leukemias.ppt
- 1. Leukemia
- 2. Leukemia
- 3. About the Disease Leukemia, lymphoma and myeloma are cancers that originate in the bone marrow (leukemia & myeloma) or in lymphatic tissues (lymphoma).
- 4. Different Types of Blood Cancers Leukemia Non-Hodgkin Lymphoma Hodgkin Lymphoma Myeloma Myelodysplastic Syndromes
- 5. What is Leukemia? Leukemia is cancer found in the blood cells There are many types of Leukemia They are classified by how quickly they progress and what type of cell they affect Leukemia is causes when there is an imbalance of healthy unhealthy blood cells in the body This occur when one cell awry and the body begins to produce large numbers of this cell
- 6. What Is Leukemia? Cancer of the white blood cells Acute or Chronic Affects ability to produce normal blood cells Bone marrow makes abnormally large number of immature white blood cells called blasts
- 7. What is Leukemia Greek word which means “white blood” Leukemia is when cells spread rapidly and destroy living tissue. It grows/invades the bone marrow which is the factory of blood and replaces normal blood elements with cancer cells. Cancer cells replace all bone marrow cells which causes infection and bleeding problems. Leukemia is basically white blood cells that don’t work well and cause trouble.
- 8. Continued Millions of immature and useless white blood cells are produced which makes it harder to kill cancer cells and preserve the good/healthy ones. Leukemia causes change in cells, DNA, and gene. If the blood matches with donator then you are curried. Bone marrow is spongy tissue that fills in the center core of bone. There are 4 different types of Leukemia.
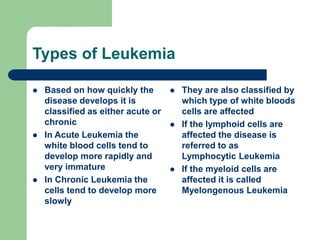
- 9. Types of Leukemia Based on how quickly the disease develops it is classified as either acute or chronic In Acute Leukemia the white blood cells tend to develop more rapidly and very immature In Chronic Leukemia the cells tend to develop more slowly They are also classified by which type of white bloods cells are affected If the lymphoid cells are affected the disease is referred to as Lymphocytic Leukemia If the myeloid cells are affected it is called Myelongenous Leukemia
- 10. Types of Leukemia Acute lymphoblastic Leukemia (ALL) Acute myeloblastic Leukemia (AML) Chronic lymphocyte Leukemia (CLL) Chronic myeloid Leukemia (CML)
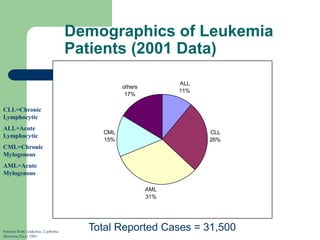
- 11. Demographics of Leukemia Patients (2001 Data) ALL 11% CLL 26% AML 31% CML 15% others 17% Total Reported Cases = 31,500 Sources from Leukemia, Lyphoma, Myeloma Facts 2001 CLL=Chronic Lymphocytic ALL=Acute Lymphocytic CML=Chronic Mylogenous AML=Acute Mylogenous
- 12. Chronic and Acute Chronic Leukemia: Progress slowly (runs a slow course) Not immediately fatal. Acute Leukemia: Progress rapidly (runs a fast course) Life expectancy short without treatment.
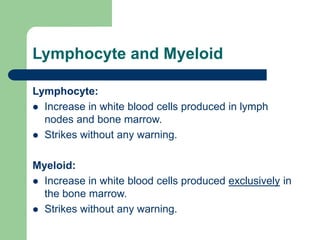
- 13. Lymphocyte and Myeloid Lymphocyte: Increase in white blood cells produced in lymph nodes and bone marrow. Strikes without any warning. Myeloid: Increase in white blood cells produced exclusively in the bone marrow. Strikes without any warning.
- 14. Acute Myeloid Leukemia (AML): Mixed group of disease It means “marrow like” and in this context it simply means arising from developing blood cells. This type of leukemia runs a rapid course.
- 15. Acute Lymphoblast Leukemia (ALL): Group of different diseases A complexity of which is still trying to be unraveled Reached a point where not all are being treated the same. This type of Leukemia runs a rapid course.
- 16. Chronic Myeloid Leukemia (CML): Characterized by increased production of granulocytes in the bone marrow. Usually associated with a specific chromosomal abnormality called the Philadelphia chromosome Progresses slowly
- 17. Chronic Lymphocyte Leukemia (CLL): This type of cancer is so rare it could be said not to arise at all in the first two decades of life. Starts of in the Bone marrow This type of cancer runs a slow course giving more time to live.
