bbec55_b34400a7914c42429908233dbd381773.pdf
- 1. Pharmacology of NSAIDS & DMARDS Newman Osafo PhD Senior Lecturer Department of Pharmacology Faculty of Pharmacy and Pharmaceutical Sciences College of Health Sciences Kwame Nkrumah University of Science & Technology, Kumasi, Ghana Lecture
- 2. Objectives § After studying this material and attending lectures you should be able to: § Know the biochemical pathways for eicosanoids production § Know the effects produced by the eicosanoids and their mechanism of action. § Understand the consequences of blockade of synthesis or action of the eicosanoids. § Describe the mechanisms of action of the NSAIDs and the DMARDs. § Know the therapeutic uses of NSAIDs and the DMARDs in relation to RA. § Understand the pharmacotherapy of gout. 2
- 3. §The eicosanoids are derived from the regulated action of acyl hydrolase on constituent membrane phospholipids to generate fatty acid precursors. §The enzymatic activity of interest is PLA2 liberating arachidonic acid. 3
- 4. Arachidonic acid metabolism 4 LOX inhibitor Zileuton 15-Lipoxygenase 12-HETE (Chemotaxin)
- 5. Actions of the eicosanoids §Prostaglandins contribute to the symptoms of inflammation along with other autacoids such as histamine and bradykinin. §PGE2 and PGI2 cause vasodilation of arterioles and venules causing increased blood flow which leads to erythema = REDNESS §Oedema is also caused in part by prostaglandins 5
- 6. Pain § PGs directly sensitize pain fibers so they respond to normally innocuous stimuli (hyperalgesia). § Subdural injection of PGE1 with small amounts of bradykinin or histamine is very painful. Fever § Endogenous PGE2 and exogenous PGF2α and PGI2 increase body temp. § A common cause is the production of pyrogens released by neutrophils fighting a bacterial infection (IL-1). § Pyrogens are thought to cause release of PGs in the preoptic area of the hypothalamus. The net effect is an imbalance in heat production and loss leading to fever. 6
- 7. §Inhibition of PG synthesis in the CNS causes cutaneous vasodilation and increases heat loss thus, reducing the fever. §A general reduction of PG synthesis in the brain and in inflamed tissues probably also reduces the symptoms of fever. §PGD2 induces physiological sleep via DP1 interaction and secondary release of adenosine. 7
- 8. The inflammatory response §Increase Prostaglandin Synthesis results in: §Increased capillary permeability (mediates local erythema and edema) §Increased sensitivity of pain receptors §Increased platelet aggregation §Increased Body temperature §Potential hypertension, neurologic disorders and respiratory dysfunction 8
- 9. Eicosanoids of therapeutic benefits Drug Name Analog of Clinical Use Epoprostenol; iloprost; selexipag PGI2 Pulmonary hypertension, useful in hemodialysis to harvest platelets Dinoprostone PGE2 Cervix dilation in inducing labor Misoprostol PGE1 Peptic ulcer prevention; labor induction; combined with mifepristone (RU-486) as abortifacient Alprostadil PGE1 Maintain a patent (open) ductus arteriosus in neonates with congenital heart disease awaiting surgery; Erectile dysfunction treatment due to its smooth muscle relaxing effect (Caverject) Carboprost tromethamine PGF2a Labor induction Latanoprost PGF2a Topically used to decrease intraocular pressure in open- angle glaucoma or ocular HPT 9
- 10. §Others §Lubiprostone is a PGE1 derivative that activates chloride channels and increases gastrointestinal secretions. §It is used for irritable bowel syndrome with constipation. §Other PGF2a analogs used in open-angle glaucoma and ocular HPT include bimaprost, tafluprost, travoprost §Bimaprost is used in hypotrichosis. 10
- 11. Inhibitors of eicosanoid production Phospholipase A2 Arachidonic acid Prostaglandins & thromboxanes Lipoxygenase products (leukotrienes) Cyclooxygenase (COX) Lipoxygenase Inflammatory effects (esp. in asthma) Inflammatory effectsHomeostatic functions NSAIDS (including aspirin) 5-ASA (IBD) Zileuton 11 montelukast, zafirlukast Pranlukast
