroepithial Tumor (DNET)
- 19. CORTICALLY BASED TUMORS WITH “CYST + NODULE” • Common – Ganglioglioma – Metastasis • Less Common – Pilocytic astrocytoma – Pleomorphic xanthoastrocytoma – Glioblastoma multiforme • Rare – Hemangioblastoma – Desmoplastic infantile astrocytoma/ganglioglioma – Papillary glioneuronal tumor – Schwannoma
- 20. CT and MR Characteristics • Fat - Calcification - Cyst
- 21. LOOK FOR… • High on T1 • Cystic versus Solid • Low on T2
- 22. Enhancement No enhancement is seen in: • Low grade astrocytomas • Cystic non-tumoral lesions: • Dermoid cyst • Epidermoid cyst
- 24. astrocytomas • 60% of all primary tumours • Circumscribed and Diffuse • Circumscribed less common
- 25. GLIOMAS • PILOCYTIC ASTROCYTOMA • PLEOMORPHIC XANTHOASTROCYTOMA • SUBEPENDYMAL GIANT CELL ASTROCYTOMA • DIFFUSE LOW GRADE ASTROCYTOMA • ANAPLASTIC ASTROCYTOMA • GLIOBLASTOMA MULTIFORMA • GLIOMATOSIS CEREBRI ASTROCYTOMA OLIGODENDROGLIOMA EPENDYMOMA CHOROID PLEXUS NEOPLASM •CHOROID PLEXUS PAPILLOMA •CHOROID PLEXUS CARCINOMA
- 26. GRADE I Circumscribed Astrocytoma Generally benign , well circumscribed tumor No tendency to progress to higher grade Types : - Pilocytic astrocytoma - Subependymal giant cell astrocytoma -Pleomorphic astrocytoma Grade II Diffuse Astrocytoma Diffusely infiltrating, well differentiated tumor Minimal pleomorphism or nuclear atypia No vascular proliferation or necrosis Imaging Homogeneous No Enhancement No Edema Grade III Anaplastic astrocytoma Pleomorphism and nuclear atypia Increased cellularity & mitotic activity Vascular proliferation No necrosis Imaging : Variable Enhancement, Edema Grade IV Glioblastoma multiforme Marked vascular proliferation and necrosis Increased cellularity , anaplasia, & pleomorphism. Imaging : Heterogeneous (Necrosis, Blood) Ring Enhancement Marked Edema and mass effect
- 27. Pilocytic astrocytomas • Well circumscribed, slow-growing tumor, often with cyst & mural nodule • Peak incidence- 5-15 yrs of age • WHO grade I • Best diagnostic clue- 1. Cystic cerebellar mass with enhancing mural nodule 2. Enlarged optic nerve/ chiasm/ tract variable enhancement • Location - Cerebellum (60%) > optic nerve/ chiasm (25-30%) > adjacent to 3rd ventricle > brainstem • 15% of NF type I patients develop PAs, M/C in optic pathway • Size - Larger lesions in cerebellum, often >3cm - Optic nerve lesion typically smaller
- 28. CT findings • NECT -Discrete cystic-solid mass Little or no surrounding edema • CECT - >90% enehnce -50% nonenhancing cyst, strongly enhancing mural nodule -40% solid with necrotic center, heteterogenous enhancement -Cyst wall may have some enhencement MR findings • T1WI - Solid portions iso/hypointense to GM, cyst iso to hyperintence to CSF • T2WI & FLAIR - Solid portions hyperintense to GM - Cyst contents iso/hyperintense to CSF (do not suppress on FLAIR) - Optic pathway hyperintense to GM
- 29. • TIWI C+ - Intense but heterogeneous enhancement of of solid portion - Cyst wall ocassionly enhances - Optic pathway – variable enhancement • MRS - Increase choline & lactate, decrease NAA • Best imaging tool - Contrast-enhanced MR
- 30. Childhood astrocytomas are illustrated. Pilocytic astrocytoma is common in the cerebellum, hypothalamus/optic nerves . Pontine tumors are diffusely infiltrating WHO II tumors. Hemispheric
- 31. Typical cerebellar pilocytic astrocytoma with a vascularappearing tumor nodule , large nonneoplastic cyst . The cyst wall consists of compressed but otherwise histologically normal brain parenchyma
- 32. NECT scan shows a posterior fossa PA with cysts , solid tumor nodule , Ca++[10-20% ] , associated obstructive hydrocephalus
- 33. Axial FLAIR MR shows a classic cyst with mural nodule appenance of cerebellar PA in a child. Typical lack of surrounding edema in adjacent cerebellum. Mass effect on the 4th ventricle seen.
