Lupus 2.0
- 2. PATHOGENESIS • Lupus nephritis develops in individuals with an unfortunate combination of genetic variants that compromise the maintenance of immune tolerance to endogenous nuclear material. • The consequence of tolerance loss is autovaccination and lifelong persistence of antinuclear antibodies (ANA), indicating persistently active autoreactive T- and B-cell clones. • Only a subset of patients develops clinical symptoms, often upon (viral) infections or hormonal influences that provide an unspecific stimulus for the expansion of these autoreactive lymphocyte clones. • The symptoms depend on interferon-alpha release, hence they are unspecific just as in any viral infection. • A further subset of patients develops organ manifestations such as lupus nephritis, which depends on the presence of additional susceptibility genes, some of which affect the kidney itself, whereas others drive persistent systemic inflammation and autoimmunity.
- 4. AUTOVACCINATION • The main pathogenesis of SLE is the loss of immune tolerance to nuclear autoantigens • SLE is usually not monogenic but is a polygenic disorder inherited as a Mendelian trait. • SLE patient has overt autovaccination/immunization to nuclear material exemplified by the presence of antinuclear antibody. • The concept of autovaccination -the immune systems will remain primed like after any other vaccine shots, and so there is no cure for SLE but lifelong monitoring and suppression of autoimmune disease activity are necessary.
- 5. PSEUDOANTIVIRAL IMMUNITY • Loss of immune tolerance and antinuclear antibodies production does not necessarily produce any clinical symptoms • Immune recognition of endogenous nucleic acids via Toll-like receptors 7 and 9 induces interferon alpha dependent antiviral immunity, which manifests clinically as fatigue, fever, arthralgia, and myalgia, as may be seen in any viral infection- PSEUDOANTIVIRAL IMMUNITY • SLE activity can be influenced by environmental factors that contribute to DNA unmasking (certain drugs) and massive cell death (ultraviolet light), or that provide an unspecific immunostimulatory effect to autoreactive lymphocyte clones (infections)
- 6. ORGAN DAMAGE • The risk of an SLE patient developing LN depends on additional genetic variants that create a predisposition for significant renal damage during the systemic autoimmune state • Some gene variants may promote mesangial cell proliferation; others affect basement membrane stability or the functions of integrin-alpha Such additional “weaknesses” or susceptibility factors determine whether a patient develops signs of nephritis. • Immune complex glomerulonephritis in SLE can present in different ways depending on the primary site of immune complex deposition
- 7. • IC form in situ via the recognition of intrarenal lupus autoantigens in the mesangium, subendothelial space, or outside the glomerular basement membrane between podocyte foot processes. • Once formed, immune complexes activate complement, which can injure adjacent cells, leading to either mesangial LN (class I, II), endothelial-proliferative LN (class III, IV), nephrotic syndrome (class V)
- 8. Kidney Disease In SLE Other Than Immune Complex Glomerulonephritis Thrombotic microangiopathy- secondary Antiphospholipid Antibody Syndrome Podocytopathies Steroid-induced diabetes or atherosclerosis, leading to diabetic nephropathy or renovascular disease
- 9. LUPUS IN MALE Less common Men with lupus have a more complex clinical course than women Higher mortality in one year than women More seizures, immune-mediated anemia (low hemoglobin level) and lupus anticoagulant level that may lead to thrombogenesis Fertile, sexually active and have normal reproductive history Kidney involvement-Higher prevalence, poorer renal outcome, and poorer overall survival rate Higher prevalence of Class IV, diffuse proliferative nephritis (DPGN)
- 10. LUPUS IN PREGNENCY Normal pregnancy, • The number of CD4+/CD25+ regulatory T cells (Tregs) is increased • Potent immunosuppressive action and contribute to fetal tolerance • Shift from a Th1 cell-mediated to a Th2 antibody- mediated immune response (commonly referred to as Th2 polarization) Lupus with Pregnency • Fewer Tregs that also are functionally defective - increased risks for pre-eclampsia and maternal and fetal morbidity • In the setting of Th2 polarization, Th2-mediated diseases, such as SLE, may worsen during pregnancy. • The risk for disease flare may be further enhanced by the hormonal changes of pregnancy (Estrogen) • Secondary Antiphospholipid Syndrome
- 11. DRUG INDUCED LUPUS Type B (hypersensitivity) reaction Drug induced lupus is uncommon GN is uncommon but has been reported with hydralazine, sulfasalazine, PTU, penicillamine and anti–TNF-α therapy Antihistone antibodies are common in DIL
- 12. Drug Clinical Features Laboratory Features Positive Antibody Tests Hydralazine Rash, fever, myalgias, pleuritis, polyarthritis nephritis <10% Anemia, leukopenia ANA, anti-dsDNA, ANCA, antihistone Procainamide Polyarthritis, polyarthralgias serositis nephritis <10% Anemia Anti-dsDNA, antihistone, anticardiolipin TNF-α inhibitors (etanercept/adalimumab/i nfliximab Systemic symptoms predominant (nephritis in 7%); skin manifestations dominate Thrombocytopenia, hypocomplementem ia ANA, anti-dsDNA, antinucleosome, anticardiolipin
- 13. ANA ANA's are a heterogenous group of circulating immunoglobulins that include IgM, IgG, and IgA. These immunoglobulins react with the whole nucleus in host tissue, and they are true autoantibodies. ANA's have no organ or species specificity and are capable of cross- reacting with nuclear material from human or various animal tissues. Each immunoglobin is composed of two heavy chains and two light chains. Light chains contribute to antigen binding and heavy chain regions determine antibody isotype ( IgM, IgD, IgG, IgA, or IgE). In lupus patients the light and heavy chains may no longer be autoreactive and eliminate a high percentage of autoreactive B-cells, which are responsible for producing antibodies.
