Cirrhosis of liver
- 1. CIRRHOSIS OF LIVER PORTAL HYPERTENSION HEPATIC ENCHEPALOPATHY By:aymen haseeb
- 2. Definition of cirrhosis Cirrhosis is derived from Greek word kirros=orange or tawny and osis=condition -WHO definition :a diffuse process characterized by liver necrosis and fibrosis and conversion of normal liver architechture into structurally abnormal nodules that lack normal lobular organisation.
- 4. CAUSES OF LIVER CIRRHOSIS -Infections:post hepatitic cirrhosis(B,D,C). -Toxins:Alcohol. -Cholestatic liver disease:PBC,PSC… -Autoimmune diseases:autoimmune hepatitis. • -Vascular disorders: cardiac cirrhosis,Budd-Chiari syndrome ,Veno occlusive disease -Metabolic and genetic :Wilson disease • ,hemochromatosis,alpha 1- antitrypsin deficiency -Non alcoholic steato hepatitis(NASH). Cryptogenic.
- 5. Pathology of cirrhosis -nodularity(regenerating nodules). • -fibrosis(deposition of dense fibrous septa)- fragmentation of sample. -abnormal liver architecture • -hepatocyte abnormalities:pleomorphism,dysplasia,hyperp lasia • -Gross pathology:irregular surface ,yellowish colour,small,firm
- 6. CirrhosisNormal Nodules surrounded by fibrous tissue HISTOLOGICALIMAGE OFANORMALANDACIRRHOTICLIVER
- 8. PATHOGENESISOFLIVERFIBROSIS Hepatocytes Space of Disse Sinusoidal endothelial cell Hepatic stellate cell Fenestrae Normal Hepatic SInusoid Retinoid droplets
- 9. PATHOGENESISOFLIVERFIBROSIS Alterations in Microvasculature in Cirrhosis Activation of stellate cells Collagen deposition in space of Disse Constriction of sinusoids Defenestration of sinusoids
- 10. Compensated cirrhosis Decompensated cirrhosis Death Chronic liver disease Natural History of Chronic Liver Disease o c Development f omplications: Variceal hemorrhage Ascites Encephalopathy Jaundice NATURALHISTORYOFCHRONICLIVERDISEASE
- 11. CLINICAL FEATURES • • • • • • • • • Hepatomegaly (although liver may also be small) Jaundice Ascites Circulatory changes • Spider telangiectasia, palmar erythema, cyanosis Endocrine changes • Loss of libido, hair loss • Men: gynaecomastia, testicular atrophy, impotence • Women: breast atrophy, irregular menses, amenorrhoea Haemorrhagic tendency • Bruises, purpura, epistaxis, menorrhagia Portal hypertension • Splenomegaly, collateral vessels, variceal bleeding, fetor hepaticus Hepatic (portosystemic) encephalopathy Other features • Pigmentation, digital clubbing
- 12. Liver insufficiency Variceal hemorrhage Complications of Cirrhosis Result from Portal Hypertension or Liver Insufficiency Cirrhosis Ascites Portal hypertension Spontaneous bacterial peritonitis Hepatorenal syndrome Encephalopathy Jaundice COMPLICATIONSOFCIRRHOSIS
- 14. In Whom Should We Suspect Cirrhosis? Any patient with chronic liver disease • Chronic abnormal aminotransferases and/or alkaline phosphatase Physical exam findings • Stigmata of chronic liver disease (muscle wasting, vascular spiders, palmar erythema) • Palpable left lobe of the liver • Small liver span • Splenomegaly • Signs of decompensation (jaundice, ascites, asterixis) DIAGNOSISOFCIRRHOSIS– CLINICALFINDINGS
- 15. Laboratory • Liver insufficiency • Low albumin (< 3.8 g/dL) • Prolonged prothrombin time (INR > 1.3) • High bilirubin (> 1.5 mg/dL) • Portal hypertension • Low platelet count (< 175 x1000/ml) • AST / ALT ratio > 1 In Whom Should We Suspect Cirrhosis? DIAGNOSISOFCIRRHOSIS– LABORATORYSTUDIES
- 17. CT Scan in Cirrhosis Liver with an irregular surface SplenomegalyCollaterals DIAGNOSISOFCIRRHOSIS– CATSCAN
- 18. No Yes Diagnostic Algorithm Patient with chronic liver disease and any of the following: Variceal hemorrhage Ascites Hepatic encephalopathy Liver biopsy not necessary for the diagnosis of cirrhosis Physical findings: Enlarged left hepatic lobe Splenomegaly Stigmata of chronic liver Laboratory findings: Thrombocytopenia Impaired hepatic synthetic function Radiological findings: Small nodular liver Intra-abdominal collaterals Ascites Splenomegaly Colloid shift to spleen and/or bone marrow Yes No disease Yes No Liver biopsy DIAGNOSTICALGORITHM
