Stemi 1
- 1. CASE PRESENTATION Presented by: Dr. Abdullah Almazyad R1 Dr. Fatimah Alghamdi R3 Under supervision of :Dr. Abdullah Alkhudair
- 2. OBJECTIVES Case presentation History Physical Examination Differential diagnosis Investigation and management Patient hospital coarse Educational topic about disease Key point
- 3. CHIEF COMPLAINT • Chest pain for 15 minutes followed with a sudden syncope
- 4. Any Further Questions About Chest Pain
- 5. DIFFERENTIAL DIAGNOSES OF CHEST PAIN • MI, Angina, Myocarditis, And Pericarditis/Dressler’s Syndrome Cardiac • PE, Pneumothorax/Hemothorax, Tension Pneumothorax, Pneumonia, Empyema, Pulmonary • Neoplasm, Bronchiectasis, Pleuritis, And TB • Pulmonary • Esophageal: GERD, Esophageal Rupture, Spasm, Esophagitis, Ulceration, Achalasia, Neoplasm, And • Mallory-weiss Syndrome • Other Structures: PUD, Gastritis, Pancreatitis, And Biliary Colic • Gastrointestinal • Lymphoma, Thymoma • Mediastinal • Dissecting Aortic Aneurysm, Aortic Rupture • Vascular
- 6. HISTORY OF PRESENTING ILLNESS • Mr. N 52-year-old M. heavy smoker • Presented to ER with of typical chest pain • Pain was stared suddenly , in public place (the restaurant) while he was standing reached maximum 10/10 in few minutes. • Pain felt like heaviness in nature , radiating to the left shoulder and back , associated with diaphoresis and was aggravated by movement, • After 15-20 of heavy chest pain M.N felt dizzy due to intense pain , people tried to make him set and feel comfortable . • As a result EMS were called by one of the public and took patient to ER, no CPR or medication ware given to his way to ED. • Patient has positive history of similar episode few days ago while sleeping , was 5/10 in severity and relieved spontaneously within few minutes
- 8. PAST MEDICAL • Mr. N is not known to have any medical illness
- 9. PAST MEDICAL HISTORY No known cardiovascular risk factors except for smoking No history of Hypertension • No history of Hyperlipidaemia • No history of Myocardial infarction • No history of Chronic kidney disease • No history of Atrial fibrillation • No history of Stroke • No history of Peripheral vascular disease No history of Respiratory vascular disease No history of Gastrointestinal disease:
- 10. MEDICATION HISTORY AND ALLERGY • Patient never received : • Anticoagulants (e.g. pulmonary embolism) • Antiplatelets (e.g. coronary artery disease) • Statins (e.g. coronary artery disease) • Calcium channel blockers (e.g. hypertension) • ACE inhibitors (e.g. hypertension) • Antibiotics (e.g. pneumonia) • Colchicine (e.g. pericarditis) • No known allergy
- 11. PAST SURGICAL HISTORY • He once was admitted for appendectomy 18 years ago , there was no immediate or late complications • No history of blood Transfusion • No history of Car Accidents
- 12. FAMILY HISTORY • No family history of premature CAD • His father is 74 alive , he is diabetic and Hypertensive • His mother is 72 alive , she is hypertensive only • He has 1 brother and 3 sisters , all of them are medically free • No history of similar episode in the family • No history of cardiac disease • No family history of Familial Hypercholesteremia
- 13. SOCIAL • He is a smoker cigarettes, 250 packyears • Sedentary lifestyle • Works in food delivery since last year , originally was an employee in a marketing agency ,setting most of the time • Doesn’t follow a healthy diet, high saturated fatty diet • No history of Recreational drug use • No history of alcohol use/abuse
- 14. REVIEW OF SYSTEMS • Respiratory : • No chough , no SOB , no hemoptysis • Gastrointestinal : • No abdominal pain , no dysphagia , no diarrhea • Genitourinary : • No dysuria , no flank pain • Neurological : • No weakness , no dizziness , one episode of syncope for few minutes • Musculoskeletal : • No joint pain , no stiffness , no history of Trauma
- 15. • Hematology : • No Bruising , no history of ease of bleeding, no history of Autoimmune disease • Endocrine : • No history of cold intolerance or Polyuria
- 16. PHYSICAL EXAMINATION • Vital Signs ER • T : 36.5 BP : 153/87 Heart Rate : 96 RR: 20 SPo2 : 99% RA • General examination after admission • Conscious , Alert , Oriented to TPP , in distress due to chest pain • Diaphoretic • Not pale or Cyanotic • Connected to IV Cannula • BMI 45
