05 hand tendon
- 1. Department of Orthopaedics Seminar on: Flexors & extensor tendon injuries of hand. Chairperson and moderator: Prof. & HOD: Dr. Kiran Kalaiah Presenter : Dr. Yashavardhan.T.M
- 2. Introduction. Tendon injuries are the second most common injuries of the hand and therefore an important topic in trauma and orthopaedic patients. “A glistening structure between muscle & bone which transmit force from muscle to the bone’” Paratenon: Loose areolar tissue encasing tendon in low mechanical stress area Tendon sheath: a dense fibrous tissue tunnel enclosing tendon in high mechanical stress area 70% collagen (Type I) Extracellular components • Elastin • Muco-polysaccharides (enhance water-binding capability) Endotenon – around collagen bundles Epitenon – covers surface of tendon Paratenon – visceral/parietal adventitia surrounding tendons in hand
- 3. Most injuries are open injuries to the flexor or extensor tendons, but less frequent injuries, e.g., damage to the functional system tendon sheath and pulley or dull avulsions, also need to be considered. After clinical examination, ultrasound and magnetic resonance imaging have proved to be important diagnostic tools. Tendon injuries mostly require surgical repair, dull avulsions of the distal phalanges extensor tendon can receive conservative therapy.
- 4. Injuries of the flexor tendon sheath or single pulley injuries are treated conservatively and multiple pulley injuries receive surgical repair. In the postoperative course of flexor tendon injuries, the principle of early passive movement is important to trigger an "intrinsic" tendon healing to guarantee a good outcome. Many substances were evaluated to see if they improved tendon healing; however, little evidence was found. Nevertheless, hyaluronic acid may improve intrinsic tendon healing
- 5. Anatomical position Flexors muscles: FDP and FDS tendons have fibrous sheaths on the palmar aspect of the digits Fibrous arches and cruciate (cross-shaped) ligaments, which are attached posteriorly to the margins of the phalanges and to the palmar ligaments hold the tendons to the bony plane and prevent the tendons from bowing when the digits are flexed. The tendons are surrounded by a synovial sheath. Flexor tendon system consists of intrinsic and extrinsic components Extrinsics: FDP: flexing the DIP joint FDS: Flexing the PIP Joint FPL: Flexing the IP joint of the thumb Intrinsics: Lumbricals: Flex the MCP joints and Extend the IP joints FDP inserts on base of distal phalanx FDS inserts on sides of middle phalanx FPL inserts on proximal portion of the distal phalanx
- 6. INTEROSSEIUS, BLOOD SUPPLY & NERVE SUPPLY
- 7. Pulleys of flexour Synovial sheath is reinforced by a system of fibrous pulleys 5 annular pulleys (A) and 3 Cruciform pulleys (C) A1: 8-10 mm over MCPJ A2: 18-20mm over proximal phalanx A3: 2-4 mm over PIPJ A4: 10-12mm over middle phalanx A5: 2-4 mm over DIPJ C1, C2, C3 proximal to A3, A4, A5 Allow shortening of the pulley system in flexion A2 and A4 are considered most important. Their disruption leads to bowstringing, reduced mechanical efficiency and decreased flexion. Function: increase the mechanical efficiency by preventing bowstringing
- 8. ZONES OF FLEXOR TENDON INJURY Zone I: Between insertion of FDP and FDS Zone II: From insertion of FDS to A1 Pulley Zone III: Between A1 pulley and distal limit of carpal tunnel Zone IV: Within the carpal tunnel Zone V: Between the entrance of Carpal tunnel and musculo-tendinous junction. FDS decussation at A1 pulley FDS slips rotate 180° around FDP Slips rejoin at PIP – Camper’s Chiasma Insert on P2
- 9. Tendon nutrition Parietal paratenon Passive nutrition by diffusion Vincula and bony attachments Direct nutrition Segmental nutrition Vincula may prevent retraction Vascularity dominance is deep surface of tendon Consider with suture placement Biomechanically superior to place suture deep
- 10. TENDON HEALING Tendons are capable of actively participating in the repair process through Intrinsic Healing Tendon healing occurs in three phases: 1. Inflammation 2. Active repair 3. Remodelling • Early tendon motion has significant role in modifying the repair response • Mobilized tendons showed progressively greater ultimate load compared with immobilized tendons • Studies confirm “Wolff’s law” which states that the strength of a healing tendon is proportional to the controlled stress applied to it
- 11. ETIOLOGY sharp object direct laceration (broken glass, kitchen knives or table saws) crush injury avulsions burns animal or human bites suicide attempts motor vehicle accidents
- 14. ZONE 1: ZONE OF FDP AVULSION INJURIES Region b/w middle aspects of middle phalanx to finger tips Contains only one tendon-fdp Tendon laceration occurs close to its insertion Tendon to bone repair is required than tendon repair Leddy classification of zone I flexor tendon injuries Type I: tendon retracted into palm (fullness in palm) Type II: tendon trapped in the sheath at PIP (unable to flex PIP) Type III: tendon trapped in A4 pully
- 15. ZONE II-NO MANS LAND From metacarpal head to middle phalanx Called so because initial attempts for tendon repair here produced poor results FDS and FDP within one sheath Adhesion formation risk is amplified at campers chiasma In each finger, the FDS tendon enters the A1 pulley and divides into two equal halves that rotate laterally and then dorsally. The two slips rejoin deep to the FDP tendon over the distal aspect of the proximal phalanx and the palmar plate of the PIP joint at Camper's chiasma Insert as two separate slips on the volar aspect of the middle phalanx.