- 19. Management of cirrhosis -Specific treatment in some pre cirrhotic lesions:wilson disease— Dpenicillamine,,hemochromatosis--- phlebotomy,,antiviral drugs for chronic viral hepatitis -in established cirrhosis---treatment of complications -screening for hepatocellular carcinoma -liver transplantation -maintenance of nutrition
- 20. CHILD-PUGH CLASSIFICATION OF PROGNOSIS IN CIRRHOSIS Score 1 2 3 Encephalopathy None Mild Marked Bilirubin (mg/dl) <2.0 2.0-3.0 >3.0 Albumin (g/dl) >3.5 3.0-3.5 <3.0 Prothrombin time (secondsprolonged) <4 4-6 >6 Ascites None Mild Marked Add the individual scores: <7 =Child'sA 7-9 =Child's B >9 =Child's C
- 21. MELD SCORE MELD = 3.8(SERUM BILIRUBIN –MG/DL)+11.2 IN INR + 9.6 IN SERUM CREATININE – MG/DL+ 6.4
- 22. PORTAL HYPERTENSION Definition:it is an increase in portal venous pressure. -normal portal pressure:5-10mmHg. -portal hypertension;>12mmHg -normal portal blood flow:1-1.5L/minute -- increased resistance to portal blood flow • +hyperdynamic circulation-----formation of porto systemic collaterals that diver blood to systemic circulation bypassing the liver
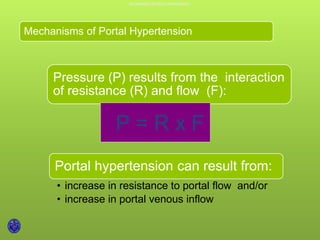
- 23. Mechanisms of Portal Hypertension Pressure (P) results from the interaction of resistance (R) and flow (F): P = R x F Portal hypertension can result from: • increase in resistance to portal flow and/or • increase in portal venous inflow MECHANISMSOFPORTALHYPERTENSION
- 25. Portal systemic collaterals Distorted sinusoidal architecture leads to increased resistance Portal vein Cirrhotic Liver Splenomegaly ARCHITECTURALLIVERDISRUPTIONISTHEMAIN MECHANISMTHATLEADSTOANINCREASEDINTRAHEPATICRESISTANCE
- 26. ANINCREASEIN PORTALVENOUSINFLOWSUSTAINSPORTALHYPERTENSION Mesenteric veins Flow Splanchnic vasodilatation Distorted sinusoidal architechure Portal vein An Increase in Portal Venous Inflow Sustains Portal Hypertension 20
- 27. CAUSES CAUSES OF PORTAL HYPERTENSION ACCORDING TO SITE OF ABNORMALITY • Budd-Chiari syndromeExtrahepatic post-sinusoidal • Veno-occlusive diseaseIntrahepatic post-sinusoidal • CirrhosisSinusoidal • • • Cystic liver disease Partial nodular transformation of the liver Metastatic malignant disease Intrahepatic pre-sinusoidal • Schistosomiasis • Sarcoidosis • Congenital hepatic fibrosis • Vinyl chloride • Drugs Extrahepatic pre-sinusoidal • Portal vein thrombosis due to sepsis* (umbilical, portal pyaemia) or procoagulopathy (thrombotic diseases, oral contraceptives, pregnancy), or secondary to cirrhosis • • • • Abdominal trauma, including surgery Malignant disease of pancreas or liver Pancreatitis Congenital
- 28. Clinical complications of PHT VARICES:esophageal,gastric,anorectal,retroperit oneal. -portal hypertensive gastropathy and colopathy. -caput medusae -ascites -congestive splenomegaly -hepatic encephalopathy
- 29. Small varices Large varicesNo varices 7-8%/year 7-8%/year Varices Increase in Diameter Progressively Merli et al. J Hepatol 2003;38:266 VARICESINCREASEIN DIAMETERPROGRESSIVELY
- 30. Predictors of hemorrhage: • Variceal size • Red signs • Child B/C Variceal hemorrhage Varix with red signs PROGNOSTICINDICATORSOFFIRSTVARICEALHEMORRHAGE
- 31. Treatment of portal hypertension -treatment of complications:variceal bleeding,,,ascites… -endoscopic procedures:sclerotherapy +band ligation+prophylactic propranolol
- 32. Treatment of Acute Variceal Hemorrhage General Management: • Iv acess and fluid resuscitation • Do not overtransfuse (hemoglobin ~ 8 g/dL) • Antibiotic prophylaxis Specific therapy: • Pharmacological therapy: terlipressin, somatostatin and analogues, vasopressin + nitroglycerin • Endoscopic therapy: ligation, sclerotherapy • Shunt therapy: TIPS, surgical shunt TREATMENTOFACUTEVARICEALHEMORRHAGE
- 33. Endoscopic Variceal Band Ligation Bleeding controlled in 90% Rebleeding rate 30% Compared with sclerotherapy: • Less rebleeding • Lower mortality • Fewer complications • Fewer treatment sessions ENDOSCOPICVARICEALBANDLIGATION
- 34. Transjugular Intrahepatic Portosystemic Shunt Portal vein Splenic vein Superior mesenteric vein Hepatic vein TIPS THETRANSJUGULARINTRAHEPATICPORTOSYSTEMIC SHUNT
