Critical care revision notes
- 1. CRITICAL CARE REVISION NOTES DR.SHERIF BADRAWY
- 2. اﻟﺮﺣﻴﻢ اﻟﺮﺣﻤﻦ ﷲ ﺑﺴﻢ ◨ This is a summary of Benington's MCQ book targeting EDIC exam ◨ This book is mainly for part 1 EDIC, with MCQs type A & K. ◨ Hope U'll find it useful 1a
- 3. 1b
- 4. The maximum rate of potassium infusion should not exceed 2a Critical Care revision notes Dr.Sherif Badrawy Digitally signed by Dr.Sherif Badrawy Date: 2015.12.18 22:58:29 +03'00'
- 5. 【40mmol/h】 as this may cause arrhythmias and asystole. 2b Critical Care revision notes Dr.Sherif Badrawy
- 6. Normal sodium requirement is 3a Critical Care revision notes Dr.Sherif Badrawy
- 7. 1-2mmol/day. 3b Critical Care revision notes Dr.Sherif Badrawy
- 8. Extracellular calcium exists in three forms: 4a Critical Care revision notes Dr.Sherif Badrawy
- 9. 40% protein bound (largely to albumin), 47% free ionised, and 13% complexed with citrate, phosphate and sulphate. 4b Critical Care revision notes Dr.Sherif Badrawy
- 10. the physiologically important form of calcium 5a Critical Care revision notes Dr.Sherif Badrawy
- 11. 【The ionised form】 as it may be reduced by alkalosis through greater protein binding 5b Critical Care revision notes Dr.Sherif Badrawy
- 12. 1g of magnesium sulphate contains 6a Critical Care revision notes Dr.Sherif Badrawy
- 13. 4mmol magnesium 6b Critical Care revision notes Dr.Sherif Badrawy
- 14. The normal range for phosphate in the plasma is 7a Critical Care revision notes Dr.Sherif Badrawy
- 15. 0.8-1.5mmol/L 7b Critical Care revision notes Dr.Sherif Badrawy
- 16. Normal QT interval is 8a Critical Care revision notes Dr.Sherif Badrawy
- 17. 0.38-0.46s (9-11 small squares) 8b Critical Care revision notes Dr.Sherif Badrawy
- 18. corrected QT interval (QTc) Bazett's formula, 9a Critical Care revision notes Dr.Sherif Badrawy
- 19. QTc = QT/√R-R, adjusting for heart rate. 9b Critical Care revision notes Dr.Sherif Badrawy
- 20. How Mains isolating transformer reduce the risk of electrical injury in the ICU 10a Critical Care revision notes Dr.Sherif Badrawy
- 21. 【isolates the power supply from earth】 If a patient comes into contact with faulty equipment the current cannot flow through the patient to earth. 10b Critical Care revision notes Dr.Sherif Badrawy
- 22. How An 【earth leakage circuit breaker】 reduce the risk of electrical injury in the ICU 11a Critical Care revision notes Dr.Sherif Badrawy
- 23. 【switches off the electrical supply】 if stray currents are detected flowing to earth, reducing the potential for microshock. 11b Critical Care revision notes Dr.Sherif Badrawy
- 24. Other methods to reduce the risk of electrical injury in the ICU 12a Critical Care revision notes Dr.Sherif Badrawy
- 25. Use of a common earth & Use of Class II equipment.(double insulation) 12b Critical Care revision notes Dr.Sherif Badrawy
- 26. inefficient methods of cooling 13a Critical Care revision notes Dr.Sherif Badrawy
- 27. cold air blankets, bladder irrigation and gastric lavage all 13b Critical Care revision notes Dr.Sherif Badrawy
- 28. efficient methods of cooling 14a Critical Care revision notes Dr.Sherif Badrawy
- 29. ♧ Ice water bodily immersion. ♧ Extracorporeal heat exchange. ♧ Rapid infusion of 30ml/kg bolus of crystalloid at 4°C. ♧ Central venous cooling catheter 14b Critical Care revision notes Dr.Sherif Badrawy
- 30. presence of sternal fracture suspect ? + no response to fluid resuscitation 15a Critical Care revision notes Dr.Sherif Badrawy
- 31. cardiac tamponade 15b Critical Care revision notes Dr.Sherif Badrawy