- 16. ZONE III-DISTAL PALMAR CREASE B/w transverse carpal ligament and proximal margin of tendon sheath formation Lumbricals origin here prevents profundus tendons from over acting Delayed tendon repairs are succesfull even after several weeks of injury
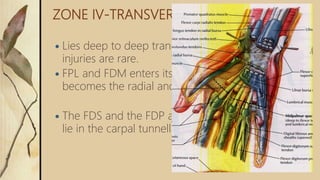
- 17. ZONE IV-TRANSVERSE CARPAL LIGAMENT Lies deep to deep transverse ligament. Tendon injuries are rare. FPL and FDM enters its continuous sheath which becomes the radial and ulnar bursae. The FDS and the FDP also enter a large sheath and lie in the carpal tunnell
- 18. ZONE V LIES PROXIMAL TO TRANSVERSE CARPAL LIGAMENT The Flexor tendons start in the distal third of the forearm at the musculotendinous junction The superficialis group lies palmar to the conjoined profundus tendon group covered by loose subcutaneous tissue and skin.
- 19. SIGNS & SYMPTOMS Unable to bend one or more finger joints Pain when bending finger/s Open injury to hand (e.g., cut on palm side of hand, particularly in area where skin folds as fingers bend) Mild swelling over joint closest to fingertip Tenderness along effected finger/s on palm side of hand Lies deep to deep transverse ligament Tendon injuries are rare
- 20. EXAMINATION: INSPECTION There is a normal arcade to hand with index finger showing least and little finger showing max flexion If affected finger shows more extension than other digits, chance of tendon injuries are high
- 21. Goals of reconstruction Coaptation of tendons anatomical repair multiple strand repair to permit active range of motion rehabilitation Pully reconstruction to minimize bow-stringing atraumatic surgical technique to minimize adhesions strict adherence to rehabilitation protocol.
- 22. Timing of flexor tendon repair: Primary: repair within 24 hours (contraindicated in case of high grade contamination i.e. human bites, infection) Delayed Primary: 1-10 days when the wound can be still pulled open without incision Early Secondary: 2-4 weeks. Late Secondary : after 4 weeks No repair if less than <25% laceration, only epitenon repair in 25-50% lacerations, core suture plus epitenon repair when >50% laceration Dorsal blocking splint for 6-8 weeks as conservative measure
- 23. Ideal tendon repair: Easy placement of sutures in the tendon Secure suture knots Smooth junction of tendon ends without gapping Minimal interference with vascularity strength
- 24. TECHNIQUES Retrieve the tendon ends through the sheath in an atraumatic manner Maintain the integrity of the pulley system (especially A2 and A4) Create “retinacular window” described by Lister for preserving the flexor sheath Extend the original laceration for better exposure Zigzag Mid-lateral Avoid linear scars that cross flexion crease
- 25. Milk the forearm with the wrist and MCP in flexion Do not attempt blind retrieval more than twice Make a separate incision if necessary Use a pediatric feeding tube to retrieve tendon stump
- 26. CORE SUTURE
- 28. Tendon Sheath Repair? Role of diffusion of nutrients from synovial fluid Tendon within the sheath have an intrinsic capacity for healing Gelberman and woo in 1990 study on dogs Reconstruction of the sheath did not significantly improve repaired tendons treated with early motion rehabilitation.