- 34. PILOCYTIC ASTROCYTOMA OF THE OPTIC NERVE enlargement (arrow) of the left optic nerve within the intraconal compartment characteristic kinking (arrowhead) of the enlarged left optic nerve. PD WI –mild hyperintensity of the mass intense enhancement of the mass. T1-weighted image PD-weighted image T1 C+
- 35. T1 and T2 W MR Images show right optic nerve pilocytic astrocytoma with posterior extension into optIc chiasm. hypointense on TI- and hyperintense on T2-weighted Images. Left side of optic chiasm is displaced but uninvolved
- 36. Bilateral optic nerve gliomas Assoc with NF 1
- 37. DIFFERENTIAL DIAGNOSIS • pituitary macroadenoma (with cystic degeneration / necrosis) – AGE – intrasellar epicentre with pituitary fossa enlargement – calcification in these cases is often absent – Heterogenous enhancement • Cranipharyngioma • Rathke's cleft cyst – no solid / enhancing component – unilocular – majority are completely or mostly intrasellar • intracranial teratoma – presence of fat is helpful, but requires fat saturated sequences or CT of confirm
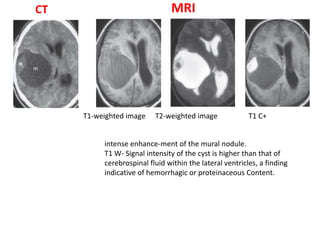
- 38. CT MRI intense enhance-ment of the mural nodule. T1 W- Signal intensity of the cyst is higher than that of cerebrospinal fluid within the lateral ventricles, a finding indicative of hemorrhagic or proteinaceous Content. T2-weighted imageT1-weighted image T1 C+
- 39. DIFFRENTIAL DIAGNOSIS • Ganglioglioma 1st two decade Discrete, solid/cystic, cortically- based enhancing mass, suptratentorial Ca++ common • PLEOMORPHIC XANTHOASTROCYTOMA younger age gp cortical based lesion with dural tail
- 40. Pleomormic xanthoastrocytoma (PXA) • Superficial location in cerebral hemisphere with involvement of meninges • Tumor of childrem & young adults (2/3 < 18 yrs) • WHO grade II • Best diagnostic clue - Supratentorial cortical mass with adjacent enhancing dural “tail” - Cyst & enhancing mural nodule typical • Location – - Peripherally located hemispheric mass, often involves cortex & meninges (98% supratentorial) - - Temporal lobe m/c (40-50%) > F & P > occipital lobe
- 41. • CT finding • NECT - - cystic/solid mass- hypodense with mixed density nodule - Minimal or no edema is typical - Ca++, haemorrhage rare • CECT - strong, sometimes heterogenous enhancement of tumor nodule • MR findings • T1WI - Mass is hypo or isointense to gray matter - Cystic portion isointense to CSF • T2WI & FLAIR - Hyperintense or mixed signal intensity mass - Cystic portion isointense to CSF • T1WI C+ - Enhancement usually moderate/ strong, well delineated - Enhancement of adjacent meninges, dural tail common
- 42. • FEATURES THAT DISTINGUISH PMA FROM PA • Pathology – Piloid cells + myxoid background – Angiocentric growth – WHO grade II • Clinical Issues – More common in infants, children < 4 years – More aggressive behavior • Imaging – Large, bulky, H-shaped tumor – Hemorrhage more common in PMA – CSF dissemination common PMA
- 43. Coronal graphic shows a cystic & solid cortical mass with thickening of the adjacent meninges characteristic of PXA. The mural nodule often abuts the pial surface & may result in dural “tail”.
