Inflammatory Myopathies
- 1. INFLAMMATORY MYOPATHIES DR. Lohit Chauhan Monday, June 15, 2015
- 2. Introduction • Inflammatory Myopathies are sporadic disorders representing the largest group of acquired and potentially treatable causes of skeletal muscle weakness. • Annual incidence ~ 1 in 100,000 • Women > Men , Polymyositis (PM) and Dermatomyositis (DM) • Men > Women , Inclusion Body Myositis (IBM)
- 3. Introduction • Age at onset for Inflammatory myopathies is different. • PM > 18 years. • DM both Juvenile population and Adulthood. • IBM affects persons aged >50 years.
- 4. Introduction • In 1888 the first American biopsy documented polymyositis in ruling out Trichinella. • Heliotrope rash was first described in 1875 in france. • In 1930 Gottron reported skin lesions . • In 1967 the pathology of IBM was described.
- 5. Classification • There is no internationally accepted classification system for Inflammatory myopathies. • For discussion purpose IM’s can be classified as :- • Polymyositis. • Dermatomyositis • Inclusion Body Myositis. • Autoimune Necrotising Myopathies. • Myositis associated with Collegen Vascular disorder. • Myositis associated with malignancy and Juvenile Dermatomyositis.
- 6. Clinical Features Polymyositis • A rare, subacute inflammatory myopathy affecting adults and rarely children. • Progressive, symmetric proximal muscle weakness with sparing of ocular and facial muscles. • Pharyngeal and Neck Flexors, also involved causing dysphagia and Head drop.
- 7. Clinical Features Polymyositis • Associated with Myalgia and Muscle tenderness in some cases • In Advanced and Acute cases Respiratory muscles may be affected. • Severe weakness if untreated leads to muscle wasting. • Sensations and DTR’s remain intact.
- 8. Clinical Features Dermatomyositis • Subacute inflammatory myopathy with muscle weakness similar to polymyositis with distinctive rash more often preceding the muscle weakness.
- 9. Clinical Features DM : Dermatologic Manifestations Heliotrope rash • Periorbital violaceous erythema with or without edema of eyelids and periorbital tissue. • Highly characteristic of DM.
- 10. Clinical Features DM : Dermatologic Manifestations Gottron Papules • Violaceous flat topped papules and plaques over dorsal aspect of interphalengeal and MCP joints • Pathognomic of DM, seen in > 80% patients with DM
- 11. Clinical Features DM : Dermatologic Manifestations V- sign • Macular violaceous erythema over V-shaped region of the neck and upper chest. • Sometimes rash is pruritic.
- 12. Clinical Features DM : Dermatologic Manifestations Shawl Sign • Macular violaceous erythema over Nape,back and shoulders. • May show photosensitivity.
- 13. Clinical Features DM : Dermatologic Manifestations Mechanic’s Hand • Also considered characteristic. • hyperkeratosis, scaling, and horizontal fissuring of the palms and fingers bilaterally. • Can be a manifestation of the antisynthetase syndrome.
- 14. Clinical Features DM : Dermatologic Manifestations Nailfold Talengectasia • Occur in 30 to 60 % early in disease.
- 15. Amyopathic and Hypomyopathic Dermatomyositis • Amyopathic DM : present with typical dermatological manifestations of DM, with normal muscle strength, enzyme levels and EMG findings. • Hypomyopathic DM : Dermatological manifestations of DM with no muscle weakness with mild elevation in Enzymes and Abnormal EMG & Biopsy.
- 16. Juvenile Dermatomyositis Presents with clinical features similar to dermatomyositis with following differences • Age of onset ~ 7 years • Less incidences of Malignancy and ILD. • Increased risk for Vasculopathy, Lipodystrophy and calcinosis. • Associations: SoJIA ; Macrophage activation syndrome • Less mortality.