- 32. Beck's triad 16a Critical Care revision notes Dr.Sherif Badrawy
- 33. ↑JVP, muffled heart sounds and hypotension 16b Critical Care revision notes Dr.Sherif Badrawy
- 34. Why A widened cardiac shadow is not a sensitive sign for acute traumatic tamponade ? 17a Critical Care revision notes Dr.Sherif Badrawy
- 35. dt only small volumes of blood (<500ml) in the pericardial space are required to cause HD compromise. 17b Critical Care revision notes Dr.Sherif Badrawy
- 36. Human albumin 4% will be more effective than crystalloid for fluid resuscitation ? 18a Critical Care revision notes Dr.Sherif Badrawy
- 37. NO 18b Critical Care revision notes Dr.Sherif Badrawy
- 38. adverse prognostic factors in severe TBI ? According to CRASH (Corticosteroid Randomisation After Significant Head Injury) trial 19a Critical Care revision notes Dr.Sherif Badrawy
- 39. ♧ risk of death also increases linearly with every point decrease in GCS. ♧ Age > 40 ♧ Dilated pupils ♧ CT pathology including petechial hges, subarachnoid blood, midline shift and obliteration of the basal cisterns ♧ Patient sex is not useful as a prognostic indicator 19b Critical Care revision notes Dr.Sherif Badrawy
- 40. Tuberculous meningitis is common in 20a Critical Care revision notes Dr.Sherif Badrawy
- 41. immigrants, the homeless, alcoholics and, increasingly, in HIV positive patients 20b Critical Care revision notes Dr.Sherif Badrawy
- 42. CSF in Tuberculous meningitis 21a Critical Care revision notes Dr.Sherif Badrawy
- 43. low glucose, moderately elevated protein, and classically a lymphocytic pleocytosis (although a CSF neutrophilia is common in the early stages, and an acellular picture may be found in HIV-related cases). 21b Critical Care revision notes Dr.Sherif Badrawy
- 44. A positive India ink stain of CSF suggests 22a Critical Care revision notes Dr.Sherif Badrawy
- 45. cryptococcus, although a negative stain does not rule this out. 22b Critical Care revision notes Dr.Sherif Badrawy
- 46. meningitis not associated with low glucose ? 23a Critical Care revision notes Dr.Sherif Badrawy
- 47. viral meningitis 23b Critical Care revision notes Dr.Sherif Badrawy
- 48. In RV infarction RA pressure is 24a Critical Care revision notes Dr.Sherif Badrawy
- 49. usually 【elevated & > 10mmHg】.R to L shunting can occur at the atrial level through a patent foramen ovale in the presence of elevated right atrial pressure 24b Critical Care revision notes Dr.Sherif Badrawy
- 50. Right ventricular infarction rarely occurs in isolation and is usually accompanied by 25a Critical Care revision notes Dr.Sherif Badrawy
- 51. inferior infarction 25b Critical Care revision notes Dr.Sherif Badrawy
- 52. The flow of crystalloid through a 16G intravenous cannula is approximately 26a Critical Care revision notes Dr.Sherif Badrawy
- 53. 150ml/min 26b Critical Care revision notes Dr.Sherif Badrawy
- 54. flow is proportional to 27a Critical Care revision notes Dr.Sherif Badrawy
- 55. ♧ the fourth power of the radius [NOT to the square of the radius] ♧ & inversely proportional to the viscosity of the fluid and the length of the tube 27b Critical Care revision notes Dr.Sherif Badrawy
- 56. Intraosseous access is contraindicated in adult patients ? 28a Critical Care revision notes Dr.Sherif Badrawy
- 57. NO, Used if intravenous access is not possible, though the tougher bony cortex makes this difficult [tibia, sternum and iliac crest] 28b Critical Care revision notes Dr.Sherif Badrawy
- 58. Lund concept for the management of traumatic brain injury 29a Critical Care revision notes Dr.Sherif Badrawy
