Case presentation
- 1. Case Presentation Atypical Depression with Panic Disorder Dr. Mohamed H Hassan Advanced Clinical Psychiatry Fellow Department of Psychiatry Hamad Medical Corporation Doha, Qatar
- 2. Disclosure • No conflicts of interest to disclose • The opinions expressed are those of the author and do not reflect the views neither of Hamad Medical Corporation nor the Psychiatry Department of Hamad Medical Corporation unless specifically stated
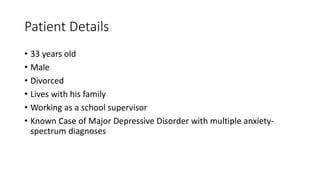
- 3. Patient Details • 33 years old • Male • Divorced • Lives with his family • Working as a school supervisor • Known Case of Major Depressive Disorder with multiple anxiety- spectrum diagnoses
- 4. Hospitalization Information • Admitted to our psychiatric inpatient unit on May 19th, 2019 after being transferred from our walk-in psychiatry clinic • Discharged on July 3rd, 2019 • Total hospitalization duration of 45 days
- 5. Reasons for admission Worsening depressive symptoms over the last 2-3 months prior to his admission & Intense suicidal ideations with irresistible suicidal urges for the last 2 days prior to his admission
- 6. History of present illness
- 7. Over the past few months prior to his admission, the patient had been exhibiting gradually progressive change in his personality and character…..
- 8. • He had been feeling very low and irritable most the days, every day, with early-morning worsening • His main concern was his “ severe inability to enjoy nearly every aspect of his life ” • Related being bored of life and “sick of all of what he is passing through” • Had been feeling extremely tired, exhausted and easily-fatigued, which made him take an extended sick-leave from his work
- 9. • Had been oversleeping excessively, yet, without feeling refreshed upon awakening • Had been overeating, craving sweet materials especially at night, which made him gain extra weight. An issue that added to his distress • Moreover, he had been experiencing significant heaviness over his shoulders and arms • His workmates critiqued him ‘ being inappropriately slow at work, inattentive – as he was committing several errors at work; which contributed to his negative emotions
- 10. • Had been feeling helpless, hopeless and pessimistic about his situation and worthless about himself • With the progressive deterioration of his condition, he started to experience frequent self-harming and suicidal thoughts - thinking everyday of slashing his wrists with a knife and was thinking lately of overdosing with all of his medications in order to end his life • Had actually tried to slash his left wrist with an old kitchen blade 1 day prior to his admission, but it wasn't sharp enough and caused superficial lacerations only • He preferred to see a psychiatrist in order to get a ' final help‘ before resorting to more lethal measures on end his life
- 11. • Furthermore, he reported experiencing a constellation of symptoms – that he identified as ‘panic attacks ‘, that occurred in line with the early morning worsening of his mood • He described these attacks as abrupt racing heart beats, shortness of breath, sweating, dizziness, tremors, associated with intense fear and terror that reaches their maximum intensity within 30 minutes and ceases spontaneously within 1 hour. No specific trigger for these attacks could be identified by the patient • There were no reported symptoms indicative of an underlying obsessive, manic or psychotic process
- 12. • Although he had been adherent to his medications, acknowledging some benefit in terms of managing his anxiety – as it decreased the frequency of the panic attacks to a maximum of 2 times a week -, he related no much advantage in terms of improving his mood • Since 2017 till his most recent admission, he had been maintained on the following medications: Quetiapine 400 mg at bedtime Venlafaxine SR 150 mg twice a day Mirtazapine 30 mg daily Propranolol 30 mg twice a day
- 13. Family History
- 14. • Has 5 brothers and 1 sister • Oldest brother died in a road traffic accident in 2000 • His father died of cardiac problems in 2001 • Has a brother similar mental presentations, however, didn’t seek help • His mother has probably developed late-onset major depressive disorder recently • Reported that his father had severe anger-related problems, which affected his marital life
- 15. Past History
- 16. Past Medical History • Had a bariatric surgery more than 7 years ago - Sleeve Gastrectomy for morbid obesity • Otherwise, he has no significant medical problems