- 44. T1 & TI C+ MR image shows enhancing cortical mass with thickening of adjacent meninges.
- 45. Pilocytic astrocytoma supratentorial location rare older age gp no dural tail Ganglioglioma Mural nodule typical, o not adjacent to meninges no enhancing dural "tail" Ca++ is common; DNET Superficial cortical tumor, Multicystic "bubbly" ,appearanc , mild enhancement DIFFRENTIAL DIAGNOSIS Cystic Meningioma Diffusely enhancing dural-based mass with dural "tail" Usually older patients Strong female preponderance
- 46. SGCA/sega • Benign slow growing glioneuronal tumor arising near foramen of monro in patient with tuberous sclerosis complex (TSC) • Typically occurs during first 2 decades • M/C CNS neoplasm in TSC (upto 15% of patient with TSC) • WHO grade I • Best diagnostic clue – - Enlarging enhanvcing foramen of monro mass in patient with TSC - Other imaging finding of TSC (cortical tubers, subependymal nodules) • SIZE- - SEGAs variable, slowly growing - Often presents when 2-3cm, causes obstructive hydrtocephalus - > 1cm subependymal nodules / symptomatic nodules
- 47. • CT findings • NECT - Hypo to isodense, Heterogeneous - Ca++ variable • CECT - Heterogeneous, strong enhancement MR findings • T1WI - Hypointense to isointense to gray matter - +- Ca++ hyperintense to hyperintense • T2WI - Hetrogeneous- isointense to hyperintense - Ca++ foci hypointense • T2 GRE - Low signal from calcification • T1WI C+ - Robust enhancement, enlarging enhancing foramen monro mass > 1.2cm suggest SGCA
- 48. Coronal graphics demostrated hydrocephalus secondary to a subependymal gaint cell astrocytoma (SGCA) arising near the left foramen of monro. Subependymal tuber also presrent.
- 49. • RADIOLOGY: - CT Radiologic hallmark is a markedly contrast- enhancing mass located at or very near the foramen of monro. Calcification + Obstructive hydrocephalus Other features of Tuberous Sclerosis present
- 50. MRI T2WT1W T1 C+
- 51. DIFFRENTIAL DIAGNOSIS CENTRAL NEUROCYTOMA Well defined, variably vascularized lobulated mass Origin near foramen of Monro or septum pellucidum Necrosis and cyst formation are common calcification not seen SUBEPENDYMOMA Tumor of middle age and elderly LOCATION Inferior 4th and frontal horn most common Non enhancing mass CHOROID PLEXUS TUMORS younger age gp <5yrs Vivid enhancement ± CSF seeding Calcification less c’mon Parenchymal invasion and peritumoral edema with CPCA
- 52. LOW-GRADE DIFFUSE ASTROCYTOMA • Well differentiated but infiltrating neoplasm, slow growth pattern • Majority occurs between 20-45 yrs • WHO grade II • Siezure is the M/C presenting feature • Best diagnostic clue • Focal or diffuse non enhancing white matter mass • Location - Cerebral hemispheres, supratentorial 2/3 - Frontal lobe 1/3, temporal lobe 1/3 - Infratentorial 1/3 • Brainstem (50% of brainstem gliomasWell differentiated but infiltrating neoplasm, slow growth pattern • Majority occurs between 20-45 yrs • WHO grade II • Siezure is the M/C presenting feature • Best diagnostic clue • Focal or diffuse non enhancing white matter mass LOW-GRADE DIFFUSE ASTROCYTOMA • Well differentiated but infiltrating neoplasm, slow growth pattern • Majority occurs between 20-45 yrs • WHO grade II • Siezure is the M/C presenting feature • Best diagnostic clue • Focal or diffuse non enhancing white matter mass • Location - Cerebral hemispheres, supratentorial 2/3 - Frontal lobe 1/3, temporal lobe 1/3 - Infratentorial 1/3 • Brainstem (50% of brainstem gliomasWell differentiated but infiltrating neoplasm, slow growth pattern • Majority occurs between 20-45 yrs • WHO grade II • Siezure is the M/C presenting feature • Best diagnostic clue • Focal or diffuse non enhancing white matter mass