- 17. Inclusion Body Myositis • Symmetric or asymmetric weakness. • Insidious onset. • After 50 years, Male to female ratio of 3:1. • Proximal and/or distal muscle involvement. • Classically forearm flexors, finger flexors and Quadriceps. • Facial and Pharyngeal muscles are more commonly involved than PM/DM.
- 18. Immune-Mediated Necrotizing Myopathy • Subacute progressive proximal muscle weakness without a rash. • Female to Male ratio 2:1. • Generally develops more rapidly than with PM, and is markedly severe. • Associated myalgia and dysphagia can be seen. • Associated with Paraneoplastic syndrome and Statin use.
- 19. Paraneoplastic NM • Rare, rapid progression, association with Adenocarcinoma. • Age > 40 years. • Presentation in Fall or Winter. • Antibodies against signal recognition particles (SRP) seen. • Coexisting cardiomyopathy and ILD maybe present. • Muscle Biopsy : Necrotic fibres infiltrated by macrophages and rare T-cells.
- 20. Statin Induced Autoimmune NM (SANAM) • Associated with statin use. • Age ~ 46 to 89 years. • Progress beyond 3 to 6 months after drug discontinuation. • Require immunosuppresive therapy.
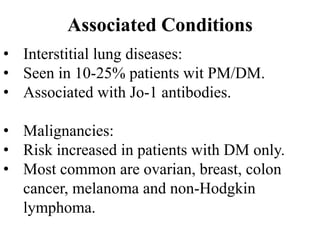
- 21. Associated Conditions • Interstitial lung diseases: • Seen in 10-25% patients wit PM/DM. • Associated with Jo-1 antibodies. • Malignancies: • Risk increased in patients with DM only. • Most common are ovarian, breast, colon cancer, melanoma and non-Hodgkin lymphoma.
- 22. Associated Conditions Deforming arthritis of anti Jo-1 antibody patient.
- 23. Characteristic Polymyositis Dermatomyositis Inclusion body Myositis Age at onset >18 years Adulthood and childhood >50 years Familial associations No No Yes, in some cases Extramuscular Manifestations Yes Yes Yes Associated Conditions Connective tissue diseases Yes Scleroderma and mixed connective tissue disease (overlap syndromes) Yes, in up to 20% of cases Systemic autoimmune diseases Frequent Infrequent Infrequent Malignancy No Yes, in up to 15% of cases No Drugs Yes Yes, rarely No Parasites and Bacterias Yes No No Viruses Yes Unproven Yes Features Associated with Inflammatory Myopathies
- 24. Pathogenesis • Both immune and non immune mechanism are involved in pathogenesis. • Immune mechanism involve T-cell, B-cells Dendritic cells, macrophages, cytokines and Antibodies. • Non immune mechanisms involve endoplasmic reticulum stress , hypoxia and Autophagy.
- 25. Immune Mechanism • Immune Activators trigger disease in myositis susceptibility gene carriers. • Environmental factors may contribute
- 26. Immune Mechanism • Innate and Adaptive responses are activated in Lymph nodes
- 27. Immune Mechanism Activated immune cells enter general circulation, and encounter with specific antigen and penetrate endothelia into local muscle
- 28. Immune Mechanism In PM and IBM CD8+ Tcells expressing perforin 1 and Granzyme invade muscle fibres expressing MHC 1 molecule leading to muscle inflammation and necrosis ( In IBM).
- 29. Immune Mechanism In DM; CD4+ T cells , B-cells , Dendritic cells and Macrophages invade perivascular and perimysial muscle tissue.
- 31. Antisynthetase syndrome • Aminoacyl-tRNA synthetase is a cytoplasmic enzyme involved in aminoacylation. • The most common ARS is histidyl-RNA- synthetase, also called Jo-1
- 32. Antisynthetase syndrome • Myositis : Polymyositis or dermatomyositis • Non-destructive polyarthritis of finger joints, wrists, elbows or knees • Fever in 80% of patients • Mechanic’s hands : Thick cracked skin over the tips and sides of the fingers • Interstitial lung disease in over 70% of patients • Raynaud phenomenon in 60% of patients
- 33. Other Myositis Specific Autoantibodies
- 34. Anti-PM-Scl antibodies • Directed against a nucleolar macromolecular complex. • Primarily polymyositis or dermatomyositis /scleroderma overlap. • Strongly associated with HLA-DR3. • Seen in 5-25% of patients with myositis.
