GN.ppt
- 1. Glomerulonephritis 1 Dr.Jiyar Jalal FIBMS urology College of Medecine University of Duhok
- 2. Glomerulonephritis : is a general term for a group of disorders in which there is bilateral, symmetrical immunologically mediated injury to the glomerulus . Glomerulopathies: is a term used for disorders of the glomerulus without evidence of inflammation. There is an overlap between these two terms. 3
- 3. Introduction • Normally, the glomerulus consists of an anastomosing network of capillaries lined by fenestrated endothelium invested by two layers of epithelium. • The glomerular capillary wall is the filtering membrane and consists of the following structure : • 1.A thin layer of fenestrated endothelial cells . 2. A glomerular basement membrane (GBM) 3.The visceral epithelial cells (podocytes) The entire glomerular tuft is supported by mesangial cells lying between the capillaries.
- 5. Glomerulonephritis means 'inflammation of glomeruli’. Most types of glomerulonephritis seem to be immunologically mediated and several respond to immunosuppressive drugs. 5
- 6. Pathogenesis of Glomerulonephritis Two forms of antibody associated injury:- • Injury resulting from deposition of soluble antigen antibody complexes in the glomerulus. • Injury by antibodies reacting in situ within the glomerulus
- 7. Although deposition of circulating immune complexes was previously thought to be a common mechanism, it now seems that most granular deposits of immunoglobulin are formed 'in situ' by antibodies which complex with glomerular antigens, or with other antigens ('planted' antigens, e.g. viral or bacterial ones) that have localised in glomeruli. 7
- 8. Sites of Glomerular injury • Subepithelial. • Within glomerular basement membrane. • Subendothelial. • Mesangial and paramesangial
- 9. Pathophysiolog y Due to any etiological factor Release of Ag substance into the circulation Formation of Ab formation of Ag and Ab complex in the glomerulus Inflammatory response proliferation of epithelial cells lining the glomerulus Leukocytes infiltration of the glomerulus Thickening of the glomerular filtration membrane
- 10. Cont… scarring and loss of glomerular filtration membrane decrease GFR and glomerulus plasma flow Retention of sodium and water Edema and hypertension
- 11. • Glomerulonephritis (GN) can be classified by the clinical syndrome/presentation(e.g. nephritic or nephrotic syndrome) • histological appearance (e.g. minimal change disease), • aetiology (e.g. post-streptococcal GN)
- 12. Clinical Syndrome • Nephrotic Minimal change glomerulonephritis Membranous glomerulonephritis Focal segmental glomerulosclerosis • Nephritic IgA nephropathy Post-streptococcal GN Rapidly progressive glomerulonephritis
- 13. Classifications of glomerulonephritis are largely histopathologic. Systemic hypertension and atherosclerosis can produce chronic glomerulosclerosis. Diabetic nephropathy is associated with thickening of the GBM secondary to the long-standing effects of hyperglycemia. 13
- 14. Approach to Glomerular Disease Patients with glomerular disease usually have some hematuria with varying degrees of proteinuria. Hematuria is typically asymptomatic. As little as 3– 5 red blood cells in the spun sediment from first voided morning urine is suspicious. Exception of IgA nephropathy and sickle cell disease is gross hematuria present. When red blood cell casts or dysmorphic red blood cells are found in the sediment, glomerulonephritis is likely. 14
- 15. Sustained proteinuria >1–2 g/24 h is also commonly associated with glomerular disease. Proteinuria is nonsustained, generally <1 g/24 h, and is sometimes called functional or transient proteinuria. Fever, exercise, obesity, sleep apnea, emotional stress, and congestive heart failure can explain transient proteinuria. Proteinuria only seen with upright posture is called orthostatic proteinuria. Selective proteinuria largely composed of albumin, while Nonselective, containing albumin and a mixture of other serum proteins. 15
- 16. 16 Urine Assays for Albuminuria/Proteinuria 24-Hour Albumina (mg/24 h) Albumina/Creatinin e Ratio (mg/G) Dipstick Proteinuria 24-Hour Urine Proteinb (mg/24 h) 8–10 <30 – <150 Normal 30-300 30–300 –/Trace/1+ – Microalbuminuri a >300 >300 Trace–3+ >150 Proteinuria aAlbumin detected by radioimmunoassay. bAlbumin represents 30–70% of the total protein excreted in the urine.