- 12. Non-steroidal anti-inflammatory agents [NSAIDs] §Aspirin and other Salicylates §Non-selective COX Inhibitors §propionic acids e.g., ibuprofen, ketoprofen, naproxen §oxicam derivatives e.g., piroxicam, §indole derivatives e.g., indomethacin, sulindac, etodolac §Selective COX-2 Inhibitors 12
- 13. NSAIDs §Analgesia §All drugs in this class relieve pain, but the type of pain is important. These drugs are most effective against mild to moderate pain, particularly pain due to inflammation. §Postoperative pain often responds favorably to aspirin and related drugs. Myalgia, arthralgia and neuralgia also respond well. §In contrast to the opiates, aspirin-like drugs are not addictive and do not alter sensory perception (except for perception of cutaneous pain). §Pain emanating from the hollow viscera is not relieved. 13
- 14. NSAIDs §Antipyresis §The anti-inflammatory drugs reduce fever, but this application is limited to the less toxic agents, e.g., aspirin. §Relief of fever with drugs does not eliminate the cause of the fever 14
- 15. NSAIDs §Anti-inflammatory Action §Treatment of inflammatory disease such as RA, and ankylosing spondylitis is a major clinical use. §Aspirin is still the reasonable DOC for newly diagnosed RA but does not satisfy the patients need for a "prescription". § The pain and inflammation of arthritis are relieved, but the progressive degeneration of the joints is not prevented. 15
- 16. Mechanism of NSAID action [eicosanoid synthesis inhibition] §Eicosanoids include §Prostaglandins, Thromboxanes and Leukotrienes §Cells subjected to trauma increase production of Prostaglandins §Synthesis of Prostaglandins and Thromboxanes are catalyzed by the enzyme Cyclooxygenase 16
- 17. Non-steroidal anti-inflammatory drugs (NSAIDs) §All NSAIDs inhibit the cyclooxygenase (COX) required for conversion of arachidonic acid to endoperoxide intermediate (PGG2 and PGH2). §arachidonic acid →endoperoxide →PGG2 →PGH2 →prostaglandins + prostacyclin + thromboxane §Some NSAIDs even block synthesis of leukotrienes § Inhibition of Cyclooxygenase eliminates a cells inflammatory response including § Pain § Fever § Platelet Aggregation 17
- 18. §Structural differences of cyclooxygenase: §COX1: mostly expressed in tissues. §COX2: is synthesized by inflammatory factors at the site of inflammation. §NSAIDs inhibit PG and TX synthesis, they are potent inhibitors of cyclooxygenase and eliminate all PGs and TX in every cell they reach 18
- 19. Aspirin §Unique among the NSAIDs in irreversible blockade of COX. §It is rapidly deacetylated by esterases producing salicylate which has antipyretic, anti-inflammatory and analgesic effects. §Blockade of prostaglandin synthesis at the thermoregulatory centers in the hypothalamus and at the peripheral target sites § e.g., PGE2 is thought to sensitize nerve endings to the action of bradykinin, histamine and other chemical mediators released locally by the inflammatory process 19
- 20. §Prevent the sensation of pain receptors to both mechanical and chemical stimuli §Also depress pain stimuli at subcortical sites §No effect on normal body temperature 20
- 21. § For the management of pain of low to moderate intensity arising from integumental structures rather than that arising from the viscera § NSAIDs are superior to opioids for the management of pain in which inflammation is involved § Combination of opioids and NSAIDs are effective in treating pain caused by a malignancy. 21
- 22. Adverse effects Gastrointestinal Distress § Normally PGI2 inhibits gastric acid secretion and PGE2 and PGF2 stimulate synthesis of protective mucus in both the stomach and small intestine § BUT in the presence of aspirin, prostanoids are not formed § Þepigastric distress, ulceration, hemorrhage 22
- 23. §Proton pump inhibitors are used in the treatment of gastric damage induced by NSAIDs or as a prevention during chronic treatment by NSAIDs §Agents such as Flurbiprofen-conjugated to NO are currently being developed to decrease the mucosal damage produced by NSAIDs. 23