- 35. Non Immune Mechanism HMGB1 : High mobility group protein B1
- 36. Diagnosis • In 1975, Bohan and Peter used the following criteria for the diagnosis and classification of PM and DM. The Bohan and Peter classification criteria 1. Symmetric proximal muscle weakness. 2. Elevation of skeletal muscle enzyme levels. 3. Abnormal EMG results - Polyphasic, short, small motor unit potentials; fibrillation; positive sharp waves; insertional irritability; and bizarre, high-frequency, repetitive discharges. 4. Muscle biopsy abnormalities -Degeneration/regeneration, perifascicular atrophy, necrosis, phagocytosis, fiber size variation, and mononuclear inflammatory infiltrate 5. Typical skin rash of DM
- 37. Drawbacks of Bohan and Peter criteria • Case series and data developed from a single institution and based on clinical observations. • Only skin features were used to differentiate DM from PM. • IBM was not recognized as a separate entity.
- 38. New Diagnostic Criteria • New diagnostic criteria considers : 1. Muscle Weakness. 2. Creatine Kinase 3. Electromyographic Findings. 4. Muscle biopsy. 5. Rash / Calcinosis.
- 39. Muscle Weakness • In PM and DM there is progressive, symmetric proximal muscle weakness with sparing of ocular and facial muscles. • In IBM : Symmetric or asymmetric weakness, involving the proximal and/or distal muscles classically forearm flexors, finger flexors and quadriceps.
- 40. Muscle Enzymes • In PM, Creatine Kinase is always elevated upto 5 – 50 times the ULN. • In DM, CK is elevated upto 50 times the ULN, in 90% of patients. While in others CK levels may be normal. • In IBM, CK levels are elevated upto 10 times of UNL or may be Normal. • Necrotising Myopathy, CK is increased 10 times or more.
- 41. EMG in Myopathies • In acute myopathies EMG must be conducted about 3 weeks from the onset of symptoms to ensure good sensitivity. • EMG of the muscle is done in two situations : at rest and at voluntary activity. • The Resting values also called spontaneous activity ( not seen in normal muscles) are of three types. 1.Fibrillations and Positive waves 2.High frequency discharges 3.Myotonic Discharges
- 42. EMG in Myopathies • Fibrillations and Positive waves These are small positive rhythmic electric potential typical of denervation.
- 43. EMG in Myopathies • High frequency discharges (Pseudomyotonic or Complex repetitive discharges) . Rhythmic electric potential with abrupt beginning and end typical of long standing denervation.
- 44. EMG in Myopathies Myotonic Discharges . Electrophysiological representations of difficulty of relaxation following voluntary muscle contraction.
- 45. EMG in Myopathies • During Voluntary activity motor unit potentials (MUP) ie. are recorded and MUP phase are studied • ≥5, phases are called polyphasic. • Acute myopathy: MUP are small in amplitude, short duration and polyphasic. • Chronic myopathy: MUP are large and of longer duration.
- 46. EMG in Myopathies • EMG in IM show • Increased insertional and spontaneous activity. • Small-amplitude low-frequency fibrillation potentials and positive sharp waves. • Occasionally pseudomyotonic and complex repetitive discharges indicating chronicity. • Electrical myotonia : SANAM. • Helpful in assessing relapse during treatment with corticosteroids.
- 47. Muscle biopsy in Polymyositis Endomysial inflammatory infiltrate (CD8+ MHC1 complexes) surrounding and invading non-necrotic muscle fibers, with no vacuolization.
- 48. Muscle biopsy in Dermatomyositis Perifascicular and Perivascular infiltrates with perifascicular atrophy.
