Heart failure
- 1. HEART FAILURE CLASSIFICATION, RISK FACTORS AND CLINICAL FEATURES GUIDE – Dr. L. S. PATIL PRESENTER – Dr DEEPAK R. CHINAGI
- 2. DEFNITION • 2013 ACC/ AHA DEFNITION- – Heart Failure is defined as “ a complex clinical syndrome that results from any structural or functional impairment of ventricular filling(diastole) or ejection of blood. (systole) ”
- 3. CLASSIFICATION BY DEFNITION • SYSTOLIC HEART FAILURE – Characterized by reduced ejection fraction and enlarged ventricle size. Clinically present with left ventricular failure and marked cardiomegaly. • DIASTOLIC HEART FAILURE – Characterized by increased resistance to filling due to increased filling pressures. Clinically present with pulmonary congestion with normal or slightly enlarged ventricles .
- 4. CLASSIFICATION BASED ON EJECTION FRACTION • Heart Failure with reserved Ejection Fraction HFrEF – Ejection fraction ≤ 40% . – These patients will have systolic dysfunction and concomitant diastolic dysfunction. Coronary artery disease is the major cause. • Heart Failure with Preserved Ejection Fraction HFpEF – Ejection Fraction 40 – 50%. – These patients can be diagnosed by 1)clinical signs and symptoms and 2)evidence of pEF or normal EF or previously rEF 3)evidence of abnormal LV diastolic dysfunction (echo / LV catheterisation)
- 5. CLASSIFICATION BASED ON CARDIAC OUTPUT • HIGH OUTPUT FAILURE- – The normal heart fails to maintain normal or increased output in conditions like anemia, hyperthyroidism, pregnancy. – Usually right sided failure occurs followed by left sided failure with presence of shortened circulatory time. • LOW OUTPUT FAILURE- – Heart fails to generate adequate output in conditions like cardiomyopathy, valvular heart disease, tamponade and bradycardia.
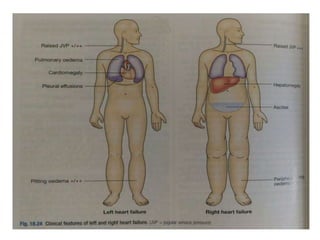
- 6. RIGHT AND LEFT SIDED HEART FAILURE • Right sided heart failure is characterised by the presence of peripheral edema, raised JVP and hypotension and congestive hepatomegaly. • Left sided heart failure – pulmonary edema is the striking feature. Other signs are tachypnea, tachycardia, third heart sound, pulsus alternans, cardiomegaly. • Congestive Cardiac Failure – Characterised by combination of both left and right sided heart failure.
- 8. FORWARD AND BACKWARD HEART FAILURE • FORWARD HEART FAILURE- – This results from inadequate discharge of blood into arterial system leading to poor tissue perfusion and excess Na+ reabsorption through RAAS. • BACKWARD HEART FAILURE- – This results from failure of one or both ventricles to fill normally and discharge its contents, causing back pressure on the atria and venous system.
- 9. ACCF/AHA FUNCTIONAL CLASSIFICATION • Stage A – At high risk of HF but witout structural hear disease. • Stage B – Structural heart disease without signs or symptoms of HF. • Stage C – Structural heart disease with prior HF or current HF. • Stage D – Refractory HF requiring special interventions.
- 10. NYHA FUNCTIONAL CLASSIFICATION • Stage 1 – no limitation of ordinary physical activity. • Stage 2 – slight limitation of ordinary physical activity. • Stage 3 – marked limitation of ordinary physical activity, but comfortable at rest. • Stage 4 – unable to carry out physical activity, symptomatic at rest.