- 29. Partial Tendon Laceration Rupture, entrapment, triggering Partial laceration involving 60% or less are best treated by early mobilization WITHOUT tenorrhaphy
- 30. Profundus Tendon Avulsion Avulsion of FDP from its insertion by forced hyperextension Most common in the ring finger Leddy and Parker classification Based on the level to which the tendon retracts Status of the tendon vascular anatomy
- 31. Type I Profundus has retracted proximally into the palm Surgery should be done in 7-10 days before a fixed muscular contracture develops Least common Distal digital exposure to confirm diagnosis In Type I, a second distal palm incision will be needed Tendon is reinserted into the base of distal phalanx Distally based periosteal flap is raised distal to volar plate Tendon is sutured through drill holes in the distal phalanx and button tied over the nail plate
- 32. Type II Profundus retracts to PIP Disruption of Vinculum Breve Nutrition is maintained by Vinculum longum May be repaired up to 3 months Delay may convert type II into a type I if longum subsequently ruptures
- 33. Type III Attached bone fragment that fractures off the volar base of distal phalanx A4 pulley prevents proximal retraction Both Vinculae are preserved Type III attention is turned to ORIF
- 34. Complications Short term: Infection Injury to neurovascular structures or pulley system Abnormal scarring Long term: Adhesion Rupture Joint contracture triggering Adhesion Most common complication despite early motion protocols Tenolysis when patients progressive gain in digital motion has plateaued, usually 3-6 months after repair
- 35. Quadriga effect Tendon advancement shortens the FDP & completes the grip before the normal fingers, if the tension on tendon graft is set too high, and limit their flexion and thus week grip
- 36. Two stage technique Create a supple pseudosynovial sheath by implanting a silicone rod Soft tissue coverage or pulley reconstruction is performed at the first stage 8 weeks later, when psuedosynovial sheath is formed, the rod is replaced by a tendon graft 1. Palmaris longus and plantaris 2. Tendon grafts that include synovial sheath
- 37. Tendon Juncture Pulvertaft weave, with two or more passes through the proximal motor tendon
- 38. Distal end may be secured in multiple ways
- 39. Tension adjustment Proximal weave is adjusted Wrist is extended to flex the fingers into the cascade of the hand Overcorrect slightly because some stretching occurs after surgery
- 40. PULLEY RECONSTRUCTION Must be done during the first stage Well-healed pulley reconstruction facilitates early mobilization and gliding of tendon graft Reconstruction during the second stage increases the likelihood of pulley rupture and adhesion formation Material used Autogenous grafts: PL, Plantaris, to extensors, EIP, Extensor retinaculum, fascia lata
- 41. Flexor compartment of thumb.
- 42. Kleinert Protocol Combines dorsal extension block with rubber- band traction proximal to wrist Originally, included a nylon loop placed through the nail, and around the nail is placed a rubber band This passively flexes fingers, & the patient actively extends within the limits of the splint
- 43. Duran protocol At surgery, a dorsal extension-block splint is applied with the wrist at 20-30° of flexion, the MCP joints at 50-60° of flexion, and the IP joints straight
- 44. Extensor Tendons 1. Extrinsic System radial N innervated 2. Intrinsic System ulnar and median N innervated Extrinsic Extensors Wrist Extensors: ECRL, ECRB, ECU Finger Extensors: EDC, EIP, EDQM Thumb Extensors: APL, EPL, EPB EDC has a common muscle belly with multiple tendons EIP & EDM lie on the ulnar side of the respective EDC tendon
- 45. Thumb Extensors APL inserts on the metacarpal and radially abducts it EPB inserts on proximal phalanx and extends MCP Joint EPL inserts on distal phalanx and extends IP Joint Testing the Extrinsics: APL:Palpate with thumb abduction EPB:MP extension with IP flexion, palpate tendon EPL:Palpate tendon with retropulsed thumb EDC:Test with wrist in neutral-extension
- 46. Vascularity & Innervation Volar and dorsal metacarpal vessels Median nerve supplies radial one or 2 lumbricals Ulnar nerve supplies ulnar 2 lumbricals
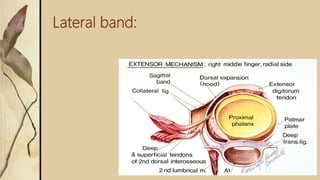
- 47. Extensor Apparatus EDC tendon trifurcates into central slip & 2 lateral slips Intrinsic extensor tendons join the lateral slips to form the lateral bands Winslow’s Rhombus The central slip inserting on the base of the middle-phalanx and two lateral slips inserting to the distal-phalanx.