- 59. focuses on the importance of【Starling's forces in the development of brain oedema】 in the presence of disordered cerebral autoregulation following traumatic brain injury 29b Critical Care revision notes Dr.Sherif Badrawy
- 60. Components of Lund concept for the management of traumatic brain injury 30a Critical Care revision notes Dr.Sherif Badrawy
- 61. ✾ BP limited to pre-injury normal levels (to prevent ↑pre-capillary pressure in the presence of impaired arteriolar autoregulation) using 【metoprolol and clonidine】. ✾ 【Albumin】 is transfused to maintain plasma colloid oncotic pressure. ✾ 【Thiopentone】is used to promote arteriolar VC (2ry to flow- metabolism coupling), ✾ 【dihydroergotamine】is used to ↑venoconstriction and ↓cerebral blood volume. ✾ A minimum【 CPP of 50mmHg】 is accepted to ↓inotropes and vasopressors which might ↑cerebral oedema by ↑cerebral blood volume (no mannitol is used). 30b Critical Care revision notes Dr.Sherif Badrawy
- 62. prerequisites for the use of recombinant factor VIIa in bleeding trauma 31a Critical Care revision notes Dr.Sherif Badrawy
- 63. ✾ 【Platelet count > 50】 ➜ generate the 'thrombin burst' which the rFVIIa provokes ✾ 【Fibrinogen >0.5 g/L 】➜ translate this thrombin generation into clot formation ✾ 【temperature > 32°C】 ✾【pH >7.20.】 ✾ 【Ionised Ca2+ >0.8mmol/L】 31b Critical Care revision notes Dr.Sherif Badrawy
- 64. Mechanism of Tranexamic acid action ? 32a Critical Care revision notes Dr.Sherif Badrawy
- 65. a competitive inhibitor of plasminogen and plasmin. 32b Critical Care revision notes Dr.Sherif Badrawy
- 66. significantly reduces blood loss and transfusion requirements in cardiac surgery ? 33a Critical Care revision notes Dr.Sherif Badrawy
- 67. ✾ 【Aprotinin】 ➜ forms irreversible complexes with a variety of proteases including plasmin ✾ isolated from bovine lungs and has a high incidence of anaphylaxis (0.5%) ✾ ±associated with an increased incidence of myocardial infarction, stroke and renal failure 33b Critical Care revision notes Dr.Sherif Badrawy
- 68. Inhalational injury, when Pharyngeal oedema is likely to increase ? 34a Critical Care revision notes Dr.Sherif Badrawy
- 69. ✾ 【once fluid resuscitation is commenced】, and early intubation is advised. ✾ Lung function is likely to worsen over the next 12 hours. 34b Critical Care revision notes Dr.Sherif Badrawy
- 70. Common sites of thermal injury in the Airway during burn ? 35a Critical Care revision notes Dr.Sherif Badrawy
- 71. Most of the heat from hot gas inhalation is dissipated in the 【upper airways】, so thermal injury below the glottis is unusual. 35b Critical Care revision notes Dr.Sherif Badrawy
- 72. Lavage with sodium bicarbonate 1.4% to the bronchial tree has a role in the management of thermal injury patient ? 36a Critical Care revision notes Dr.Sherif Badrawy
- 73. may be performed 【following intubation to neutralise acidic deposits】 and remove soot contamination, although evidence for the effectiveness of this therapy is lacking. 36b Critical Care revision notes Dr.Sherif Badrawy
- 74. A cherry red visage has several causes other than carbon monoxide poisoning ? 37a Critical Care revision notes Dr.Sherif Badrawy
- 75. alcohol, emotion and heat 37b Critical Care revision notes Dr.Sherif Badrawy
- 76. Risk factors for antimicrobial-resistant infection 38a Critical Care revision notes Dr.Sherif Badrawy
- 77. ✾ Prolonged hospital admission, Prolonged MV ✾ indwelling devices ✾ poor hand hygiene ✾ High nursing workload. ✾ Understaffing in the ICU. 38b Critical Care revision notes Dr.Sherif Badrawy