- 24. Effect of aspirin (NSAIDs) on platelets §Normally TXA2 enhances platelet aggregation, whereas PGI2 decreases it §Low doses aspirin can irreversibly inhibit TX production in platelets without markedly affecting TXA2 production in the endothelial cells of the blood vessel §The lack of TX persists for the lifetime of the platelet (3-7 days) §¯TXA2 Þ platelet aggregation is reduced, producing an anticoagulant effect with a prolonged bleeding time. 24
- 25. Effect of aspirin (NSAIDs) on kidney §Normally PGE2 and PGI2 are responsible for maintaining renal blood flow and glomerular filtration through their local vasodilating effects. §During the treatment by NSAIDs, decreased synthesis of PGs can result in oedema and hyperkalemia in some patients. §Interstitial nephritis can also occur with all NSAIDs. § Read on the role of PGs in Bartter syndrome 25
- 26. Therapeutic use of aspirin (NSAIDS) §Antipyretic, analgesic, anti-inflammatory §Rx of gout, rheumatic fever, RA §Salicylic acid is used topically to treat corns, calluses, epidermophytosis §Cardiovascular applications of aspirin (salicylates): to inhibit platelet aggregation. Low doses of aspirin prophylactically to decrease the incidence of transient ischemic attack and unstable angina in men as well as coronary thrombosis 26
- 27. Pharmacokinetics of salicylates §Absorption - Rapidly absorbed from the stomach and upper intestine. Aspirin is rapidly hydrolyzed to salicylate by enzymes circulating in the plasma, liver and erythrocytes. Salicylic acid and methyl salicylate, which are used in analgesic ointments, are rapidly absorbed from the skin. §Distribution - widely distributed throughout the fluids of the body including the synovial fluid, an important site of anti- arthritic-pain action. Salicylate does not readily enter the CSF due to the high fraction in the plasma that is ionized. Salicylate and aspirin are highly bound to plasma proteins. 27
- 28. §Metabolism - Salicylates are metabolized by the liver primarily to glycine conjugates and are excreted by the kidneys. 28
- 29. Adverse effects §GIT: epigastric distress, nausea, vomiting, microscopic GIT bleeding §Blood: prolonged bleeding time Þ should not be taken for at least one week prior to surgery. When salicylates are administered, anticoagulants may have to be given in reduced doses. §Respiration: Higher synthesis of leukotrienes Þ irritation of respiratory tract. In toxic doses salicylates cause respiratory depression and a combination of uncompensated respiratory and metabolic acidosis. 29
- 30. §Hypersensitivity: Urticaria, bronchoconstriction or anaphylaxis, angioneurotic oedema §Reye syndrome: Happens during viral infection. Often fatal, culminating in hepatitis with cerebral oedema. Especially in children Þ contraindicated till 12 years, they should use acetaminophen to reduce fever §Reye Syndrome is marked by fatty degenerative liver failure and non-inflammatory encephalopathy. 30
- 31. Toxicity of salicylates & treatment §Mild intoxication: it is called salicylism. §Nausea, vomiting, marked hyperventilation, headache, mental confusion, dizziness, tinnitus. §Severe intoxication: commonly happens in children. § CNS disturbances, skin eruptions and serious acid-base imbalance. § Acute accidental or intentional overdose is the most common cause of severe toxicity in older patients 31
- 32. §Salicylate intoxication is a potentially fatal medical emergency. §Treatment depends on the symptoms and may include gastric lavage, reducing hyperthermia and treating acid-base imbalance with bicarbonate solution and glucose to reverse metabolic acidosis. §Blood transfusion and vitamin K may reverse hemorrhage, and dialysis may be necessary to clear plasma salicylate. 32
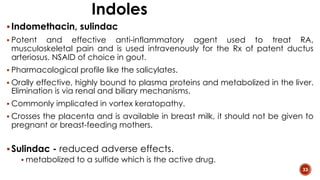
- 33. Indoles §Indomethacin, sulindac § Potent and effective anti-inflammatory agent used to treat RA, musculoskeletal pain and is used intravenously for the Rx of patent ductus arteriosus. NSAID of choice in gout. § Pharmacological profile like the salicylates. § Orally effective, highly bound to plasma proteins and metabolized in the liver. Elimination is via renal and biliary mechanisms. § Commonly implicated in vortex keratopathy. § Crosses the placenta and is available in breast milk, it should not be given to pregnant or breast-feeding mothers. §Sulindac - reduced adverse effects. § metabolized to a sulfide which is the active drug. 33
