Overview of Childhood Constipation
- 1. Overview of Childhood Constipation GI Block Fatima Farid Pediatric Resident Year 2
- 2. Contents • Practice case • Basics of constipation • Clinical assessment • Investigation options • Treatment strategies 2
- 3. “A Constipated Toddler” Source: Case 29, 100 Cases Book 3
- 4. History Tanya is a four-year-old girl who presents to outpatients with a two-year history of constipation. • She opens her bowels about once every 5 days and strains. • She soils her knickers on most days. • She has intermittent abdominal pain, which is relieved by opening her bowels. • Recently, there has been fresh blood on the toilet tissue. • Lactulose has been used, with little success. 4
- 5. History • She was delivered by emergency Caesarean section because of fetal distress and meconium staining. • Her mother states that she did not have a dirty nappy until 40 hours of age. • She has recently had a urine infection diagnosed by her GP. The illness was mild and responded well to antibiotics. 5
- 6. Exam • Blood pressure is 101/62 mmHg. • Weight is on the 50th centile and height is on the 25th centile. • A faecal mass is palpable in the left iliac fossa. • The anus appears normal. • Rectal examination – hard stool palpated. • The back is normal. • There are no other signs. 6
- 7. Questions 7 What is the most likely diagnosis? Would you carry out any investigations? What is the treatment?
- 8. Brief answers! 1. Functional constipation with bleeding anal fissure 2. No investigations necessary 3. Mx: i. Lifestyle modification with disempaction then maintenance regimens ii. Analgesia for anal fissures iii. Psychosocial support & counselling 8
- 9. Introduction [1] • Constipation is one of the most common chronic disorders of childhood, affecting 1 to 30% of children worldwide. • It is responsible for 3% of all primary care visits for children and 10% to 25% of pediatric gastroenterology visits. • Children with constipation cost the health care system three times as much as children without constipation, and the negative effect on quality of life often persists into adulthood. 9 [1] AAFP- Evaluation and Treatment of Constipation in Children and Adolescents, July 15, 2014
- 10. Terminology • Parents often use the term constipation to refer to any number of concerns such as: • large stool size • excessively hard stools • infrequent defecation • pain during passing stool • Healthcare providers may often hold a different understanding of the word ‘constipation’ than parents, hence deeper inquiry is pertinent. 10
- 11. Questions • Do all children have identical stool patterns? • Will age influence normal frequency of defecation? 11
- 12. Normal bowel habits • The normal frequency of defecation is highly variable & changes with age. • An infant averages three to four stools a day in the first week of life, two stools a day later in infancy and the toddler years, and once a day to every other day after the preschool years. [1] • Many healthy breastfed infants go several days or longer without a bowel movement! 12 [1] AAFP- Evaluation and Treatment of Constipation in Children and Adolescents, July 15, 2014
- 13. Remember! • Less frequent defecation patterns may be normal and must be considered in the context of stool caliber, associated symptoms, and physical examination findings 13
- 14. Definition The North American Society of Gastroenterology, Hepatology, and Nutrition (NASPGHAN) defines constipation as "a delay or difficulty in defecation, present for 2 weeks or more, and sufficient to cause significant distress to the patient.“ * 14 * Identical definition in Nelson Textbook of Pediatrics- 19th edition
- 15. Etiology • Outside of the neonatal period, childhood constipation is usually functional (i.e., there is no evidence of an organic condition). • Functional constipation accounts for more than 95% of cases of constipation in healthy children one year and older. [2] • Organic causes are responsible for fewer than 5 percent of children with constipation but are more common among young infants and those presenting with atypical features. 15 [2] UpToDate: Functional constipation in infants, children, and adolescents: Clinical features and diagnosis
- 16. Questions • Why and how does functional constipation develop? • Can constipation cause fecal incontinence? If yes, how? 16