- 11. RISK FACTORS • Epidemiology – – Worldwide 2 crore people are affected by heart failure. Approximate 2 % prevalence in developed countries. Women have better survival than men. – Coronary artery disease is the major cause for heart failure. (60 – 75%) • Etiology and Risk Factors – – Any condition that leads to alteration of LV structure and function can lead to heart failure
- 12. Etiologies of Heart Failure • HFrEF (EF < 40%) – – Coronary Artery Disease (Infarction/Ischemia) – Chronic Pressure Overload (Hypertension/ Valvular Heart Disease - Stenotic) – Chronic Volume Oveload(Valvular Heart Disease- Regurgitant/ Intracardiac shunting) – Non ischemic DCM (Familial/ Infiltrative/ Endocrine/ Toxic/ Inflammatory/ Peripartum/ Stress)
- 13. Etiologies of Heart Failure • HFpEF (EF 40 – 50%)- – Hypertrophic Cardiomyopathy – Hypertensive heart disease – Restrictive Cardiomyopathy(Amyloidosis / Sarcoidosis / Hemochromatosis) – Fibrosis / Endomyocardial Disorders / Aging • Right Heart diseases- – Cor pulmonale – Pulmonary Vascular disorders
- 14. Etiologies of Heart Failure • High output states – Thyrotoxicosis – Nutritional – Beriberi – Anemia
- 15. LV Remodeling • DEFNITION – It refers to change in LV Mass , Volume or Shape or the Composition of the heart after Cardiac injury or index event. • Progress of HF associated with changes in geometry of remodeled LV • Changes that occur include – – LV dilatation – LV thinning – Increase in LV end diastolic volume – Decrease in stroke volume
- 16. LV Remodeling – Subendocardial hypoperfusion – Increased oxidative stress and free radical generation – Stress activated hypertrophic signaling pathways – Incompitence of mitral valve apparatus and functional MR
- 17. CLINICAL FEATURES • Important symptoms – – Fatigue – Exertional Breathlessness • Cause of breathlessness is multifactorial – Pulmonary congestion due to LVF – Accumulation of interstitial and intra alveolar fluid , stimulating juxta capillary J receptors, causing Rapid Shallow breathing – Decreased pulmonary compliance – Increased airway resistance – Respiratory fatigue and Anemia
- 18. CLINICAL FEATURES • Orthopnea – – Dyspnea in recumbent position – Occurs due to redistribution of fluid from splanchnic circulation and lower extremities – Causes increase in pulmonary capillary pressure. – Nocturnal cough is usually asociated with this symptom – Relieved by sitting upright . – This symtom is more common in patients with co morbid obesity or ascites
- 19. CLINICAL FEATURES • Paroxysmal Nocturnal Dyspnea- – Defnition – it refers to acute episode of shortness of breath and coughing that generally occur at night and awken patient from sleep usually 1 – 3 hours after recline. – Associated with coughing or wheeze – Mechanism – increased pressure in bronchial arteries leading to airway compression (+) interstitial pulmonary edema = increased airway resistance. – Orthopnea symptoms resolve after upright posture, but symptoms of PND persist even after upright posture.
- 20. CLINICAL FEATURES • Cheyne stokes respiration – Also called periodic / cyclic respiration – It is present in nearly 40 % cases of HF – It is caused by decreased sensitivity of RESPIRATORY CENTRE to PaCO2. – Due to transient fall in PaO2 , rise in PaCO2 there is an apneustic phase. PaCO2 rises steadily till it stimulates depressed respiratory centre and causes hyperventilation and hypocapnia (low PaCO2).
- 21. CLINICAL FEATURES • Other symptoms like – Anorexia – Nausea – Early satiety – Abdominal pain – Abdominal fullness – Congestive hepatomegaly – Confusion , disorientation, sleep disturbances, – Nocturia
- 22. PHYSICAL EXAMINATION • Patient will present with laboured breathing in an acute LVF. He/she may not be able to finish the sentence due to shortness of breath. He / she may have difficulty to talk due to shortness of breath. • Blood pressure may be normal or high in early HF , may decrease consequently and is usually low. • Low pulse pressure (reduced stroke volume) • Sinus tachycardia (increased sympathetic activity) cool peripheries, cyanosis of tips of fingers and nail bed.
- 23. PHYSICAL EXAMINATION • Jugular venous pressure – – Indicates right atrial pressure – It is measured in terms of (cm of H2O) – Normal < 8 cm of H2O – Method – measure highest point of JVP vertically from sternal angle and add 5 cm of H2O – Positive Abdomino- Jugular reflex
- 24. PHYSICAL EXAMINATION • Respiratory system – Bilateral rales/crepitations may be present as a result of transudate of fluid from intravascular space to intraalveolar space. – May be accompanied by expiratory wheeze (cardiac asthma). – Pleural effusion may/may not be present. (common in CCF)
- 25. PHYSICAL EXAMINATION • Cardiovascular system – Apical impulse may shift inferiorly / laterally. – Sustained apical impulse is felt in severe LVH. – S3 gallop (protodiastolic gallop) can be heard. – Left parasternal impulse in cases if severe RVH – S4 gallop is usually present in diastolic dysfunction. – MR or TR may be present additionally.
- 26. PHYSICAL EXAMINATION • Per abdomen – Hepatomegaly is present (tender / pulsatile) – Pulsations in liver indicate tricuspid regurgitation – Ascites , Jaundice , raised liver enzymes – Peripheral edema can be pre tibial or pre sacral edema • Cardiac cachexia – Cause for cachexia is multifactorial • Elevation of BMR • Elevated circulating cytokines like TNF • Congestion of intestinal veins
- 27. Other Important Comorbidities in HF • Atrial Fibrillation • Anemia • Depression • Others – Diabetes – Arthritis – CKD – COPD
- 28. THANK YOU