FRO.ppt
- 2. • The Knee Joint Structure Movements Biomechanics • Manual Muscle Testing Hamstrings Quadriceps Femoris • Floor reaction Orthosis Introduction Prerequisites Indications Design Fabrication Biomechanics Advantages Disadvantages Contraindications
- 4. • Knee is the largest and most complex joint of the body. It is a compound Synovial joint, incorporating- Two Condylar joint between the condyles of Femur and Tibia. One Saddle joint between the Femur and Patella. • The femoral condyles articulate with tibial condyles below and behind and with the patella in front.
- 5. • Flexion/ Extension- Flexion is the rolling of the femoral condyles posteriorly on the tibial condyle. Extension is the anterior rolling of the femoral condyles on the tibial plateau, displacing the femoral condyles back to a neutral position.
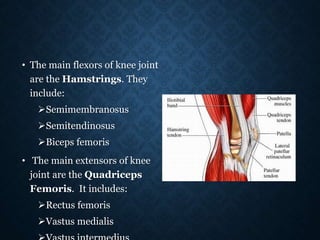
- 6. • The main flexors of knee joint are the Hamstrings. They include: Semimembranosus Semitendinosus Biceps femoris • The main extensors of knee joint are the Quadriceps Femoris. It includes: Rectus femoris Vastus medialis
- 7. • Medial/ Lateral rotation- • Medial/ Lateral rotation of the knee joint are angular motions that are named for the motion of the tibia on the femur. • These axial rotations of the knee joint occur about a longitudinal axis that runs through or close to the medial tibial intercondylar tubercle. • Consequently, the medial condyle acts as a pivot point while the lateral condyle moves through an arc of motion, regardless of the direction of rotation.
- 8. • As the tibia laterally rotates on the femur, the medial tibial condyle moves only slightly anteriorly on the relatively fixed medial femoral condyle, whereas the lateral tibial condyle moves a larger distance posteriorly on the relatively fixed lateral femoral condyle. • During tibial medial rotation, the medial tibial condyle moves only slightly posteriorly, whereas the lateral condyle moves anteriorly through a larger arc of motion.
- 9. • The medial rotators of the knee joint are: Popliteus Semimembranosus Semitendinosus • The lateral rotator of the knee joint are: Biceps femoris
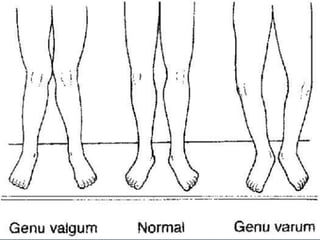
- 10. • The longitudinal axis of femur is oblique, directed inferiorly & medially from proximal to distal end. The longitudinal axis of tibia is directed almost vertical. • The femoral and tibial longitudinal axes normally form an angle medially at the knee joint of 180°-185°. • If the medial tibiofemoral angle is greater than 185°, an abnormal condition called Genu Valgum (Knock Knees) exists. • If the medial tibiofemoral angle is 175° or less, an abnormal condition called Genu Varum (Bow Legs) exist.
- 11. • Both active (muscular) and passive (capsuloligamentous) forces contribute to the stability of knee joint. These forces not only depend upon the position of knee joint but also of the surrounding tissues, magnitude & direction of applied forces and availability of secondary restraints.
- 14. • Position of Patient: Prone with limbs straight and toes hanging over the edge of table. • Position of Therapist: Standing next to the limb to be tested. Hand giving resistance is contoured around the posterior surface of the leg just above the ankle. Resistance is applied in the direction of knee extension for Grades 5 and 4. the other hand is placed over the hamstring tendons on the posterior thigh. • Test: Patient flexes knee while maintaining leg in neutral position.