- 15. LUPUS PODOCYTOPATHY • A patient with SLE, presenting with nephrotic syndrome and kidney biopsy findings of • Normal glomeruli or focal segmental glomerulosclerosis (FSGS) lesions (with or without mesangial proliferation) on light microscopy and the absence of subepithelial or subendothelial deposition • The prevalence of lupus podocytopathy represents approximately 1% of LN biopsies. • Acute kidney injury (AKI) is uncommon in lupus podocytopathy (34%). • Microscopic hematuria and hypertension are also rare in lupus podocytopathy (18%)
- 17. MEMBRANOUS LUPUS • Differentiating MLN from pMN can be challenging. • Antibodies • Neutral Endopeptidase (NEP) • Phospholipase A2 receptor (PLA2R) in pMN. (approximately 70% of patients with pMN ) • Anti-Thrombospondin Type 1 Domain Containing 7 Autoantibodies (anti THSD7A) • Exostosin 1 and 2 (differentiate primary from autoimmune forms of membranous nephropathy) • Histology • Mesangial hypercellularity • Electron microscopy –mesangial and subendothelial immune complex deposition, and tubuloreticular inclusions. • Immunofluorescence examination in MLN demonstrates positive staining for immunoglobulin G (IgG), C3, IgM, IgA, and C1q. • Predominant IgG in MLN is usually IgG1 and/or IgG3. In contrast, IgG4 subclass deposits are typical of pMN
- 19. TREATMENT
- 22. KADIGO • Class I LN (minimal-mesangial LN) treated for extrarenal clinical manifestations of lupus. • Class II LN (mesangial-proliferative LN) • Treat patients with class II LN and proteinuria <1 g/d as dictated by the extrarenal clinical manifestations of lupus. • Proteinuria >3 g/d be treated with corticosteroids or CNIs as described for MCD
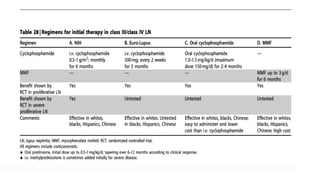
- 23. • Class III LN (focal LN) and class IV LN (diffuse LN)— • Initial therapy -We recommend initial therapy with corticosteroids + either cyclophosphamide or MMF • We suggest that, if patients have worsening LN (rising SCr, worsening proteinuria) during the first 3 months of treatment, a change be made to an alternative recommended initial therapy, or a repeat kidney biopsy be performed to guide further treatment KADIGO
- 24. KADIGO • Maintenance therapy - Azathioprine (1.5–2.5 mg/kg/d) or MMF (1–2 g/d in divided doses), and low-dose oral corticosteroids (r10 mg/d prednisone equivalent). • CNIs with low-dose corticosteroids (intolerant of MMF and azathioprine • After complete remission is achieved, maintenance therapy be continued for at least 1 year before consideration is given to tapering the immunosuppression. • If complete remission has not been achieved after 12 months of maintenance therapy, consider performing a repeat kidney biopsy before determining if a change in therapy is indicated. (Not Graded) • While maintenance therapy is being tapered, if kidney function deteriorates and/or proteinuria worsens, we suggest that treatment be increased to the previous level of immunosuppression that controlled the LN.
