fluids.ppt
- 1. Fluids and Electrolytes Ahmed Mayet, Pharm.D., BCPS Associate Professor KSU
- 2. Learning Objectives Total Body Fluid Intravascular Volume Depletion Fluid resuscitation vs. Maintenance IV Fluid Osmolarity of IV Fluids Hyponatremia Hypernatremia Hypokalemia Hyperkalemia Hypomagnesemia Hpermagmesemia
- 3. Hypophosphatemia Hyperphosphatemia Hypocalcemia Hypercalcermia
- 4. Fluids Body weight of adult male 55-60% Female 50-55% Newborn 75-80% Very little in adipose tissues Loss of 20% - fatal Elderly - decreases to 45-50% of body weight Decreased muscle mass, smaller fat stores, and decrease in body fluids 4
- 6. Compartments Intracellular (ICF) Fluid within the cells themselves 2/3 of body fluid Located primarily in skeletal muscle mass High in K, Po4, protein Moderate levels of Mg 6
- 7. Compartments Extracellular (ECF) 1/3 of body fluid Comprised of 3 major components Intravascular Plasma Interstitial Fluid in and around tissues Transcellular Over or across the cells 7
- 8. Compartments Extracellular Nutrients for cell functioning Na Ca Cl Glucose Fatty acids Amino Acids 8
- 9. Compartments Intravascular Component Plasma fluid portion of blood Made of: water plasma proteins small amount of other substances 9
- 10. Compartments Interstitial component Made up of fluid between cells Surrounds cells Transport medium for nutrients, gases, waste products and other substances between blood and body cells Back-up fluid reservoir 10
- 11. Compartments Transcellular component 1% of ECF Located in joints, connective tissue, bones, body cavities, CSF, and other tissues Potential to increase significantly in abnormal conditions 11
- 12. Body Fluid Compartments: ICF: 28L Intravascular plasma 5.6L Extravascular Interstitial Fluid 8.4L TBW ECF 3/4 1/4 Male 60% of LBW is fluid female 50% of LBW is fluid 70 kg male BW x 0.6 = TBW 70kg x 0.6 = 42 L ICF= 2/3 x 42 = 28L ECF= 1/3 x 42 = 14L ECF 1/4 is intravascular plasma 1/4 x 14 = 5.6L 3/4 is interstitial 3/4 x 14 = 8.4L 2/3 1/3
- 13. Water Steady State Amount Ingested = Amount Eliminated • Pathological losses vascular bleeding (H20, Na+) vomiting (H20, H+) diarrhea (H20, HCO3-).
- 14. Fluid Requirement The average adult requires approximately 35- 45 ml/kg/d NRC* recommends 1 to 2 ml of water for each kcal of energy expenditure *NRC= National research council
- 15. Fluid Requirement 1st 10 kilogram 100 cc/kg 2nd 10 kilogram 50 cc/kg Rest of the weight 20 to 30 cc/kg Example: 50 kg patient 1st 10 kg x 100cc = 1000 cc 2nd 10 kg x 50cc = 500cc Rest 30 kg x 30cc = 900cc total = 2400 cc
- 16. Fluid Fluid needs are altered by the patient's functional cardiac, hepatic, pulmonary, and renal status Fluid needs increase with fever, diarrhea, hemorrhage, surgical drains, and loss of skin integrity like burns, open wounds
- 17. Regulation of Fluids: Response to Decreased volume and Blood pressure
- 18. Regulation of Fluids: Response to increased volume and Blood pressure
- 19. Hypovolemia
- 20. Causes of Hypovolemia Hypovolemia Abnormally low volume of body fluid in intravascular and/or interstitial compartments Causes Vomiting Diarrhea Excess sweating Diabetes insipidus Uncontrolled diabetes mellitus
- 21. Other Causes of Water Loss Fever Burns N-G Suction Fistulas Wound drainage
- 22. Signs and Symptoms Acute weight loss Decreased skin turgor Concentrated urine Weak, rapid pulse Increased capillary filling time Sensations of thirst, weakness, dizziness, muscle cramps
- 23. Signs of Hypovolemia: Diminished skin turgor Dry oral mucus membrane Oliguria - <500ml/day - normal: 0.5~1ml/kg/h Tachycardia (100 beats/min) Hypotension (SBP < 90 mm Hg) Hypoperfusion cyanosis Altered mental status
- 25. Clinical Diagnosis of Hypovolemia: Thorough history taking: poor intake, GI bleeding…etc BUN : Creatinine > 20 : 1 Increased specific gravity Increased hematocrit Electrolytes imbalance Acid-base disorder
- 26. Labs Increased HCT Increased BUN out of proportion to Cr High serum osmolality Increased urine osmolality Increased specific gravity Decreased urine volume, dark color 26
- 27. Complications Reduced cardiac function, organ hypo perfusion and multi-organ failure, renal failure, shock and death.