- 17. Past Psychiatric History After passing through a series of legal proceedings following his divorce in 2008, he started to develop symptoms suggestive of Generalized Anxiety Disorder (GAD) in the form of: • Continuous worries and ruminations about the future • Various bodily symptoms including Musculo-skeletal tensions, headaches, restlessness and agitation with disrupted sleeping • He started to self-medicate with alcohol in order to alleviate his distress
- 18. • In 2014, he started to exhibit symptoms of depression which developed concurrently with the increasingly heavy consumption of alcohol • Saw a private psychiatrist for the first time and after a series of assessments he was diagnosed with Major Depressive Disorder, G.A.D and Panic Disorder • Was prescribed various medications from 2014 to 2016 with modest effect including Olanzapine 10 mg daily, Sertraline (100 mg morning + 50 mg at night) and Agomelatine 25 mg daily
- 19. • Had his 1st encounter with our outpatient psychiatric services in Hamad Medical Corporation in March 2016 • Was tried on multiple antidepressants and anxiolytics under an impression of MDD, Panic Disorder and Social Anxiety Disorder • Had his 1st psychiatric admission in May 2016. Was admitted for 2 weeks after exhibiting symptoms similar to his most recent admission (i.e. Intense recurrent suicidal thoughts - of knifing himself - on a background of depressive symptoms, In addition to multiple somatic complaints and panic attacks • Discharge diagnosis then was MDD with comorbid Panic Disorder (with claustrophobia) and Social Anxiety Disorder
- 20. • In late 2016, he had 12 sessions of Electro-Convulsive Therapy (ECT) as an outpatient – after exhibiting limited response to his prescribed medications then – with remarkable efficacy that lasted for around 6 months afterward. For the 1st time ever his mood symptoms improved on a therapeutic regimen which was ECT • Had been maintained on the same medications since 2016 – till his most recent admission – with satisfactory effect on his anxiety, however with only negligible benefit in terms of his mood symptoms • Till his most recent admission, he had been regularly visiting his primary psychiatrist and compliant with his medications – despite the significant increase in his weight they caused
- 21. • Was offered psychotherapy sessions – both as an outpatient and inpatient when he was admitted – however, was very reluctant to attend • Never attempted suicide or any self-harming behaviors or attempts except for the ones described in his most recent admission – See HPI
- 22. Social History • Educated till secondary school level. Couldn’t pursue further higher due to family financial constraints. His scholastic achievement was below average – attributing that to family-related stressors • Has been working in his high school as a students supervisor – following his father’s death in 2001 until now, in order to support his family. However, has been taking numerous sick leaves due to his illness • Ran a couple of businesses in the past – however, all failed eventually with significant financial loss
- 23. Personal History • Described his childhood as ‘ Traumatic’, as he used to witness frequent physical fights between his parents as a child • Married once for 1 year. Described his marriage as ‘unsuccessful with lots of troubles, including domestic violence ‘. No children • Used to enjoy a number of activities including painting and travelling with friends. However, interest in these activities got diminished in line with the severity of his symptoms • Described himself as an introvert
- 24. Substance Use History • Heavy smoker at the current time being – smokes 1-3 packs a day • Consumed alcohol heavily for around 6 years. Last intake was in 2014. Used to drink 5 Vodka shots daily to control his anxiety symptoms. No reported alcohol related problems though • Has history of infrequent cannabis abuse many years ago
- 25. Forensic History • No contacts with the legal system before
- 26. Significant physical findings on examination • Physical Examination: Essentially unremarkable, except for morbid obesity – Weight was 137 kgs, BMI was 55 • Labs were grossly normal including complete blood count (CBC), Liver and Kidney functions, electrolytes, Vit B12 and Folate levels • However, thyroid functions revealed subclinical hypothyroidism: TSH 5.58 [Normal range: 0.30-4.2 mIU/L] FT4 11.9 [Normal range: 11.6-21.9 pmol/L] • CT Head was essentially unremarkable
- 27. Mental Status Examination on Admission Appearance and Behavior: • Young aged man looking his stated age, cooperative despite appearing distressed • With fair groom and hygiene, with markedly overweight built • His eye contact was interrupted • With no evident Psycho-motor abnormality noted