- 53. • Location - Cerebral hemispheres, supratentorial 2/3 - Frontal lobe 1/3, temporal lobe 1/3 - Infratentorial 1/3 - Brainstem (50% of brainstem gliomas are low grade astrocytoma- occur in pons & medulla of children/ adolescents) • Homogenous mass with enlargement & distortion of affected structures CT findings • NECT - Ill-defined homogeneous hypodense/ isodense mass - 20% Ca++, cystd are rare • CECT - No enhancement or very minimal - Enhancement should raise suspicion of focal malignant degeneration
- 54. MR findings • T1WI - Homogeneous hypointense mass • T2WI & FLAIR - Homogeneous hyperintense mass • DWI - Typically no diffusion restriction • T1WI C+ - Usually no enhancement - Enhancement suggest progression to higher grade • MRS - High choline, low NAA typical but not specific • MR perfusion • Relatively lower r CBV compared ton AA, GBM • PROTOCOL advice • Contrast-enhanced MR
- 55. Coronal graphic shows an infiltrating mass centered in the white matter
- 56. Ill defined , homogenous , hypo / isodense WM mass distortion of affected structures calcification in 15-20% Hge ,Cyst rare No enhancement , enhancement if +nt s/o malignant degeneration No peritumoral edema CT
- 57. MRI : T1WI - Hypointense T2WI, PD and FLAIR - Hyperintense Hge ,Cyst rare No enhancement , enhancement if +nt s/o malignant degeneration No peritumoral edema
- 58. Sagittal T2 MR image shows a pontine & medullary mass that
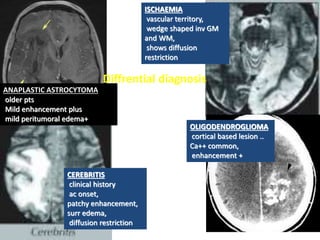
- 59. ISCHAEMIA vascular territory, wedge shaped inv GM and WM, shows diffusion restriction CEREBRITIS clinical history ac onset, patchy enhancement, surr edema, diffusion restriction OLIGODENDROGLIOMA cortical based lesion .. Ca++ common, enhancement + Diffrential diagnosis ANAPLASTIC ASTROCYTOMA older pts Mild enhancement plus mild peritumoral edema+
- 60. SIGNS OF PROGRESSION • Hge • Edema • progressive necrosis • enhancement
- 61. ANAPLASTIC ASTROCYTOMA • Diffusely infiltrating malignant astrocytoma with focal or diffuse anaplasia & marked proliferative potential • Etiology 75% evolve from low-grade diffuse astrocytoma • Pathology • 1/3 of all astrocytomas..Second only to GBM • Lacks necrosis, hemorrhage. WHO grade III • Clinical Issues • Peak age = 40-50 years • Degenerates into GBM • Best diagnostic clue - Infitrating mass that predominantly involves white matter with variable enhancement • Location - Hemispheric white matter – commonly involve frontal & temporal lobes • Morphology – ill- defined hemispheric white matter mass typical
- 62. Imaging CT findings • NECT - Low density, ill-defined mass - Ca ++ , hemorrhage & cyst rare • CECT - Majority do not enhance, enhancement often focal, patchy, heterogeneous - If ring enhancement, consider malignant progression to GBM • T2/FLAIR- diffusely infiltrating heterogenous hyperintense WM mass. • DWI- no diffusion restriction is typical • T1WI C+ - Usually no enhancement, less common: focal, nodular, patchy enhancement. - Ring enhancement is suspicious for GBM ( poor prognosis) • MRS - Elevated cho/cr ratio, decreased NAA • Protocol advice- contrast-enhanced MR
- 63. Axial graphic shows an infiltrative white matter mass with extension along the corpus callosum focal hemorrhage & local mass effect. White matter extension is typical of anaplastic astrocytoma.