- 17. Spectrum of glomerular diseases 17
- 18. Acute nephritic syndrome producing 1–2 g/24 h of proteinuria, hematuria with red blood cell casts, pyuria, hypertension, fluid retention, and a rise in serum creatinine associated with a reduction in glomerular filtration. Nephrotic syndrome describes the onset of heavy proteinuria (>3.0 g/24 h), hypertension, hypercholesterolemia, hypoalbuminemia, edema/anasarca, and microscopic hematuria; if only large amounts of proteinuria are present without clinical manifestations, the condition is sometimes called nephrotic-range proteinuria. Primary glomerulonephritis :glomerulonephritis is 18
- 19. Clinical Syndrome Nephrotic Proteinuria(>3 g/24hr) Oedema Hypoalbuminemia(<30g/l) Hyperlipidemia Intravscular volume depletion with hypotension or expansion with hypertension Nephritic Haematuria Oedema Hypertension oligouria
- 20. Nephritic Syndrome • Acute nephritic syndromes classically present with hypertension, hematuria, red blood cell casts, oliguria and azotemia, and mild to moderate proteinuria. • Extensive inflammatory damage to glomeruli causes a fall in GFR and eventually produces uremic symptoms with salt and water retention, leading to edema and hypertension.
- 21. 21
- 22. Acute Nephritic Syndromes Postinfectious Glomerulonephritis: This is most common following infection with certain strains of streptococcus and therefore is often called post-streptococcal nephritis, but it can occur following other infections. It is much more common in children than adults. The latency is usually about 10 days after a throat infection or longer after skin infection, suggesting an immune mechanism rather than direct infection. 22
- 23. Postinfectious Glomerulonephritis Sodium retention, hypertension and oedema, are particularly pronounced. Flank pains (due to swelling of the renal capsule) are reported in as many as 50% of cases. Five percent of children and 20% of adults have proteinuria in the nephrotic range. There is also reduction of GFR, proteinuria, haematuria and reduced urine volume. Characteristically, this gives the urine a red or smoky appearance. There are low serum concentrations of C3 and C4, evidence of streptococcal infection (perform antistreptolysin O (ASO) titre, culture of throat swab, and other swab tests if skin infection is suspected). 23
- 24. Postinfectious Glomerulonephritis (cont.) Typically affects children between the ages of 2 -14 years Management is by fluid and sodium restriction and use of diuretic and hypotensive agents is usually adequate. Antibiotic treatment for streptococcal infection should be given to all patients and their cohabitants. 24
- 25. Remarkably, the renal lesion in almost all children and most adults seems to resolve completely despite the severity of the glomerular inflammation and proliferation seen histologically. Recurrent poststreptococcal glomerulonephritis is rare. Overall, the prognosis is good, with permanent renal failure being very uncommon (1–3%), and even less so in children. 25
- 26. Lupus Nephritis Most common clinical sign of renal disease is proteinuria, but hematuria, hypertension, varying degrees of renal failure, and active urine sediment with red blood cell casts can all be present. Anti-dsDNA antibodies that fix complement correlate best with the presence of renal disease. Hypocomplementemia is common in patients with acute lupus nephritis (70–90%) and declining complement levels may herald a flare. Renal biopsy, however, is the only reliable method of identifying the morphologic variants of lupus nephritis. 26
- 27. Classification for Lupus Nephritis Excellent prognosis and generally do not need therapy for their lupus nephritis Minimal mesangial Class I Mesangial proliferation Class II Therapy with steroids alone Focal nephritis Class III Treatment must combine high-dose steroids with either cyclophosphamide or mycophenolate mofetil. Diffuse nephritis Class IV Therapy with inhibitors of the renin- angiotensin system Membranous nephritis Class V Renal transplantation Sclerotic nephritis Class VI 27
- 28. Anti-GBM Disease • Patients who develop autoantibodies directed against glomerular basement antigens frequently develop a glomerulonephritis termed antiglomerular basement membrane disease. When they present with lung hemorrhage and glomerulonephritis, they have a pulmonary-renal syndrome called Goodpasture’s syndrome. • Goodpasture’s syndrome appears in two age groups: 1. In young men in their late twenties 2. And in men and women in their sixties and seventies. – Disease in the younger age group is usually explosive, with hemoptysis, a sudden fall in hemoglobin, fever, dyspnea, and hematuria. Hemoptysis is largely confined to smokers.