- 28. Fluid Replacement Crystalloids Normal saline (0.9% NaCl) Dextrose 5% Colloids Albumin 5%, 25% Hetastarch
- 29. Parenteral Fluid Therapy: Crystalloids: (0.9% NaCl) Contain Na, and Cl as the main osmotically active particle do not freely cross into cells but they will distribute evenly in the EC ( IV + IT) Crystalloids: (D5W) D5W - H2O + CO2 Water will distribute in TBW
- 30. Body Fluid Compartments: ICF: 28L Intravascular plasma 5.6L Extravascular Interstitial Fluid 8.4L TBW ECF 3/4 1/4 2/3 1/3 If 1 liter of NS is given, only 250 ml will stay in intravascular. 1000ml x 1/4 = 250 ml (Intravascular) 1000ml x 3/4 = 750 ml (Interstitial) If 1 liter of D5W is given, only about 100 ml will stay in intravascular. 1000ml x 2/3 = 667ml (ICF) 1000ml x 1/3 = 333 ml (ECF) 333 ml x 1/4 = 83 ml (IV) 333 ml x 3/4 = 250 ml (IT)
- 31. Crystalloids: Isotonic crystalloids - Lactated Ringer’s, 0.9% NaCl - only 25% remain intravascularly Hypotonic solutions - D5W - less than 10% remain intra- vascularly, inadequate for fluid resuscitation
- 32. Colloid Solutions: Contain high molecular weight substances too large to cross capillary walls Preparations - Albumin: 5%, 25% - Dextran - Hetastrach
- 33. Body Fluid Compartments: ICF: 28L Intravascular plasma 5.6L Extravascular Interstitial Fluid 8.4L TBW ECF 3/4 1/4 2/3 1/3 If 1 liter of 5% albumin is given, all will stay in intravascular because of its large molecule that will not cross cell membrance. 1000ml x 1 = 1000 ml If 100 ml of 25% albumin is given, it will draw 5 times of its volume in to intravascular compartment. 100ml x 5 = 500 ml
- 34. The Influence of Colloid & Crystalloid on Blood Volume: 1000cc 500cc 500cc 100cc 200 600 1000 NS or Lactated Ringers 5% Albumin 6% Hetastarch 25% Albumin Blood volume Infusion volume
- 35. Fluid Resuscitation Calculate the fluid deficit base on serum sodium level (assume patient Na is 120 mmole/l and patient weight is 70 kg) Fluid deficit = BW x 0.5 ( Avg Na – pt Na ) Na avg = 70 x 0.5 ( 140 – 120) 140 = 5 L
- 36. Fluid Resuscitation Calculate the fluid deficit base on patient actual weight if you know the patient weight before the dehydration then simply subtract patient current weight from patient previous weight Pt wt before dehydration – pt current wt Exp if pt weight was 70 kg before and now pt weight 65 kg then 70 kg – 65 kg = 5 kg equal to 5 L of water loss (s.g for water is 1)
- 37. Fluid Resuscitation Use crystalloids (NS or Lactate Ranger) Colloids is not superior to crystalloids Administer 500-1000 ml/hr bolus(30-60 mins) and then 250-500 ml/hr for 6 to 8 hours and rest of the fluid within 24 hours Maintain IV fluid (D5 ½ NS) until vital signs are normalized and patient is able to take adequate oral fluid
- 38. Regulation of Fluids in Compartments Osmosis Movement of water through a selectively permeable membrane from an area of low solute concentration to a higher concentration until equilibrium occurs Movement occurs until near equal concentration found Passive process 38
- 40. Regulation of Fluids Diffusion Movement of solutes from an area of higher concentration to an area of lower concentration in a solution and/or across a permeable membrane (permeable for that solute) Movement occurs until near equal state Passive process 40
- 42. Osmosis versus Diffusion Osmosis Low to high Water potential Diffusion High to low Movement of particles Both can occur at the same time 42
- 43. Regulation of Fluids Active Transport Allows molecules to move against concentration and osmotic pressure to areas of higher concentration Active process – energy is expended 43
- 44. Active Transport Na / K pump Exchange of Na ions for K ions More Na ions move out of cell More water pulled into cell ECF / ICF balance is maintained 44
- 46. Active Transport Insulin and glucose regulation CHO consumed Blood glucose peaks Pancreas secretes insulin Blood glucose returns to normal 46
- 47. Osmolarity Concentration of body fluids – affects movement of fluid by osmosis Reflects hydration status Measured by serum and urine Solutes measured - mainly urea, glucose, and sodium Measured as solute concentration/L 47
- 48. Osmolarity Serum Osm/L = (serum Na x 2) + BUN/3 + Glucose/18 Serum Osm/L = (serum Na x 2) + BUN + Glucose Normal serum value - 280-300 mOsm/L Serum <240 or >320 is critically abnormal Normal urine Osm – 250 – 900 mOsm / L 48
- 49. Factors that affect Osmolarity Serum Increasing Osm Free water loss Diabetes Insipidus Na overload Hyperglycemia Uremia 49
- 50. Factors that affect Osmolarity Serum Decreasing Osm SIADH Renal failure Diuretic use Adrenal insufficiency 50
- 52. Factors that affect Osmolarity Urine Increasing Osm Fluid volume deficit SIADH Heart Failure Acidosis 52
- 53. Factors that affect Osmolality Urine Decreasing Osm Diabetes Insipidus Fluid volume excess Urine specific gravity Factors affecting urine Osm affect urine specific gravity identically 53
- 54. Fluid Volume Shifts Fluid normally shifts between intracellular and extracellular compartments to maintain equilibrium between spaces Fluid not lost from body but not available for use in either compartment – considered third-space fluid shift (“third-spacing”) Enters serous cavities (transcellular) 54
- 55. Causes of Third-Spacing Burns Peritonitis Bowel obstruction Massive bleeding into joint or cavity Liver or renal failure Lowered plasma proteins Increased capillary permeability Lymphatic blockage 55
- 57. Assessment of Third-Spacing More difficult – fluid sequestered in deeper structures Signs/Symptoms Decreased urine output with adequate intake Increased HR Decreased BP, CVP Increased weight Pitting edema, ascites 57
- 58. Osmolarity Isotonic solution Hypotonic solution Hypertonic solution
- 59. Osmolarity Plasma osmolarity pOsm = Na + Cl + BUN + Glucose exp: if pt Serum Na = 145 mmol/l and Glucose is 6 mmole/l and B BUN is 6 mole/l, then osmolarity of serum is 145 + 145 + 6 + 6 = 302
- 60. Osmolarity Calculate the osmolarity of 1L NS? MW of Na = 23, Cl = 35.5 0.9% NaCL of 1 L 9 gm NaCl 9/23+35.5 = 0.154 mole (154 mmole) 1 mole of NaCl = 1 mole Na + 1 mole CL = 2 154 mmole/l x 2 =308
- 61. Osmolarity Calculate the osmolarity of 1L 3%NaCl? MW of Na = 23, Cl = 35.5 3% NaCL of 1 L 30 gm NaCl 30/23+35.5 = 0.154 mole (513 mmole) 1 mole of NaCl = 1 mole Na + 1 mole CL = 2 513 mmole/l x 2 =1026
- 62. Osmolarity Calculate the osmolarity of 1L D5W? MW of dextrose 180 D5W of 1 L 50 gm dextrose 50/180 = 0.278 mole (278 mmole) 278 mmole/l x 1 =278 mosm/l
- 63. Osmolarity Calculate the osmolarity of D5WNS?