- 18. Risk Factors As of now we do not know the exact cause of Leukemia Exposure to these have been identified as risk factors High energy radiation Some genetic syndromes People working with chemical benzene for a long period of time
- 19. Causes High level radiation/toxin exposure Viruses Genes Chemicals Mostly unknown Can’t be caught
- 20. Development of Leukemia in the Bloodstream Stage 1- Normal Stage 2- Symptoms Stage 3- Diagnosis Stage 4- Worsening Stage 5a- Anemia Stage 5b- Infection Legend White Cell Red Cell Platelet Blast Germ Sources from Leukemia, by D. Newton and D. Siegel
- 21. Effects On the Body Attacks the immune system Infections Anemia Weakness No more regular white blood cells, red blood cells, and platelets Blasts clog blood stream and bone marrow
- 22. Symptoms When there are excessive white blood cells - -> Infections When there are few red blood cells: Paleness --> Anemia When there are few platelets --> Excessive bleeding
- 23. Signs Of Leukemia Most of the symptoms of leukemia are similar to those of a common illness such as the flu. The symptoms will vary according to the type of leukemia. Tired Frequent infections Easy bruising or bleeding Bone tenderness Headache Enlarged lymph nodes Low red blood count Pale skin Poor appetite
- 24. Tests For Diagnosis Finger prick Blood sample Blood dye Bone marrow sample Spinal Tap/Lumbar Puncture
- 25. Diagnosis As immature cells increase in the body leads to lower amounts of red blood cells and platelet cells The low amounts of red blood cells cause patient to be tired and pale Low amounts of platelet cells cause the patient to easily bruise or bleed During a physical exam the doctor detects swollen spleen, liver, or lymph nodes Then there is a blood test conducted to see if it is leukemia The type of Leukemia is determined after bone marrow is extracted and tested
- 26. Diagnosis Most commonly leukemia is diagnosed by a blood test to count the number of red cells, white cells and platelets. A biopsy of the bone marrow may also be performed
- 27. Pictures Of Blood Normal human blood White Cell Red Cell Platelet Blood with leukemia Blasts Red Cell Platelet White Cell Sources from Arginine.umdnj.edu Sources from beyond2000.com
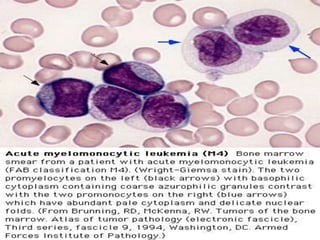
- 29. Diagnosis Requires all of the following diagnostic components: a) Documentation of bone marrow infiltration b) Myeloid origin of the leukemic cells c) FAB/WHO classification of the leukemia d) Karyotypic analysis
- 30. Differential Diagnosis chronic myelogenous leukemia other myeloproliferative disorders reactive leukocytosis: leukemoid reaction acute leukemia
- 33. BCR-ABL p210 Fusion Protein Activity Higher tyrosine kinase activity. – Increases progenitor cells, reduces the pool of stem cells. Semin Hematol 1988;25:1-19. – Defective cytoadherence. Hematol Oncol Clin North Am 1988;12:1-29. – Suppression of apoptosis. Blood 1994;83:1575-85.
- 34. BCR-ABL p210 Fusion Protein Evidence of its role in CML In vitro: cause factor-independent, leukemogenic cell growth in hematopoietic cell lines. In vivo: generate in mice CML-like syndrome. Science 1990;247:824-30.
- 35. FAB Classifications M0: minimally differentiated M1: without maturation M2: with maturation. May have t(8;21) translocation. M3: promyelocytic. Good prognosis. Can be associated w/ t(15;17). M4: myelomonocytic; assoc. w/ t(16;16) or inv(16)(p13q22). M5: monoblastic M6: erythroleukemia M7: megakaryoblastic. Poor overall survival.
- 45. Clinical Course Median survival: 3.5~8 yr. Chronic phase: 3~4 yr. Accelerated phase (15%): 3~6 mo, then enters acute phase. Acute phase (blast crisis), 25% in each year, findings: blasts > 30%, cytogenetic changes other than Ph chromosome, progression likes acute leukemia. 70% enters AML, 30% ALL.
- 46. Prognosis “Good risk”: favorable karyotype, including t(8;21), t(15;17), inv(16)/t(16;16)/del(16q) or FAB subtype M3 “Poor risk”: adverse karyotype or resistant disease after first course of chemo (i.e. >15% blasts in post-tx bone marrow bx) 5-yr survival for good, standard, and poor risk patients 70, 48, and 15% respectively. Relapse rates are 33, 50, and 78% respectively.