- 28. Mood and Affect: • His mood was ' Miserable ‘ • With congruent restricted dysphoric affect - Tearful during the whole interview Speech: • Slightly below average volume and tone, with average rate, coherent and relevant
- 29. Though Form: • His thought process was linear, logical and goal-directed Though Content: • No elicited psychotic delusional thoughts • No elicited obsessions • Evident suicidal thoughts, with active plans, intents and gestures ' looking for a sling to hang himself or a window to jump from while in the ward’ • Evident hopelessness, helplessness, worthlessness, anhedonia and pathological guilt feeling
- 30. Perception: • No evident abnormal perceptual experiences Insight and Judgement: • With fair insight and proper judgment
- 31. Cognition: • Was conscious, alert and oriented to time, place and person • Immediate, recent and remote memory functions were intact • Intact focused and sustained attention span • Mini Mental Status Examination (MMSE) score was 30/30 • With proper abstraction: she was able to interpret a proverb
- 32. Hospital Course
- 33. Initially… • Was exhibiting evident symptoms and signs indicative of severe major depressive disorder and panic disorder • Was actively suicidal ‘ was trying to find a way to act upon his suicidal thoughts and intents as he was looking for a window to jump from or a sling to hang himself over’ • Was socially isolated and disengaged, preferring to spend most of his time alone in his room • Wasn’t participating in the ward’s intensive Occupational Therapy (OT) sessions or activities
- 34. Progress of management… • He was initially maintained on his home medications namely: Quetiapine 400mg at bedtime, Mirtazapine 30 mg at bedtime Venlafaxine SR 150mg twice a day and Propranolol 30 mg twice a day • We supplemented the patient with Levothyroxine 100 mcg daiy – mainly to control for his subclinical hypothyroidism which might had contributed to his obesity problem and as an augmentation strategy to his antidepressant regimen • After thoroughly reviewing the patient's old charts and following a series of extensive assessment interviews, we came with a clinical impression that the patient suffers from MDD – with Atypical Features with comorbid Panic Disorder (DSM-5 Diagnostic Criteria)
- 35. • The patient consented for 12 ECT sessions – but completed 10 only due to significant improvement in his condition • Quetiapine was gradually withdrawn during the course of ECT * • Upon completion of ECT, Lithium therapy was initiated, reaching a dose of 800 mg daily * *These steps were taken given the atypical nature of his depression, as an approved augmentation strategy and to alleviate suicidality. Also, due to Quetiapine's significant metabolic side effects – especially that the patient had been on it since 2016 with modest efficacy and eventually suffered from morbid obesity
- 36. Summary of medications changes • Venlafaxine SR 150mg BID no change since admission • Mirtazapine 30 mg No change since admission • Propranolol 30mg BID No change since admission • Levothyroxine 100 mcg Added on May 21st • Quetiapine Gradually tapered off till discontinuation on June 24th • ECT was started on May 26th, and completed on Jun 27th • Lithium Started on 400mg daily on June 24th, and titrated to 800 on June 27th
- 37. • Achieved remarkable improvement with the progress of his hospitalization, as his sleep gradually improved, and so did his energy, motivation and social engagement • Started to actively engage in OT activities including art therapy • His marked anhedonia and pessimism resolved and maintained a futuristic and optimistic thinking style and pattern • With the progress of his treatment, he became no longer suicidal and hadn’t exhibited any self-harming thoughts, intents or gestures
- 38. • Started psychological work – mainly basic Cognitive Behavioral Therapy (CBT) focusing on behavioral modification, In addition to basic mindfulness and progressive muscle relaxation targeting his depressive and anxiety symptoms respectively • Allowed for multiple therapeutic leaves with excellent feedback and satisfactory outcome, till his discharge back to his home
- 40. Bio Psycho Social Predisposing Factors 1. Positive Family History of mental illness indicating a strong genetic predisposition as similar psychiatric symptoms are present in a sibling indicating a probable underlying mental illness – in the form of irritability and significant anger management , in addition to anger-related problems in his father; However, it was never evaluated 2. Significant history of alcohol misuse prior to the onset of his depressive symptoms 1. The sudden, unexpected loss of his past-older brother – with whom he had strong bond – after a road traffic accident 2. Significant history of difficulties and indirect traumas during childhood – i.e. witnessing frequent incidents of domestic violence; when his past father used to be aggressive towards the mother 1. Stress due to early responsibilities towards the family