- 29. Anti-GBM Disease • The performance of an urgent kidney biopsy is important in suspected cases of Goodpasture’s syndrome to confirm the diagnosis and assess prognosis. • Glomeruli show segmental necrosis and GBM breaks, with resulting proliferation of the parietal epithelial cells in response to the exudation of plasma proteins and the deposition of fibrin in Bowman’s space. These distinctive lesions of proliferation are called crescents owing to their shape as they fill Bowman’s space. • As these lesions progress, there is concomitant interstitial nephritis with fibrosis and tubular atrophy. • The presence of anti-GBM antibodies and complement is recognized on biopsy by linear immunofluorescent staining for IgG (rarely IgA).
- 30. Deposition of linear immune complexes, characteristic of classic anti-glomerular basement membrane (anti-GBM) antibody glomerulonephritis.
- 31. Anti-GBM Disease • Prognosis at presentation is worse if there are >50% crescents on renal biopsy with advanced fibrosis, if serum creatinine is >5–6 mg/dL, if oliguria is present, or if there is a need for acute dialysis. Although frequently attempted, most of these latter patients will not respond to plasmapheresis and steroids. • Patients with advanced renal failure who present with hemoptysis should still be treated for their lung hemorrhage, as it responds to plasmapheresis and can be lifesaving. Treated patients with less severe disease typically respond to 8–10 treatments of plasmapheresis accompanied by oral prednisone and cyclophosphamide in the first 2 weeks. • Kidney transplantation is possible, but because there is risk of recurrence, experience suggests that patients should wait for 6 months and until serum antibodies are undetectable.
- 32. IgA nephropathy • IgA nephropathy is one of the most common forms of glomerulonephritis worldwide. It is classically characterized by episodic hematuria associated with the deposition of IgA in the mesangium. • There is a male preponderance, a peak incidence in the second and third decades of life, and rare familial clustering. • Deposits of IgA are also found in the glomerular mesangium in a variety of systemic diseases, including chronic liver disease, Crohn’s disease, gastrointestinal adenocarcinoma, chronic bronchiectasis, idiopathic interstitial pneumonia, ankylosing spondylitis, and Sjogren’s syndrome. IgA deposition in these entities is not usually associated with clinically significant glomerular inflammation or renal dysfunction and thus is not called IgA nephropathy. • The two most common presentations of IgA nephropathy are recurrent episodes of macroscopic hematuria during or immediately following an upper respiratory infection often accompanied by proteinuria or persistent asymptomatic microscopic hematuria.
- 33. IgA nephropathy • IgA nephropathy is the most common glomerular disease revealed by renal biopsy worldwide. • Histologically, the lesions in IgA nephropathy vary considerably: 1. The glomeruli may be normal 2. Mesangial widening and segmental inflammation confined to some glomeruli (focal proliferative GN). 3. Diffuse mesangial proliferation (mesangioproliferative GN); or (rarely) overt crescentic GN. – The characteristic immunofluorescence picture is of mesangial deposition of IgA, often with C3 and smaller amounts of IgG or IgM. – Electron microscopy confirms the presence of electron-dense deposits in the mesangium.
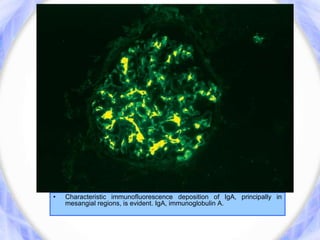
- 34. • Characteristic immunofluorescence deposition of IgA, principally in mesangial regions, is evident. IgA, immunoglobulin A.
- 35. IgA nephropathy • IgA nephropathy is a benign disease for the majority of patients, and 5– 30% of patients may go into a complete remission, with others having hematuria but well preserved renal function. In the minority of patients who have progressive disease, progression is slow, with renal failure seen in only 25–30% of patients with IgA nephropathy over 20–25 years. • risk factors for the loss of renal function include the presence of hypertension or proteinuria, the absence of episodes of macroscopic hematuria, male sex, older age of onset, and extensive glomerulosclerosis or interstitial fibrosis on renal biopsy. • The management of less acute disease is largely directed towards the control of blood pressure in an attempt to prevent or retard progressive renal disease. There is some evidence for additional benefit from several months of high-dose corticosteroid treatment in high-risk disease, but no strong evidence for other immunosuppressive agents. Other therapies are under investigation.