- 15. • Position of Patient: Prone with knee flexed to less than 90˚. Leg in internal rotation (toes pointing towards midline). • Position of Therapist: Hand giving resistance grasps the leg at the ankle. Resistance is applied in oblique direction (down and out) towards knee extension. • Test: Patient flexes knee, maintaining the leg in internal rotation (heel towards examiner, toes pointing
- 16. • Position of patient: Prone with knee flexed to less than 90˚. Leg is in external rotation (toes pointing laterally). • Position of Therapist: Therapist resists knee flexion at the ankle using a downward and inward force. • Test: Patient flexes knee, maintaining leg in external rotation (heel away from
- 17. • Grade 5 (Normal) for all three tests: Resistance will be maximal and the end knee flexion position (approx 90˚) cannot be broken. • Grade 4 (Good) for all three tests: End knee flexion position is held against strong to moderate resistance. • Grade 3 (Fair) for all three tests: Holds end range
- 18. • Position of patient: Side-lying with test limb (uppermost limb) supported by examiner. Lower limb flexed for stability. • Position of Therapist: Standing behind the patient at knee level. One arm is used to cradle thigh, providing hand support at the medial side of thigh. Other hand supports the leg at the ankle just above the malleolus. • Test: Patient flexes knee through available range of motion. • Instructions to the patient: “Bend your knee.” Grade 2 (Poor): Completes available
- 19. • Position of Patient: Prone. Limbs are straight with toes extending over end of table. Knee is partially flexed and supported at ankle by examiner. • Position of Therapist: Standing next to test limb at knee level. One hand supports the flexed limb at the ankle. The opposite hand palpates both medial and lateral hamstring tendons just above posterior knee. • Test: Patient attempts to flex the knee.
- 20. • Instructions to Patient: “Try to bend your knee.” • Grade 1 (Trace): Tendons become prominent, but no visible movement occurs. • Grade 2 (Zero): No palpable contraction of the muscles and tendons do not stand out.
- 21. • Position of Patient: Short sitting. Place the wedge or pad under the distal thigh to maintain the femur in horizontal position. Hands rest on the table on either side of the body for stability, or may grasp the table edge. The patient should be allowed to lean backward to relieve hamstring muscle tension. Do not allow the patient to hyperextend the knee because this may lock it into position.
- 22. • Position of the Therapist: Standing on the side of limb to be tested. The hand giving resistance is contoured over the anterior surface of the distal leg just above the ankle. For Grades 5 &4, resistance is applied in a downward direction in the direction of knee flexion. • Test: Patient extends knee through available ROM but not beyond 0˚ • Instructions to Patient: “Straighten your knee. Hold it! Don’t let me bend it.”
- 23. • Grade 5 (Normal): Holds and position against maximal resistance. • Grade 4 (Good): Holds end position against strong to moderate resistance. • Grade 3 (Fair): Completes available range and holds
- 24. • Position of Patient: Side- lying with test limb uppermost. Lowermost limb may be flexed for stability. Limb to be tested is held in about 90˚of knee flexion. The hip should be in full extension. • Position of Therapist: Standing behind patient at knee level. One arm cradles the test limb around the thigh with the hand supporting the underside of the knee. The other hand holds the leg just above the
- 25. • Test: Patient extends knee through the available ROM. The therapist supporting the limb provides neither assistance nor resistance to the patient’s voluntary movement. • Instructions to Patient: “Straighten your knee.” • Grade 2 (Poor): Completes available ROM.
- 26. • Position of Patient: Supine. • Position of Therapist: Standing next to the limb to be tested at knee level. Hand used for palpation should be on the quadriceps tendon just above the knee with the tendon “held” gently between the thumb and fingers. The examiner may also want to palpate the patellar tendon with 2 or 4 fingers just below the knee. • Test: Patient attempts to
- 27. Instructions to Patient: “Push the back of your knee down to the table:” or “tighten your kneecap” Grade 1 (Trace): Contractile activity can be palpated in muscle through the tendon. No joint movement occurs. Grade 0 (Zero): No palpable contractile activity.
- 29. • It is a device that harnesses the Ground Reaction Force as primary source of sagittal plane stability for knee joint during stance. • It relies on foot planter flexion-knee extension couple where a fixed, slightly planter flexed ankle creates an extension moment at knee. • Plantar flexion angle, length and rigidity of toe-plate helps to determine the magnitude of knee extension moment.