- 65. Osmolarity What happen if you infuse hypotonic solution? RBC will swell and rapture Also will cause brain edema
- 66. Osmolarity What happen if you infuse hypertonic solution to you RBC? RBC will shrink and will not carry oxygen properly
- 67. Solutions Volumes Na+ K+ Ca2+ Mg2+ Cl- HCO3 - Dextrose mOsm/L ECF 142 4 5 103 27 280-310 Lactated Ringer’s 130 4 3 109 28 273 0.9% NaCl 154 154 308 0.45% NaCl 77 77 154 D5W D5/0.45% NaCl 77 77 50 406 3% NaCl 513 513 1026 6% Hetastarch 500 154 154 310 5% Albumin 250,500 130- 160 <2.5 130- 160 330 25% Albumin 20,50,100 130- 160 <2.5 130- 160 330 Common parenteral fluid therapy
- 68. Hypervolemia Excess fluid in the extracellular compartment as a result of fluid or Na retention when compensatory mechanisms fail to restore fluid balance or from renal failure
- 69. Causes Cardiovascular – Heart failure Urinary – Renal failure Hepatic – Liver failure, cirrhosis Other –Drug therapy (i.e., corticosteriods), high sodium intake, protein malnutrition
- 70. Signs/Symptoms Physical assessment Weight gain Distended neck veins Periorbital edema, pitting edema Adventitious lung sounds (mainly crackles) Mental status changes Generalized or dependent edema 71
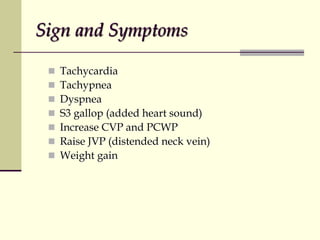
- 71. Sign and Symptoms Tachycardia Tachypnea Dyspnea S3 gallop (added heart sound) Increase CVP and PCWP Raise JVP (distended neck vein) Weight gain
- 72. Lab Abnormalities Lab data ↓ Hct (dilutional) Low serum osmolality Low specific gravity ↓ BUN (dilutional)
- 73. Signs / Sympotms Radiography Pulmonary vascular congestion Pleural effusion Pericardial effusion Ascites 74
- 74. Management Sodium restriction with no more than 2 grams of salt per day Fluid restriction if necessary Diuretic 1. Furosemide dose and route depends on patient condition and underlining diseases
- 75. IV Loop diuretic (Furosemide) Patient with a cute CHF with pulmonary edema and difficult in breathing Patient with a cute or chronic renal failure with massive fluid overload Patient with liver cirrhosis and refractory to oral diuretic (furosemide) Dose can be range from 80-240 mg/day Can be bolus in divided doses or continuous infusion range from 5-10mg/hour
- 76. Monitoring Parameters Fluid intake and output (trying to create at least 1-2 liters of negative fluid balance) Patient weight Monitor the vital sign BP, RR, PR ABG or oxygen saturation Chest auscultation If dyspnea or orthopnea Urea and electrolytes ( make sure that patient does not develop renal impairment or hyponatremia or hypokalemia
- 77. Composition of Body Fluids and electrolytes: Ca+ 2 Mg +2 K+ Na+ Cl- PO4 3- Organic anion HCO3 - Protein 0 50 50 100 150 100 150 Cations Anions ECF ICF
- 78. Sodium Normal 135-145 mEq/L Major cation in ECF Regulates voltage of action potential; transmission of impulses in nerve and muscle fibers Main factors in determining ECF volume Helps maintain acid-base balance
- 80. Hyponatremia Results from excess Na loss or water gain GI losses (vomiting and diarrhea) Diuretic therapy Severe renal dysfunction (ATN) Administration of hypotonic fluid (1/2NS) DKA, HHS Unregulated production of ADH (pneumonia, brain trauma, lung cancer etc) Some drugs (Li, thiazide)
- 81. Sign and Symptoms Clinical manifestations ↓ BP Confusion, nausea, malaise, vomiting Lethargy and headache (115-120 mmol/l) Seizure and coma (110-115 mmol/l) Decreased muscle tone, twitching and tremors Cramps
- 82. Assessment Labs Decreased Na, Cl, Bicarbonate Urine specific gravity ↓ 1.010 Estimated Na deficit (calculation) Na deficit = 0.6 x LBW (140 – patient serum Na) Exp: if patient is 70 kg and his serum Na=120 = 0.6 x 70 (140 – 120) = 42 x 20 = 840 mmole
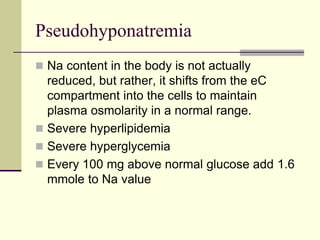
- 83. Pseudohyponatremia Na content in the body is not actually reduced, but rather, it shifts from the eC compartment into the cells to maintain plasma osmolarity in a normal range. Severe hyperlipidemia Severe hyperglycemia Every 100 mg above normal glucose add 1.6 mmole to Na value
- 84. Treatment Interventions If patient is normovolemic or edematous Fluid restriction If patient is intravascular volume depletion IV 0.9% NS or LR Avoid rapid Na correction A change of no more than 10-12 mmole/day Raid correction of Na can cause central pontine myelinolysis and death 120-125 mmole/l is a reasonable goal and safe
- 85. HS should be given through central intravenous access because the osmolarity is greater than 900 mOsm/l.1. Some practitioners use 3% Hs through a peripheral intravenous access site in an emergency situation because the osmolarity is close to the cutoff range for peripheral administration. If a peripheral site is used, monitor for phlebitis and obtain central access as soon as possible.