- 49. Inclusion body myositis Basophilic rimmed vacuoles Vacuole filled with granules Vacuolated muscle fibres infiltrated with CD8/MHC-1complexes. Beta-amyloid deposits and cytochrome oxidase negative fibres may be seen.
- 50. Necrotizing Myopathy Scattered necrotic myofibres with myophagocytosis in the paucity of T-lymphocytic infiltration.
- 51. Diagnostic criteria for IM Polymyositis Criterion Definite Probable Dermatomyositis Inclusion Body Myositis Myopathic muscle weakness Yes Yes Yes Yes; slow onset, early involvement of distal muscles, frequent falls EMG findings Myopathic Myopathic Myopathic Myopathic with mixed potentials Muscle enzymes Elevated (up to fiftyfold) Elevated (up to fiftyfold) Elevated (up to fiftyfold) or normal Elevated (up to tenfold) or normal Muscle biopsy findings "Primary" inflammatio n with the CD8/MHC-I complex and no vacuoles Ubiquitous MHC-I expression but minimal inflammati on and no vacuoles Perifascicular, perimysial, or perivascular infiltrates, perifascicular atrophy Primary inflammation with CD8/MHC-I complex; vacuolated fibres with -amyloid deposits; cytochrome oxygenase–negative fibers; signs of chronic myopathy Rash or calcinosis Absent Absent Present Absent
- 52. Other Investigations • MRI-T1-weighted, T2-weighted, and sequences using fat suppression techniques and short “tau” inversion recovery (aka STIR), provides useful information to: – diagnose myositis – monitor treatment response, – and identify a muscle site for biopsy. • Muscle biopsy guided by MRI contains significantly more inflammatory cells than the biopsy taken from MRI non-affected sites.
- 53. STIR imaging show fibrosis or diffuse or patchy signal symmetric increase in the proximal muscles and intramuscular fascia indicative of muscle oedema due to inflammation.
- 54. Other Investigations Malignancy work up (for DM and PM) • Chest , Abdomen and Pelvic CT scans • Mammogram, Breast and Pelvic examination in women • Colonoscopy in patients – Age >50 years or in those with GI symptoms.
- 55. Other Investigations In patients with IM: • Chest X-ray, PFT and HRCT – especially in Jo1 positive patients to rule out ILD. • ECG- for myocardial involvement • Echocardiogram- in patients with symptoms and signs of heart failure. • Video fluoroscopy- to objectively assess swallowing in patients with dysphagia.
- 56. Treatment Goals • To eliminate inflammation. • To restore muscle performance. • To prevent chronic muscle disease. • To prevent other organ system damage • To regain quality of life.
- 58. Prednisone, 0.5-1 mg/kg/day. for 2-4 wk Concurrent with: Initial Treatment Approach
- 59. Prednisone, 0.5-1 mg/kg/day. for 2-4 wk Concurrent with: MTX, 15 mg/wk, to Target dose of 25 mg/wk Mycophenolate mofetil, 500 mg Twice daily. Increase by 500 mg/wk until 1000 mg twice daily Azathioprine, 2 mg/kg IBW Twice daily Initial Treatment Approach
- 60. Prednisone, 0.5-1 mg/kg/day. for 2-4 wk Concurrent with: MTX, 15 mg/wk, to Target dose of 25 mg/wk Mycophenolate mofetil, 500 mg Twice daily. Increase by 500 mg/wk until 1000 mg twice daily Azathioprine, 2 mg/kg IBW Twice daily Taper prednisone every 2 wk until completed: 60mg/d 40mg/d 30mg/d 25mg/d 20mg/d 17.5mg/d 15mg/d 12.5mg/d 10mg/d 7.5mg/d 5mg/d 2.5mg/d Initial Treatment Approach
- 61. Treatment Initiate treatment with high dose corticosteroids and steroid sparing agents. • Prednisolone – Dose 0.5 to 1 mg/kg/day for 2- 4 weeks and then taper off. • Duration : 3 to 6 months. • If no objective benefits after 3 months of high dose therapy switch over to next immunosuppresive drug. • Long term use of steroids may lead to steroid myopathy.