- 17. HANDS AND HEENT • Hands : • No Nail Clubbing • No flapping Tremor • No Osler Nodes , Janeway lesions , or Splinter Hemorrhage • Eyes : • No pallor • No Jaundice • Nose : • No septal Deviation , No discharge • Ear : • No bulging of membrane or Perforation • Throat/Oral : • Poor Dental Hygiene , No central Cyanosis , No Erythema
- 18. CARDIOVASCULAR • Pulse : regular , no Radio-radial delay , no Radio-femoral delay • Inspection : • No scars , no prominent veins , no skin changes , no chest deformity , no visible pulsation • JVP not raise , no cannon wave • Palpation : • Apex beat in 5th intercostal space , midclavicular line • No palpable thrills , or Parasternal heaves • No Tenderness • Auscultation : • First and second heart sounds are audible throughout auscultatory area • No murmur , no S3 or S4? , no pericardial rub • Lower Limbs : no lower limbs edema
- 19. RESPIRATORY • Inspection : • Chest movement was symmetrical • Palpation : • Trachea was central ,equal chest expansion , no Subcutaneous emphysema • No palpable lymph nodes (anterior and posterior triangle , Supraclavicular , and axillary region) • Percussion : • Bilateral Resonant all over chest • Auscultation : • Vesicular Breathing equal bilaterally all over chest • No Wheezing or crackles
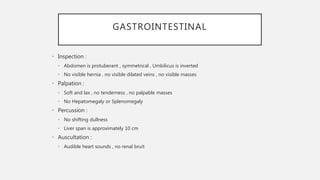
- 20. GASTROINTESTINAL • Inspection : • Abdomen is protuberant , symmetrical , Umbilicus is inverted • No visible hernia , no visible dilated veins , no visible masses • Palpation : • Soft and lax , no tenderness , no palpable masses • No Hepatomegaly or Splenomegaly • Percussion : • No shifting dullness • Liver span is approximately 10 cm • Auscultation : • Audible heart sounds , no renal bruit
- 21. MUSCULOSKELETAL • Joints : • No visible joint or bone deformities • No tenderness on movement or palpation • No decreased ROM , swelling or erythema
- 22. NEUROLOGICAL • GCS : 15/15 • Upper Limb • Sensory : intact for touch and pain • Normal power , tone and reflexes • Lower Limb : • Sensory : intact to touch and pian • Normal power , tone and reflexes
- 24. • Acute Coronary Syndrome • Pulmonary Embolism • Pneumothorax • Aortic Dissection • Acute Pericarditis
- 25. HOW WOULD YOU APPROACH MR. N IN EMERGENCY DEPARTMENT
- 26. ECG AT ADMISSION
- 27. LOCALIZATION OF MI ON ECG
- 28. STEMI ECG • ST elevation criteria • new ST elevation in two contiguous leads of >0.1 mV in all leads other than leads V2-V3 • for leads V2-V3: 0.2 mV in men 40 yr, 0.25 mV in men <40 yr, or 0.15 mV in women
- 29. “TYPICAL” SEQUENTIAL CHANGES OF EVOLVING MI • 1. hyperacute T waves (tall, symmetric T waves) in the leads facing the infarcted area, with or without ST elevation • 2. ST elevation (injury pattern) in the leads facing the infarcted area usually in the first hours post infarct • in acute posterior MI, there is ST depression in V1-V3 (reciprocal to ST elevation in the • posterior leads that are not recorded in the standard 12-lead ECG) hence get a 15- lead ECG • 3. significant Q waves: >40 msec or >1/3 of the total QRS amplitude and present in at least 2 • consecutive leads in the same territory (hours to days post-infarct) • Q waves of infarction may appear in the very early stages, with or without ST changes • non-Q wave infarction: there may be only ST or T
- 31. LABS AT ADMISSION 4/11/20 • WBC : 8.61 • HGB : 17.6 • PLT : 342 • PT : 12.5 • INR : 1.1 • PTT : 35.5 • Na : 139 • K : 3.8 • Cr : 84 • Troponin : 30 , is it enough? • on 5/11/20 it was 89000 • BNP : less then 10
- 32. LABS • AST : 71 • ALT : 73 • ALP : 38 • HDL : 0.71 • LDL 4.11 • Triglycerides :1.76 • Cholesterol : 4.92 • Bilirubin total : 26 • Bilirubin Direct : 7.2
- 33. CXR
- 34. ECHOCARDIOGRAPHY • LV normal in size, mildly reduced. LVEF =40% • large sized apical, septal, anteroseptal, and anterior wall motion abnormality with hypokinesis to akinesis of the segments • RV is normal in size and function. • Inadequate TR jet to assess RVSP. • No hemodynamically significant valve disease. • There is no pericardial effusion.
