ECMO
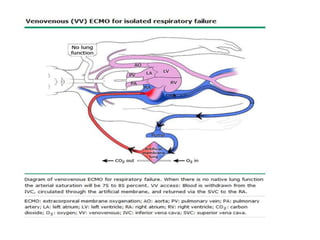
- 2. INTRODUCTION Prolonged cardiopulmonary support is called extracorporeal membrane oxygenation (ECMO), extracorporeal life support, or extracorporeal lung assist. Two types of ECMO 1). Venoarterial (VA) 2). Venovenous (VV). Both provide respiratory support, but only VA ECMO provides hemodynamic support.
- 7. OUTCOMES Survival — can be categorized according to the indication for the ECMO: Acute respiratory failure — survival rates from 50 -71%
- 8. CESAR TRIAL Conventional ventilatory support v/s ECMO for Sev. Acute Resp. failure (CESAR; 2009) trial Randomly assigned 180 pt`s with sev acute resp failure to either ECMO or continued conventional management. ECMO group pt had significantly increased survival without disability at six months compared to conventional management (63 v/s 47%).
- 9. EOLIA TRIAL ECMO to rescue lung injury in severe ARDS (EOLIA; 2018) trial Randomly assigned 249 pts with severe ARDS to receive early VV ECMO or conventional (low-TV, low-pressure) ventilation. ECMO resulted in improved oxygenation, more days free of renal failure (46 v/s 21%), and fewer pt`s with ischemic stroke (0 vs 5%). Study was stopped early by the data safety and monitoring board for interim results that were in favor of ECMO, after the final analysis, the 11 % difference in actual 60-day mortality, while also in favor of early ECMO, was not significant (35 v/s 46%).
- 10. META-ANALYSES One meta-analysis of two randomized trials and three observational studies reported the 60-day mortality rate was lower in pt`s receiving VV ECMO (34 v/s 47%; RR 0.73, 95% CI 0.58-0.92).
- 11. CARDIAC FAILURE VA ECMO can provide acute support in card. shock or cardiac arrest in adults. Observational studies and case series have reported survival rates of 20 – 50% among pt`s who received ECMO for card. arrest, severe card. shock, or failure to wean from CPB following cardiac surgery.
- 12. ELSO registry: 9000 adults who underwent ECMO, 41% survived to hospital discharge with the lowest survival reported in those with cong. heart disease (37 percent). In a systematic review of adults with refractory out of hospital cardiac arrest, survival was 22% in the 833 pts who received ECMO during resuscitation and half of these had good neurological recovery.
- 13. PATIENT SELECTION INDICATIONS — acute sev. cardiac or pulm. failure that is potentially reversible and unresponsive to conventional management. Examples, Hypoxemic respiratory failure, PaO2/FiO2 <100 mmHg despite optimization of the ventilator settings (TV, PEEP, and I:E ratio). The Berlin consensus document on ARDS, ECMO in (PaO2/FiO2 <70). Hypercapnic respiratory failure, pH <7.20. Ventilatory support as a bridge to lung transplantation. Cardiac/circulatory failure/Refractory cardiogenic shock. Massive pulmonary embolism. Cardiac arrest. Failure to wean from CPB after cardiac surgery. As a bridge to either cardiac or lung transplantation or placement of VAD.
- 14. CONTRAINDICATIONS The only absolute CI to ECMO is a pre-existing condition that is incompatible with recovery (sev neurologic injury, end stage malignancy). Relative CI`s : uncontrollable bleeding and very poor prognosis from the primary condition. Results in resp. failure are better when ECMO is instituted early (within seven days of intubation).
- 15. TECHNIQUE ECMO should only be performed by clinicians with training and experience in its initiation, maintenance, and discontinuation.
- 16. ECMO can be venovenous (VV) or venoarterial (VA): During VV ECMO, blood is extracted from the vena cava or RA and returned to the RA. VV ECMO provides resp. support, but the pt is dependent upon his or her own hemodynamics. During VA ECMO, blood is extracted from the RA and returned to the arterial system, by passing the heart and lungs. VA ECMO provides both respiratory and hemodynamic support. The additional benefit of hemodynamic support comes with additional risks.
- 17. INITIATION Pt is anticoagulated (usually with IV heparin) and then the cannulae are inserted. ECMO support is initiated once the cannulae are connected to the appropriate limbs of the ECMO circuit.
- 18. CANNULATION Cannulae are usually placed p/c by Seldinger technique. Largest cannulae that can be placed in the vessels are used. VV ECMO, venous cannulae are usually placed in the right or left CFV (for drainage) and right IJV (for infusion). Tip of the femoral cannula should be maintained near the jn of the IVC & RA, while the tip of the internal jugular cannula should be maintained near the jn of the SVC &RA.