- 86. Central pontine myelinolysis and death
- 87. Hypertonic Saline 3% NaCl Use in patient with symptomatic hyponatremia such as in seizure, comatose patient, or patient with brain edema 3% NaCl 250ml with an infusion rate of 1-2ml/kg/hr exp; 70 kg patient 70kg x 1ml/kg = 70 ml 250ml/70ml = 3.5 hours
- 88. Complications of HS Central pontine myelinolysis can occur with rapid correction of hyponatremia. Characterized by permanent neurologic damage such as paraparesis, quadriparesis, dysarthria, dysphagia, and coma More likely to occur with rapid correction of chronic hyponatremia compared with acute hyponatremia. Advisable not to administer Hs in patients with chronic asymptomatic
- 89. Complications of HS Prevent by avoiding changes in serum Na of more than 10–12 mmol/l in 24 hours or more than 18 mmol/l in 48 hours. Hypokalemia can occur with large volumes of HS Hyperchloremic acidosis can occur because of the administration of Cl salt Phlebitis if administered in a peripheral vein Heart failure - Fluid overload can occur because of initial volume expansion
- 90. Hypotonic IV fluid Hypotonic fluids administered intravenously can cause cell hemolysis and patient death. Albumin 25% diluted with sterile water to make albumin 5% has an osmolarity of about 60 mOsm/l and can cause hemolysis “Quarter saline” or 0.25% naCl has an osmolarity of 68 mOsm/l and can cause hemolysis.
- 91. Hypotonic IV fluid Avoid using intravenous fluid with an osmolarity less than 150 mOsm/l. Sterile water should never be administered intravenously. Use D5W administered intravenously if only water is needed. Use a combination of D5W and 0.25% NaCl
- 92. Q & A A 55-year-old man is hospitalized for community- acquired pneumonia. After 2 days of appropriate anti- biotic treatment, his WBC has decreased, and he is afebrile. His BP is 135/85 mm Hg, and he has good urine output. His laboratory values are normal. His weight is 80 kg. His appetite is still poor, and he is not taking adequate fluids. Which of the following is the best intravenous fluid and rate?
- 93. Q & A A. 0.9% NaCl + KCl 20 meq/l to infuse at 150 ml/hour. B. D5W/0.9% NaCl + KCl 20 meq/l to infuse at 70 ml/hour. C. D5W/0.45% NaCl + KCl 20 meq/l to infuse at 110 ml/hour. D. 0.9% NaCl 1000-ml fluid bolus. 3
- 94. Q & A A 72-year-old woman with a history of hypertension has developed hyponatremia after starting hydrochlo-rothiazide 3 weeks earlier. She complains of dizziness, fatigue, and nausea. Her serum Na is 116 meq/l. Her weight is 60 kg, her BP is 86/50 mm Hg, and her Hr is 122 beats/minute. Which of the following initial treatment regimens is recommended? A. 0.9% NaCl infused at 100 ml/hour. B. 0.9% NaCl 500-ml bolus. C. 3% NaCl infused at 60 ml/hour. D. 23.4% NaCl 30-ml bolus as needed. 2
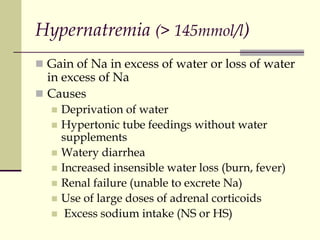
- 95. Hypernatremia (> 145mmol/l) Gain of Na in excess of water or loss of water in excess of Na Causes Deprivation of water Hypertonic tube feedings without water supplements Watery diarrhea Increased insensible water loss (burn, fever) Renal failure (unable to excrete Na) Use of large doses of adrenal corticoids Excess sodium intake (NS or HS)
- 96. Signs/Symptoms Early: Generalized muscle weakness, faintness, muscle fatigue, headache, tachycardia, nausea and vomiting Moderate: Confusion, thirst Late: Edema, restlessness, thirst, hyperreflexia, muscle twitching, irritability, seizures, possible coma (Na > 158 mmol/l) Severe: Permanent brain damage form cerebral dehydration and intracerebral hemorrhage, hypertension (Na > 158 mmol/l)
- 97. Labs Increased serum Na Increased serum osmolality Increased urine specific gravity
- 98. Treatment (Euvolemic with hypernatremia) IV D5W to replace ECF volume if patient is symptomatic with hypernatremia D5W need = 0.4 x LBW (pt serum Na – Na normal) Na exp: patient 70 kg serum Na = 158, normal Na = 135 = 0.4 x 70 (158 – 135) 135 = 4.77 L Gradual lowering with Na level with D5W Decrease by no more than 0.5 mmol/l/hr or 12 mmol/l/day
- 99. Treatment (Euvolemic with hypernatremia) Non- symptomatic patient Orally (plain water) to replace ECF volume if patient is not symptomatic with excessive free water losses
- 100. Treatment (hypovolemic with hypernatremia) Non- symptomatic patient Orally (plain water) to replace ECF volume if patient is not symptomatic with excessive free water losses Symptomatic patient IV D5W to replace ECF volume if patient is symptomatic with hypernatremia
- 101. Treatment (Hyporvolemic with hypernatremia) If hypovolemia is due to osmotic diuretic or gastroenteritis Signs of intravascular depletion Treat with 1/2NS or D5 1/4NS