- 17. Functional constipation • Persistently difficult, infrequent, or seemingly incomplete defecation, without evidence of a primary anatomic or biochemical cause. • Cycle commonly coincides with toilet training, changes in routine or diet, stressful events, illness, lack of accessible toilets, or in a busy child who defers defecation. 17
- 18. Functional constipation • No gender preference. • Three main peaks in children: a. 6 months- 1 year: introduction of cereals & solid food b. 2- 3 years: toilet training c. 3- 5 years: start of school • Children with autism spectrum disorders are also at high risk- due to abnormal sensory processing/ medication side effect • Triggers of adolescent constipation: a. Busy routine/ school stressors b. Anorexia nervosa/ bulimia: dehydration/ low fiber c. ADHD 18
- 19. 19 Please let me take my time to learn
- 21. Pathophysiology 1. To avoid the passage of another painful bowel movement, the child will contract the anal sphincter or gluteal muscles by stiffening his or her body, hiding in a corner, rocking back and forth, or fidgeting with each urge to defecate. Parents often confuse these withholding behaviors as straining to defecate. 2. Withholding of stool can lead to prolonged fecal stasis in the colon with reabsorption of fluid, causing the stool to become harder, larger, and more painful to pass. 3. Over time, as the rectum stretches to accommodate the retained fecal mass, rectal sensation decreases, and fecal incontinence may develop. 21
- 22. 22
- 23. Rome IV criteria 23 Source: UpToDate
- 24. Fecal incontinence • Voluntary or involuntary passage of feces in the underwear or in socially inappropriate places in a child with a developmental age of at least four years. • It occurs in 1% to 4% of school-aged children and is almost always associated with underlying constipation. • Involuntary soiling may occur as contractions of the full rectum inhibit the internal anal sphincter, leading to overflow. • Condition improves once underlying constipation is treated. 24
- 25. 25 Wish I could stop it
- 26. Questions • Can we diagnose functional constipation without ruling out serious underlying diseases? • Do you know any organic causes of constipation? 26
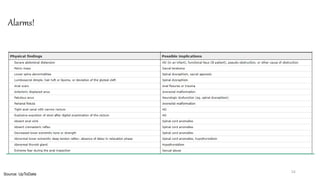
- 27. 27
- 28. Neurogenic 1. Hirschsprung disease 2. Cerebral palsy 3. Myelomeningocele, sacral teratoma, closed spinal dysraphism 4. Neurofibromatosis 5. Muscular weakness (down syndrome, prune belly syndrome, gastroschisis) 6. Infantile botulism 7. Pseudo-obstruction (myopathies, visceral neuropathies, mitochondrial disorders) 8. Intestinal neuronal dysplasia 9. Duchenne muscular dystrophy 10. Familial/ acquired dysautonomia 28 Source: UpToDate
- 29. Endocrine & metabolic 1. Cystic fibrosis (meconium ileus, distal intestinal obstruction syndrome) 2. Hypokalemia 3. Lead poisoning 4. Vitamin D intoxication 5. Hypo or hypercalcemia 6. Hypothyroidism 7. Diabetes mellitus 8. Pheochromocytoma 9. Multiple endocrine neoplasia type 2B (MEN 2B) 10. Polyuria leading to dehydration 11. Juvenile systemic sclerosis (scleroderma) or mixed connective tissue diseases 12. Acute intermittent porphyria 29 Source: UpToDate
- 30. Anatomic & others 1. Anorectal anomalies (imperforate or anteriorly displaced anus) 2. Intestinal obstruction 3. Small left colon syndrome 4. Celiac disease 5. Medications: opiates, anticholinergics, antidepressants, chemotherapy, aluminum containing antacids 6. Generalized joint hypermobility 30 Source: UpToDate
- 36. Investigations • In most cases, organic causes of constipation can be excluded based on a careful history and physical examination. • If warning signs of possible organic constipation are present, focused laboratory and radiographic testing should be performed. 36
- 37. Radiology • Abdomen x- ray: • Not routinely recommended- does not add to rectal exam findings, non- specific for constipation and may falsely exclude more serious causes of presenting complaint • Can be used if examination is limited for child’s sake (obesity, cooperation, psychologic issues) • Barium enema: • Good tool to detect features of Hirschsprung disease • Should be followed by rectal biopsy for confirmation • Lumbosacral x- rays: • Done for children with evidence of spinal dysraphism or neurologic impairment of the perianal area/ lower extremities • If high degree of suspicion is present, MRI is considered to investigate the possibility of tethered cord and spinal cord tumors 37 Source: UpToDate
- 38. 38 Barium enema of an infant with Hirschsprung disease, showing the transition zone (arrow) between the lower aganglionic bowel and the normal colon above.