- 19. VA ECMO, a venous cannula is placed in the IVC or RA (for drainage) and an arterial cannula is placed into Rt. FA (for infusion). Femoral access is preferred for VA ECMO bcz insertion is relatively easy. Main drawback of femoral access is ischemia of the I/L lower extremity.
- 20. TITRATION Following cannulation, the pt is connected to the ECMO circuit and the blood flow is increased until resp and hemodynamic parameters are satisfactory. Reasonable targets include: Arterial oxyhemoglobin saturation of >90% for VA ECMO, or >75% for VV ECMO
- 21. MAINTENANCE When the venous oxyhemoglobin saturation is below target, interventions that may be helpful include increasing one or more of the following: blood flow, intravascular volume, or hemoglobin concentration. Decreasing the systemic oxygen uptake by reducing the temp. Unfractionated heparin or direct thrombin inhibitor titrated to an ACT of 180 - 210 sec.
- 22. Platelets are continuously consumed during ECMO bcz they are activated by exposure to the foreign surface area. Platelet counts should be maintained greater than 50,000/microliter, which may require platelet transfusion. ECMO circuit is often the only source of oxygen in pts with complete cardiac or pulmonary failure. Oxygen delivery depends on the amount of Hb and blood flow. Risks of high blood flow outweigh the risk of transfusion, so hemoglobin is maintained over 12 g/dL in ECMO pt`s.
- 23. Ventilator settings are reduced during ECMO in order to avoid barotrauma, volutrauma (ie, ventilator-induced lung injury), and oxygen toxicity. Plateau airway pressures should be maintained <20 cm H2O and FiO2 <0.5. Reduction of ventilator support is usually accompanied by increased venous return, which improves cardiac output.
- 24. SPECIAL CONSIDERATIONS VV ECMO is typically used for resp. failure VA ECMO is used for cardiac failure. Unique considerations for each type of ECMO, which influence management. Blood flow – Near-maximum flow rates are usually desired during VV ECMO to optimize oxygen delivery.
- 25. In contrast, the flow rate used during VA ECMO must be high enough to provide adeq. perfusion pressure and venous oxyhemoglobin saturation but low enough to provide sufficient preload to maintain LV output. Diuresis – Since most pts are fluid overloaded when ECMO is initiated, aggressive diuresis is warranted once the pt is stable on ECMO. Ultrafiltration can be easily added to the ECMO circuit if pts are unable to produce sufficient urine for diuresis.
- 26. Left ventricular monitoring –LV output must be rigorously monitored during VA ECMO because LV output may worsen. Cause is usually multifactorial, including the underlying LV dysfunction and insufficient unloading of the distended LV due to ongoing blood flow to the LV from the bronchial circulation and RV. IABP to reduce afterload and facilitate LV output. LV decompression is essential to avoid pulmonary haemorrhage if LV ejection cannot be maintained despite IABP counter pulsation and inotropic agents. Methods of P/C LV decompression include transatrial balloon septostomy or insertion of a LA or ventricular drainage catheter.
- 27. Weaning from ECMO For pt`s with respiratory failure-: improvements in radiographic appearance, pulmonary compliance, and arterial oxyhemoglobin saturation indicate that the pt may be ready to be liberated from ECMO. For pt`s with cardiac failure- : enhanced aortic pulsatility correlates with improved LV output and indicates that the pt may be ready to be liberated from ECMO.
- 28. COMPLICATIONS • The major complications are bleeding and thromboembolism. Bleeding — 30 - 50 % of pt`s who receive ECMO and can be life-threatening . It is due to both the continuous anticoagulation and platelet dysfunction. Intervention is necessary when major bleeding occurs. Bleeding from surgical wounds often requires prompt exploration with liberal use of electrocautery.
- 29. Plasminogen inhibitors (eg, aminocaproic acid) can be infused or heparin can be discontinued for several hours- but may increase the risk of circuit thrombosis. Infusion of activated factor VII has been reported with mixed results and should only be considered for life- threatening hemorrhage after all other options have failed. Target ACT is usually reduced once bleeding occurs and infusions of anticoagulant are reduced or held. With modern devices the anticoagulation can be stopped altogether for days if bleeding is a problem. Recombinant factor VIIa has been administered to some cases of refractory bleeding. Eur J Cardiothorac Surg. 2016 Jan;49(1):78-84. Epub 2015 Apr 23
- 30. THROMBOEMBOLISM Systemic thromboembolism due to thrombus formation within the ECMO circuit Pulmonary embolism as high as 16%. A CT Scan Study. Crit Care Med 2020; 48:192. DVT may be higher (up to 70%) and may be associated with cannulation, especially femoro femoral cannulae. Its impact is greater with (VA) ECMO than (VV) ECMO bcz infusion is into the systemic circulation. Anticoagulation - target ACT, vigilant observation of the circuit for signs of clot formation.
