seminarShein.ppt
- 1. Department of Computer Science Knowledge Discovery From Massive Healthcare Claims Data Varun Chandola, Sreenivas Sukumar, Jack Schryver Presented by Anatoli Shein (aus4@pitt.edu)
- 2. Department of Computer Science Motivation: US health care 7/12/2023 Anatoli Shein 2008: 15.2% of GDP 2017: 19.5% of GDP
- 3. Department of Computer Science Goal: Improve cost-care ratio • Improve healthcare operations. • Reduce fraud, waste, and abuse. 7/12/2023 Anatoli Shein
- 4. Department of Computer Science Big Data Analytics in HealthCare 7/12/2023 Anatoli Shein
- 5. Department of Computer Science Big Data in HealthCare Categorized 7/12/2023 Anatoli Shein
- 6. Department of Computer Science Data quality and availability • Clinical Data, Behavior data, and Pharmaceutical Data: –Useful but unavailable 7/12/2023 Anatoli Shein
- 7. Department of Computer Science Data quality and availability • Health insurance Data – Available but needs preparation 7/12/2023 Anatoli Shein
- 8. Department of Computer Science State of the Art Analytics for Massive HealthCare Data: • Network analysis • Text mining • Temporal analysis • Higher order feature construction 7/12/2023 Anatoli Shein
- 9. Department of Computer Science Health Insurance • 85% of Americans have it • It’s data is stored to : – Track payments – Address fraud 7/12/2023 Anatoli Shein
- 10. Department of Computer Science Health Insurance Data Model • Fee-for-service model • Provider -> Service -> Patient -> Cost -> Justification -> Payor 7/12/2023 Anatoli Shein
- 11. Department of Computer Science Data Maintained for Operation • Claims information • Patient enrollment and eligibility • Provider enrollment 7/12/2023 Anatoli Shein
- 12. Department of Computer Science Challenges and Opportunities • Fraud • Waste • Abuse 7/12/2023 Anatoli Shein
- 13. Department of Computer Science Fraud • Billing for not provided services • Large scale fraud 7/12/2023 Anatoli Shein
- 14. Department of Computer Science Waste • Improper payments – Double payments – Duplicate claims – Outdated fee schedule 7/12/2023 Anatoli Shein
- 15. Department of Computer Science Abuse • Prospective payment system • Upcoding 7/12/2023 Anatoli Shein
- 16. Department of Computer Science Data Used • Claims data (48 million beneficiaries in the US) from transactional data warehouses • Provider enrollment data (from private organizations) • Fraudulent providers (from Office of Inspector General’s exclusion) – The rest are treated as non-fraudulent 7/12/2023 Anatoli Shein
- 17. Department of Computer Science Claims Data 7/12/2023 Anatoli Shein
- 18. Department of Computer Science Analysis • Identification of typical treatment profiles • Identification of costly areas 7/12/2023 Anatoli Shein
- 19. Department of Computer Science Text Analysis, profile building • Apache Mahout • Hadoop Based technology – Map Reduce 7/12/2023 Anatoli Shein
- 20. Department of Computer Science Entities as Documents • Document-term matrixes – P(providers) – B(beneficiaries) – C(procedures) – G(diagnoses) – D(drugs) • Ex: PG (providers/diagnoses) 7/12/2023 Anatoli Shein
- 21. Department of Computer Science 7/12/2023 Anatoli Shein
- 22. Department of Computer Science Interesting find • Some seemingly different diagnosis codes got grouped to the same topics – Ex: Diabetes and Dermatoses 7/12/2023 Anatoli Shein
- 23. Department of Computer Science Social Network Analysis • Estimate the risk of a provider fraud before making any claims by constructing social network 7/12/2023 Anatoli Shein
- 24. Department of Computer Science Provider Network 7/12/2023 Anatoli Shein
- 25. Department of Computer Science Texas Provider Network 7/12/2023 Anatoli Shein
- 26. Department of Computer Science Extracting Features from Provider Network 7/12/2023 Anatoli Shein
- 27. Department of Computer Science Information complexity measure • Most distinguishing features showed to be: – Node degree – Number of fraudulent providers in 2-hop network – Eigenvector centrality – Current-flow closeness centrality 7/12/2023 Anatoli Shein
- 28. Department of Computer Science 7/12/2023 Anatoli Shein
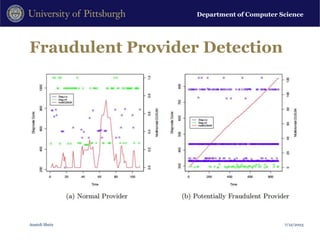
- 29. Department of Computer Science Temporal Feature Construction • By looking at provider data over time we can find anomalies • Increase in number of patients • Taking patients with conditions different from their past profiles 7/12/2023 Anatoli Shein
- 30. Department of Computer Science Fraudulent Provider Detection 7/12/2023 Anatoli Shein
- 31. Department of Computer Science Conclusions • Introduced domain of “big” healthcare claims data • Analyzed health care claims data on a country level using state of art analytics for massive data • Problem was transformed to well known analysis problems in the data mining community • Several approaches presented for identifying fraud, waste and abuse 7/12/2023 Anatoli Shein
- 32. Department of Computer Science • Thank you. • Questions? 7/12/2023 Anatoli Shein
Editor's Notes
- #10: Address economic challenges. Strong analytic insight into healthcare.