- 35. CORONARY ANGIOGRAPHY • Was Done • Insert vid
- 36. HOSPITAL COARSE • During admission patient was started on IHD Medications : • Received loading dose of Aspirin 300 mg PO , and Clopidogrel 180 mg PO • Then kept on : • Aspirin 100 mg PO OD • Clopidogrel 75 mg PO OD • Tirofiban infusion during and after cath for 18 hour • Atorvastatin 80 mg PO OD • Heparin Infusion until day of CABG • Bisoprolol 2.5 mg PO OD
- 37. EDUCATIONAL REVIEW FOR STEMI MANAGEMENT GOALS Preventing re-occlusion • Antiplatelet • antithrombosis Preventing mechanical complication • B-Blocker • ACEI • ARBs • Aldosterone antagonist Preventing recurrent Infarction • Statin • Cardiac rehab Preventing sudden cardiac death • AICD
- 38. EDUCATIONAL REVIEW FOR ACS MANAGEMENT AND COMPLICATION • ACS includes the spectrum of unstable angina (UA), NSTEMI, and STEMI; this distinction aids in providing the appropriate therapeutic intervention
- 39. 1. GENERAL MEASURES • 1. General Measures • ABCs: assess and correct hemodynamic status First • bed rest, cardiac monitoring, oxygen(if less 92) • nitroglycerin SL followed by IV • morphine IV
- 40. 2. ANTI-PLATELET AND ANTICOAGULATION THERAPY • NSTEMI • Ticagrelor, in addition to ASA or if ASA contraindicated, subcutaneous low molecular weight heparin or IV unfractionated heparin (UFH) • – LMWH preferable, except in renal failure or if CABG is planned within 24 h • clopidogrel used if patient ineligible for ticagrelor • If PCI is planned: ticagrelor or prasugrel and consider IV GP IIb/IIIa inhibitor (e.g. abciximab) • Clopidogrel used if patient ineligible for ticagrelor and prasugrel • Prasugel contraindicated in those with a history of stroke/TIA, and avoidance of or lower dose is recommended for those >75 year old or weighing under 60 kg (TRITON-TIMI 38) • ANTICOAGULATION OPTIONS DEPEND ON REPERFUSION STRATEGY: • Primary PCI: UFH during procedure; bivalirudin is a possible alternative • Thrombolysis: LMWH (enoxaparin) until discharge from hospital; can use UFH as alternative because of possible rescue PCI • no reperfusion: LMWH (enoxaparin) until discharge from
- 41. 3. B-BLOCKERS • STEMI: contraindications include signs of heart failure, low output states, risk of cardiogenic shock ,heart block, asthma or airway disease; initiate orally within 24 h of diagnosis when indicated • )
- 42. 4. INVASIVE STRATEGIES AND REPERFUSION OPTIONS STEMI After diagnosis of STEMI is made, do not wait for results of further investigations before implementing reperfusion therapy THROMBOLYSIS Goal is Door to Balloon <30 min preferred if patient presents 12 h of symptom onset, has contraindications to PCI, or PCI cannot be administered within 90 min Criteria for successful THROMBOLYSIS : • ST segment elevation resolution below half its initial magnitude • no chest pain • Reperfusion rhythms • PCI • Primary PCI: without prior thrombolytic therapy • Rescue PCI: following failed thrombolytic, improves mortality vs. thrombolysis with fewer intra-cranial hemorrhages and recurrent MIs
- 43. THANK YOU