ARDS (Case study)
- 1. Patrick Laird, DNP(C), MSN, RN, ACNP-BC, CCRN; Susan D. Ruppert, PhD, RN, ANP-BC, NP-C, FCCM, FAANP, 2011. Published on Wolters Kluwer Health Case Study
- 2. Pathophysiology of the disease ECMO Summary First patient encounter Day 2-4 V/S P/E Lab result CXR Plan Outline:
- 3. 55 y/o male recently diagnosed with influenza A. Presented to the emergency department (ED) accompanied by his wife with worsening shortness of breath, fever, productive cough ( green ) sputum, and new onset altered mental status. Primary assessment revealed oxygen saturation of 61% on room air. Respirations were labored with abdominal accessory muscle use. BIPAP was used but his respiratory status continued to deteriorate ------- ( intubation ) . Difficult intubation.
- 4. After intubation the patient became hypotensive. A Levophed drip was initiated. Once hemodynamically stable the patient was admitted to the intensive care unit (ICU) for continued management. Continue
- 5. CHIEF COMPLAINT : “Shortness of breath and confusion” PAST MEDICAL AND SURGICAL HISTORY : • Hypertension — Diagnosed in 2009. • Hyperlipidemia — Diagnosed in 2009. • No history of surgical procedures. • Denied any history of smoking and drinks approximately 2 alcoholic beverages per week. SOCIAL AND FAMILY HISTORY : Married for 28 years , Employed with Anadarko petroleum division. His parents both diagnosed with hypertension treated with medication.
- 6. CURRENT HOSPITAL MEDICATIONS : Levophed infusion at 0.4 μg/kg/min intravenous (IV). Propofol infusion at 55 μg/kg/min IV. Protonix 40 mg IV daily. Lovenox 40 mg subcutaneous daily. Azithromycin 500 mg IV daily.
- 7. REVIEW OF SYSTEMS : Patient orally intubated at the time of interview and examination. Chest : Complains of increased dyspnea and cough with increased green sputum production 2 days prior to admission. Heart: Complains of weakness for 10 days prior to arrival. Urinary system: decrease in normal urinary output because of decreased oral intake.
- 8. Neurological : His wife reports change in his mental status over last 2 days. States patient is “not making any sense and is saying inappropriate things.
- 9. Day 2
- 10. Vent management: IBW = 90 Kg A/C VC Tube size 8 Fr, at point of 22 near lip line.
- 11. VS: Temp.: 37.2oC. HR: 93b/min. RR: 16 b/min. BP: 8950 mmHg. O2 Sat.: 86% Day 2
- 12. Overall status: General: well nourished. Skin: No skin rashes/lesions observed. HEENT. Chest: Symmetrical expansion. Heart: (S1, S2) are noted. Regular rhythm. No murmurs, gallops, or rubs are appreciated. Abdomen: Soft, nontender and nondistended. Day 2
- 13. Cont. Extremities: Warm. No edema, clubbing, or cyanosis was appreciated. Capillary refill: +2 seconds. Nail beds are pale. Neurological: Sedated on mechanical ventilation. Spontaneous movement of all 4 extremities is noted. Does not follow verbal commands. Day 2
- 14. CXR: Endotracheal tube tip located 2 cm above the carina. Interval worsening perihilar air space opacity suggestive of worsening pulmonary edema or ARDS. No pneumothorax or pleural effusion. Day 2
- 15. ABG: parameters Values pH: 7.42 PCO2: 41 mmHg. PO2: 34 mmHg. HCO3: 26 mmol/L Normal acid base balance with sever hypoxemia. Day 2
- 16. CBC WBC 10.2 kg/mm3 4.0-10 kg/mm3 Hb 15.1 gm/dL 13.0-16.8 gm/dL Platelets 325 kg/mm3 150-430 kg/mm3 Na 143 mEq/L 135-148 mEq/L K 3.9 mEq/L 3.5-5.5 mEq/L Cl 97 mEq/L 98-106 mEq/L BUN 42 mg/dL 10-26 mg/dL Cret. 2.2Mg/dL 0.5-1.2 mg/dL BNP 18 0-100 pg/mL Day 2
- 17. DIAGNOSTIC IMPRESSIONS Differential Diagnoses: ALI, ARDS, pneumonia, cardiogenic pulmonary edema, PE. Working diagnosis Acute respiratory distress syndrome (ARDS). Additional Diagnoses: CAP, severe sepsis, recent influenza A (H1N1), and acute renal failure. Day 2
- 18. ARDS
- 19. Berlin definition: ARDS is an acute, diffuse, inflammatory lung injury , defined by: Severity is defined by degree of oxygenation impairment.
