Diabetes in pregnancy Part 1 introduction and screening
- 1. Diabetes in pregnancy Presenter – Dr. Sujita Shrestha 1st year resident OBGYN
- 2. Diagnosis of GDM • Can be done on the basis of 2 or more positive values in 100gm 3 hour OGTT. • Also suggest one step screening and diagnostic test outlined in IADPSG guidelines. • Women with previous GDM should be offered OGTT at 16-18 weeks and further repeat testing at 24-28 weeks williams obstetrics 26th ed
- 3. 100 gm oral glucose tolerance test TIME NDDG Carpenter & Coustan (mg/dl) (mmol/l) (mg/dl) (mmol/l) Fasting 105 5.8 95 5.3 1Hr 190 10.6 180 10 2 Hr 165 9.2 155 8.6 3Hr 145 8.0 140 7.8 williams obstetrics 26th ed
- 4. 75mg OGTT by IADPSG and ADA Plasma glucose Glucose concentration(mg/dl) Threshold(mmol/l) Fasting 92 5.1 1 hr 180 10 2 hr 153 8.5 williams obstetrics 26th ed
- 5. WHO criteria for diagnosis of GDM • Fasting blood glucose >= 126mg/dl • 2 hour blood glucose >140mg/dl williams obstetrics 26th ed
- 6. DIPSI (Diabetes in pregnancy study group India) • Single step diagnostic procedure • 75gm glucose load orally irrespective of fasting status or timing of previous meal • Post 2 hr glucose values- >=140mg/dl diagnose GDM Arias high risk pregnancy
- 7. Advantages of DIPSI • Both a screening as well as diagnostic procedure • No need of fasting and can be performed at first visit • Can be repeated at 2nd and 3rd trimester • Hardly affects daily routine of women Arias high risk pregnancy
- 8. Diagnosis of overt diabetes (ADA) Measure of glycemia Threshold(mg/dl) (mmol/l) Fasting plasma glucose 126 7 HbA1C 6.5 Random plasma glucose 200 11.1 williams obstetrics 26th ed
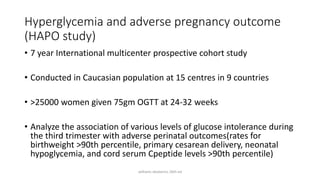
- 9. Hyperglycemia and adverse pregnancy outcome (HAPO study) • 7 year International multicenter prospective cohort study • Conducted in Caucasian population at 15 centres in 9 countries • >25000 women given 75gm OGTT at 24-32 weeks • Analyze the association of various levels of glucose intolerance during the third trimester with adverse perinatal outcomes(rates for birthweight >90th percentile, primary cesarean delivery, neonatal hypoglycemia, and cord serum Cpeptide levels >90th percentile) williams obstetrics 26th ed
- 10. williams obstetrics 26th ed
- 11. Outline for GDM management • Patient education • Medical nutrition therapy • Pharmacological therapy • Glycemic monitoring • Fetal monitoring • Planning on delivery • Postpartum care
- 12. Medical nutrition therapy Goal – • Adequate nutrition • Adequate weight gain • Prevention of ketosis • Prevention of postprandial hyperglycemia Nutrition plan • Calorie allotment • Calorie distribution williams obstetrics 26th ed
- 13. Calorie allotment • BMI 25kg/m2 – 3000 cal/day • Overweight (BMI 25–30kg/m2) – 2500 cal/day • Morbid obesity (BMI .40kg/m2) – 1250 cal/day • Total calorie requirement should consist of 40% carbohydrate, 20% protein and 40% fat (mainly unsaturated fats) • Total caloric intake should be divided into three meals and three snacks per day spaced 2 to 3 hours apart williams obstetrics 26th ed
- 14. • Foods with low glycemic index (e.g., complex carbohydrates with high fiber content) are preferable because this results in a slower rise in glucose levels after ingestion. • Adding protein to all meals and snacks generally helps stabilize glycemic control. • Weight management should be individualized in consultation with a registered dietician. • Patients should be encouraged to keep a daily record of dietary intake. manual of obstetrics
- 15. Physical activity • Physical activity is a major determinant of glycemic control and insulin requirement. • Around 30 minutes of mild to moderate exercise daily helps in improving glycemic control williams obstetrics 26th ed
- 16. Blood glucose monitoring ACOG & ADA recommend glucose assessment four times daily Self monitoring of blood glucose- • Timing of SMBG must be individualized, but postprandial values have the strongest correlation with fetal growth • Frequency of monitoring- at least seven times per day initially in GDM -Daily SMBG at fasting, preprandial 1 to 2 hours after the start of each meal, and before the bedtime snack williams obstetrics 26th ed
- 17. Target goals for glycemic control with SMBG should be established in order to optimize perinatal outcome Pre prandial glucose levels of 70 to 100mg/dL Peak 2-hour postprandial values of 100 to 120 mg/dL Mean daily glucose concentrations <110 mg/dL williams obstetrics 26th ed
- 18. Glycemic targets • Fasting plasma glucose- <95mg/dl and either • 1 hour post-prandial glucose- < 140mg/dl, or • 2 hour post prandial glucose- <120mg/dl • HBA1C < 6 • Continuous glucose monitoring in addition to SMBG- reduce macrosomia and neonatal hypoglycemia in type 1 diabetes williams obstetrics 26th ed
- 19. Insulin therapy • Standard therapy – first line agent • Doesn’t cross placenta • Tight glycemic control achieved
- 20. Commonly Prescribed Insulins during Pregnancy Manual of obstetrics by Evans
- 21. Dose adjustment • Starting insulin dose - 0.7 to 1.0 U/kg/d given in divided doses • 2/3rd in the morning and 1/3rd at night • combination of intermediate-acting and short-acting insulin used • dose adjustments are based on glucose levels at particular times of the day williams obstetrics 26th ed
- 22. • Morning dose - 2⁄3 NPH & 1⁄3 short acting; • Predinner dose - 1⁄2 NPH & 1⁄2 short acting • Side effects- hypoglycemia, pain at injection site, infection, lipodystrophy williams obstetrics 26th ed
- 23. Calculating Split-Dose Weight-Based Insulin Manual of obstetrics by evans
- 24. Split-Dose Pathway manual of obstetrics by Evans
- 25. Basal–Bolus Pathway manual of obstetrics by Evans
- 26. Insulin adjustment guidelines • Manipulation of caloric intake, meal plan, schedule for meals/snacks, or changes in injection site may obviate the need for altering the insulin dosage • The goal is to first achieve normal fasting values and then focus on the rest of the glucose profile • Fasting hyperglycemia may result from inadequate levels of insulin to cover the caloric intake from the previous night, the Somogyi effect, or the dawn phenomenon
- 27. • If a postprandial glucose is elevated greater than 120 mg/dL despite a normal preprandial glucose level, the premeal rapid-acting insulin dose should be increased by 10% to 20%.