- 39. Labs • Celiac screening: • For children with failure to thrive or recurrent abdominal pain, perform a CBC and serologic screening for celiac disease (usually IgA antibodies to tissue transglutaminase). • The symptoms of celiac disease may be subtle. Therefore, we have a low threshold for performing celiac screening in children with constipation despite limited information about its clinical utility in this population. • Urine routine and culture: • For children with a history of rectosigmoid impaction, especially in association with encopresis, perform a urine analysis and urine culture. • This is because fecal impaction may predispose to urinary tract infections due to the mechanical effects of the distended rectum compressing the bladder. 39 Source: UpToDate
- 40. Labs • TSH: • For children with impaired linear growth and depressed reflexes, or those with a history of central nervous system disease, we suggest screening for hypothyroidism. • If central hypothyroidism is suspected, the screen should include measurement of free thyroxine (T4) as well as TSH. • Urea/ electrolytes & calcium (for those with metabolic abnormalities or inability to tolerate adequate fluids) • Blood lead level: • Screening for lead toxicity should be performed in children with risk factors. Screening recommendations vary by community. • Children at particular risk include those with pica, developmental disabilities, a family history of lead poisoning in a sibling, or those living in housing built before 1950 or housing that recently has been renovated. 40 Source: UpToDate
- 41. Treatment • Main concept is that chronic constipation causes the distended colon to be unresponsive to stool burden. • Effective treatment requires consistent and complete emptying of the colon, so that it becomes conditioned to work on its own, a concept known as "bowel retraining." • The goal of therapy is the passage of soft stools, ideally once per day, and no less than every other day. • Weeks to months, and sometimes years, of laxative and behavior therapy may be necessary before this goal is achieved. 41
- 42. Bowel re-training • There are four general steps in bowel retraining: 1. Disempaction 2. Prolonged laxative treatment and behavior therapy to achieve regular evacuation and avoid recurrent constipation 3. Dietary changes (primarily increasing fiber content) to maintain soft stools 4. Gradual tapering and withdrawal of laxatives as tolerated 42
- 43. Plan Disempaction (6- 7 days) Maintenance (> 6 months) Rescue Therapy (as needed) 43
- 44. Disempaction • This step is described as a ‘clean out’ to the caregivers • Indicated for fecal impaction, which in practice includes most patients coming under medical attention • Characteristics of candidate children include: a. Constipation associated with fecal incontinence b. Significant stool mass palpable on DRE, abdomen exam or abdomen x- ray c. History of infrequent or incomplete evacuation 44
- 45. Basics • Oral, rectal or combined routes can be used – consider patient/ family preference • Main oral therapy is polyethylene glycol 3350 (Movicol Pediatric Plain) • Start with high dose for six days, then taper down as per guideline to achieve desired stool habit • Some children will need rectal therapy first to release large disempactions to allow tolerance to oral therapy (enemas are mostly used) 45
- 46. Disempaction modalities Oral • Polyethylene glycol 3350 • Polyethylene glycol- electrolyte solution • Mineral oil Rectal • Sodium phosphate enema • Saline enema • Mineral oil enema • Bisacodyl suppositories 46 * Doses of all above medications are on UpToDate
- 47. Movicol (polyethylene glycol 3350) • Macrogol 3350 acts by virtue of its osmotic action in the gut, which induces a laxative effect. • It increases the stool volume, which triggers colon motility via neuromuscular pathways. • The physiological consequence is an improved propulsive colonic transportation of the softened stools and a facilitation of the defecation. • Electrolytes combined with macrogol 3350 are exchanged across the intestinal barrier (mucosa) with serum electrolytes and excreted in fecal water without net gain or loss of sodium, potassium and water. 47
- 48. Dosing • Dosage: • One pediatric sachet is 6.9 grams • 1 to 1.5 g/kg/day by mouth for up to 6 days • Daily dose is dissolved in approximately 10 mL/kg body weight of water or flavored beverage • Example: 10 kg child 15 g/ kg every day = 2 sachets per day 48
- 49. Practical tip 49 Source: NHS UK & medicines.org.uk Remember: One sachet is 6.9 grams Do not exceed 12 sachets! The daily number of sachets should be taken in divided doses, all consumed within a 12- hour period. The above dosage regimen should be stopped once disempaction has occurred.