- 48. Lateral band:
- 49. Juncturae Tendinium Functional roles: spacing of ED tendons force redistribution coordinate extension MP stabilization Ring finger has least independent extension due to the orientation of the juncturae The most common patterns single extensor indicis proprius inserting to the ulnar side of the index extensor digitorum communis a single extensor digitorum communis to the index finger a single extensor digitorum communis to the long finger, a double extensor digitorum communis to the ring finger, an absent extensor digitorum communis to the small finger, and a double extensor digiti quinti with double insertions
- 50. SAGITTAL BANDS Stabilize the common extensor during digital flexion over MCPJ Limit the excursion of the common extensor tendon during digital extension EDC allows extension of MP joint via insertion onto the sagittal bands There is usually no tendinous insertion of EDC to the dorsal base of the proximal phalanx No MP joint hyperextension: EDC extends MP, PIP, and DIP joints even in the absence of intrinsic muscle function. INTRINSIC PARALYSIS: “slack” develops in EDC system distal to the sagittal bands all producing a flexion posture at PIP and DIP joints, the “claw” finger.
- 51. Transverse & oblique fibres of Interosseous Hood Transverse & oblique fibres of Interosseous Hood 1) EDC Tendon 2) Central Slip 3) Lateral Slip 4) Intertendinous Connection 5) Volar Interosseous Muscle 6) Lumbrical Muscle
- 52. Triangular Ligament Connects both lateral bands over the middle phalanx. • Limits the volar and lateral shifting of the lateral conjoined extensor tendon during digital flexion • In boutonniere deformity; elongated • In fixed swan neck deformity; retracted
- 53. Retinacular Ligament Lateral continuation of the triangular ligament extending from the lateral margin of the lateral conjoined extensor tendon to PIPJ articular volar plat
- 55. Extensor Tendon Injury Extensor apparatus Extrinsic muscles (ED, EI, EDM) Intrinsic Muscles ( Lumbricals and Interossei) Fixed fibrous structures. Zone 1 • Mallet finger – persistent flexon of distal phalanx • Closed: splinting 6-8 weeks • Open: suture repair, Soft tissue reconstruction
- 56. Pullout Wire and K pin
- 57. Zone II injury- Middle Phalanx Level: • Repair by interrupted suture. • Immobilization for 5-6 weeks • DIP joint in extension • PIP joint left free
- 58. Zone III injury- PIP joint level Most complex anatomically and physiologically Causes two deformities Boutonniere disruption of central tendon Closed: splinting MCP and PIP in hyperextension for 6 weeks Open: suture repair (figure of 8 suture) Swan Neck excessive traction of central tendon Closed: splinting DIP & Open: suture repair
- 59. Zone IV injury- shaft of proximal phalanx level Repair relatively easy Adhesion is the problem
- 60. Zone V injury – MP joint level. Closed: splinting, 45 extension at wrist and 20 flexion at MCP & Open: suture repair by 5.0 prolene Zone VI injury- Metacarpal level Better prognosis than in fingers All structures, even inter-tendinous band should be repaired. Core type suture possible. Delayed suture is possible. Zone VII- wrist level Extensor tendons are under dorsal retinaculum. Retinaculum should be repaired or partially preserved. Adhesion is the Grasping core suture should be used. Immobilization for 5-6 weeks.
- 61. IMMOBILIZATION Keep the tendon in a shortened position through splinting or casting Tendons immobilized for 3 weeks In week 4, gentle active motion of the repaired tendon is introduced Rehabilitation depends on zone of injury
- 62. IMMOBILIZATION INJURIES IN ZONES PROXIMAL TO MCPs INJURIES IN ZONES DISTAL TO MCPs May be immobilized for 3 weeks. Afterwards, finger may be placed in removable volar splint between exercise periods for 2 weeks Progressive ROM after 3 weeks If full flexion is not regained rapidly, dynamic flexion may be started after 6 weeks Require a longer period of immobilization (usually 6 weeks) A progressive exercise program is initiated Dynamic splinting during day and static splinting at night to maintain extension
- 63. EARLY PASSIVE MOTION Extensors are held in extension by dynamic, gentle rubber band traction, and the patient is allowed to actively flex the fingers—passively moving repaired extensor tendons
- 64. EARLY ACTIVE MOTION Early active short arc program (developed by Evans) allows tendon to actively move 3 days after surgery Therapist must take care to ensure stress applied by early active motion does not overpower strength of surgical repair Splinting program is complex and specific and requires a skilled occupational therapist
- 65. Manchester Short Splint. Wrist ◦ Finishes at dorsal wrist crease ◦ Allows 45 degrees extension MCPJ ◦ 30 degrees flexion Exercises ◦ Commence 4th or 5th day ◦ Motion initiated at DIPJ
- 66. THANK YOU !!!
