Renal Dynamic Scan - Isotope Scan - DTPA
- 1. Renal Isotope Scan Dr Bhanumurthy Kaushik M. Senior Resident – Pediatric Surgery Institute of Medical Sciences Banaras Hindu University, Varanasi
- 2. Renal Evaluation • History and Examination (decreased urine output / facial puffiness / anasarca) • Urine routine microscopy • Albumin • Casts • Blood Urea • Serum Creatinine
- 3. • Ultrasound • Size (length / width) • Thickness (cortical / parenchymal) • Pelvis (size and AP diameter) • Corticomedullary differentiation • CT Scan • CT KUB • CTU or CT IVU or CT IVP • Plain Xray KUB • Xray dye studies • Intravenous Urogram / Pyelogram (IVU/IVP) • Retrograde Pyelography / Pyeloureterography • Urethra Study • Ascending or Retrograde Urethrography • Descending or Voiding or Micturating Cystourethrography
- 4. All the mentioned imaging modalities can show the anatomy of the kidneys and KUB only The function of the kidneys (GFR) and the differential function of the kidneys cannot be assessed by these routine imaging modalities Furthermore, the non-functional regions of the kidneys cannot be assessed as well
- 5. Renal Isotope Scan – Renal Scintigraphy • Department of Nuclear Medicine – Diagnostic / Therapeutic • Isotopes = Same element with different mass (difference in the number of neutrons – Hence additional properties) • Unstable nucleus – results in decay – alpha, beta or gamma rays emitted • Scintillation = Flash or Sparkle of light (because of rays emitted) • Carrier molecule directs the isotope to the tissue which is desired to be studied i.e. target organ • Radiopharmaceutical = Radio-isotope + Carrier molecule • Radio-Isotope produces the sparkle • Gamma Camera – identifies the sparkle of the isotope
- 6. • Iodine is element • Iodine 131 = Radio-isotope • Radio Pharmaceutical for renal study • OIH = ortho Iodo hippuric acid Technetium-99 is preferred because of its shorter half life for gamma emission (6 hours) and approximately 94% of it decays in 24 hours
- 7. • Technetium is element • Technetium 99 = Radio-isotope • Carrier molecule or Ligand (for Renal Study) • DMSA = Dimercapto Succinic Acid • DTPA = Diethylene Triamine Penta-acetic acid • MAG3 = Mercapto Acetyl Triglycine
- 8. Mechanism of Carrier molecule
- 9. Mechanism of Carrier molecule (contd.) Pharmaceutical Property Renal Handling Application DMSA Tightly binds to renal tubular cells and only small amount is excreted into urine Localizes and binds to Proximal convoluted tubules Excellent visualization of renal parenchyma – Renal Parenchymal imaging DTPA Little plasma protein binding and cleared ‘almost’ exclusively by glomerular filtration GFR dependent for clearance (hence results are suboptimal in immature kidneys or in low GFR or in patients with compromised renal function) Excellent visualization of PCS, Ureter and bladder – Renography MAG3 90% bound to plasma protein and principally cleared by tubular secretion. Shows both parenchyma and collecting system Principally cleared by tubular secretion Renography – 1. Requires comparatively low radiation dose 2. Can be used in low GFR / immature kidneys 3. Both parenchyma and collecting system visualized
- 10. Procedure • Pre-requisite, Patient has to be adequately hydrated before the procedure • Radiopharmaceutical is initially taken (in desired dilution) • Before injecting – the pharmaceutical is placed in front of Gamma camera to identify the number of Radioisotopes being injected into the patient • Once injected, (during) the camera which is already placed behind the patient is used to identify and quantify the pharmaceutical reaching the tissue of interest
- 11. Procedure (continued) • The target organ here is the Kidney • The isotopes reaching both the kidneys can be identified separately • Lasix might be or might not be injected (to let the pharmaceutical be filtered out fast) – as per the protocol being used • After the required images are captured, the residual pharmaceutical left in the syringe is calculated by placing Infront of gamma camera • Images are generated and computed by the computer
- 12. Administration of Pharmaceutical Distribution Emission Detection Image formation (by computer) Overview of Procedure
- 13. Phases of Renal Scintigraphy Perfusion Phase or Vascular Transit Phase (One) First passage of radioactive bolus into kidney Blood flow and initial uptake Parenchymal Phase or Tubular concentration Phase or Extraction Phase (Two) Filtration and/or secretion of the RP from the blood into the nephron – Before any excretion Tissue function Excretory phase (Three) Passage of dye into collecting system Noted by downslope Drainage Is there a Phase Zero?
- 14. Time Activity Curve = Graphical Representation of the Phases
- 17. Time To Peak – TTP or Tmax • The time to peak refers to the time from radiopharmaceutical injection to the peak height of the renogram curve. • 99mTc-MAG3 and 99mTc-DTPA renograms normally peak by 5 min • Delayed Tmax indicated ?Renal perfusion issues
- 18. Concept of ‘t’ half (t1/2) • The time taken for half of the radionucleotide to be cleared from the renal pelvis is termed as (t half) T1/2 • Usually in the absence of obstruction – half of the radionucleotide is cleared from the renal pelvis within 10 to 15 minutes i.e. t1/2= 10 to 15 min. • t1/2 > 20 minutes indicates obstruction • t1/2 < 15 min. generally considered to be normal • t1/2 between 15 to 20 minutes is indeterminate
- 19. Residual Cortical Activity – RCA • To determine the activity remaining at the cortical region 20 minutes post injection of radiopharmaceutical • RCA is calculated by 𝐶𝑜𝑟𝑡𝑖𝑐𝑎𝑙 𝐶𝑜𝑢𝑛𝑡𝑠 𝑎𝑡 20 𝑚𝑖𝑛𝑢𝑡𝑒𝑠 ÷
- 20. Furosemide (Lasix) Protocol • To hasten the process of renal excretion a diuretic = Furosemide is injected to the patient • Dose = max of 1mg/kg • F + 20 protocol = Lasix is injected after 20 minutes of administering the radiopharmaceutical. This is conventionally performed. (corresponding with the t1/2 as previously discussed) • F 0 protocol = Lasix is injected at the same time as radiopharmaceutical • F - 15 protocol = Lasix is injected 15 minutes before the radiopharmaceutical • F + 10, F + 15 protocols are also followed in some regions
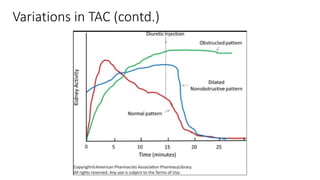
- 21. Variations in TAC F + 20 Protocol was followed
- 22. O’Reilly Classification of MAG3 TAC: Type A = Normal Type B = Obstructed Type C = Dilated, Non Obstructed Type D = Partially Obstructed
- 23. Variations in TAC (contd.)
- 24. Color Coding – Lt and Rt Kidneys
- 25. Differential Renal Function = Simple math • Sparkles noted before injection – (minus) Sparkles left over in syringe after injection = Actual amount of Radiopharmaceutical injected into the patient (say x) • Sparkles noted in Left kidney (say a) and Sparkled noted in Right kidney (say b) are identified by the gamma camera separately • Hence Differential Renal Function (DRF) is easily calculated • Left Kidney function = a/x • Right Kidney function = b/x
- 26. Patient 1
- 30. Patient 2
- 35. PCN was placed
- 40. Indication for Surgical intervention in PUJO • Differential Renal Function <35 to 40% and • t1/2 of > 20 minutes and • Ultrasound finding consistent with Anatomical obstruction