- 62. Treatment • Azathioprine : Dose 2 mg/kg/day for 3 months. • Before starting Azathioprine patients thiopurine- methyl-transferase levels should be checked, otherwise it may lead to myelosuppression. • Side Effects : Nausea, Loose stools, fever, and Liver toxicity
- 63. Treatment • Methotrexate : Initial dose of 15 mg orally once weekly to a target dose of 25 mg once weekly within 3 to 6 months. • Folic acid supplementation to be given along. • Side Effects : BM suppression, Liver toxicity, Pneumonitis. • Should be used cautiously in patients with ILD.
- 64. Treatment • Mycophenolate Mofetil (MMF) : initial dose of 500mg BD to a dose of 1000mg BD over 4 weeks. • Side Effects : Nausea, Loose stools, Leukopenia, elevation in liver enzymes and Teratogenicity. • Concurrent treatment : In Patients with ILD or on Prednisolone or Immunosuppressive agents TMP-SMX prophylaxis is given for Pneumocystis.
- 65. Treatment Monitoring • Within 2 to 4 weeks of starting MTX or azathioprine, a complete blood cell count, liver enzyme function tests, and creatinine measurement should be obtained once a month for 3 consecutive months. • Once a stable dosage is achieved, laboratory follow-up every 2 to 3 months thereafter is appropriate. • DEXA scan is obtained at Baseline and Every year while patients receive steroids.
- 66. Severe and Refractory IM • Myopathy refractory to conventional therapy or with severe organ-threatening manifestations like ILD, severe dysphagia, notable weight loss, severe rash, or weakness.
- 67. Methylprednisolone, 500-1000 mg/d IV (10-30 mg/kg/ day in JDM), for 1-3 days IVIG, 1 g/kg (divided doses over 1-2 days) Repeated once monthly for 1-6 months CPM, 0.6-1.0 g/m2 IV every 4 Wk or 1-2 mg/kg/day orally, for 3-12 months Rituximab, 1000 mg repeated on day 15, Or 375 mg/m2 once weekly for 4 wk CSA, 3.0-3.5 mg/kg/day Treatment of refractory IM or severe organ-threatening IM
- 68. Treatment : IBM • Treat patients of IBM with immunosuppression using the same algorithms as used for DM and PM • Goal is to suppress muscle inflammation, although the disease typically is resistant to standard immunotherapy.
- 69. Treatment : JDM • Begin Prednisone at 2mg/kg to a max of 60mg/day. • Subcutaneous MTX, at 15 mg/m2 once weekly is added at the onset.
- 70. Special Considerations Therapy for Skin disease. • Avoid UV rays. • Judicious use of Sunscreen with SPF of > 50. • Topical steroids and Tacrolimus. • Hydroxychloroquine at 200mg BD. • For refractory cases MMF can be used.
- 71. Special Considerations Therapy for Calcinosis. • Not satisfactory • Drugs used are • Diltiazem • Colchicine • Bisphosponates • Intralesional Steroids. • Abatacept • Sodium Thiosulphate
- 72. Prognosis • Older studies (before the availability of steroids) revealed a 50% mortality from complications. • Current estimates of mortality, excluding patients with malignancy, is less than 10% at 5 years after initial diagnosis. • DM has a favorable prognosis among all, IBM has least favorable prognosis.
- 73. Poor prognostic factors • Older age • Malignancy • Delayed steroid treatment • Dysphagia with aspiration • ILD
- 74. Take Home Message • Inflammatory myopathies should be considered in all patients with proximal muscle weakness. • Diagnosis is made by Clinical findings, raised CPK, typical EMG and muscle biopsy findings. • Treatment is by immunosuppression. • Prognosis is generally good for DM and worst for IBM.