- 41. Bio Psycho Social Precipitating Factors 1. Atypical nature of his depressive illness 2. Undiagnosed hypothyroidism 3. Resistance to antidepressant therapy Unclear - Breakup with his wife as apparently, he was against the divorce? 1. Divorce from his wife in 2008, after a 1 year of marriage due to family conflicts 2. Legal proceedings following the divorce – which he described as quite stressful and lengthy meetings – in 2008 3. Financial problems – due to failed businesses, in 2014
- 42. Bio Psycho Social Perpetuating Factors 1. Possibility of Lithium- induced hypothyroidism 2. Possibility of future losing of ECT effect 3. Frequent benzodiazepines use?? 1. Very limited frustration tolerance 2. Dependence on others/external objects in terms of solutions – evidenced by almost complete reliance on pharma for assuring relief 1. Limited social circle – very few friends and social activities 2. Single??
- 43. Bio Psycho Social Protective Factors 1. Strong adherence to medical regimens 2. Maintained abstinence/sobriety from substances 1. Various coping strategies 2. Therapeutic alliance with service providers 1. Supportive, flexible and relatively stress-free work conditions 2. Supportive family environment
- 44. Computational Formulation The BrainProfiler Platform
- 45. • Recording of the patient’s clinical progress using the BrainProfiler platform • Measured regularly as a requirement of conducting ECT course, as pre-ECT, during ECT course and post-ECT • Severity grading corresponds to scores of the depression and anxiety subscales of the Hamilton Depression Scale (HAM-D)
- 47. May 22nd, 2019 Before 1st ECT session
- 48. Computational Psychiatry Plasticity Diagnosis of the Patient Generalized Anxiety (Moderate) = Dist’ Constraint frustration • Possible generalized anxiety syndrome Sensible Instability of brain systems (reactive plasticity) cause moderate anxiety. Consider anxiety meds Depression (Marked) = Atrophy and De-optimization • Depression Marked decrease in brain plasticity (adaptive plasticity i.e., growth dynamics of brain-cells) cause severe depression. Start medications for depression
- 49. Explanation of Computational Psychiatry Diagnosis of the Patient Moderate Generalized Anxiety = Dist’ Constraint frustration • Moderate Disturbances to longer timescale those of minutes to hours, the stabilizing network plasticity in the face of perturbations caused from large alterations of environmental dynamics (i.e., stress). Stress and intense network computational activity perturbs brain network stability resulting in "Constraint Frustration" among neurons and network systems. A connection is considered "frustrated" when the weighted value of connectivity is in discrepancy with the value of neuronal activation. In other words within neuronal ensembles when the value of connection weights are incompatible with that of values of neuronal activation. The emergent property of that condition manifests as anxious sensation. Any increase of computational demand on the neuronal network can cause frustration to constraints, obviously connectivity imbalances cause frustration to constraints but also optimization shifts and abrupt stimulus can generate such frustrations of constraints. Here increase of computational demand generates Anxiety (as emergent property). When validated by signal processing of brain-imaging it is expected to find slightly reduced Correlation-matrixes, slight disconnection in graph-analysis, minimal increase error predictions in Dynamic-Causal-Modeling. Slight Increase in entropy-measurements (Free Energy). Slight resting-state-networks disconnected when activated all operating over timescales of minutes and hours
- 50. Marked Depression = Atrophy and De-optimization • Marked Disturbance to “Adaptive Plasticity” slower time-scales, those that span hours to weeks and are responsible for reducing free energy the differences between internal representations (emergent constructs) and external environmental occurrences. Deoptimization takes place when free energy increases and mismatch between internal representations and external events becomes larger. Deopitmization dynamics caused by reduced neuronal plasticity, emerging (Emergent Property) as depressed mood. Normally the brain continually updates internal representations (error-prediction and correction); these are internal representations of the world of our experiences built from memories of past