- 47. Treatment As of yet there is no cure for Leukemia Many advances have been made in the past couple years The survival rate of children with Acute Lymphocytic is around 82% Treatments include: Chemotherapy Radiotherapy Immunotherapy Bone marrow transplant
- 48. Research New drugs Cord blood and planceta
- 49. Treatment Depending on the type of cancer treatments may vary. Treatments of leukemia may include chemotherapy, radiation therapy, or bone marrow transplant. They also treat leukemia patients with the infusion of healthy blood cells and platelets. During and after the treatment blood counts are done to see if the patient is being controlled or in remission.
- 50. Treatments Blood and marrow stem cell transplantation. Research. Development of new drugs. Immunotherapy. Vaccines. Reversal of multidrug resistance. Gene therapy.
- 51. Management (1) Chronic phase – Hydroxyurea or busulfan, relieves symptoms and control of disease. – Interferon-a: 20% cytogenetic response, prolongation of survival. . It can gain 20 more months survival than C/T. This advantage must be weighed against its significant side effects.
- 52. Management (2) BMT or PBSCT Allogeneic bone marrow transplantation in the chronic phase is the only therapy known to cure CML 5YS > 50%, relapse < 20%, 20~40% BMT related death in the first year. It should be done as soon as possible for patients – Chronic phase. – <50 years old. – Has an HLA-identical sibling.
- 53. Management (3) STI571 STI 571:Inhibitors of the BCR-ABL fusion proteins (tyrosine kinase) After six months of therapy with Glivec (STI571), preliminary findings showed that half of 290 patients tested were improving. They had what's known as a cytogenic remission -- a reduction in the 'Philadelphia Chromosome' which causes the disease. "In these patients we found a very high response rate, there was some response seen in 91 percent of the patients," said Dr. Talpaz of the M.D. Anderson Cancer Center. "Some of the patients returned to the chronic phase of the disease."
- 54. Allogeneic Stem Cell Transplantation eradicates of the marrow cells (marrow- ablating C/T or R/T) implantation of allogeneic stem cells homing of the stem cells to the marrow cavity growth of the stem cells and recovery of the blood cells
- 55. Complications of SCT rejection, graft failure graft-versus-host disease infection VOD obliterative bronchiolitis sepsis relapse of disease
- 56. GVHD (Graft versus Host Disease) Immunologic reaction of donor lymphocytes to “foreign” antigens present on the surface of host cells “foreign” antigens: – HLA antigens – “minor” antigens not detected by current typing techniques
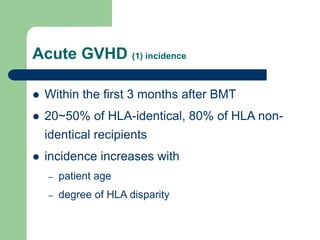
- 57. Acute GVHD (1) incidence Within the first 3 months after BMT 20~50% of HLA-identical, 80% of HLA non- identical recipients incidence increases with – patient age – degree of HLA disparity
- 58. Acute GVHD (2)manifestations Histology: lymphocytic infiltration of the epidermis and GI tract fever dermatitis: diffuse macular dermatitis, bullas, desquamation enteritis: cramping abdominal pain, watery to bloody diarrhea hepatitis: jaundice, cholestasis, hepatocellular necrosis infection: frequently related to mortality hyperacute GVHD (no prophylaxis): 7 days after BMT: exfoliative dermatitis, shock, hyperpyrexia
- 59. Chronic GVHD (1) incidence develops > 3 months after BMT 20~50% of allografts, usually following acute GVHD 20~30% develops de novo, without prior acute GVHD
- 60. Chronic GVHD (2) manifestations like collagen diseases skin: pigmentation, sclerosis mucosa: lichenoid oral plaque, esophagitis, polyserositis, oral and eye sicca syndrome liver: elevated ALP and GOT in 90% cases chronic wasting due to anorexia chronic pulmonary disease: 10~20% (diffuse interstitial pnuemonitis and obliterative bronchiloitis) death usually caused by infection, low mortality related to de novo onset & less tissue involvement.
- 61. Blast Crisis 30% ALL, 70% AML Treatment likes de novo acute leukemia with poor success. Chance of achieving remission is possible in ALL, which may last 4~8 months, but low in AML. Survival is usually 2~4 months.
- 62. CML in Blast Crisis