- 35. Management of Uncomplicated Ascites Definition: in Ascites responsive to diuretics the absence of infection and renal dysfunction Sodium restriction • Effective in 10-20% of cases • Predictors of response: mild or moderate ascites, Urine Na excretion > 50 mEq/day Diuretics • Should be spironolactone-based • A progressive schedule (spironolactone à furosemide) requires fewer dose adjustments than a combined therapy (spironolactone + furosemide) MANAGEMENTOFUNCOMPLICATEDASCITES
- 36. Diuretic Therapy Dosage • Spironolactone 100-400 mg/day • Furosemide (40-160 mg/d) for inadequate weight loss or if hyperkalemia develops Increase diuretics if weight loss <1 kg in the first week and < 2 kg/week thereafter Decrease diuretics if weight loss >0.5 kg/day in patients without edema and >1 kg/day in those with edema Side effects • Renal dysfunction, hyponatremia, hyperkalemia, encephalopathy, gynecomastia Management of Uncomplicated Ascites MANAGEMENTOFUNCOMPLICATEDASCITES:DIURETICTHERAPY
- 37. Early Diagnosis of SBP Diagnostic paracentesis: • If symptoms / signs of SBP occur • Unexplained encephalopathy and / or renal dysfunction • At any hospital admission Diagnosis based on ascitic fluid PMN count >250/mm3 Rimola et al., J Hepatol 2000; 32:142 EARLYDIAGNOSISOFSPONTANEOUSBACTERIALPERITONITIS(SBP)
- 38. Treatment of Spontaneous Bacterial Peritonitis Recommended antibiotics for initial empiric therapy • i.v. cefotaxime, amoxicillin-clavulanic acid • oral nofloxacin (uncomplicated SBP) • avoid aminoglycosides Minimum duration: 5 days Re-evaluation if ascitic fluid PMN count has not decreased by at least 25% after 2 days of treatment Rimola et al., J Hepatol 2000; 32:142 TREATMENTOFSPONTANEOUSBACTERIALPERITONITIS(SBP)
- 40. Type C Hepatic Encephalopathy is the Encephalopathy of Cirrhosis Neuropsychiatric complication of cirrhosis Results from spontaneous or surgical / radiological portal-systemic shunt + chronic liver failure Failure to metabolize neurotoxic substances Alterations of astrocyte morphology and function (Alzheimer type II astrocytosis) TYPECHEPATICENCEPHALOPATHYISTHEENCEPHALOPATHYOFCIRRHOSIS
- 41. Stage Mental state 1 Mild confusion: limited attention Neurologic signs Incoordination, tremor, impaired handwritingspan, irritability, inverted sleep pattern 2 Drowsiness, personality changes, Asterixis, ataxia, dysarthria intermittent disorientation 3 Somnolent, gross disorientation, marked confusion, slurred speech Hyperreflexia, muscle rigidity, Babinski sign No response to4 Coma pain, Stages of Hepatic Encephalopathy STAGESOFHEPATICENCEPHALOPATHY
- 42. STAGESOFHEPATICENCEPHALOPATHY Confusion Drowsiness Somnolence 1 2 3 Coma 4 Stage Stages of Hepatic Encephalopathy
- 43. Hepatic Encephalopathy Is A Clinical Diagnosis Clinical findings and history important Ammonia levels are unreliable Ammonia has poor correlation with diagnosis Measurement of ammonia not necessary Number connection test Slow dominant rhythm on EEG HEPATICENCEPHALOPATHYISACLINICALDIAGNOSIS
- 44. Hepatic Encephalopathy Precipitants GI bleedingExcess protein Sedatives / hypnotics TIPS Diuretics Serum K+ Plasma volume Azotemia Temp Infections HEPATICENCEPHALOPATHYPRECIPITANTS
- 45. Hepatic Encephalopathy Pathogenesis Bacterial action Protein load Failure to metabolize NH3 NH3 Shunting GABA-BD receptors Toxins PATHOPHYSIOLOGYOFHEPATICENCEPHALOPATHY
- 47. 2 3 4 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 5 Begin 1 End 25 Number Connection Test (TNimCeTto) complete Sample handwriting Draw a star NUMBERCONNECTIONTEST 70
- 48. Treatment of Hepatic Encephalopathy Identify and treat precipitating factor • Infection • GI hemorrhage • Prerenal azotemia • Sedatives • Constipation Lactulose (adjust to 2-3 bowel movements/day) Protein restriction, short-term (if at all) TREATMENTOFHEPATICENCEPHALOPATHY
- 49. Actions of Lactulose Lactic acid Lactulose Urease-producing bacteria Increase cathartic effect NH3 NH3 Decreased pH NH4 + ACTIONSOFLACTULOSE
- 50. Hepatic Encephalopathy Treatment: Summary Decrease ammonia production in gut: Lactulose Antibiotics Adjustment in dietary protein Increase ammonia fixation in liver: Ornithine aspartate Benzoate Shunt occlusion or reduction HEPATICENCEPHALOPATHY– TREATMENTSUMMARY Flumazeni l
- 51. Thank you