- 36. Henoch-Schonlein Purpura • This condition most commonly occurs in children but can also be observed in adults. It is characterised by a systemic vasculitis that often arises in response to an infectious trigger. • The presentation is with a characteristic petechial rash typically affecting buttocks and lower legs, and abdominal pain due to the occurrence of vasculitis involving the gastrointestinal tract. The presence of glomerulonephritis is usually indicated by the occurrence of haematuria. When Henoch–Schönlein purpura occurs in older children or adults, the glomerulonephritis is usually more prominent and less likely to resolve completely. • Renal biopsy shows mesangial IgA deposition and appearances that are indistinguishable from acute IgA nephropathy. • Treatment is supportive in nature; in most patients, the prognosis is good, with spontaneous resolution, but some, particularly adults, progress to develop ESRD.
- 37. RAPIDLY PROGRESSIVE GLOMERULONEPHRITIS (RPGN) This describes an extreme inflammatory nephritis which causes rapid loss of renal function over days to weeks. It is typically seen in Goodpasture's disease, but can also be seen in SLE and occasionally IgA and other nephropathies. 37
- 38. 38 Mesangiocapillary glomerulonephritis (MCGN) (= membranoproliferative glomerulonephritis, MPGN) Clinical features Association Usually proteinuria, may be haematuria Most common pattern found in association with subacute bacterial infection No proven treatments except where cause can be treated Bacterial infection Hepatitis B virus Cryoglobulinaemia (± hepatitis C virus infection) Type I Also known as dense deposit disease C3 nephritic factor and partial lipodystrophy Type II
- 39. Nephrotic Syndrome Nephrotic syndrome classically presents with heavy proteinuria, minimal hematuria, hypoalbuminemia, hypercholesterolemia, edema, and hypertension. Consequences of Nephrotic syndrome : 1.Oedema 2.Hyperlipidemia. 3.Hemostasis disorder: venous + arterial thrombosis. 4.Infections. 39
- 40. Minimal change glomerulonephritis • Most common cause of nephrotic syndrome in children.it causes about 70-90% of nephrotic syndrome in children but only 10-15% of nephrotic syndrome in adults. • It may be idiopathic or secondary )e.g.Hodgkin disease or use of NSAIDs) • C/P : nephrotic generalised oedema, heavy proteinuria which over an extended period of time leads to a state of protein depletion with muscle wasting, thinning of the skin, and growth failure.less common clinical features include hypertension, microscopic haematuria and decreased renal function..
- 41. • The glomeruli are normal by light microscopy (hence ‘ minimal change ’ ). By EM, there is uniform and diffuse effacement of the Podocyte foot processes. • Tx: high-dose CS (e.g. prednisolone) for 6-8 weeks. Relapse occurs in 70-75% of children after first remission. The frequency of relapse decreases after puberty. • other immunosuppressant like Cyclophosphomide, mycophenolate M. are saved for frequent relapses, steroid dependent patient or steroid resistant patients.
- 42. Focal segmental glomerulosclerosis • FSGS is a histological description, the segmental lesions may involve only a minority of the glomeruli and may be missed if the biopsy specimen contains an insufficient number of glomeruli. • Idiopathic FSGS typically presents as nephrotic syndrome(66%) or subnephrotic proteinuria (33%) in association with hypertension, mild renal insufficiency, and an abnormal urine sediment that contains red blood cells and leukocytes and it typically shows liitle response to CS However, a proportion of patients with FSGS do respond to corticosteroids(a good prognostic sign)
- 43. • Secondary FSGS is a potential long-term consequence of nephron loss from any cause. It can complicate congenital renal diseases such as congenital oligomeganephronia, in which both kidneys have a reduced complement of nephrons, and congenital unilateral agenesis. • In addition, FSGS may develop following acquired loss of nephrons from reflux nephropathy;interstitial nephritis; sickle cell disease; and the combined effects of ischemia, cyclosporine nephrotoxicity, and rejection on renal allograft function. • This disease frequently recurs after renal transplantation, and sometimes proteinuria recurs almost immediately. 50% of nephrons must be lost for development of secondary FSGS.