- 30. • Anterior shell and medio-lateral trimlines are padded at proximal pre-patellar areas so that the extra extension force being transmitted to knee is more tolerable. • FRO can be fabricated as Single solid unit (May be difficult to don). Solid ankle AFO with an additional anterior shell that is snugly strapped in place (Anterior shell can be removed and the orthosis can be used as traditional AFO).
- 31. Absence of knee or hip flexion contracture exceeding 10˚. Careful determination of the angle to which the ankle is set within the orthosis. Presence of some trunk balance and/or ability to use auxiliary walking aids in the event of diminished trunk balance. Presence of minimum of Grade 3 quadriceps strength. Whether or not the orthosis is U/L or B/L.
- 32. • Post polio paralysis • Cerebral palsy (FRAFOs in children with spastic diplegic CP who exhibit a moderate or severe knee flexion (crouch gait) with excessive ankle dorsiflexion motion during the stance phase. FRAFO use showed significant kinematic gait improvements including a reduction of abnormal ankle dorsiflexion and knee flexion motion). • Brain injury • Spina bifida • Spinal cord injury In these cases, FRO functions to maintain affected joints in proper alignment , to accentuate knee extension in midstance and compensate for weak or absent gastrocnemius-soleus muscles.
- 33. • Poliomyelitis often called polio or infantile paralysis, is an acute, viral, infectious disease spread from person to person, primarily via the fecal-oral route. • It generally affects lowerlimbs and causes partial or full paralysis. • The main muscle of the knee joint that is paralysed is the quadriceps.
- 34. Quadriceps paralysis Loss of Knee extension power Patient will press the knee by hand to extend it Hand-to-Knee gait
- 35. • The conventional remedy for paralysed quadriceps is a long leg calliper made out of mild steel, leather and wood. • This not only weighs excessively but the long lever arm rigidises the limb and adds to the difficulties. • All the joints provided in the side bars are not congruent with the axis of movements of anatomical joints. • Apart from this, its fabrication is labour-intensive and time-consuming. • When a polio patient with paralysed quadriceps, comes initial contact at heel it causes the weight line to pass posterior to the knee. Here quadriceps action is needed to prevent buckling but this action is absent in polio affected limb. • To compensate for this, FRO is prescribed.
- 36. • Spina bifida is a developmental congenital disorderr caused by the incomplete closing of the embryonic neural tube. • Patients with myelomeningocele tend to stand in a crouched position (flexed hips, knees, and ankles) due to lower-extremity weakness.
- 37. • In this crouched position, the ground-reaction forces generally act posterior to the knee center, encouraging further knee flexion. • A floor-reaction ankle-foot orthosis (FRAFO) may be prescribed with the goal of shifting the ground-reaction force more anterior to the knee center, providing a knee-extension moment and increasing knee extension in stance. • Compound this problem with knee-flexion contractures, and the patient's ability to achieve an efficient gait pattern is severely decreased. • The loss of knee extension due to the contractures result in a shortening of step length seen at terminal swing. • The inability to appropriately extend the knee in mid and terminal stance increases the force on the quadriceps.
- 38. • Cerebral palsy (CP) is an umbrella term encompassing a group of non-progressive , non-contagious motor conditions that cause physical disability in human development, chiefly in the various areas of body movement • In patients with cerebral palsy, labored gait associated with excessive knee flexion in stance phase is presented with significant
- 39. • Crouch gait commences with overactivity of the hamstrings, which increases knee flexion and thus requires large increase in quadriceps force to stabilize the knee. • The FRO involves harnessing the floor reaction and directing it to the anterior aspect of the distal shank, thus stabilizing the joint in extension.
- 40. • One piece: encloses the back of lower calf, shin and bottom of the foot. • Two piece: same as one piece but has a removable anterior panel. • The design of a FRAFO included a full toe plate, rigid ankle, and an anterior tibial shell section. The combination of these three components allow the plantarflexion-knee extension couple (PF/KE) to occur, causing a knee-extension moment. This knee-extension couple helps to support weak quadriceps and plantarflexor muscles.