- 78. BP of 75/50mmHg and a HR of 125bpm, PAP 15/7mmHg, CVP 3mmHg, PAOP 5mmHg, cardiac index 1.6L/min/m2, SVR 2750 dyne/sec/cm5. The MOST LIKELY diagnosis 39a Critical Care revision notes Dr.Sherif Badrawy
- 79. Hypovolaemia. 39b Critical Care revision notes Dr.Sherif Badrawy
- 80. BEST guide to the need for further intravenous fluid replacement? ✾ Response of oesophageal Doppler to passive leg raising. ✾ PA catheter ✾ Titrate fluid resuscitation against repeated blood lactate ✾ pulse pressure variation ✾ UOP 40a Critical Care revision notes Dr.Sherif Badrawy
- 81. ✾ 【Response of oesophageal Doppler to passive leg raising.】 ❅ Passive leg raising autotransfuses about 300ml of blood into the central circulation. If stroke volume ↑significantly 【>10% by oesophageal Doppler】 , indicates preload-responsiveness. it is reversible if no improvement is seen 40b Critical Care revision notes Dr.Sherif Badrawy
- 82. PAOP as a guide to the need for further intravenous fluid replacement? 41a Critical Care revision notes Dr.Sherif Badrawy
- 83. ✸ PAOP is a poor predictor of whether a fluid bolus will ↑COP 41b Critical Care revision notes Dr.Sherif Badrawy
- 84. Blood lactate & UOP as a guide to the need for further intravenous fluid replacement? 42a Critical Care revision notes Dr.Sherif Badrawy
- 85. ✸ Blood lactate & UOP will not DD bw cardiogenic shock and septic shock 42b Critical Care revision notes Dr.Sherif Badrawy
- 86. Pulse pressure variation as a guide to the need for further intravenous fluid replacement? 43a Critical Care revision notes Dr.Sherif Badrawy
- 87. ✸ 【Pulse pressure variation of >13%】 accurately predict response to fluid, but is【only reliable in MV patients without spontaneous respiratory effort】. 43b Critical Care revision notes Dr.Sherif Badrawy
- 88. sources of error in pulse oximetry 44a Critical Care revision notes Dr.Sherif Badrawy
- 89. ✸ Use of 【local anaesthetic may cause a fall in SpO2】 ✸ Jaundice, foetal haemoglobin and dark skin do not affect the signal ✸ 【Severe tricuspid regurgitation】 reduces the SpO2 reading ✸ Readings are 【unreliable below 70% SpO2】 ✸ any reading below 90% indicates serious hypoxaemia due to the steep fall in the oxygen dissociation curve at this point. 44b Critical Care revision notes Dr.Sherif Badrawy
- 90. most useful indicator when considering a diagnosis of massive pulmonary embolism? 45a Critical Care revision notes Dr.Sherif Badrawy
- 91. ✸ 【A fall in end-tidal CO2 to 1.3kPa】. dt degree of V/Q mismatch ✸ S1Q3T3 us infrequently seen in and is therefore insensitive 45b Critical Care revision notes Dr.Sherif Badrawy
- 92. Normal Capnograph VS Bronchospasm Capnograph 46a Critical Care revision notes Dr.Sherif Badrawy
- 93. 46b Critical Care revision notes Dr.Sherif Badrawy
- 94. daily interruption of sedation 47a Critical Care revision notes Dr.Sherif Badrawy
- 95. ✸ 【↓Length of ICU stay】 ✸【↓ period of MV】 ✸ 【↓CT brain scans are required】 ✸ In-hospital 【mortality is unaffected】 ✸ drug-sparing effect was greater with midazolam. 47b Critical Care revision notes Dr.Sherif Badrawy
- 96. serotonin syndrome CP ? 48a Critical Care revision notes Dr.Sherif Badrawy
- 97. ✸ mental status 【hallucinations, restlessness, confusion, coma】 ✸ neuromuscular 【clonus, myoclonus, ataxia, hyper-reflexia】 ✸ autonomic 【hyperthermia, tachycardia, swings in BP】 48b Critical Care revision notes Dr.Sherif Badrawy
- 98. serotonin syndrome precipitated by 49a Critical Care revision notes Dr.Sherif Badrawy