- 45. Treatment: • Tx: BP control, restriction of diatary salt intake, diuretics, reduction of proteinuria with ACEi or ARB, treat the underlying cause. • Current evidence, mostly derived from retrospective analyses, favors prolonged corticosteroids therapy (6 months or longer) to induce remission in patients with idiopathic FSGS. proteinurias remits in only 20-45% of patients receiving CS. • Cyclophosphamide and cyclosporine, induce partial or complete remission in 50 to 60% of steroid-responsive patients but are generally ineffective in steroid-resistant cases. • Outcome: Progression to ESRD in 50% at 5 years if untreated. Poor prognostic factors at presentation include hypertension, abnormal renal function, black race, and persistent heavy proteinuria
- 46. Membranous Nephropathy This Accounts for approximately 30% of cases of nephrotic syndrome in adults. Secondary causes: 1. Infections: HBV and HCV, syphilis, malaria, schistosomiasis, leprosy, filariasis. 2. Cancer: Breast, colon, lung, stomach, kidney, esophagus. 3. Drugs: gold, mercury, penicillamine, NSAIDs, probenecid. 4. Autoimmune diseases: SLE, RA, primary biliary cirrhosis, Sjögren's syndrome, Hashimoto's thyroiditis 5. Other systemic diseases: Sickle cell anemia, diabetes, Crohn's disease, sarcoidosis, Guillain-Barré syndrome. 46
- 47. Eighty percent of patients with MGN present with nephrotic syndrome and nonselective proteinuria. Of this group, approximately one-third remit spontaneously, one-third remain in a nephrotic state, and one-third show progressive loss of renal function. In addition to the treatment of edema, dyslipidemia, and hypertension, inhibition of the renin-angiotensin system is recommended. Treatment with high doses of corticosteroids and alkylating agents (e.g. cyclophosphamide) reserve for those with severe nephrotic syndrome or deteriorating renal function. 47
- 48. Diabetic Nephropathy Is the single most common cause of chronic renal failure accounting for 45% of patients receiving renal replacement therapy. Approximately 40% of patients with Types 1 or 2 diabetes develop nephropathy, but due to the higher prevalence of Type 2 diabetes (90%) compared to Type 1 (10%). Renal biopsies from patients with Types 1 and 2 diabetes are largely indistinguishable. 48
- 49. Diabetic nephropathy is usually diagnosed without a renal biopsy. Blood sugar and blood pressure control as well as inhibition of the renin-angiotensin system in retarding the progression of diabetic nephropathy. 49
- 50. Inherited Glomerular Disease Alport’s Syndrome: Most cases arise from a mutation or deletion of the COL4A5 gene on the X chromosome which encodes type IV collagen, resulting in inheritance as an X-linked recessive disorder. Less common and cause autosomal recessive disease. Approximately 85% of patients with Alport's syndrome have an X-linked inheritance of mutations in the α5(IV) collagen chain on chromosome Xq22–24. Fifteen percent of patients have autosomal recessive disease of the 3)IV) or α 4(IV) chains on chromosome 2q35–37. Rarely, some kindred have an autosomal dominant inheritance of dominant-negative mutations in α 3)IV) or α 4(IV) chains. 50
- 51. Some other basement membranes containing the same collagen are similarly affected, notably in the cochlea, so that Alport's syndrome is associated with sensorineural deafness and ocular abnormalities. No specific treatment has been devised to slow the progress of this condition, but patients with Alport's syndrome are good candidates for renal replacement therapy as they are young and usually otherwise healthy. 51
- 52. Cholesterol Emboli Aging patients with clinical complications from atherosclerosis sometimes shower cholesterol crystals into the circulation—either spontaneously or, more commonly, following an endovascular procedure One may see cerebral transient ischemic attacks; livedo reticularis in the lower extremities; Hollenhorst plaques in the retina with visual field cuts; necrosis of the toes and acute glomerular capillary injury leading to focal glomerulosclerosis sometimes associated with hematuria, mild proteinuria, patients have fever, eosinophilia, or eosinophiluria. A skin biopsy of an involved area may be diagnostic. 52
- 53. Cholesterol Emboli There is no therapy to reverse embolic occlusions, and steroids do not help. Controlling blood pressure and lipids and cessation of smoking are usually recommended for prevention 53