- 50. Making Movicol • Each sachet should be dissolved in 62.5 ml (quarter of a glass) of water. • The correct number of sachets may be reconstituted in advance and kept covered and refrigerated for up to 24 hours. For example, for use in fecal impaction, 12 sachets can be made up into 750 ml of water. • Sachet: Do not store above 25°C. • Reconstituted solution: Store in a refrigerator (2°C - 8°C) and covered. • Any unused solution should be discarded within 24 hours. 50 Source: Medicines.org.uk
- 52. Sodium phosphate enema • 33 mL enema for children 2 to <5 years; 66 mL enema for children 5 to 12 years; and 133 mL enema for children ≥12 years. • These enemas should not be used in children younger than two years of age. • This dose may be repeated once within 12 to 24 hours, if necessary. • Because these are small-volume enemas, the caregiver should be instructed to point the tip of the enema device toward the child's back after it is inserted, to direct the contents toward the bowel wall where it will be effective, rather than into the fecal mass. 52
- 53. Caution • More frequent dosing should be avoided because there are several case reports of life- threatening hyperphosphatemia and hypocalcemic tetany, particularly in young children, those with colonic dysmotility, and/or with repeated administration of enemas. • Phosphate-based enemas should be avoided in children with renal insufficiency. 53
- 54. Maintenance • After disempaction, patients should be treated with a maintenance regimen of oral laxatives to "retrain" the bowel and avoid reimpaction, which could restart the constipation cycle. • Adequate doses of medication should be given to maintain a pattern of soft bowel movements once or twice a day. • It is important to start this maintenance regimen of laxatives immediately after disempaction to avoid reaccumulation of stools. 54
- 55. Options • Polyethylene glycol 3350 • Magnesium hydroxide (milk of magnesia) • Lactulose • Mineral oil The best studied medication is PEG without electrolytes, which appears to be efficacious and safe The type of laxative is not as important as using an adequate dose and ensuring compliance 55
- 56. Maintenance regimen • Parents should be advised to adjust the laxative dose according to the response, and to increase the dose every two days until the child has one or two soft stools each day, or to decrease it if the patient develops diarrhea. • Parents should be warned that some leaking or soiling may continue at first, especially if the child fears or continues to resist having a bowel movement. • After starting the laxative treatment, parents should be advised to encourage the child to use the toilet for 5 to 10 minutes at the same time each day, preferably after breakfast or dinner. • In children who are not fully toilet trained, delay this toileting plan until the child has had at least two to four weeks of effective laxative treatment, to make sure that he or she is not experiencing any pain or hard stools when using the toilet. 56
- 57. Drugs • Movicol: • Dose: 0.4 to 0.8 g/kg per day (up to 17 g) • Clinical trials indicate that PEG without electrolytes has efficacy greater than or like that of lactulose and magnesium hydroxide with fewer adverse effects and greater acceptance • Lactulose: • Typical doses are 1 mL/kg (up to 30 mL), once or twice daily • Some patients report loss of effectiveness over time, presumably due to altered degradation by the colonic bacteria • Side effects include flatulence and abdominal cramps, which occur when the sugar is metabolized by colonic flora 57
- 58. Movicol for maintenance 58 If the dose needs increasing this is best done every second day. For children below 2 years of age, the maximum recommended dose should not exceed 2 sachets a day. For children aged 2 to 11 years, the maximum recommended dose needed does not normally exceed 4 sachets a day. Treatment of children with chronic constipation needs to be for a prolonged period (at least 6 – 12 months) Source: NHS UK & medicines.org.uk