familiarities. The experience continually updates the internal formations to match what is transpiring, this process of update reduces inconsistencies (Free Energy) and is called “optimization,” because it optimizes internal representations to match real life events and occurrences, when neural plasticity is hampered the optimization process is disturbed and De-optimization dynamics takes over. Mismatch between internal configurations and actual occurrences transpire, with depressed mood as a consequent emergent property • When validated by signal processing of brain-imaging it is expected to find reduced dynamics of Correlation-matrixes compared over long time scales of months, the same in graph-analysis over long time scales of months, increase error predictions (free energy) in Dynamic-Causal-Modeling over long time scales of months. The same with increase of entropy-measurements (Free Energy) over long time scales of months
- 51. June 3rd, 2019 After 3rd ECT session
- 52. Computational Psychiatry Plasticity Diagnosis of the Patient Generalized Anxiety (Moderate) = Dist’ Constraint frustration • Possible generalized anxiety syndrome Sensible Instability of brain systems (reactive plasticity) cause moderate anxiety. Consider anxiety meds Depression (Mild) = Atrophy and De-optimization • Check for possible depressive syndrome Mild decrease in brain plasticity (adaptive plasticity) (i.e., growth dynamics of brain- cells) cause somewhat mild depression Follow-up if medications for depression are required
- 53. Explanation of Computational Psychiatry Diagnosis of the Patient Moderate Generalized Anxiety = Dist’ Constraint frustration • Moderate Disturbances to longer timescale those of minutes to hours, the stabilizing network plasticity in the face of perturbations caused from large alterations of environmental dynamics (i.e., stress). Stress and intense network computational activity perturbs brain network stability resulting in "Constraint Frustration" among neurons and network systems. A connection is considered "frustrated" when the weighted value of connectivity is in discrepancy with the value of neuronal activation. In other words within neuronal ensembles when the value of connection weights are incompatible with that of values of neuronal activation. The emergent property of that condition manifests as anxious sensation. Any increase of computational demand on the neuronal network can cause frustration to constraints, obviously connectivity imbalances cause frustration to constraints but also optimization shifts and abrupt stimulus can generate such frustrations of constraints. Here increase of computational demand generates Anxiety (as emergent property). When validated by signal processing of brain-imaging it is expected to find slightly reduced Correlation-matrixes, slight disconnection in graph-analysis, minimal increase error predictions in Dynamic-Causal-Modeling. Slight Increase in entropy-measurements (Free Energy). Slight resting-state-networks disconnected when activated all operating over timescales of minutes and hours
- 54. Mild Depression = Atrophy and De-optimization • Mild Disturbance to “Adaptive Plasticity” slower time-scales, those that span hours to weeks and are responsible for reducing free energy the differences between internal representations (emergent constructs) and external environmental occurrences. Deoptimization takes place when free energy increases and mismatch between internal representations and external events becomes larger. Deopitmization dynamics caused by reduced neuronal plasticity, emerging (Emergent Property) as depressed mood. Normally the brain continually updates internal representations (error-prediction and correction); these are internal representations of the world of our experiences built from memories of past familiarities. The experience continually updates the internal formations to match what is transpiring, this process of update reduces inconsistencies (Free Energy) and is called “optimization,” because it optimizes internal representations to match real life events and occurrences, when neural plasticity is hampered the optimization process is disturbed and De-optimization dynamics takes over. Mismatch between internal configurations and actual occurrences transpire, with depressed mood as a consequent emergent property • When validated by signal processing of brain-imaging it is expected to find reduced dynamics of Correlation-matrixes compared over long time scales of months, the same in graph-analysis over long time scales of months, increase error predictions (free energy) in Dynamic-Causal-Modeling over long time scales of months. The same with increase of entropy-measurements (Free Energy) over long time scales of months