- 31. NEUROLOGICAL —Incidence of neurologic injury ELSO registry is 10% (adult resp pt). In those with card. failure and those in whom ECMO is administered during CPR = 50% Arch Neurol 2011; 68:1543. CANNULATION-RELATED — Vessel perforation with hemorrhage, arterial dissection, distal ischemia, and incorrect location (eg, venous cannula within the artery). These complications are rare (<5%). HEPARIN-INDUCED THROMBOCYTOPENIA —HIT can occur in pt`s receiving ECMO. When HIT is proven, the heparin infusion should be replaced by a non-heparin anticoagulant. e.g argatroban bcz its half-life is short and a similar ACT target range is effective.
- 32. VA ECMO-specific complications PULMONARY HEMORRHAGE – Pulm. edema and h`ge can occur in pt`s who have no LV emptying during VA ECMO. Edema occurs when LA pr. >25 mmHg. It is treated by venting the LA or LV. CARDIAC THROMBOSIS – There is retrograde blood flow in the asc.aorta whenever the femoral artery and vein are used for VA ECMO. Stasis of the blood can occur if LV output is not maintained, which may result in thrombosis.
- 33. NEUROLOGICAL INJURY – approx. 50 %. neurological injury - coma of uncertain cause, encephalopathy, anoxic brain injury, stroke, brain death and myoclonus. These findings may be a consequence of the condition that prompted ECMO, rather than a complication of the ECMO process. Low levels of hemolysis that can occur during VA-ECMO may predispose to nonhemorrhagic stroke.
- 34. CORONARY OR CEREBRAL HYPOXIA During VA ECMO, fully saturated blood infused into the FA from the ECMO circuit will preferentially perfuse the lower extremities and the abdominal viscera. Blood ejected from the heart will selectively perfuse the heart, brain, and upper extremities. As a result, the oxyhemoglobin saturation of the blood perfusing the lower extremities and abdominal viscera may be substantially higher than that perfusing the heart, brain, and upper extremities. Cardiac and cerebral hypoxia could exist and be unrecognized if oxygenation is monitored using only blood from the lower extremity. To avoid this complication, arterial oxyhemoglobin saturation should be monitored in the right upper extremity. Poor arterial oxyhemoglobin saturation measured from the upper extremity is corrected by infusing some oxygenated blood into the right atrium (called VA-V access).
Editor's Notes
- #3: Mechanical cardiopulmonary support is most often applied intra operatively to facilitate cardiac surgery (ie, cardiopulmonary bypass). However, cardiopulmonary support can also be delivered in a more prolonged fashion in an intensive care unit, although it is less common.
- #12: cardiopulmonary bypass = CPB
- #13: extracorporeal life support organization =ESLO
- #14: cardiopulmonary bypass =CPB,, ventricular assist device=VAD
- #15: Contraindication=CI
- #17: right atrium =RA
- #19: common femoral vein =CFVAlternatively, a double lumen cannula is available that is large enough to accommodate 4 to 5 L/min of blood flow. It is available in a variety of sizes, with 31 French being the largest and most appropriate for adult males. The drainage and infusion ports have been engineered to minimize recirculation.
- #20: I/L= IPSILATERAL,, The likelihood of this complication can be decreased by inserting an additional arterial cannula distal to the femoral artery cannula and redirecting a portion of the infused blood to the additional cannula for "reperfusion" of the extremity.
- #21: Venous oxyhemoglobin saturation 20 - 25 % lower than the arterial saturation, measured on the venous line Adequate tissue perfusion, as determined by the arterial blood pressure, venous oxygen saturation, and blood lactate level
- #22: If AT3 deficiency is suspected, the level can be measured. If less than 50 percent normal, AT3 is replaced by fresh frozen plasma.
- #24: Early tracheostomy to reduce dead space and improve pt comfort.
- #27: LV output can be closely monitored by identifying pulsatility in the arterial line's waveform and by frequent echocardiography. Interventions that can improve LV output include inotropes (eg, dobutamine, milrinone) to increase contractility and
- #29: activated clotting time
- #30: As an example, the target ACT may become 170 - 190 seconds, instead of 210 - 230 sec.
- #31: deep venous thrombosis ,, venoarterial,, venovenousObservation of the circuit for signs of clot formation includes routine inspection of all connectors and monitoring the pressure gradient across the oxygenator. A sudden change in the pressure gradient suggests that a thrombus had developed. Large or mobile clots require immediate circuit or component exchange. Primed circuits are usually kept at the bedside if the target ACT has been reduced due to bleeding bcz the risk of thrombus formation is greatest in this situation. Having a primed circuit available facilitates urgent exchange, if necessary.
- #32: Extracorporeal Life Support Organization
- #35: femoral artery =FA