- 99. 【MAOI, TCA】, lithium, valproate, fentanyl, ondansetron and sympathomimetic drugs of abuse 49b Critical Care revision notes Dr.Sherif Badrawy
- 100. Cyproheptadine MOA ? 50a Critical Care revision notes Dr.Sherif Badrawy
- 101. a 【serotonin antagonist】 which has been used in the treatment of the serotonin syndrome 50b Critical Care revision notes Dr.Sherif Badrawy
- 102. Etiology of serotonin syndrome 51a Critical Care revision notes Dr.Sherif Badrawy
- 103. a 【dose-related】 phenomenon, unlike the neuroleptic malignant syndrome. The latter is an idiosyncratic drug reaction to dopamine antagonists 51b Critical Care revision notes Dr.Sherif Badrawy
- 104. DD in onset bw serotonin syndrome & neuroleptic malignant syndrome 52a Critical Care revision notes Dr.Sherif Badrawy
- 105. ✸ onset of the neuroleptic malignant syndrome is usually gradual over a period of several days. 【 ﻧﻤﺲ NMS = gradual】 ✸ Onset of serotonin syndrome is rapid over a period of hours 52b Critical Care revision notes Dr.Sherif Badrawy
- 106. neuroleptic malignant syndrome CP ? 53a Critical Care revision notes Dr.Sherif Badrawy
- 107. ✸ extrapyramidal 【lead pipe rigidity, bradykinesia】 ✸ autonomic 【hyperthermia, tachycardia, swings in BP】 ✸ fluctuating consciousness 53b Critical Care revision notes Dr.Sherif Badrawy
- 108. most strongly predictive of outcome in acute pancreatitis? 54a Critical Care revision notes Dr.Sherif Badrawy
- 109. White cell count. 【NOT amylase or lipase or CRP】 54b Critical Care revision notes Dr.Sherif Badrawy
- 110. Non-invasive ventilation in pts with idiopathic pulmonary fibrosis (IPF) ? 55a Critical Care revision notes Dr.Sherif Badrawy
- 111. NIV is 【ineffective in preventing the need for ETT & MV】 (in contrast to pts with obstructive lung disease) 55b Critical Care revision notes Dr.Sherif Badrawy
- 112. commonest cause of worsening respiratory failure in patients with IPF ? 56a Critical Care revision notes Dr.Sherif Badrawy
- 113. progression of the disease process (47%), followed by pneumonia (31%) 56b Critical Care revision notes Dr.Sherif Badrawy
- 114. NOT an propriate treatment for acute severe asthma ? 57a Critical Care revision notes Dr.Sherif Badrawy
- 115. Heliox.【NOT Intravenous aminophylline】 ✸ Heliox did not alter outcome and could not be recommended in the emergency Rx of acute severe asthma ✸ Heliox is not recommended in the latest British Thoracic Society guidelines 57b Critical Care revision notes Dr.Sherif Badrawy
- 116. 76-y F, Hx of AF, SOB, bibasal crackles, 80/50, SpO2 of 87% on 15L/min oxygen NRBM, ECG AF ventricular rate of 170bpm.takes warfarin, her INR is 1.3 , Action ? 58a Critical Care revision notes Dr.Sherif Badrawy
- 117. ✸【 synchronised DC shock】 Although there is a risk of embolisation when cardioverting a patient with longstanding (AF) who is not anticoagulated (6.8%), this is outweighed by the need for urgent heart rate control. 58b Critical Care revision notes Dr.Sherif Badrawy
- 118. FEV1 as a predictor of ICU survival in patients with IPF ? 59a Critical Care revision notes Dr.Sherif Badrawy
- 119. FEV1 is not a useful predictor of ICU survival in patients with IPF 59b Critical Care revision notes Dr.Sherif Badrawy
- 120. (IABP) for cardiac failure 60a Critical Care revision notes Dr.Sherif Badrawy
- 121. ❤ inserted via the 【femoral artery or subclavian artery】 ❤ The balloon【inflates immediately following the dicrotic notch】on the arterial waveform. ❤ The balloon 【deflates during isovolumetric contraction】 of the LV. ❤ The augmentation pressure is the peak pressure during IABP inflation in diastole. ❤ 【SBP usu ➜↓during IABP use】. 60b Critical Care revision notes Dr.Sherif Badrawy