- 26. • Class V LN (membranous LN) • normal kidney function, and non–nephrotic-range proteinuria be treated with antiproteinuric + antihypertensive medications, and only receive corticosteroids and immunosuppressives as dictated by the extrarenal manifestations of systemic lupus. • Persistent nephrotic proteinuria be treated with corticosteroids plus an additional immunosuppressive agent: cyclophosphamide or CNI or MMF or azathioprine • General treatment of LN • LN of any class are treated with hydroxychloroquine (maximum daily dose of 6–6.5 mg/kg ideal body weight), • Class VI LN (advanced sclerosis LN) • Corticosteroids and immunosuppressives only as dictated by the extrarenal manifestations of systemic lupus. (2D) KADIGO
- 27. • Relapse of LN • Relapse of LN after complete or partial remission be treated with the initial therapy followed by the maintenance therapy that was effective in inducing the original remission. • Risk for excessive lifetime cyclophosphamide exposure, - non cyclophosphamide-based initial regimen be used • Consider a repeat kidney biopsy during relapse if there is suspicion of histologic class change or rising SCr and/or worsening proteinuria represents disease activity or chronicity. • Treatment of resistant disease • In patients with worsening SCr and/or proteinuria after completing one of the initial treatment regimens, consider performing a repeat kidney biopsy to distinguish active LN from scarring • Treat patients with worsening SCr and/or proteinuria who continue to have active LN on biopsy with alternative initial treatment regimens • Nonresponders who have failed more than one of the recommended initial regimens - treatment with rituximab, i.v. immunoglobulin, or CNIs. KADIGO
- 29. • Systemic lupus and thrombotic microangiopathy • APLA-involving the kidney in systemic lupus patients, with or without LN, be treated by anticoagulation (target INR 2–3). • Plasma exchange • Systemic lupus and pregnancy • counselled to delay pregnancy until a complete remission of LN has been achieved. • Cyclophosphamide, MMF, ACE-I, and ARBs not be used during pregnancy. • Hydroxychloroquine be continued during pregnancy. • MMF be switched to azathioprine. • Relapse during pregnancy, they receive treatment with corticosteroids and, depending on the severity of the relapse, azathioprine. • Drugs not be tapered during pregnancy or for at least 3 months after delivery. Administer of low-dose aspirin during pregnancy to decrease the risk of fetal loss. KADIGO
- 39. The Euro-Lupus Nephritis Trial • Multicenter, prospecitive trial of 90 LN pts with Proliferative LN Initial • Follow 41 months, subsequent long-term follow • Monthly High dose IVCYT ( 6 mo IVP 0.5-1 g/m2+ 2 quarterly pulses ) vs Low dose IV CYT ( 500 mg IVP every 2 wks x 3 months followed by oral AZA )
- 49. ALMS vs MAINTAIN TRIAL • Blind study • n-227 • various ethnic group • Only patient who responded entered maintenance phase • Open • n-105 • White • all patient received EURO LUPUS regimen and entered maintenance phase
- 53. Completed Clinical Trials Abatacept – BMS Completed clinical trials CTLA4-B7 interaction Phase 3 – Failed to meet end point Abatacept – ACCESS Completed clinical trials CTLA4-B7 interaction Phase 2 – Failed to meet end point Anti-CD40L Completed clinical trials CD40-ligand Phase 2 – Terminated Anti-TWEAK Completed clinical trials TWEAK Phase 2 – Terminated Bortezomib Completed clinical trials Plasma cells Phase 4 – Terminated Laquinamod Completed clinical trials Inflammation Phase 2 – Encouraging Rituximab Completed clinical trials CD20 Phase 3 – Failed to meet end point Ocrelizumab Completed clinical trials CD20 Phase 3 – Failed to meet end point
- 54. Active Clinical Trials Anifrolumab Active clinical trials IFN-α Phase 2 – Recruiting Belimumab Active clinical trials B lymphocyte stimulator Phase 3 – Recruitment closed Ixazomib Active clinical trials Plasma cells Phase 1 – Recruiting Obinutuzumab Active clinical trials CD20 Phase 2 – Recruiting Rituximab Active clinical trials CD20/steroid reduced Phase 3 – Recruiting Rituximab/Belimumab Active clinical trials CD20/B lymphocyte stimulator Phase 2 – Recruiting Voclosporin Active clinical trials Calcineurin Phase 2 – Recruitment closed
- 55. THANK YOU…