COPD and AE of COPD
- 1. Presentation on COPD & Acute Exacerbation of COPD INTERN DOCTOR SUNIL KUMAR YADAV 13TH BATCH MEDICINE DEPARTMENT NMCTH
- 2. INTRODUCTION COPD refers to chronic, slowly progressive disorder of airway obstruction that is not fully reversible, with little or no variability. It includes chronic bronchitis and emphysema. Chronic Bronchitis A condition associated with excessive mucus production sufficient to cause cough with expectoration on most days of a week for at least 3 months of the year for more than 2 consecutive years. Emphysema Emphysema is defined as the permanent, abnormal distention of the air spaces distal to the terminal bronchiole with destruction of alveolar septa and without obvious fibrosis.
- 4. Etiology of Chronic Bronchitis and Emphysema 1. Cigarette smoking • Cigarette smoking is the most commonly identified factor associated with both chronic bronchitis during life and extent of emphysema at post-mortem. • Prolonged cigarette smoking impairs ciliary movement, inhibits function of alveolar macrophages, and leads to hypertrophy and hyperplasia of mucus-secreting glands. It is probable that smoke also inhibits antiproteases and causes polymorphonuclear leukocytes to release proteolytic enzymes acutely. Inhaled cigarette smoke can produce an acute increase in airways resistance due to vagally mediated, smooth-muscle constriction. 2. Air pollution Air pollution with sulphur dioxide and particulate matter is associated with exacerbations of chronic bronchitis, and the incidence and mortality rates for chronic bronchitis and emphysema is probably higher in heavily industrialized urban areas.
- 5. 3. Occupation: Occupations exposing workers to inorganic or organic dusts, or to noxious gases. 4. Acute respiratory infections 5. Familial and genetic factors 6. α1-Antitrypsin (a1AT) deficiency 7. Cystic fibrosis
- 6. Pathophysiology • The hallmark of chronic bronchitis is hypertrophy of the mucus-producing glands found in the submucosaof large cartilaginous airways. • Quantitation of this anatomic change is based on the ratio of the thickness of the submucosal glands to that of the bronchial wall (Reid's index). • Histologically there is goblet cell hyperplasia, mucosal and submucosal inflammatory cells, edema, peribronchial fibrosis, intraluminal mucus plugs, and increased smooth muscle in small airways. • Inflammation in chronic bronchitis occurs at the alveolar epithelium and differs predominantly eosinophilic inflammation of asthma by the predominance of neutrophils and the peribronchiolar location of fibrotic changes.
- 9. Classification of Emphysema Based on the site of damage: 1. Centri-acinar emphysema: Distension and damage of lung tissue is concentrated around the respiratory bronchioles, whilst the more distal alveolar ducts and alveoli tend to be well preserved. This form of emphysema is extremely common. Cigarette smoking. 2. Pan-acinar emphysema: This is less common. Here, distension and destruction appear to involve the whole of the acinus, and in the extreme form the lung becomes a mass of bullae. This type of emphysema occurs in alpha1-antitrypsin deficiency. 3. Irregular emphysema: There is scarring and damage affecting the lung parenchyma patchily without particular regard for acinar structure .
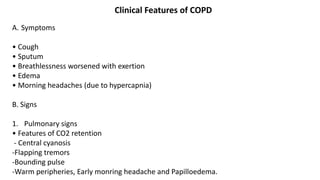
- 12. Clinical Features of COPD A. Symptoms • Cough • Sputum • Breathlessness worsened with exertion • Edema • Morning headaches (due to hypercapnia) B. Signs 1. Pulmonary signs • Features of CO2 retention - Central cyanosis -Flapping tremors -Bounding pulse -Warm peripheries, Early monring headache and Papilloedema.
- 13. • Features of Cor pulmonale (RVF+ Pulmonary HTN) -Peripheral edema -Raised JVP -Right ventricular heave -Loud P2 -Enlarged liver (hepatomegaly) 2. Extra pulmonary signs • Altered fat metabolism contributing to weight loss , and Muscular weakness reflecting deconditioning and cellular changes in skeletal muscles. • Increased prevalence of osteoporosis, and Increased circulating inflammatory markers. • Impaired salt and water excretion leading to peripheral oedema.
- 15. Diagnostic Tests 1. Chest X-ray: Best initial test. • Increased anterior-posterior (AP diameter) • Hyperinflation: >6 anterior ribs seen above diaphragm in mid clavicular line, or ≥ 10 Posterior Ribs. • Large central pulmonary arteries, Decreased peripheral vascular markings and Bulla. • Tubular heart shadow • Air trapping and flattened diaphragms 2. Pulmonary function test: Most accurate test Decreased FEV1, decreased FVC, decreased FEV1/FVC ratio (<70%) • Increased TLC because of increased residual volume. • Incomplete improvement with bronchodilators (<12%) • Little or no worsening with methacholine.