- 20. RISK FACTORS: Direct “pulmonary etiologies” Indirect “extrapulmonary etiologies”? Pneumonia. Aspiration. Inhalational injury. Pulmonary contusion. Fat emboli. Sepsis. massive blood transfusion. Burns. Acute pancreatitis. Severe trauma.
- 21. Pneumonia 35% Sever Sepsis 26% Aspiration 15% Trauma 11% Other 13% Causes of ARDS June 20, 2012,
- 22. Pathophysiology: ↓ surfactant Accumulatio n of fluid Atelectasis Pulmonary edema ❶ ❷
- 23. Pathophysiology Consequences of lung injury include: Impaired gas exchange V/Q mismatch Increased dead space Decreased compliance
- 24. PLAN The main goal is to optimize oxygenation and prevent further inflammation that may lead to multi-organ failure and that may done by : Low tidal volume Low PEEP/high Fio2 Initial ventilator settings made by ED physician were not compliant with current therapy recommendations. Ventilator settings were adjusted in the ICU immediately following initial evaluation. Day 2
- 25. Ventilator management A/C VC IBW = 90 Kg VT= 8mL/Kg = 700mL PEEP= 10 cm H2O RR = 18 bpm Fio2 = 100% VT= 6mL/kg = 540mL PEEP= 14 cm H2O Day 2
- 26. Community Acquired Pneumonia .. For the treatment of CAP for patients in the ICU include a B-lactam, and either azithromycin or a respiratory fluroquinolone. Patients with a penicillin allergy should receive a respiratory fluroquinolone and aztreonam.
- 27. Neuromuscular blocking agents (NMBA) Are used : In the ICU to facilitate and optimize mechanical ventilation. To improve chest wall compliance, eliminate dysynchrony, and reduce peak airway pressures. Muscle paralysis used : In decreasing the work of breathing and respiratory muscle blood flow thereby reducing oxygen consumption
- 28. Cont. The patient displayed mild ventilator dysynchrony and refractory hypoxemia. Paralytics were initiated to gain full control of ventilation and eliminate ventilator asynchrony. Once paralytics were initiated, the patient’s ventilator asynchrony resolved.
- 29. Day 4
- 30. Subjective data .. • Remains critically ill. • Orally intubated on mechanical ventilation. • Oxygen saturations remain less than 86%. Day 4
- 31. Objective data .. oVital Signs: • T = 38.4 C • Pulse = 102 B/min • RR = 20 B/min • BP = 101/52 • O2 sat =84 % Day 4
- 32. Physical examination .. No murmurs, gallops, or rubs.CV Bilateral breath sounds with course crackles; diminished in bilateral bases; no wheezes noted. RESP Warm, 2+ pitting edema to bilateral lower extremities, no cyanosis or clubbing noted. EXT Paralyzed on Nimbex drip at 3 μg/kg/min , Sedated on propofol infusion at 50 μg/kg/min. NEURO Day 4
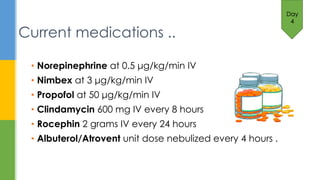
- 33. • Norepinephrine at 0.5 μg/kg/min IV • Nimbex at 3 μg/kg/min IV • Propofol at 50 μg/kg/min IV • Clindamycin 600 mg IV every 8 hours • Rocephin 2 grams IV every 24 hours • Albuterol/Atrovent unit dose nebulized every 4 hours . Day 4 Current medications ..
- 34. Chest X-ray films .. • Bilateral infiltrates and pulmonary edema • Endotracheal tube in adequate position above the carina. Day 4
- 36. ASSESSMENT .. • ARDS • Metabolic acidosis • Septic shock • Community acquired pneumonia • Acute renal failure • Recent influenza A (H1N1) Day 4
- 37. PLAN .. Despite optimal medical therapy, the patient failed conventional treatment, and without further intervention death was eminent. Day 4
- 38. Controversial ( adults ) Common indications for use of ECMO in adults include postcardiotomy, postcardiac transplant, severe refractory heart failure, ARDS, pneumonia, trauma, or primary graft failure following lung transplant. Consult cardiovascular surgeon for placement of extracorporeal membrane oxygenation (ECMO):
- 39. Use of ECMO results in 1 extra survivor for every 6 patient treated .
