Thiopentone upendra
- 1. THIOPENTONE Guided by Dr. Abhay Bodhey Presented by Dr. Upendra
- 2. INTRODUCTION Sulphur derivative of Barbituric Acid. i.e. Thio barbiturate. Ultra short acting barbiturate. Synthesised by Tabern and Volwiler in 1935. Introduce clinically by Ralph waters and John Lundy for induction of anaesthesia.
- 3. Poor analgesic, weak muscle relaxant. Commonest inducing agent used.
- 4. Fig : Chemical Structure of Thiopentone Sulphur make it more lipid soluble and more potent Sulphur at second carbon atom position. 5-ethyl-5-(1-methylbutyl)-2-thiobarbituric acid
- 5. PROPERTIES Highly soluble in water / NS yielding highly alkaline solution,stable for 48 hrs. Must be prepared freshly. Powder form stable at room temperature. Refrigerated solution stable up to 2 week.
- 6. PROPERTIES pH of 2.5% solution is 10.5. Commercial preparation contain it sodium salt with anhydrous sodium carbonate to prevent ppt.of acid form. Available as 0.5 gm and 1 gm powder for reconstitution. • Refrigerated solutions- stable upto 2 weeks
- 7. PHARMACOKINETICS Onset of action of i.v. injection - 10-20 sec. peak 30-40 sec. duration for awakening 5-15 min. Prompt awakening after single i.v. inj. is due to rapid redistribution to lean body tissue (muscle) Volume of distribution is 2.5 Lit. per Kg.
- 8. Ultimate elimination due to hepatic metabolism. Effect site equilibration time is rapid. Brain – 30 Sec. Muscle – 15 Min. Fat > 30 Min. Context sensitive half life is prolonged.
- 9. TERMINATION OF ACTION 1) Redistribution a) Lipid solubility (most important factor) High Lipid Solubility makes it to cross blood brain barrier & lean body tissue rapidly. b) Protein Binding Highly bound to albumin & other plasma protein. 72 – 86% Binding. Only unbound fraction crosses Blood-Brain-Barrier.
- 10. Affected by physiological PH. Disease state & parallels lipid solubility Hepatic disease & chronic renal disease decrease protein Binding, increase free form. c) Ionization Only non-ionized part crosses Blood-Brain-Barrier. Thiopentone has PKA 7.6 so 61% of it is non-ionized at physiologic PH As PH decreases (acidosis) non-ionized form increases. Metabolism induced changes in PH affect more.
- 11. Rapid distribution half life – 8.5 Min. Slow distribution half life – 62.7 Min
- 12. 2)Metabolism By liver microsomal enzymes mainly, Slightly in CNS & kidney. 10 – 24 % Metabolised each hour.
- 13. By oxidation, dealkylation & conjugation to hydroxy Thiopental & carboxylic acid derivatives more water soluble & excreted rapidly. Affect by hepatic enzyme activity more than blood flow. Metabolism at 4-5 mg./Kg. dose exhibits first order kinetics. At very high doses (300-600 mg/Kg.) exhibit zero order kinetics.
- 14. 3) Renal Excretion Protein Binding limits filtration. High lipid solubility increase reabsorption.
- 15. Elimination Half Life 11.6 Hours Low elimination clearance(3.4ml/kg/min) Prolonged in obese patient & pregnancy. Short in paediatric patient.
- 16. MECHANISM OF ACTION Sedation & Hypnosis by interaction with inhibitory neurotransmitters GABA on GABAA receptor. GABA facilitatory & GABA mimetic action. GABAA receptor has 5 glycoprotein sub unit. Increases GABA mediated transmembrane conductance of Cl– ion, Causes hyperpolarization & inhibition of post synaptic neuron.
- 17. ↓↓ rate of dissociation of GABA from receptor. It high doses itself activate GABA receptor. Fig. GABAA Channel Complex Inhibit synaptic transmission of excitatory neurotransmitter via glutamate & neuronal nicotinic acetylcholine receptors.
- 18. PHARMACODYNAMI CS Central nervous system Dose dependent effect sedation → sleep → anaesthesia → coma.
- 19. Acts on Reticular Activating System & Thalamus. Induces General Anaesthesia → loss of consciousness, amnesia & ↓↓ response to pain R.S. & C.V.S. depression. Depresses transmission in sympathetic nervous system, ↓↓ BP.
- 20. Dose related ↓↓ CMRO2, reduces metabolic activity, neuronal signalling & impulse trafficking. ↓↓ CMRO2 ↓ ↑↑ cerebral vascular resistance ↓ ↓↓ cerebral blood flow ↓ ↓↓ Intracranial pressure Somatosensory, Brainstem auditory & visual evoked potential are depressed.
- 21. ↓↓ burst suppression, protect in profound hypotension. ↓↓ infract size in cerebral emboli & temporary focal ischemia.
- 22. High doses desulfurationHigh doses desulfuration pentobarbitalpentobarbital (long lasting CNS Depressant)(long lasting CNS Depressant)
- 23. Respiratory system . Neurogenic, Hypercapnic & hypoxic drive depressed. Depression of medullary & pontine ventilatory centres. Apnoea likely in presence of narcotics.
- 24. Cough & laryngeal reflexes not depressed until high doses given. Bronchospasm & laryngospasm likely in light plane, added by sympathetic depression
- 25. Cardiovascular system At 5 mg/Kg doses, 10-20 mmHg ↓↓ in BP due to sympathetic blockade. Compensated by carotid sinus baroreceptor mediated ↑↑ in peripheral sympathetic nervous system activity.
- 26. Leads to unchanged myocardial contractility & 15 – 20 beats/min ↑↑ in Heart Rate. Direct myocardial depression occurs at doses used to ↓↓ intracranial pressure.