- 122. IHD vs CRRT vs SLED1 61a Critical Care revision notes Dr.Sherif Badrawy
- 123. 61b Critical Care revision notes Dr.Sherif Badrawy
- 124. IHD vs CRRT vs SLED2 62a Critical Care revision notes Dr.Sherif Badrawy
- 125. 62b Critical Care revision notes Dr.Sherif Badrawy
- 126. Which is more efficient at removing urea IHD vs CRRT 63a Critical Care revision notes Dr.Sherif Badrawy
- 127. 【IHD is much more efficient at removing urea】 (clearance 198ml/min) than CVVHDF (30ml/min) and, So, requires a much < time frame, and < labour-intensive for the ICU staff. Mortality is similar in ICU pts Rx with IHD or CRRT. IHD can be used successfully in HD unstable pts. CRRT is > labour-intensive for the ICU staff. 63b Critical Care revision notes Dr.Sherif Badrawy
- 128. Electrolyte disturbances in rhabdomyolysis ? 64a Critical Care revision notes Dr.Sherif Badrawy
- 129. ✬ Hyperkalaemia. ✬ mild hypocalcaemia ✬ Hyperphosphataemia. ✬ Elevated serum creatinine. ✬ Hyperuricaemia. 64b Critical Care revision notes Dr.Sherif Badrawy
- 130. Etiology of mild hypocalcaemia in rhabdomyolysis ? 65a Critical Care revision notes Dr.Sherif Badrawy
- 131. ✬ seen early in the course of rhabdomyolysis ➜ 【Phosphate binds with calcium in the extracellular fluid】 ➜ may precipitate in the tissues ✬ in the recovery phase ➜ calcium is mobilised from the tissues to the extracellular space ➜ avoided calcium supplementation unless ionised levels are dangerously↓ 65b Critical Care revision notes Dr.Sherif Badrawy
- 132. paracetamol toxicity N-acetylcysteine 66a Critical Care revision notes Dr.Sherif Badrawy
- 133. ✬ Serious liver damage is unlikely if N- acetylcysteine is given within 12hours of ingestion ✬ NAC may be continued indefinitely at 150mg/kg/day in cases of acute liver failure until improvement occurs or a transplant is obtained 66b Critical Care revision notes Dr.Sherif Badrawy
- 134. the most sensitive prognostic marker in paracetamol toxicity 67a Critical Care revision notes Dr.Sherif Badrawy
- 135. raised prothrombin time 67b Critical Care revision notes Dr.Sherif Badrawy
- 136. silhouette sign in CXR 68a Critical Care revision notes Dr.Sherif Badrawy
- 137. the absence of the normally well-defined interface between lung and soft tissue structures. If the air in the lung at the interface is removed e.g.【consolidation】, the radiographic boundary will disappear. 68b Critical Care revision notes Dr.Sherif Badrawy
- 138. Pleural capping sign in CXR 69a Critical Care revision notes Dr.Sherif Badrawy
- 139. obliteration of the medial aspect of the left upper lobe seen in some cases of aortic dissection 69b Critical Care revision notes Dr.Sherif Badrawy
- 140. Bat's wing sign in CXR 70a Critical Care revision notes Dr.Sherif Badrawy
- 141. shadowing is perihilar oedema of the lung fields adjacent to the heart seen in congestive cardiac failure. 70b Critical Care revision notes Dr.Sherif Badrawy
- 142. Air bronchograms sign in CXR 71a Critical Care revision notes Dr.Sherif Badrawy
- 143. (radiolucent) intrapulmonary airways made visible by their passage through a zone of (radio-opaque) consolidation. 71b Critical Care revision notes Dr.Sherif Badrawy
- 144. Wedge-shaped shadows sign in CXR 72a Critical Care revision notes Dr.Sherif Badrawy
- 145. may represent an area of infarcted lung in pulmonary embolism 72b Critical Care revision notes Dr.Sherif Badrawy
- 146. Cocaine effects on anticoagulation ? 73a Critical Care revision notes Dr.Sherif Badrawy