- 34. Fenamates § Mefenamic acid and Meclofenamate § Mefenamic acid inhibits cyclooxygenase and has analgesic, antipyretic and anti-inflammatory actions. § Meclofenamate may also block PG receptors. § The major limiting adverse effect is potentially severe gastrointestinal irritation leading to severe diarrhea. § Mefenamic acid is extensively bound to plasma proteins and can displace several drugs including the oral anticoagulants. § It may offer some benefits in Alzheimer’s disease (PMID: 16223958; PMID: 34150033). § These agents decrease fertility in animal studies. No data is available in humans. Should not be given to pregnant or breast-feeding mothers. 34
- 35. Benzopyrrole § Tolmetin § Has anti-inflammatory, analgesic and antipyretic activity. § It is a more potent anti-inflammatory drug than aspirin, but less potent than indomethacin. The primary use of the drug is in treatment of RA § Adverse effects include gastrointestinal and CNS effects, tinnitus and rashes. § Tolmetin is excreted in breast milk and should be avoided by nursing mothers. § Tolmetin binds extensively to plasma protein but is unusual for the nonsteroidal anti-inflammatory drugs in that it does not increase clotting time if given with warfarin. 35
- 36. Propionic acid derivatives § Ibuprofen, Naproxen, Ketoprofen, Fenoprofen, Flurbiprofen, Oxaprozin § Have analgesic, antipyretic and anti-inflammatory effects. § This group has advantages over aspirin and indomethacin in treating arthritis because side effects are less frequent and less severe. § The major adverse effect is gastrointestinal distress which is less severe than with aspirin or indomethacin. Increased bleeding time is also a potentially important side effect. § The propionic acid derivatives are all highly bound to plasma proteins and there is potential for serious drug-drug interaction with warfarin and possibly oral hypoglycemics. 36
- 37. Propionic acid derivatives § Flurbiprofen § It is used for postoperative analgesia and ophthalmic pain. § Sodium salt available for topical ophthalmic formulation for inhibition of intraoperative miosis. § Its use is associated with cogwheel rigidity, ataxia and myoclonus (muscle jerks). § Ibuprofen § Effective in closing patent ductus arteriosus in preterm infants (safer than indomethacin). § Decreases TNF-a and IL-1β. § Causes “compensated hypogonadism” with decrease testosterone product and 20 increase in LH/FSH. This results in normal testosterone levels but a stressed system. 37
- 38. Propionic acid derivatives § Naproxen § Naproxen’s free fraction is significantly higher in women than in men, but half-life is similar in both sexes. § Naproxen is effective for OA, RA, pain, and bursitis/tendonitis. § It is also used to treat JIA, acute gout, and migraine. § It has a more favourable cardiovascular risk profile than ibuprofen. 38
- 39. Oxicams § Piroxicam § Nonsteroidal anti-inflammatory, analgesic, antipyretic agent used to treat OA, RA and JRA. § Long plasma half-life (50 h) allows once-a-day dosing for chronic arthritis. § Meloxicam § Relatively selective for COX2 than COX1 inhibition but at high doses it is non-selective. § This can be an advantage if patient compliance is a problem. § Very high plasma protein binding (99%). § G.I. distress is most common side effect but less severe than piroxicam. 39
- 40. Phenylacetic acids §Diclofenac, aceclofenac § Diclofenac is available in potassium, sodium, and epolamine salts. § In addition to inhibition of COX activity, diclofenac appears to block the release of arachidonic acid in leukocytes which may participate in its anti- inflammatory effects. § Diclofenac undergoes significant (50%) first-pass effect and exhibits very high plasma protein binding (99%). In addition, this drug appears to accumulate in synovial fluid explaining its longer therapeutic effect than plasma T1/2. § In addition to GI side effects, hepatic toxicity is known, and hepatic transaminases should be followed. This drug is useful in the treatment of RA, osteoarthritis and ankylosing spondylitis. § Diclofenac is embryotoxic in animal studies and should be avoided in pregnant women or in nursing mothers. 40