- 42. • The patient is seated on a casting chair and all the bony prominences are identified & marked with an indelible pencil. • A latex rubber tube is run anteriorly over the dorsum of the foot along the tibial crest to the level of neck of fibula. This allows easy and safe removal of the cast. • A length of stockinette is wrapped to act as a cast separator and the shank is then wrapped with bandage to the level of fibular neck. • The foot is then placed on a footboard in neutral subtalar position with slight planterflexion to accommodate the heel height of patient’s shoe. • Care must be taken to position the foot in the correct amount of toe-out and to maintain the shank in proper orientation to mid-sagittal alignment.
- 43. • When the ankle-foot section has hardened, the knee is extended to approx. 15˚ of flexion and wrapped with the bandage to the level of proximal border of patella. • The patellar tendon is then outlined as a reaction point from floor for knee extension by compressing with thumb and forefinger pressing in the same manner as with PTB orthosis casting. • Since weight bearing is not a consideration, the popliteal area and contour of the posterior calf need not be disturbed.
- 44. • The negative cast is removed and filled in for modification. • Modification follows standard procedures with plaster build ups over all bony prominences for pressure relief. • The foot plate is then modified for support of the medial and lateral longitudinal arches. • In addition, a slightly more aggressive modification is made under the sustentalaculum tali ( eminence on the medial surface of calcaneum for the attachment of spring ligament) and transverse metatarsal arch to provide a stable base for calcaneum in a slight planterflexion position and comfortable distal reaction point under metatarsal heads.
- 45. • A sheet of COPP is drape vacuum formed over the positive model from posterior to anterior, creating an anterior seam. • In the area of patellar tendon, the seam is pinched together tightly to endure good bonding at this point. • The orthosis is trimmed as follows: Proximal trimline: Anteriorly, it should extend just above the patellar tendon. Posteriorly, it should extend till the level of maximum calf. Distal trimline: It extends to the end of the toes. Medial trimline: It encompasses the medial malleolus and lies just anterior to it.
- 47. • The ankle joint is kept in 5 to 7 degrees of plantar flexion in order to shift the line of floor reaction. • By keeping ankle in plantar flexion, the resultant of floor reaction passes posterior to the ankle joint and anterior to the knee joint generating a posteriorly directed moment which tends to push the knee in extension thus controlling knee flexion allowing the patient to remove his or her hand. • The brace acta as a First class lever and the planterflexed attitude at the ankle utilizes the fulcrum establised by the distal trimline of the footplate.
- 50. • Besides stabilizing the ankle and subtalar joints, it assists the knee extension capabilities of the patient with fair quadriceps strength and therefore, helps prevent the knee joint from buckling. • The ankle in FRO is almost in neutral position, so that patient can begin gait cycle with heel strike and descend stairs more easily. • Gait is more physiological because it provides opportunity for quadriceps to work as the patient walks. • Provides patient good security and gives him a sense of freedom. • Light weight. • Device provides total-contact, thus preventing pressure sores over bony prominences. • Durable. • Compact.
- 51. • FRO may have a negative impact on balance reactions. If the patient do not have effective postural control, an assistive device may be required. • Fabrication is time-consuming. • Lack of adjustibility in the degree of ankle equinus & consequently the amount of knee extension moment control force. • Long term use can lead to Genu recurvatum.
- 52. • Inapproriate for the patients with Genu recurvatum. • Not suitable in case of structural instability of knee joint. • Difficult for the patients with fixed flexion contracture of more than 10˚.(In this case, FRO will resist dorsiflexion and knee flexion but does not create a true extension moment.) • If used in bilateral cases, tip-toe type of gait will be achieved which is very uncomfortable for the patients and hard to maintain the balance, hence contraindicated in bilateral cases.
- 53. • It was observed that by using FRO in patients with cerebral plasy and spina bifida, crouch gait was greatly reduced or eliminated. • When the pre requisites and specifications were met, FRO proved to be more successful than its predecessor, the KAFO. • Following the careful determination of candidacy in the patients, the floor reaction orthosis can provide more stability and minimize componentary, weight and bulk.