- 17. 3. ABG: Acute exacerbations associated with increased PCO2 and hypoxia. Respiratory acidosis may be present. 4. CBC (increased Hb, increased PCV) 5. ECG • Right atrial and ventricular hypertrophy (cor pulmonale) •Poor progression of R wave •Atrial fibrillation or multifocal atrial tachycardia. 6. High resolution (CT scan (HRCT))
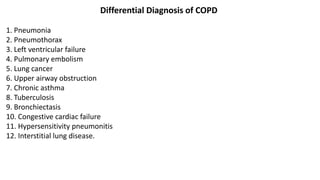
- 19. Differential Diagnosis of COPD 1. Pneumonia 2. Pneumothorax 3. Left ventricular failure 4. Pulmonary embolism 5. Lung cancer 6. Upper airway obstruction 7. Chronic asthma 8. Tuberculosis 9. Bronchiectasis 10. Congestive cardiac failure 11. Hypersensitivity pneumonitis 12. Interstitial lung disease.
- 20. Management 1. Non pharmacological Smoking cessation and oxygen therapy are the only treatment modalities that delay the progression of disease and improve mortality. • Smoking cessation • Use of domiciliary oxygen (at least 15 hours/day) Criteria for domiciliary oxygen use in COPD - --PaO2 <55mmHg or SaO2 <88% -or- -If there are signs of right sided heart failure/disease or hematocrit >55%, use when - PaO2 <60mmHg or SaO2 <90% •Influenza and pneumococcal vaccination -Influenza vaccine annually -Pneumococcal vaccine once (Give only one lifetime booster if the patient was <65 years age at first vaccination) • Encourage exercise • Treatment of poor nutrition and obesity • Pulmonary rehabilitation
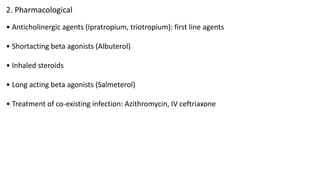
- 21. 2. Pharmacological • Anticholinergic agents (Ipratropium, triotropium): first line agents • Shortacting beta agonists (Albuterol) • Inhaled steroids • Long acting beta agonists (Salmeterol) • Treatment of co-existing infection: Azithromycin, IV ceftriaxone
- 22. 3. Surgery Lung volume reduction surgeries are done in selected patients such pulmonectomy. lobectomy. Indications for surgery are: • Recurrent pneumothoraces • Isolated bullous disease Prognosis COPD has a variable natural history but is usually pro- gressive. The prognosis is inversely related to age and directly related to the post-bronchodilator FEV1. Other poor prognostic indicators include weight loss and pul-monary hypertension. A composite comprising the body mass index (B), the degree of airflow obstruction(O), a measurement of dyspnoea (D) and exercise capacity (E) may assist in predicting death from respiratory and other causes (Box 19.33). Respiratory failure, cardiac disease and lung cancer represent common modes of death.
- 25. Acute Exacerbation of copd Characterised by 1. increased Symptoms. 2. deterioration in lungs function 3. Health Status if ds. Progress then become More frequent; Are usually triggerded by 1. Bacteria 2. virus 3. change in Air quality ↓ Finally may lead to 1. Development of Respiratory failure 2. fluid Retention 3. Important case of Death.
- 26. Refferal to Hospital 1. presence of cynosis 2. peripheral Edema 3. Alternation in consciousness.
- 27. Difference between Blue bloaters and Pink puffers
- 28. Management of Acute Exacerbation of COPD Note: Management of AE-COPD is similar to that of acute asthma, as both are type Il respiratory failure, except the oxygen flow is low in AE COPD. Investigation 1. Pulmonary function test → FEV., peak flow 2. ABG 3. ECG 4. Chest x-ray 5. Sputum for culture. 6. CBC 7. Urine R/E 8. Electrolytes, urea/creatinine.
- 29. Treatment 1. Oxygen • 24-28% via face mask, 2L/min by nasal prongs. • Check ABG within 60 mins and adjust according to PaCO2 or pH. •Keep Pa02 ≥ 7.5 KPa • May require ventilation in coma, respiratory arrest. Note: O2 supply should be low flow because in COPD patients, hypoxia is the stimulus for respiration instead of hypercarbia in normal people, so removal of hypoxia by high flow results in cessation of respiration. 2. Nebulization • Short acting B2 agonists (salbutomol) 5mg in 2-4 ml NS. • 1st dose in 30 min. Repeat of necessary in 2-4 hours. • Add ipratropium bromide if response is inadequate 0.5mg 4 hourly.
- 30. 3. Corticosteroids • IV hydrocortisone 200mg 6 hourly • If oral intake possible, oral predisolone (30-60mg) 1mg/kg tapered over 1 week. 4. Monitoring • Oxygen • Serum potassium 5. Hydration • IV fluids • K+ supplementation may be needed as repeated doses of salbutamol can lower plasma K+. 6. Appropriates antibiotics • If patient fails to improve
- 31. 7. Add IV MgSO4 1.2-2g over 20 mins or, • IV aminophylline 5mg/kg loading dose and 1mg/kg/hr maintainance dose over 20 minutes or • Inj. adrenaline SC 0.3mg x ⅟ 2 hourly * 3 doses. 8. Monitoring of vitals and electrolytes. 9. Others • Diuretics, if JVP elevated and oedema present • If patient continues to deteriorate, respiratory stimulant like doxapram can be considered. • Prophylactic subcutaneous low molecular weight heparin, for DIC.
- 32. Complications of COPD 1. Cor-pulmonale 2. Acute exacerbation 3. Respiratory failure 4. Pneumothorax 5. Mental status deterioration 6. Osteoporosis 7. Renal failure
- 33. THANK YOU