- 41. Others § Nimesulide § Sulfonanilide, weak inhibitor of PG synthase but good blocker of leukocyte function. § Also blocks metalloproteinase activity on articular chondrocytes. § useful in patients who are allergic to aspirin or other NSAIDs. § Ketorolac § Potent agent with the usual spectrum of activities, analgesic, antipyretic and anti- inflammatory. § Chemically related to indomethacin and is 40x as potent an anti-inflammatory as ibuprofen. § The major advantage offered with this drug is that it can be given by im injection or orally. It is indicated for use in the treatment of pain but is not recommended for use beyond 1-2 weeks. § Dazoxiben, Primogrel and Ridogrel § Thromboxane synthase inhibitors being developed for treatment of vascular ischemia and thrombosis. Ridogrel also blocks TX receptor as well as blocking the synthase. 41
- 42. § Etodolac § less GI side effects compared to aspirin. Uses and precautions are the same as for other NSAIDs. § Nabumetone (Relafen) § The only non-acid NSAID in current use and resembles naproxen in structure § Not a very good COX inhibitor but it is a good anti-inflammatory. § May work through other pathways and thus, could be useful in combination with other NSAIDs. § Recent evidence suggests that this drug is an inhibitor of COX-2, the inducible form of cyclooxygenase as well as COX-1. § It is a pro-drug that is converted to the active form in the liver. § The incidence of GI ulceration is lower than that seen with most other NSAIDs. 42
- 43. Drug interactions of NSAIDs § Drug interactions of clinical significance include avoidance of concurrent therapy with agents that cause hypoprothrombinemia, thrombocytopenia or gastric ulceration. § Propionic acids (ibuprofen et al.) can compete with phenytoin for protein binding. § The concurrent use of cephalosporin antibiotics and NSAIDs may increase the risk of bleeding. § In general, the use of two NSAIDs is unwarranted due to the increase incidence of gastric side effects. 43
- 44. Drug interactions of NSAIDs § Concurrent use of NSAIDs and lithium can result in increases in plasma lithium concentrations of as much as 50% due to decrease in the clearance of lithium by NSAIDs. § Methotrexate use in conjunction with NSAIDs is cautioned. Specifically, methotrexate should not be used with phenylbutazone due to the risk of agranulocytosis or bone marrow depression. § It is recommended that NSAIDs be withheld for 24 to 48 hours prior and for 12 hours following methotrexate dosing. § Indomethacin may cause ¯ renal excretion aminoglycosides or digitalis leading to plasma levels and potential toxicity. § Probenecid increases the plasma concentration of NSAIDs. 44
- 45. Drug interactions of NSAIDs § Anticoagulants such as coumarin, heparin or thrombolytic agents such as plasminogen activator, streptokinase or urokinase. § The fenamates and the salicylate congener diflunisal are less likely to cause this antithrombotic effect. § Indomethacin inhibits the hepatic glucuronidation and clearance of zidovudine. Also been implicated in the worsening of depression, parkinsonism and epilepsy and thus, should be avoided in such patients 45
- 46. § COX-2 § Enzyme induced by inflammatory cytokines § Induced during tissue injury § Results in Prostaglandins causing pain and inflammation § COX-2 Inhibitors e.g. Celecoxib (Celebrex), Etoricoxib (Arcoxia), Rofecoxib (Vioxx), Valdecoxib (Bextra) § No effect on platelet aggregation § Rofecoxib and valdecoxib taken off some markets due to their associated strokes and heart attacks. 46 Cox-2 selective inhibitors - coxibs
- 47. Celecoxib § Useful in the treatment of RA and osteoarthritis. § Appears to be free of COX-1 antagonistic properties. § Orally effective. § Complexes to some extent with food or co-administration of antacids. Highly protein bound. 60% of the drug is eliminated in the feces/ 30% in the urine. § Significantly less GI damage is claimed § Renal insufficiency, increase the risk of hypertension 47
