diffcult airay in obstetrics.ppt
- 1. Difficult airway in obstetrics University of Gondar College of medicine and health science department of anesthesia Misganaw M 1
- 2. INTRODUCTION The difficult airway is a clinical situation which includes either difficulty with mask ventilation or tracheal intubation, laryngoscopic. Obstetric patients are at increased risk of failed tracheal intubation during obstetric GA because of a number of unique clinical situational, situational factors. Difficult or failed intubations will occur, and the only safe way to manage them is to be well prepared . 2
- 3. What is the Incidence of Difficult Intubation, Failed Intubation and pulmonary aspiration in Obstetrics patients? The incidence of failed tracheal intubation in the general surgical population is approximately 1:2200, but the incidence in the obstetric population may be as high as 1:250. 3
- 4. Failed Intubation occurs in approximately 0.13% to 0.35% or 1:750 to 1:280, of obstetric patients versus 1:2,000 for all patients. Incidence of Pulmonary aspiration of gastric contents for obstetric patients is 1:500-400 versus 1:2,000 for all patients. 4
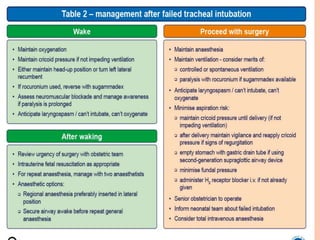
- 5. Failed intubation is an important factor contributing to both maternal and fetal mortality. Ideally we should be able to predict, and plan for, all difficult intubations. However, most airway tests are unreliable so we will inevitably be faced with some unexpectedly difficult or impossible intubations. o The next best option is to have a robust plan for the management of such a situation. 5
- 6. WHY IS OBSTETRIC AIRWAYMANAGEMENT MORE DIFFICULT? Anatomical and Physiological Factors Human Factors 6
- 7. PRACTICAL APPROACH TO OBSTETRIC AIRWAY MANAGEMENT Planning and Preparation for Safe Obstetric GA important components of safe obstetric airway management include adequate and timely airway assessment, fasting status, pharmacologic aspiration prophylaxis, optimal patient positioning, adequate preoxygenation, and provision of a secure airway 7
- 8. AIRWAY ASSESSMENT every woman undergoing obstetric surgery should have a documented airway assessment. This should highlight potential difficulties with tracheal intubation as well as potential difficulties with face mask and supraglottic airway device (SAD) placement and front-of-neck access. Several factors have been identified that may predict airway difficulties in this population 8
- 9. 9
- 10. PULMONARY ASPIRATION RISK REDUCTION Gastric emptying in a nonlabouring pregnant woman is similar to that in a nonpregnant woman; however, gastric emptying is delayed by labour and opioid analgesia. The use of point-of-care ultrasound (US) assessment of gastric contents to individualise the risk of regurgitation in obstetric patients has recently been described 10
- 11. PATIENT POSITIONING A 20 to 30 degree head-up position may facilitate insertion of the laryngoscope, improve the view of the glottis, increase functional residual capacity (FRC), and reduce the risk of gastric regurgitation. 11
- 12. PREOXYGENATION Currently, there is interest in alternative techniques to provide preoxygenation and/or apnoeic oxygenation during tracheal intubation in both nonobstetric and obstetric patients. Insufflation of oxygen at 5 L/min via nasal cannula may prolong the apneic time by maintaining bulk flow of oxygen during intubation attempts. 12
- 13. Cricoid pressure Controversies with the use of CP CP often not correctly applied CP can cause a difficult airway/FI CP may compromise mask ventilation CP effectiveness > 4mins is questionable NAP4 recommended continued use of CP for RSI 13
- 14. ELECTIVE USE OF SADS FOR CAESAREAN SECTION Tracheal intubation following RSI is generally recommended in the obstetric patient. However, there are a number of reports of the elective use of SADs in fasted patients undergoing elective caesarean section. While significant airway-related complications have not been reported in such studies, high-risk women (including those with obesity) were generally excluded . 14
- 15. ILMA /prosealLMA has been used in parturients after failed intubation –Gonzales: Rev Esp Anesthesiol Reanim 2005;52(1):56-57 – M i n i v i l l e A n e s t h A n a l g 2004;99(6):1873 15
- 16. DIRECT AND INDIRECT (VIDEO) LARYNGOSCOPY New disposable intubating laryngoscope Designed to provide a view of the glottis without alignment of oral, pharyngeal, and tracheal axis VL shown to be superior to conventional laryngoscopy 16
- 17. 17
- 18. 18
- 19. 19
- 20. 20
- 21. 21
- 22. 22
- 23. EXTUBATION AND POSTOPERATIVE CARE Focus on airway management must continue until the patient has recovered from GA and is able to maintain their own airway. The anaesthetist should remain vigilant, and the obstetric patient should be extubated awake in the left lateral or head- up position with full reversal of neuromuscular blockade ( 23
- 24. 24