- 102. Treatment (Hypervolemic with hypernatremia) If patient is hypervolemic with hypernatremia Loop diuretic is the drug of choice
- 103. Evaluation Normalization of serum Na level over days Resolution of symptoms
- 104. Potassium Normal 3.5-5.5 mEq/L Major ICF cation Vital in maintaining normal cardiac and neuromuscular function, influences nerve impulse conduction, important in glucose metabolism, helps maintain acid-base balance, control fluid movement in and out of cells by osmosis
- 105. Hypokalemia Serum potassium level below 3.5 mEq/L Causes Loss of GI secretions (diarrhea) Excessive renal excretion of K Movement of K into the cells with insulin (Rx DKA) Prolonged fluid administration without K supplementation Diuretics (some) and beta agonist (albuterol) Alkalosis
- 106. Hypokalemia Renal excretion –diuretic Increased Gi losses of k+ can occur with vomiting, diarrhea, intestinal fistula or enteral tube drainage, and chronic laxative abuse Asthma treatment salbutamol Hypomagnesemia is commonly associated with hypokalemia caused by increased renal loss of k+
- 107. Signs/Symptoms Skeletal muscle weakness, ↓ smooth muscle function, ↓ respiratory muscle function EKG changes, possible cardiac arrest Paralytic ileus Nausea, vomiting Metabolic alkalosis Mental depression and confusion
- 108. Treatment Deficit can be estimated as 200 -400 mmol K for every 1 mmol/l reduction in plasma K
- 109. Treatment Patients without EKG changes or symptoms of hypokalemia can be treated with oral supplementation.
- 110. Avoid mixing k+ in dextrose, which can cause insulin release with a subsequent IC shift of K+. Use NS Avoid irritation, no more than about 60-80 meq/l should be administered through a peripheral vein. Recommended infusion rate is 10 meq/hour up to a maximum of 40 meq/hour Patients who receive K+ at rates faster than 10–20 meq/hour should be monitored using a continuous EKG.
- 111. Plasma K levels Mmol/l Treatment Comments 3 – 3.5 Oral KCl 60-80 mmol/d if no sign or symptoms Plasma K level rise by about 1.5 mmol/l 2.5 -3 Oral KCl 120 mmol/d or IV 10 -20 mmol/hr if sign or symptoms Plasma K level rise by about 2.0 mmol/l 2 -2.5 IV KCl 10 -20 mmol/hr Consider continous EKG monitoring Less than 2 IV KCl 20 -40 mmol/hr Requires continous EKG monitoring
- 112. Caution Don’t mix K in dextrose No more than K 10 mmol/hr to be infused in general ward If rate exceed more than 10 mmol/hr, then consider EKG monitor
- 113. Monitoring Monitor Potassium level EKG Bowel sounds Muscle strength
- 114. Hyperkalemia Serum potassium level above 5.3 mEq/L Causes Excessive K intake (IV or PO) especially in renal failure CRF Tissue trauma Acidosis Catabolic state ACE inhibitors, K-sparing diuretics, B blockers
- 115. Signs/Symptoms ECG changes – tachycardia to bradycardia to possible cardiac arrest Peaked, narrowed T waves Cardiac arrhythmias (VF Muscle weakness and paralysis Paresthesia of tongue, face, hands, and feet N/V, cramping, diarrhea Metabolic acidosis
- 117. Treatment Asymptomatic elevation of plasma K Use cation exchange resin (calcium or sodium polystyrene sulfonate Kayexalate ) 15- 30 grams 3 to 4 times/day as orally or rectal enema Specially used in chronic renal failure patient with hyperkalemia. Avoid K containing food
- 118. Treatment (symptomatic) Urgent immediate treatment is needed if patient 1. Plasma K+ of 8mmol/l 2. Severe muscle weakness 3. ECK changes 10% Ca gluconate 20ml should be given immediately if a patient has hyperkalemia - induced-arryhymias (2 grams IV bolus)
- 119. Treatment (symptomatic) Sodium bicarbonate 1 mmol/kg can be given if patient has acidosis (pH of < 7) 50% glucose solution 50 ml (25 gm) with 10 units of insulin push K+ intracellular and lower serum K+ level by 1 to 1.5 mmol/l in one hour B2 adrenergic agonist salbutamol 10 -20 mg in NS as nebulizer over 10 mins lower K+ level by 1 to 1.5 mmol/l in one hour to two hours Kayexalate PO or PR Hemodialysis Avoid K in foods, fluids, salt substitutes
- 120. Evaluation Normal serum K values Resolution of symptoms Treat underlying cause if possible
- 121. Calcium Normal 2.25-2.75 mmol/L 99% of Ca in bones, other 1% in ECF and soft tissues ECF Calcium – ½ is bound to protein – levels influenced by serum albumin state Ionized Calcium – used in physiologic activities – crucial for neuromuscular activity
- 122. Calcium Required for blood coagulation, neuromuscular contraction, enzymatic activity, and strength and durability of bones and teeth Nerve cell membranes less excitable with enough calcium Ca absorption and concentration influenced by Vit D, calcitriol (active form of Vitamin D), PTH, calcitonin, serum concentration of Ca and Phos