- 64. a large ill-defined mass (arrows) centered in the right insula with extension to the frontal and temporal lobes. heterogeneous high T2 signal intensity, cystic areas (arrowheads), mass effect and minimal enhancement. Necrosis (ring enhancement) does not occur, and cyst and hge is occ. Axial T2W T1W post contrast
- 65. LOW GRADE GLIOMA younger age gp Focal or diffuse white matter mass Typically non enhancing no surr edema Hge and cysts rare GBM older age gp hge and cysts more likely necrotic core, Mod enhancement Extensive surrounding edema and invasiion OLIGODENDROGLIOMA middle age adulta Cortical mass with variable enhancement Ca++ common DIFFRENTIAL DIAGNOSIS ROLE OF MRS, DWI , PERFUSION IMAGING
- 66. GLIOBLASTOMA MULTIFORME • Rapidly enlarging malignant astrocytic tumor characterized by necrosis & neovascularity • Most common of all primary CNS neoplasm • 60-75% of astrocytomas • Any age, but peak = 45-75 years • Relentless progression, survival < 1 year • WHO grade IV • Etiology • 2 types: “Primary” GBM: De novo, probably from neural stem cells - >90% of GBMs • “Secondary” GBM: Malignant progression of lower grade astrocytoma - <10% of GBMs • Necrosis & microvascular proliferation is hallmark • Best diagnostic clue • Hemispheres > > pons > > cerebellum, spinal cord • Thick, irregularly enhancing “rind” of neoplastic tissue surrounding central necrotic core (95%) • Hemorrhage common, Ca++ rare • Location - Supratentorial white matter- M/C - Frontal, temporal, parietal > occipital lobes - Cerebral hemisphere > brainstem > cerebellum
- 67. • Morphology - Poorly marginated, diffusely infiltrating necrotic hemispheric mass - Tumor typically crosses white matter tract to involve contralateral hemisphere - corpus callosum ( butterfly glioma), anterior & poterior commissures Imaging CT findings • NECT - Irregular isodense or hypodense mass with central hypodensity representing necrosis - Marked mass effect & surrounding edema/ tumor infiltration - Hemorrhage common, Ca++ rare - CECT • Strong, heterogeneous, irregular rim enhancement MR findings • T1WI - Iiregular isointense, hypointense WM mass - Necrosis, cysts, subcaute hemorrhage & irregular margin common
- 68. • T2WI & FLAIR - Heterogeneous, hyperintense mass with adjacent tumor infiltration/ vasogenic edema • T2 GRE- Susceptibility artifact related to blood products • DWI- variable diffusion restriction in solid portion of tumor • T1WI C+ - thick, irregular rind of enhancement surrounding central necrosis • MRS- decreased NAA, myoinositol & elevated choline • Best imaging tool- contrast-enhanced MR is most sensitive Differential Diagnosis – Common: Metastasis[multiple , oval not infiltrating , GW junction ], abscess[regular rim ,DWI restriction, A peak] – Less common: AA, anaplastic oligo, lymphoma [not necrotic] – Rare: “Tumefactive” demyelination[open rim toward cortex]
- 69. SPREAD OF GLIOMA common- along compact WM tract around ventricular ependyma - CSF seeding into leptomeninges Uncommon- dural invasion Rare – extracerebral metastasis RECURRENCE OF GBM surgical resection s nearly alwys subtotal