- 54. Nephrotic Syndrome Nephrotic syndrome is kidney disease with proteinuria, hypoalbuminemia, and edema. Nephrotic range proteinuria is 3 grams per day or more. Nephrotic syndrome can be primary; being a disease specific to the kidneys, or it can be secondary, being a renal manifestation of a systemic general illness. In all cases, injury to glomeruli is an essential feature. 54
- 55. Primary causes of nephrotic syndrome include, in approximate order of frequency: 1. Minimal-change nephropathy 2. Focal glomerulosclerosis 3. Membranous nephropathy 4. Hereditary nephropathies Secondary causes include, again in order of approximate frequency: 1. Diabetes mellitus 2. Lupus erythematosus 3. Amyloidosis and paraproteinemias 4. Viral infections (eg, hepatitis B, hepatitis C, HIV) 5. Preeclampsia 6. Others: IgA nephropathy, Sickle cell disease. 55
- 56. Pathogenesis of edema 1. Hypoalbuminemia : lowers the plasma colloid osmotic pressure. 2. Renal sodium retention occurs because of the proteinuria. 3. Enhanced peripheral capillary permeability to albumin . 56
- 57. Metabolic consequences of proteinuria 1. Lipids are usually elevated: a) hypoproteinemia that stimulates protein, including lipoprotein, synthesis by the liver, and (b) diminution of lipid catabolism caused by reduced plasma levels of lipoprotein lipase. 2. Risk for venous thrombosis: The loss of antithrombin III and plasminogen via urine 3. Vitamin D–binding protein may be lost in the urine, leading to hypovitaminosis D. 4. Urinary immunoglobulin losses may lower the patient's resistance to infections 57
- 58. History Swelling of the face; this is followed by swelling of the entire body. Adults can present with dependent edema. Foamy urine may be a presenting feature. A thrombotic complication, such as deep vein thrombosis of the calf veins or even a pulmonary embolus. 58
- 59. Physical Edema , increase in weight, the development of ascites, or pleural effusions. Hematuria and hypertension manifest in a minority of patients. Features on exam will vary according to cause 59
- 60. Laboratory Studies Urinalysis is the first test used in the diagnosis of nephrotic syndrome. The serum albumin is classically low in nephrotic syndrome Urine protein electrophoresis. Serum tests for kidney function are essential. Ultrasonographic scanning Hepatitis B and C, HIV May require a renal biopsy for diagnosis 60
- 61. Management Specific treatment of nephrotic syndrome depends on the disease's cause. Hospitalization should be considered if there is respiratory distress, if a patient has tense scrotal or labial edema, in the presence of complication. Diuretics will be needed; furosemide (1 mg/kg/d) and spironolactone (2 mg/kg/d) will help when fluid retention is severe, provided no signs of renal failure or volume contraction are evident. And even metolazone may be used When the patient's serum albumin level is less than 1.5 g/dL. Albumin at 1 g/kg may be given, followed by intravenous furosemide. 61
- 62. With regard to infection, oral penicillin can be prescribed as prophylaxis for children with gross edema. Abdominal paracentesis should be performed if the patient develops signs of peritonitis. Anticoagulation has been advocated by some for use in preventing thromboembolic complications, but its use in primary prevention is of unproven value. Hypolipidemic agents may be used, but if the nephrotic syndrome cannot be controlled, there will be persistent hyperlipidemia. In secondary nephrotic syndrome, such as that associated with diabetic nephropathy. ACEI and/or ARB are widely used. These may reduce proteinuria by reducing the systemic blood pressure, by reducing intraglomerular pressure, and also by direct action on podocytes. 62
- 63. Diet: Diet should provide adequate energy (caloric) intake and adequate protein (1-2 g/kg/d). Supplemental dietary protein is of no proven value. A diet with no added salt will help to limit fluid overload. Management of hyperlipidemia could be of some importance if the nephrotic state is prolonged. Fluid restriction per se is not required. Activity: There are no activity restrictions for patients with nephrotic syndrome. Ongoing activity, rather than bedrest, will reduce the risk of blood clots. 63
- 64. Thank You 64