- 123. PTH
- 124. Causes of Hypocalcemia Hypoparathyroidism (depressed function or surgical removal of the parathyroid gland) Hypomagnesemia Hyperphosphatemia Administration of large quantities of stored blood (preserved with citrate) Renal insufficiency ↓ Absorption of Vitamin D from intestines
- 125. Signs/Symptoms Abdominal and/or extremity cramping Tingling and numbness Positive Chvostek or Trousseau signs Tetany; hyperactive reflexes Irritability, reduced cognitive ability, seizures Prolonged QT on ECG, hypotension, decreased myocardial contractility Abnormal clotting
- 127. Treatment Asymptomatic hypocalcaemia associated with hypoalbuminemia check for corrected Ca++ Corrected Ca = Serum Ca + (normal S albumin – pt serum albumin x 0.02 Exp: if patient serum Ca is 1.8 mmol/l and albumin is 20 gm/l then corrected Ca is (assume Normal Ca is 45 gm/l = 1.8 + (45 – 20) x 0.02 = 1.8 + 25 x 0.02 = 1.8 + 0.5 = 2.3
- 128. Treatment Asymptomatic hypocalcemia Oral calcium salts (mild) – 2 – 4 gm of elemental Ca++/day with Vit D supplementation Symptomatic hypocalcemia IV calcium as 10% calcium chloride 10 ml or 10% calcium gluconate 20ml (270 mg elemental Ca)– give with caution over 5-10 mins followed by continous infusion of Ca at a rate of 0.5 – 2 mg/kg/hr Don’t exceed infusion rate 60 mg/min Close monitor for hypotension and bradycardia Vitamin D supplementation
- 129. Monitoring Close monitoring of serum Ca++ Phosphorus level Magnesium level Vitamin D level Albumin level
- 130. Hypercalcemia Causes Mobilization of Ca from bone Malignancy (non-small cell and small cell lung cancer, breast cancer, lymphomas, renal cell) Hyperparathyroidism Immobilization – causes bone loss Thiazide diuretics and hormonal therapy Thyrotoxicosis Excessive ingestion of Ca or Vit D
- 131. Signs/Symptoms Anorexia, constipation Generalized muscle weakness, lethargy, loss of muscle tone, ataxia Depression, fatigue, confusion, coma Dysrhythmias and heart block Deep bone pain and demineralization Renal calculi Pathologic bone fractures
- 132. Hypercalcemic Crisis Emergency – level of 4-4.5 mmol/L Intractable nausea, dehydration, stupor, coma, azotemia, hypokalemia, hypomagnesemia, hypernatremia High mortality rate from cardiac arrest
- 133. Treatment NS IV infusion 3 – 6 L over 24 hours followed by loop diuretic to prevent over load I and O hourly to avoid over hydration Biphosphonate- pamindronate 60mg IV once (inhibit bone resorption) Corticosteroids (HC 100 q6 hr) and Mithramycin in lymphomas and myeloma patient Calcitonin 2-8 IU/kg IV or SQ q6 to q12 to inhibit PTH effect Phosphorus in patient with hypophosphatemia Encourage fluids Dialysis in renal patient with hypercalcemia
- 134. Evaluation Normal serum calcium levels Improvement of signs and symptoms specially heart block, PVC, tachycardia, mental status
- 135. Magnesium Normal 0.7 to 1.25 mmol/l Important in CHO and protein metabolism Plays significant role in nerve cell conduction Important in transmitting CNS messages and maintaining neuromuscular activity Causes vasodilatation Decreases peripheral vascular resistance
- 136. Hypomagnesemia Causes Decreased intake or decreased absorption or excessive loss through urinary or bowel elimination Acute pancreatitis, starvation, malabsorption syndrome, chronic alcoholism, burns, prolonged hyperalimentation without adequate Mg supplement Hypoparathyroidism with hypocalcemia Diuretic therapy
- 137. Signs/Symptoms Tremors, tetany, ↑ reflexes, paresthesias of feet and legs, convulsions Positive Babinski, Chvostek and Trousseau signs Personality changes with agitation, depression or confusion, hallucinations ECG changes (PVC’S, V-tach and V-fib)
- 139. Treatment Mild Diet – Best sources are unprocessed cereal grains, nuts, green leafy vegetables, dairy products, dried fruits, meat, fish Magnesium salts (MgO 400mg/d) More severe MgSO4 IM MgSO4 IV slowly
- 140. Treatment of Severe Symptomatic Hypomagnesemia Treated with 2gm Mg sulfate (4mmol/ml) IV over 15 min, followed by infusion of 6g Mg sulfate in 1L or more IV fluid over 24hrs or 0.5 meq/kg/day added to intravenous fluid and administered as a continuous infusion. Need to replenish intracellular stores, the infusion should be continued for 3-7 days Serum Mg should be measured q24h and the infusion rate adjusted to maintain a serum Mg level of <1.25 mmol/L Singer G: Fluid and electrolyte management. In: The Washington Manual of Therapeutics. Lippencott. 30th edition, 2001. p68-69.