- 70. CT : heterogenous mass Hemorrhage and cysts usu present >> AA Necrosis ++ Strong but heterogenous, thick irregular enhancing rind surrounding a necrotic center extensive perilesional edema with mass effect calcification rare unless 2◦ to previous low gr astrocytoma CORPUS CALLOSUM INV COMMON
- 71. Heterogeneous mass, focal low signal intensity’ suggestive of hge high signal intensity suggestive of Cyst or necrosis. Extensive vasogenic edema sur-rounds the tumor Heterogenous enhancement thick, irregular, enhancing walls and areas of central necrosis. T2-weighted MR image CE T 1 -weighted image MRI
- 72. DWI: lower measured ADC than low grade tumors diffusion restriction typical PWI: high rCBV increased
- 73. Left- Axial T2 MR image shows a heterogeneously hyperintense mass
- 74. PRIMARY CNS LYMPHOMA • Periventricular inv more c’mon • Often crosses corpus callosum • Typically isointense/hypointense on T2WI •Vasogenic edema minimal •Homogenous enhancement, heterogenous d/t necrosis in AIDS pts ANAPLASTIC ASTROCYTOMA • LESSER AGE GP •MILD ENHANCEMENT •NECROSIS ABSENT •HGE LESS COMMON DIFFRENTIAL DIAGNOSIS
- 75. MRS: decreased Naa, elevated Cho/ Cr, lactate/water ratios Abscess Ring-enhancement typically thinner than GBM T2 hypointense rim, diffusion restriction + typical MRS may show metabolites such as succinate, amino acids
- 76. conclusion AGE AND ASTROCYTOMAS • Newborn/Infant – Rare – Supratentorial > > infratentorial – Large, bulky, malignant (GBM) hemispheric mass – Less common = pilomyxoid astrocytoma
- 77. • Children/Young Adults • Common • Infratentorial > supratentorial • Pilocytic > diffusely infiltrating astrocytoma > subependymal giant cell astrocytoma (SEGA) • Pilocytic astrocytoma – Cerebellum, fourth ventricle > pons, medulla – Optic chiasm/hypothalamus > tectum – Hemispheric PA rare • Diffusely infiltrating astrocytoma – Low grade > high grade – Brainstem, cerebral hemispheres > cerebellum • SEGA – Look for signs of tuberous sclerosis – Most at/around foramen of Monro
- 78. • Middle-Aged/Older Adults • Older the patient, the more malignant the astrocytoma • GBM > anaplastic > > low-grade astrocytoma • Usually involve hemispheric WM • Posterior fossa very rare






























![NECT scan shows a posterior fossa PA with cysts , solid
tumor nodule , Ca++[10-20% ] , associated obstructive
hydrocephalus](https://image.slidesharecdn.com/braintumourspart-1-181026061031/85/Brain-tumours-part-1-32-320.jpg)

































![• T2WI & FLAIR
- Heterogeneous, hyperintense mass with adjacent tumor infiltration/
vasogenic edema
• T2 GRE- Susceptibility artifact related to blood products
• DWI- variable diffusion restriction in solid portion of tumor
• T1WI C+ - thick, irregular rind of enhancement surrounding central
necrosis
• MRS- decreased NAA, myoinositol & elevated choline
• Best imaging tool- contrast-enhanced MR is most sensitive
Differential Diagnosis
– Common: Metastasis[multiple , oval not infiltrating , GW junction ],
abscess[regular rim ,DWI restriction, A peak]
– Less common: AA, anaplastic oligo, lymphoma [not necrotic]
– Rare: “Tumefactive” demyelination[open rim toward cortex]](https://image.slidesharecdn.com/braintumourspart-1-181026061031/85/Brain-tumours-part-1-68-320.jpg)