- 48. Etoricoxib § Useful in the treatment of RA, gouty and osteoarthritis. § 106x more selective for COX-2. § Has less interference with cardioprotective COX-1-mediated antiplatelet activity of low-dose aspirin in vitro than celecoxib. § Significantly less GI damage § Renal insufficiency, increase the risk of hypertension 48
- 49. 49
- 50. 50
- 51. Chronic inflammation §DMARDs § Include conventional synthetic (csDMARDs), targeted synthetic (tsDMARDs) and biologics (bDMARDs) § Used in autoimmune and in some autoinflammatory diseases, such as RA, SLE, Muckle-Wells syndrome, FMF, IBD, to slow down disease progression. § They reduce evidence of disease progression § They are not typical anti-inflammatory agents § Include the following: § csDMARDs: methotrexate, hydroxychloroquine § bDMARDs: Abatacept, rituximab § tsDMARDs: tofacitinib, upadacitinib, baricitinib 51
- 52. Chronic inflammation §Include: §TNF alpha-induced apoptosis inhibitor: Sulphasalazine, hydroxychloroquine §5-LOX inhibitor: zileuton, Minocycline §Purine metabolism inhibitor: Methotrexate §Gold compounds: Auranofin §Janus Kinase (JAK) pathway inhibitors: Baricitinib, Tofacitinib §PDE4 inhibitors: effective in psoriatic arthritis with its mechanism not well defined. E.g., Apremilast 52
- 53. Chronic inflammation § Long term reaction associated with organ transplantation and autoimmunity. § IMMUNOSUPPRESSION § Calcineurin inhibitors § A calcium dependent serine-threonine phosphatase. In T cells normally bound to FKBP-12. § It acts to dephosphorylate Nuclear factor of activated T-cells (NF-AT), which translocates to the nucleus to regulate the expression of cytokines like IL-2. The constitutive phosphorylation of NF-AT prevents its passage into the nucleus § Cyclosporin – binds to cytosolic cyclophilin which as a complex inhibits calcineurin § Tacrolimus/FK506 – binds to FKBP12, which in turn inhibits calcineurin. § By reducing NF-AT transcriptional activity, reduces T-cell proliferation 53
- 54. § Others § Sirolimus/Rapamycin – blocks mammalian target of rapamycin (mTOR) signalling pathway – preventing maturation of APC and inflammatory cell proliferation § Azathioprine and Mycophenolate mofetil – inhibitors of cell proliferation § Transplantation – typical drug regimen would include calcineurin inhibitors, such as cyclosporin or tacrolimus; glucocorticoids, such as cortisol, dexamethasone; and inhibitors of T cell proliferation such as azathioprine or mycophenolate mofetil 54
- 55. Methotrexate §Pivotal DMARD in RA management §MTX affects cell survival by decreasing folate availability §Effective in early arthritis and has been shown to reduce the progression of erosion. §GI disorders common (ulcers, nausea, vomiting, etc.); Stomatitis §Rare but life-threatening haematological disorders §Pulmonary toxicity §Fetal death and congenital abnormalities common in pregnancy 55
- 56. Sulfasalazine §A combo of mesalazine or 5-ASA and sulfapyridine §Suppresses neutrophil activities such as chemotaxis, degranulation. §Inhibits PGE2 synthetase and extracellular release of PLA2 §Suppress activation of T, B and NK cells with decreased pro- inflammatory cytokines and immunoglobulin production. §GI disorders common §Reversible oligospermia and bone marrow toxicity 56
- 57. 57 Sulfasalazine
- 58. Antimalarials § The 4-aminoquinolones: chloroquine (CHQ) and HCQ are commonly used § Low incidence of adverse effect. § In SLE, considered as universal therapy § Play a role in lysosomal acidification leading to TLR inhibition § HCQ identified to prevent thrombosis (Annexin A5 activity). § Retinopathy, myopathy, tinnitus, cardiomyopathy and psychotic behavior § GI disorders § Skin pigmentation of oral mucosal membranes § Haemolysis in G6PD deficiency (rare) 58
- 59. Azathioprine §Used in IBD, SLE and RA §A prodrug of 6-MP, acts as antagonist of endogenous purines. §Suppresses activation of MAPK and NF-kB §GI disorders common §Neutropenia common in Thiopurine methyltransferase (TPMT) deficient individuals §Long term therapy increases risk of malignancies 59