- 141. Treatment of Severe Symptomatic Hypomagnesemia In patient with normal renal function, excess Mg is readily excreted, and there is little risk of causing hypermagnesemia with recommended doses Mg must be given with extreme caution in renal failure due to the risk of accumulation of Mg and can cause hypermagnesemia
- 142. Monitoring Monitor Mg level q 12 – 24 hrs Monitor VS Knee reflexes Check swallow reflex
- 143. Hypermagnesemia Most common cause is renal failure, especially if taking large amounts of Mg- containing antacids or cathartics DKA with severe water loss Signs and symptoms Hypotension, drowsiness, absent DTRs, respiratory depression, coma, cardiac arrest ECG – Bradycardia, cardiac arrest
- 144. Treatment Withhold Mg-containing products Calcium chloride or gluconate IV for acute symptoms (10% Ca gluconate 10-20ml over 15-30 mins) NS IV hydration and diuretics Hemodialysis
- 145. Evaluation Serum magnesium levels WNL Improvement of symptoms
- 146. Phosphorus Normal 0.8 to 1.6 mmol/l The primary anion in the intracellular fluid Crucial to cell membrane integrity, muscle function, neurologic function and metabolism of carbs, fats and protein Functions in ATP formation, phagocytosis, platelet function and formation of bones and teeth Influenced by parathyroid hormone and has inverse relationship to Calcium
- 147. Hypophosphotemia Causes Malnutrition Hyperparathyroidism Certain renal tubular defects Metabolic acidosis (esp. DKA) Disorders causing hypercalcemia Diuretics, glucocorticoids, na bicarbonate Rapidly refeeding Diabetic ketoacidosis (shift IC)
- 148. Sign and Symptoms Musculoskeletal Muscle weakness Respiratory muscle failure Osteomalacia Pathological fractures CNS Confusion Anxiety Seizures Coma
- 149. Sign and Symptoms Cardiac hypotension decreased cardiac output Hematologic hemolytic anemia easy bruising infection risk
- 150. Treatment Treatment of moderate to severe deficiency IV phosphate Symptomatic patients should receive 15–30 mmol of phosphorus (Na phosphate or K+ phosphate) administered intravenously over 3–6 hours. Oral phosphorus (neutra-Phos) can be used for asymptomatic patients.(15 mmol/d) Monitor levels during treatment
- 151. Hyperphosphatemia Causes Chronic renal failure (most common) Hyperthyroidism, hypoparathyroidism Severe catabolic states Conditions causing hypocalcemia Net effect of PTH ↑ serum calcium ↓ serum phosphate Net effect of calcitriol ↑ serum calcium ↑ serum phosphate
- 152. Role of PTH Stimulates renal reabsorption of calcium Inhibits renal reabsorption of phosphate Stimulates bone resorption Inhibits bone formation and mineralization Stimulates synthesis of calcitriol Net effect of PTH ↑ serum calcium ↓ serum phosphate
- 153. Sign and Symptoms Cardiac irregularities Hyperreflexia Eating poorly Muscle weakness Nausea
- 154. Treatment Prevention is the goal Restrict phosphate-containing foods Administer phosphate-binding agents (Ca carbonate, sevelamar, lanthanum) Diuretics Cinacalcet –increase the sensitivity of Ca receptor on PTH gland to Ca conc PTH Treatment may need to focus on correcting calcium levels
- 155. Evaluation Lab values within normal limits Improvement of symptoms
- 156. Acid-Base Disorders
- 157. Regulation of blood pH The lungs and kidneys play important role in regulating blood pH. The lungs regulate pH through retention (hypoventilation) or elimination (hyperventilation) of CO2 by changing the rate and volume of ventilation. The kidneys regulate pH by excreting acid, primarily in the ammonium ion (NH4 +), and by reclaiming HCO3 - from the glomerular filtrate (and adding it back to the blood).
- 158. Normal Values for Blood Buffer in Arterial Blood. The following values are determined by blood gas analyzer: pH 7.35 – 7.45 PCO2 35 – 45 mm Hg H2CO3 2.4 mmoles/L of plasma HCO3 - 24 mmoles/L of plasma PO2 80 – 110 mm Hg
- 159. Four Basic Types of Imbalance Respiratory Acidosis Respiratory Alkalosis Metabolic Acidosis Metabolic Alkalosis
- 160. Respiratory Acidosis Carbonic acid excess Exhaling of CO2 inhibited Carbonic acid builds up pH falls below 7.35 Cause = Hypoventilation (see chart) When CO2 level rises hypoventilation, producing more H2CO3, the equilibrium produces more H3O+, which lowers the pH – acidosis. CO2 + H2O H2CO3 H3O+ + HCO3 - H2CO3
- 161. Respiratory Acidosis: CO2 ↑ pH ↓ Symptoms: Failure to ventilate, suppression of breathing, disorientation, weakness, coma Causes: Lung disease blocking gas diffusion (e.g., emphysema, pneumonia, bronchitis, and asthma); depression of respiratory center by drugs, cardiopulmonary arrest, stroke, poliomyelitis, or nervous system disorders
- 162. Acid-Base Imbalances Normal H2CO3 ……………… HCO3 24 mEq/L 1.2 mEq/L 7.4 1 20
- 164. Respiratory Acidosis Respiratory acidosis compensates by metabolic alkalosis Compensated by the kidney increasing production of bicarbonate Acute Hypercapnia: HCO3 increases 1 mmol/L for each 10 mmHg increase in PaCO2 >40 Chronic Hypercapnia: For each 10 mmHg increase in PaCO2 >40 HCO3 incr. 3.5 mmol/L
- 166. Acute Respiratory Acidosis: 25 y.o. IV drug user s/p heroin overdose: pH 7.10 pCO2 80 Bicarbonate 24 80 – 40 = 40. For every 10 CO2 inc 3.5 mmol HCO3 increases 10---------------- 3.5 40--------------- ? 40/10 = 4 x 3.5 = 14 24 + 14 = 38 HCO3
- 167. Chronic Respiratory Acidosis: 65 y.o. patient with stable COPD: pH 7.32 pCO2 70 Bicarbonate 35 Significant Renal Compensation But when he arrives in the ED, this is the only ABG you have: 7.23/85/pO2/35 35-24=11. 11/3.5 = 3. 3 x 10 =30. 40 + 30 = 70 Baseline pCO2 = 70. Pt. has acute resp acidosis.