- 27. Depression of sympathetic nervous system & medullary vasomotor center ↓ Dilatation of peripheral capacitance vessel ↓ Pooling of blood ↓ ↓↓ venous return ↓ ↓↓ cardiac output ↓ ↓↓ Blood Pressure
- 28. Changes exaggerated in hypovolemic patient, patient on B-blocker drugs & centrally acting anti hypertensive. Skeletal muscle ↓↓ Neuro muscular excitability.
- 29. 5) Kidney ↓↓ blood flow & GFR . 6) Suppression of adrenal cortex & ↓↓ cortisol level, but it is reversible.
- 30. 7) Liver ↓↓ hepatic blood flow Induction of microsomal enzyme & increase metabolism of drugs, For Ex. Oral-anticoagulant, Phenytoin, TCA, Vit. K, Bile Salt, corticosteroid. ↑↑ Glucouronyl transferase activity. ↑↑ δ aminolavilunate activity & precipitate porphyria’s.
- 31. Placental transfer occurs but drug metabolised by foetal liver & diluted by its blood volume so less depression.
- 32. CLINICAL USES 1) Induction 3 – 5 mg/Kg. produces unconsciousness in 30 sec. with smooth induction & rapid emergence. Loss of eyelid reflex & corneal reflex used for testing induction. Consciousness regained 10-20 Min. but residual CNS depression persist for more than 12 Hours. Dose requirement ↓↓ in early pregnancy, ↑↑ child with thermal injury.
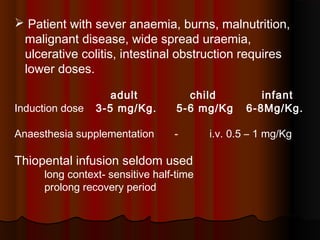
- 33. Patient with sever anaemia, burns, malnutrition, malignant disease, wide spread uraemia, ulcerative colitis, intestinal obstruction requires lower doses. adult child infant Induction dose 3-5 mg/Kg. 5-6 mg/Kg 6-8Mg/Kg. Anaesthesia supplementation - i.v. 0.5 – 1 mg/Kg Thiopental infusion seldom used long context- sensitive half-time prolong recovery period
- 34. 2) Anticonvulsant for rapid control of status epilepticus dose 0.5 – 2 mg/kg. repeated as needed
- 35. 3) Treatment of increased intracranial pressure Cerebral vasoconstriction ↓ ↓↓ cerebral blood Flow ↓ ↓↓ cerebral blood volume ↓ ↓↓ intracranial pressure ↓↓ cerebral metabolic O2 demand by 55% dose 1 – 4 mg/kg i.v.
- 36. 4) Cerebral Protection In focal ischemia eg. Carotid endarterectomy, thoracic aneurysm resection, profound controlled-hypotension, Incomplete cerebral emboli. Barbiturate narcosis – i.v. bolus 8 mg/Kg. EEG burst suppression – mean total dose 40 mg/Kg. Infusion – 0.05 to 0.35 mg/Kg/min with inotropic & ventilatory support.
- 37. SIDE EFFECTS Garlic onion taste. Allergic reaction. Local tissue reactions & necrosis. Urticarial rash, facial edema, hives, bronchospasm & anaphylaxis. Pain at injection site.
- 38. Cardiovascular system Cardiovascular depression a) Peripheral vasodilation & pooling of blood - ↓↓ BP. b) ↓↓ availability of Ca++ to myofibrils-↓↓ contractility. c) Direct negative inotropic action, ↓↓ ventricular filling. These changes more when i.v. bolus given If given to hypovolemic patient, reduces cardiac output (69%), in patient without compensatory mechanism cardiovascular collapse.
- 39. Respiratory System Dose related respiratory depression Transient apnea, patient with chronic lung disease more susceptible. Laryngospasm, bronchospasm. Central nervous system Emergence delirium, prolonged somnolence & recovery, Headache
- 40. Gastro-intestinal system Nausea, Emesis, Salivation Dermatologic Phlebitis, necrosis, gangrene. .
- 41. Contraindications Patient with respiratory obstruction & inadequate airway. Cardiovascular instability & shock. Status asthmaticus. Porphyria’s eg. Acute intermittent, variegate porphyria, hereditary copro-porphyria Known hypersensitivity.
- 42. CAUTION Hypertension, hypovolemia, ischemic heart disease, Acute adrenocortical insufficiency, Addison’s disease, myxedema. Uraemia, septicaemia, hepatic dysfunction. .
- 43. Accidental Intrarterial injectionAccidental Intrarterial injection Intense vasoconstrictionIntense vasoconstriction ThrombosisThrombosis Tissue necrosisTissue necrosis
- 44. TreatmentTreatment Intrarterial admininistration ofIntrarterial admininistration of Lignocaine(procaine).Lignocaine(procaine). HeparinisationHeparinisation Sympathectomy(stellate ganlion block,Sympathectomy(stellate ganlion block, brachial plexus block).brachial plexus block).
- 45. Thiopentone solution is highly alkaline incompatible for mixture with drug such as opioid catecholamines neuromuscular blocking drugs as these are acidic in nature. Probenecid prolongs action, aminophylline antagonize. CNS depressant eg. narcotics, sedative, hypnotic, alcohol, volatile anaesthetic agent prolongs & potentiate its actions. INTERACTIONS
- 46. Induces metabolism of oral anticoagulants, digoxin, B-blocker, corticosteroids, quinidine, theophylline. Action prolonged by MAO inhibitors, chloramphenicol.
- 47. Dose should be reduced In geriatric- 30- 40% decrease central compartment volume & slowed redistribution Hypovolemic Patient, High risk surgery patient with concomitant use of narcotic & sedatives