- 40. A total of 201 adult patients received mechanical ventilation for confirmed or suspected influenza. 68 of these patients received ECMO and the remaining 133 received conventional mechanical ventilation. 48 patients (71%) that received ECMO survived to ICU discharge and 32 patients survived to hospital discharge. Overall mortality of the ECMO group was 21%. The researchers contributed the lower mortality to the age of the study participants and the cause of ARDS (H1N1).
- 41. Use of ECMO has a multitude of potential complications including life-threatening bleeding, coagulopathy, air embolism, thromboembolism, intracerebral hemorrhage (in neonates), and limb ischemia. risks must carefully be weighed against benefit prior to initiation
- 42. Despite optimal medical therapy, the patient failed conventional treatment, and with- out further intervention death was eminent. After consulting cardiovascular surgery, available therapy options were discussed with the patient’s spouse and the decision was made to place the patient on ECMO as salvage therapy. In this scenario
- 44. VT = 4-6 ml/kg RR= 5-10 bpm PEEP= 12-15 cm H2O Inspiratory time longer FiO2= 0.21 Recommended Ventilator Settings
- 45. day 4 : taken to OR , ECMO was initiated. ECMO for 6 days day 10 ,returned to the OR for removal of ECMO and insertion of a percutaneous tracheostomy , and percutaneous endoscopic gastrostomy (PEG) tube placement
- 46. continued to make marked improvements following removal of ECMO . Day 18 :was weaned from the ventilator. Physical therapy, occupational therapy, and speech therapy were consulted. Day 21, the patient was discharged from the ICU. day 25 transferred to a long-term acute care (LTAC) facility for continued physical and occupational therapy
- 47. On day 25 transferred to a long-term acute care facility for continued physical and occupational therapy( 2 weeks ). The patient was discharged to his home with no physical or cognitive deficits noted. Since his discharge from LTAC, the patient has returned to work and has no limitations .
- 48. Summary
- 49. 55 y/o male recently diagnosed with influenza A. Presented to the emergency department (ED) accompanied by his wife with worsening shortness of breath, fever, productive cough ( green ) sputum, and new onset altered mental status. This case study explores the management of an unusually complicated case of (ARDS) extending over 52 days of hospitalization. Despite the utilization of conventional medical treatments and optimum respiratory support modalities, the patient’s condition worsened and death was imminent without salvage therapy. After cardiovascular surgery consultation, (ECMO) therapy was initiated for 6 days. The patient recovered and was able to return to regular employment.
- 50. Conclusion Acute respiratory distress syndrome (ARDS) is a life- threatening medical condition where the lungs can't provide enough oxygen for the rest of the body. ARDS can affect people of any age and usually develops as a complication of a serious existing health condition. (ARDS) has a mortality rate of 34% to 58% .
Editor's Notes
- #4: Flu (influenza) viruses are divided into three broad categories: influenza A, B or C. Influenza A is the most common type. H1N1 flu is a variety of influenza A. Influenza A viruses are divided into subtypes based on two proteins on the surface of the virus: the hemagglutinin (H) and the neuraminidase first Intubation ------- without success. A Combi-tube was placed then replace it with a traditional endotracheal tube.
- #5: to keep the mean arterial pressure greater than 70 mm Hg.
- #7: Levophed :Treating low blood pressure Prpofol : sedative Sodium chloride inhalation can remove certain bacteria in body secretions. / n catheter flush injections or intravenous infusions Protonix :is a proton pump inhibitor that decreases the amount of acid produced in the stomach. Levonex :Anticoagulant Azithromycin : antibiotic.
- #8: Information was gath- ered from the spouse and from the patient’s chart.
- #12: Interpretation.
- #13: Go through each more in details.
- #14: Go through each more in details.
- #16: Brain-natriuretic peptide: -18 < refer to the lecture for more info.
- #21: Indirect – acute systemic inflammation response
- #23: Direct or indirect injury to the alveolus causes alveolar macrophages to release pro-inflammatory cytokines Cytokines attract neutrophils into the alveolus and interstitum, where they damage the alveolar-capillary membrane (ACM). ACM integrity is lost, interstitial and alveolus fills with proteinaceous fluid, surfactant can no longer support alveolus
- #24: V/Q mismatch = shunt VD = Results in high minute ventilation Dec.C = Fluid filled lung becomes stiff
- #26: height—72 inches
- #27: CAP originates outside of the hospital may becaused by Streptococcus pneumoniae, Mycoplasma pneumoniae, Haemophilus influenzae, and Chlamydophila pneumoniae
- #39: Use of ECMO in adults remains controversial. Two early randomized controlled trials utilizing ECMO in adults failed to identify any benefit of therapy.