- 59. Rescue therapy • Stimulant laxatives, such as senna and bisacodyl, are sometimes used for brief periods to avoid recurrence of impaction ("rescue" therapy), and their use for this purpose is supported by extensive clinical experience and expert guidelines • Most pediatric providers reserve stimulant laxatives for patients with severe constipation who do not respond to osmotic laxatives and dietary changes, preferably under supervision from a pediatric gastroenterologist • These laxatives are often used in conjunction with a stool softener such as docusate (Colace) or lubricant such as mineral oil • Stimulant laxatives also may be helpful for patients with anorectal malformations or other disorders that affect anorectal innervation, which can affect sensory and motor function and predispose to both constipation and fecal incontinence 59
- 61. 61 Constipation with fecal incontinence Source: UpToDate
- 62. 62 Constipation without fecal incontinence Source: UpToDate
- 63. Additional therapy • Behaviour modification: • Toilet sitting regularly for 5- 10 mins BD with proper positioning • Reward system for effort • Monitoring using stool diary • Dietary changes: • Balanced diet with fruits, vegetables & whole grains • Adequate fluid intake • Trial of cow milk elimination in select circumstances 63
- 65. 65
- 66. Follow- up • Planned follow-up is particularly important during the first few days of treatment, especially if disempaction was warranted. • The initial discussion can be by telephone, but the child may need to return to the office if he or she is still passing hard stools. • Patients who require disempaction also should have an office visit soon after completing the disempaction protocol to review the details of maintenance therapy. • After entering the maintenance phase, the child should have regular follow-up visits, initially on a monthly basis and then less frequently (eg, every three to four months). • The clinician should review the child's stool records and repeat the abdominal and rectal examinations. • The follow-up visits provide opportunities to evaluate progress, adjust medication regimens, anticipate challenges, and celebrate successes. • As laxative therapy is gradually discontinued, the importance of dietary and behavioral interventions should be reinforced. 66
- 67. References • AAFP: Evaluation and Treatment of Constipation in Children and Adolescents, July 15, 2014 • Medscape: Pediatric Constipation • UpToDate: Functional constipation in infants, children, and adolescents: Clinical features and diagnosis • UpToDate: Chronic functional constipation and fecal incontinence in infants, children, and adolescents: Treatment • Illustrated textbook of pediatrics, fourth edition • Nelson textbook of pediatrics, nineteenth edition 67
- 68. Thank you!









![Introduction [1]
• Constipation is one of the most common chronic disorders of childhood, affecting 1 to 30% of
children worldwide.
• It is responsible for 3% of all primary care visits for children and 10% to 25% of pediatric
gastroenterology visits.
• Children with constipation cost the health care system three times as much as children without
constipation, and the negative effect on quality of life often persists into adulthood.
9
[1] AAFP- Evaluation and Treatment of Constipation in Children and Adolescents, July 15, 2014](https://image.slidesharecdn.com/overviewofchildhoodconstipation-210625115313/85/Overview-of-Childhood-Constipation-9-320.jpg)


![Normal bowel habits
• The normal frequency of defecation is highly variable & changes with age.
• An infant averages three to four stools a day in the first week of life, two stools a day later in
infancy and the toddler years, and once a day to every other day after the preschool years. [1]
• Many healthy breastfed infants go several days or longer without a bowel movement!
12
[1] AAFP- Evaluation and Treatment of Constipation in Children and Adolescents, July 15, 2014](https://image.slidesharecdn.com/overviewofchildhoodconstipation-210625115313/85/Overview-of-Childhood-Constipation-12-320.jpg)


![Etiology
• Outside of the neonatal period, childhood constipation is usually functional (i.e., there is no
evidence of an organic condition).
• Functional constipation accounts for more than 95% of cases of constipation in healthy children
one year and older. [2]
• Organic causes are responsible for fewer than 5 percent of children with constipation but are
more common among young infants and those presenting with atypical features.
15
[2] UpToDate: Functional constipation in infants, children, and adolescents: Clinical features and diagnosis](https://image.slidesharecdn.com/overviewofchildhoodconstipation-210625115313/85/Overview-of-Childhood-Constipation-15-320.jpg)