- 60. Cyclosporin A § Preferred in refractory disease given the significant risk of toxicity on long term therapy § It impairs production of IL-2 and reduces lymphocyte proliferation >>> A calcineurin inhibitor § GI toxicity common § Hypertrichosis, gingival hyperplasia, hyperkalemia, hypermagnesemia, uricemia § HPT and renal dysfunction § Inhibitors of CYP3A4 such as CCB, macrolide antibiotics, azole antifungals increase the serum concentration in 2-5 folds 60
- 61. § Plasma IL-1 levels are increased in patients with active inflammation § Anakinra is an approved recombinant, non-glycosylated form of human IL-1RA for the management of joint disease in rheumatoid arthritis. § Others: Rilonacept, Canakinumab § Rilonacept is approved to treat the familial cold autoinflammatory syndrome (FCAS) and Muckle Wells syndrome, gout and recurrent pericarditis. § Canakinumab lowers recurrent MIs, decreased the incidence and deaths from lung cancer, and improved osteoarthritis pain 61 IL-1 receptor inhibitors
- 62. § Tocilizumab, an IL-6R antagonist, is approved for treatment of rheumatoid arthritis and systemic juvenile idiopathic arthritis § Siltuximab, another IL-6R antagonist, is approved for treatment of multicentric Castleman disease if the patient is HIV positive § Ustekinumab is a human IL-12R and IL-23R antagonist indicated for the treatment of plaque psoriasis and psoriatic arthritis. URTI is common side effect § Secukinumab is a bDMARD anti-IL-17A antagonist indicated for treatment of plaque psoriasis. It may exacerbate IBD 62 Other IL receptor inhibitors
- 63. §Inhibitor of PDE4, hindering cAMP to AMP conversion §Increased intracellular cAMP and decreased production of proinflammatory cytokines including IL-2, -8, -12, -23. §Elimination is 58% by the kidneys and 39% by the faeces §It is indicated for plaque psoriasis, psoriatic arthritis, and oral ulcers associated with Behçet disease §Principal adverse effects are gastrointestinal (diarrhoea, nausea), but upper abdominal pain, vomiting, upper respiratory tract infections, arthralgia, weight loss, headaches, mood disorders, and suicidal ideation are reported rarely 63 Apremilast
- 64. §Anti-inflammatory, target synthetic small molecule (tsDMARD) that in vitro, selectively, and reversibly inhibits the JAK/STAT signalling pathway §It is excreted mainly by the kidneys, so it should be used cautiously if at all in patients whose glomerular filtration rate is <60 mL/min/1.73 §It can be used as monotherapy or in combination with methotrexate or other csDMARDs §It increases the risk of infection and of herpes virus reactivation. §Common side effects include Neutropenia, lymphopenia, anaemia, liver enzyme elevation, and lipid elevation 64 Baricitinib
- 65. §It binds TNF and molecules and also inhibits lymphotoxin. §It is approved for the treatment of RA, juvenile chronic arthritis, psoriasis §Decreases the rate of formation of new erosions relative to methotrexate alone. §Adverse effects include viral, bacterial, or fungal infections, as well as injection site reactions. §Rare toxicities include GI problems, skin rashes, lupus-like syndrome, pancytopenia, and lymphoma 65 Etanercept
- 66. § E. coli–derived chimeric (25% mouse, 75% human) IgG monoclonal antibody that binds and inhibits membrane bound TNF. Its mechanism of action is probably the same as that of adalimumab. § Infliximab treats RA, Crohn disease, ulcerative colitis, paediatric inflammatory bowel disease, and psoriasis. § In RA, infliximab plus methotrexate decreases the rate of formation of new erosions. § It increases the risk of bacterial infection and HBV reactivation § TNFα–blocking agents increase the risk for lymphoma and skin cancers, including melanoma, which necessitates periodic skin examination, especially in high risk patients 66 Infliximab