- 168. Respiratory Alkalosis Decreasing of CO2 level due to a hyperventilation, which expels large amounts of CO2, leads to a lowering in the partial pressure of CO2 below normal and the shift of the equilibrium from H2CO3 to CO2 and H2O. This shift decreases H3O+ and raises blood pH – alkalosis. CO2 + H2O H2CO3 H3O+ + HCO3 -
- 169. Respiratory Alkalosis: CO2 ↓ pH ↑ Symptoms: Increased rate and depth of breathing, numbness, light-headedness, tetany Causes: hyperventilation due to anxiety, hysteria, fever, exercise; reaction to drugs such as salicylate, quinine, and antihistamines; conditions causing hypoxia (e.g., pneumonia, pulmonary edema, and heart disease) Treatment: Elimination of anxiety producing state, rebreathing into a paper bag
- 170. Acid-Base Imbalances Normal H2CO3 ……………… HCO3 24 mEq/L 1.2 mEq/L 1 20 7.4
- 173. Acute Hypocapnia: HCO3 decreases 2 mmol/L for every 10 mmHg decrease in PaCO2 <40 Chronic Hypocapnia: For every 10 mmHg decrease in PaCO2 <40 HCO3 decreases 5 mmol/L
- 174. Respiratory Alkalosis: 15 y.o. girl who just who has panic attack pH 7.70 pCO2 20 Bicarbonate 24 Reality: 7.65/20/pO2/20, because hypocapnia leads to lower bicarb as well. 40 – 20 = 20. For every 10 CO2 HCO3 dec by 5 mmol 20/10 = 2 x 5 = 10 24 – 10 = 14
- 175. 3 most important equations so far Chronic resp. acidosis: steady-state pCO2 is increased by 10 for every 3.5 increase in HCO3 Acute metabolic acidosis: pCO2 = 1.5 x HCO3 + 8 (+/- 2) Acute metabolic alkalosis: pCO2 = 0.9 x HCO3 + 15
- 176. Metabolic Acidosis
- 177. METABOLIC ACIDOSIS Metabolic acidosis represents an increase in acid in body fluids . Reflected by a decrease in [HCO3 -] and a compensatory decrease in pCO2.
- 179. Metabolic Acidosis Impaired cardiac contractility Decreased threshold for v fib Decreased Hepatic and Renal perfusion Increased Pulm Vasc resistance Inability to respond to catecholamines Vascular collapse
- 180. Test Case 23 year old AIDS patient c/o weakness and prolonged severe diarrhea. He appears markedly dehydrated. pH 7.25 pCO2 25 pO2 110 HCO3 11 151 129 60 2.0 12 2.0 Acute metabolic acidosis: pCO2 = 1.5 x HCO3 + 8 (+/- 2) = 1.5 x 11 + 8 = 24.5
- 181. Metabolic Acidosis 18 y.o. WF presents in DKA ABG: pH 7.00 pCO2 25 Bicarbonate 6 If Pure metabolic acidosis, then pCO2=(1.5)(6) + 8= 17 . pCO2=1.5 x HCO3 + 8 +/- 2 = 1.5 x 6 + 8 = 9 + 8 = 17
- 182. Respiratory Compensation Metabolic Acidosis: Occurs rapidly Hyperventilation “Kussmaul Respirations” Deep > rapid (high tidal volume) Metabolic Alkalosis: Calculation not as accurate Hypoventilation Restricted by hypoxemia PCO2 seldom > 50-55 pCO2=1.5 x HCO3 + 8 +/- 2 Winter’s formula pCO2=0.9 x HCO3 + 15
- 183. METABOLIC ALKALOSIS: Metabolic alkalosis represents an increase in [HCO3 -] with a compensatory rise in pCO2.
- 185. Test Case An 80 year old man has been confused and c/o SOB for one week. He also has a hearing problem and has seen 3 ENT docs in the past month. Family denies medications. pH 7.53 pCO2 15 pO2 80 HCO3 12 140 108 3.0 13 120 Diagnosis? AG = 140 - 121 = 19













































































































































































![METABOLIC ACIDOSIS
Metabolic acidosis represents an increase in
acid in body fluids .
Reflected by a decrease in [HCO3 -] and a
compensatory decrease in pCO2.](https://image.slidesharecdn.com/6293212-220811145701-fb4570fa/85/fluids-ppt-177-320.jpg)





![METABOLIC ALKALOSIS:
Metabolic alkalosis represents an increase in
[HCO3 -] with a compensatory rise in pCO2.](https://image.slidesharecdn.com/6293212-220811145701-fb4570fa/85/fluids-ppt-183-320.jpg)