Editor's Notes
- #27: Massachusetts general hospital
- #40: cascade
- #43: Active range of motion rehabilitation
- #45: Eip extensor indicis proprios Edc exten digitorum comminus
- #62: The immobilization method maintains the tendon in a shortened position by way of splinting or casting. “Tendons are immobilized for three weeks; in week 4, gentle active motion of the repaired tendon is introduced” (Poole, 2013, p. 609).
- #63: Extensor tendons damaged proximal to the MCP joints frequently become adherent to the structures above and below them. This will require the occupational therapist to initiate a splinting program. A removable volar splint is utilized between exercise periods to protect the tendon for two additional weeks. Dynamic flexion splinting may be started 6 weeks after surgery to recover flexion if required (Poole, 2013, p. 609). Extensor tendons injured proximal to the MCP joint may be immobilized for 3 weeks. After this, the digit might be placed in a removable volar splint that is worn between exercise periods for an additional two weeks (Hall, 2010). Progressive ROM is initiated after 3 weeks, and if full flexion is not recovered promptly, dynamic flexion may be initiated after 6 weeks (Poole, 2013, p. 609). Extensor tendon injuries that occur distal to the MCP joint necessitate a longer period of immobilization—usually for 6 weeks. A progressive exercise program is then initiated with dynamic splinting during the day and static splinting at night to preserve extension (Poole, 2013, p. 609).
- #64: The early passive motion method reverses what was done for the flexor tendons (Hall, 2010). The extensor tendons are held in extension by dynamic, gentle rubber band traction, and the patient is permitted to actively flex the fingers, thus passively moving the surgically repaired extensor tendons. “These splints must have a dorsal component to provide a block to flexion so as not to move the tendons too much, which could lead to overstretching or rupture of the extensor tendon. This method facilitates tendon strength and can prevent the scarring that ultimately limits motion and function” (Poole, 2013, p. 609).
- #65: The early active short arc program, developed by Evans, permits the tendon to actively move 3 days after surgery. The therapist must take care to make sure that the stress applied by early active motion does not override the strength of the surgical repair. “The splinting program is quite complex and specific and requires a skilled occupational therapist” (Poole, 2013, p. 609).
- #66: 30 secs The Manchester guideline is for for robust uncomplicated repairs with compliant patients It has a dorsal blocking splint which finishes on the dorsal wrist crease which allows 45 degrees extension and full flexion. MCP joints are splinted at 30 degrees flexion Exercises commence on the 4th or 5th day Motion is initiated at the DIP joints, rather than the PIP or MCP joints In the early phase they do not encourage a full active fist They do not do place and hold READ FROM SLIDE ONLY (Info below only if questioned) Wrist 45 degrees extension – In 1988 Suave suggested that a wrist position of 45 degrees extension was optimal for minimising the force required to move the Ipj’s against passive resistance. Other authors have confirmed the superiority of synergistic wrist motion on tendon glide. In Manchester they have removed the forearm part of the splint for compliant patients with uncomplicated repairs. The splint is fabricated to finish at the proximal wrist crease, allowing the wrist to extend to 45 degrees during active digital flexion and to flex during active digital extension (demo with model) Care must be taken in the position of the MCP joints Fiona writes in her article that In an oedematous finger, where there is resistance to tendon glide, placing MP joints in excessive flexion, will bias motion to the PIPj and force the patient to attempt DIPjoint flexion at the end of range, thereby increasing the work of flexion Therefore too much MCP joint flexion rather than being protective, actually increases the risk of rupture. A common complication of injuries in zone 2 is cross union of the flexor tendons. During active motion it is paramount that motion is initiated from the DIP joint to optimise differential glide. Fiona writes that therefore, a position of 30 degrees MCP join flexion is both effective and comfortable Oedema peaks around 3rd or 4th day increasing WOF. Fiona writes that it is judicious to commence the exercise regimen when the gliding resistance is likely to be lower at around the 4th or 5th day post op. Motion should be initiated at the DIPj to maximise differential glide During the early phase of rehabilitation motion should be confined to the outer range or first third of flexion. She writes that early range of flexion is not necessary or safe Care should be taken if using a ‘place and hold’ regimen that patients are not required to put a greater effort into holding a full fist position.