- 67. Other DMARDS § Intramuscular gold therapy: improve swollen joint count, pain and disability. Early use retards joint erosion. Used less due to risk of cytopenia and proteinuria. § D-penicillamine: withdrawn due to no advantage over placebo in RA coupled with adverse side effects. § Minocycline: inhibits matrix metalloproteinases and decreases synovial T cell proliferation and cytokine production. Side effects include vertigo and liver toxicity and drug-induced SLE. Also known to inhibit 5- LOX. 67
- 68. §Gout is a metabolic disease characterized by recurrent episodes of acute arthritis due to deposits of monosodium urate in joints and cartilage. §Monosodium urate crystals activate monocytes/macrophages via the TLR pathway mounting an innate immune response. §This results in the activation of the cryopyrin inflammasome, the secretion of cytokines (e.g., IL-1β and TNF-α), endothelial activation, and attraction of neutrophils to the site of inflammation. §The treatment of gout aims to relieve acute gouty attacks and prevent recurrent gouty episodes and urate lithiasis. 68
- 69. §Gout treatment aims at: §Relieving inflammation and pain (NSAIDs, colchicine, glucocorticoids) §Preventing inflammatory responses to crystals (colchicine and NSAIDs) §Inhibiting of urate formation (e.g., allopurinol, febuxostat) §Augmenting urate excretion (probenecid) 69
- 70. §Colchicine §It is used in management and prevention of acute gout. §It has antimitotic activity by arresting cell division in G1 in cells with rapid turnover (e.g., neutrophils) §It reduces neutrophil recruitment and adhesion to inflamed tissues. §It inhibits inflammasome activation and IL-1β and IL-18 formation – this explains its benefits in FMF. § The exact metabolism of colchicine in humans is unknown, but in vitro studies indicated that it may undergo oxidative demethylation by CYP3A4; glucuronidation may also be involved 70
- 71. §Allopurinol §Allopurinol inhibits XO and prevents the synthesis of urate from hypoxanthine and xanthine. §It is used to treat hyperuricemia in patients with gout and to prevent it in those with haematological malignancies about to undergo chemotherapy §It is absorbed relatively rapidly after oral ingestion, and peak plasma concentrations are reached within 60–90 min. About 20% is excreted in the faeces in 48–72 h. §Colchicine use must precede the use of allopurinol §It must be avoided in acute gouty attacks 71
- 72. §Febuxostat §Allopurinol inhibits XO and prevents the synthesis of urate from hypoxanthine and xanthine. §It is rapidly absorbed with maximum plasma concentration at 1- 1.5 h. Food, Al( OH)3 and Mg(OH)2 affect its GI absorption. Uricosuric agent §Probenecid inhibits the reabsorption of uric acid by OATs, principally URAT-1 §The uricosuric action of probenecid is blunted by the coadministration of salicylates 72
- 73. §Uricase §Pegloticase (pegylated uricase) catalyses the oxidation of uric acid into allantoin, a soluble, inactive metabolite. §It is used in severe, refractory, chronic gout. §Its effectiveness reduces with production of antibodies against it. §Anaphylactic rxn and haemolysis in G6PD-deficient patients is reported. §Rasburicase is a recombinant uricase which is more effective than allopurinol. §Used to lower urate in individuals with leukaemia, lymphoma, and solid tumour malignancies who are receiving anticancer therapy expected to result in tumour lysis and significant hyperuricemia. 73











![Non-steroidal anti-inflammatory agents
[NSAIDs]
§Aspirin and other Salicylates
§Non-selective COX Inhibitors
§propionic acids e.g., ibuprofen, ketoprofen, naproxen
§oxicam derivatives e.g., piroxicam,
§indole derivatives e.g., indomethacin, sulindac, etodolac
§Selective COX-2 Inhibitors
12](https://image.slidesharecdn.com/bbec55b34400a7914c42429908233dbd381773-250805180406-650ead9b/85/bbec55_b34400a7914c42429908233dbd381773-pdf-12-320.jpg)



![Mechanism of NSAID action
[eicosanoid synthesis inhibition]
§Eicosanoids include
§Prostaglandins, Thromboxanes and Leukotrienes
§Cells subjected to trauma increase production of
Prostaglandins
§Synthesis of Prostaglandins and Thromboxanes are
catalyzed by the enzyme Cyclooxygenase
16](https://image.slidesharecdn.com/bbec55b34400a7914c42429908233dbd381773-250805180406-650ead9b/85/bbec55_b34400a7914c42429908233dbd381773-pdf-16-320.jpg)