- 55. June 12th, 2019 After 6th ECT session
- 56. Computational Psychiatry Plasticity Diagnosis of the Patient Generalized Anxiety (Mild) = Dist’ Constraint frustration • Check for possible generalized anxiety syndrome Slight Instability of brain systems (reactive plasticity) cause somewhat mild anxiety. Follow- up if anxiety meds are required Depression (Mild) = Atrophy and De-optimization • Check for possible depressive syndrome Mild decrease in brain plasticity (adaptive plasticity) (i.e., growth dynamics of brain- cells) cause somewhat mild depression Follow-up if medications for depression are required
- 57. Explanation of Computational Psychiatry Diagnosis of the Patient Mild Generalized Anxiety = Dist’ Constraint frustration • Mild Disturbances to longer timescale those of minutes to hours, the stabilizing network plasticity in the face of perturbations caused from large alterations of environmental dynamics (i.e., stress). Stress and intense network computational activity perturbs brain network stability resulting in "Constraint Frustration" among neurons and network systems. A connection is considered "frustrated" when the weighted value of connectivity is in discrepancy with the value of neuronal activation. In other words within neuronal ensembles when the value of connection weights are incompatible with that of values of neuronal activation. The emergent property of that condition manifests as anxious sensation. Any increase of computational demand on the neuronal network can cause frustration to constraints, obviously connectivity imbalances cause frustration to constraints but also optimization shifts and abrupt stimulus can generate such frustrations of constraints. Here increase of computational demand generates Anxiety (as emergent property). When validated by signal processing of brain-imaging it is expected to find slightly reduced Correlation-matrixes, slight disconnection in graph-analysis, minimal increase error predictions in Dynamic-Causal-Modeling. Slight Increase in entropy-measurements (Free Energy). Slight resting-state-networks disconnected when activated all operating over timescales of minutes and hours
- 58. Mild Depression = Atrophy and De-optimization • Mild Disturbance to “Adaptive Plasticity” slower time-scales, those that span hours to weeks and are responsible for reducing free energy the differences between internal representations (emergent constructs) and external environmental occurrences. Deoptimization takes place when free energy increases and mismatch between internal representations and external events becomes larger. Deopitmization dynamics caused by reduced neuronal plasticity, emerging (Emergent Property) as depressed mood. Normally the brain continually updates internal representations (error-prediction and correction); these are internal representations of the world of our experiences built from memories of past familiarities. The experience continually updates the internal formations to match what is transpiring, this process of update reduces inconsistencies (Free Energy) and is called “optimization,” because it optimizes internal representations to match real life events and occurrences, when neural plasticity is hampered the optimization process is disturbed and De-optimization dynamics takes over. Mismatch between internal configurations and actual occurrences transpire, with depressed mood as a consequent emergent property • When validated by signal processing of brain-imaging it is expected to find reduced dynamics of Correlation-matrixes compared over long time scales of months, the same in graph-analysis over long time scales of months, increase error predictions (free energy) in Dynamic-Causal-Modeling over long time scales of months. The same with increase of entropy-measurements (Free Energy) over long time scales of months
- 59. June 24th, 2019 Before last -10th - ECT session
- 61. For any inquiry please contact me at mhassan28@hamad.qa mohammdhmohasan@gmail.com
























![Significant physical findings on examination
• Physical Examination: Essentially unremarkable, except for morbid obesity
– Weight was 137 kgs, BMI was 55
• Labs were grossly normal including complete blood count (CBC), Liver and
Kidney functions, electrolytes, Vit B12 and Folate levels
• However, thyroid functions revealed subclinical hypothyroidism:
TSH 5.58 [Normal range: 0.30-4.2 mIU/L]
FT4 11.9 [Normal range: 11.6-21.9 pmol/L]
• CT Head was essentially unremarkable](https://image.slidesharecdn.com/casepresentation-190722130002/85/Case-presentation-26-320.jpg)


