- 28. Oral hypoglycemic agent • ACOG recognizes Metformin and glyburide as reasonable choices for second-line glycemic control • The safety and effectiveness of oral agent therapy as an alternative to insulin in women with GDM failing nutrition therapy have not yet been confirmed • However, are widely used in clinical practice
- 29. OHA Classification USMLE first aid
- 30. USMLE first aid
- 31. Metformin MOA- increase insulin sensitivity -stimulation of glucose uptake by peripheral tissues -inhibit hepatic gluconeogenesis -Decrease carbohydrate absorption from intestines • Crosses placental barrier • More convenient, less expensive • Patient compliance is better
- 32. • Reduce PIH, weight gain, neonatal hypoglycemia, NICU admission • Pregnancy category – B • Given with meal • Not FDA approved to use on pregnancy Side effects- GI upset, metallic taste, lactic acidosis, bloating, indigestion
- 33. Glyburide • Class – 2nd generation sulfonylureas • Mechanism of action- binds to ATP sensitive potassium channel in pancreatic beta cells, triggering insulin release • No difference in glycemic control between glyburide and insulin treated group • However higher birth weight, 2 fold higher neonatal hypoglycemia, and fetal macrosomia
- 34. • Side effects- hypoglycemia weight gain hepatotoxicity thrombocytopenia
- 36. Fetal surveillance • An early scan at 11–12 weeks can detect neural tube defects • Nuchal translucency (NT) >3.5mm • Anomaly scan at 18-20 WOG • Fetal echocardiography at around 24 WOG • The American College of Obstetricians and Gynecologists (2020) suggests initiating such testing at 32 to 34 weeks gestation williams obstetrics 26th ed
- 37. • In cases of diabetes complicated with hypertension or restricted fetal growth, an umbilical artery Doppler • The NICE guidelines suggest 4 weekly monitoring of fetal growth from 28–36 weeks • DFMC • Modified biophysical profile weekly williams obstetrics 26th ed
- 38. Intrapartum management When to deliver? With reassuring testing and no other complications, delivery is anticipated between 39(0/7) and 39(6/7) weeks (ACOG) Women on insulin are admitted, glycemic control records are evaluated and insulin doses adjusted, with no other complications planned delivery at 38 weeks Earlier delivery is planned for those with poor glycemic control or significant comorbidities. williams obstetrics 26th ed
- 39. Insulin Management for Labor Induction or Scheduled Cesarean Delivery • Give the evening dose of insulin • Withhold morning dose • Infusion of iv normal saline @ 100-125ml/hr • Regular insulin is infused at 1-1.25units/hr if glucose level is >100mg/dl • Measure glucose level hourly • If glucose level >70mg/dl change from iv normal saline to 50% dextrose @ 100-150ml/hr with target glucose level of nearly 100mg/dl williams obstetrics 26th ed
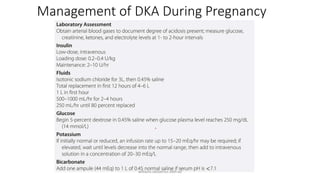
- 40. Management of DKA During Pregnancy williams obstetrics 26th ed
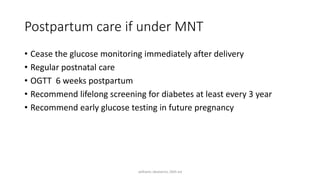
- 41. Postpartum care if under MNT • Cease the glucose monitoring immediately after delivery • Regular postnatal care • OGTT 6 weeks postpartum • Recommend lifelong screening for diabetes at least every 3 year • Recommend early glucose testing in future pregnancy williams obstetrics 26th ed
- 42. Postpartum care if under pharmacological therapy • Cease the medications • Preprandial glucose monitoring QID for 24 hours • If it is between 72-126mg/dl, stop monitoring • If deranged , seek medical review • Some may require to continue OHA’s williams obstetrics 26th ed
- 43. Metabolic assessment recommended after pregnancy with GDM williams obstetrics 26th ed
- 44. Patient counselling • Prophylaxis against infection • Encourage and support breast feeding • Contraception • Education about future risks of diabetes • Follow up
- 45. Breastfeeding • Should be encouraged immediately after delivery to avoid neonatal hypoglycemia • Prevent childhood obesity • Reduce insulin requirement by 25%
- 46. Contraceptives • Barrier • LARC • POP/ DMPA