- 147. a hypercoagulable state by decreasing protein C and antithrombin III levels, and increases platelet activation. 73b Critical Care revision notes Dr.Sherif Badrawy
- 148. 'crack lung' with Cocaine abuse ? 74a Critical Care revision notes Dr.Sherif Badrawy
- 149. Cocaine has immunogenic properties act as a hapten triggers a 【hypersensitivity pneumonitis】 when combined with albumin or globulins characterised by fever, dyspnoea, wheezing and diffuse interstitial infiltrates 74b Critical Care revision notes Dr.Sherif Badrawy
- 150. commonest gastrointestinal complication of cocaine 75a Critical Care revision notes Dr.Sherif Badrawy
- 151. ✺ 【Bowel ischaemia】 dt vasospasm of the mesenteric circulation ✺ Gastroduodenal perforation can also occur 75b Critical Care revision notes Dr.Sherif Badrawy
- 152. Phencyclidine (PCP) 76a Critical Care revision notes Dr.Sherif Badrawy
- 153. ✺ a recreational drug of abuse ✺ a weak base ✺ highly lipid-soluble and 78% protein-bound ➜ HD is ineffective. ✺ cholinergic, anticholinergic, sympathomimetic, dopaminergic, narcotic and serotonergic effects ✺ Hypertension agitation with pinpoint pupils 76b Critical Care revision notes Dr.Sherif Badrawy
- 154. physiology of pregnancy 77a Critical Care revision notes Dr.Sherif Badrawy
- 155. ✺ SVR normally falls in early pregnancy. ✺ The RAS is up-regulated. ✺ SBP decreases to a lesser extent than diastolic. ✺ Hypertension detected in the first trimester is likely to be longstanding. 77b Critical Care revision notes Dr.Sherif Badrawy
- 156. Pre-eclampsia is a predictor of difficult laryngoscopy 78a Critical Care revision notes Dr.Sherif Badrawy
- 157. 【potentially difficult airway of pregnancy is accentuated】, with facial and tongue oedema making direct laryngoscopy difficult. 78b Critical Care revision notes Dr.Sherif Badrawy
- 158. dobutamine effects 79a Critical Care revision notes Dr.Sherif Badrawy
- 159. ✺ LVEDP is reduced. ✺ half-life of 2 minutes ✺ SVR is reduced. ✺ Cardiac index is increased 79b Critical Care revision notes Dr.Sherif Badrawy
- 160. Remifentanil is metabolised by 80a Critical Care revision notes Dr.Sherif Badrawy
- 161. 【non-specific plasma esterases】and can be used as normal if hepatic metabolism is impaired 80b Critical Care revision notes Dr.Sherif Badrawy
- 162. DD bw Drugs with a low extraction ratio & Drugs with a flow-limited in hepatic metabolism in shock state 81a Critical Care revision notes Dr.Sherif Badrawy
- 163. Drugs with a low extraction ratio are【metabolism-limited 】(they depend on saturable enzyme systems for metabolism) rather than flow-limited, and will not be affected by reduced liver blood flow, unless the reduction is so severe as to cause hepatocellular injury and reduced enzyme function. 81b Critical Care revision notes Dr.Sherif Badrawy
- 164. The Venturi effect (based on the Bernoulli principle) 82a Critical Care revision notes Dr.Sherif Badrawy
- 165. 【when a gas passes through a constriction the pressure falls, allowing a second gas to be entrained】. The Venturi mask has a constriction through which oxygen flows, entraining a fixed ratio of air dependent on the size of the constriction and the flow of oxygen. This allows a high volume of gas of a known FiO2 to be available for inspiration (fixed performance). 82b Critical Care revision notes Dr.Sherif Badrawy
- 166. oxygen administration 83a Critical Care revision notes Dr.Sherif Badrawy
- 167. ✺ Maximum inspiratory flow may exceed 30L/min during spontaneous breathing. ✺ Nasal cannulae significantly improve oxygenation even if the patient breathes through the mouth. ✺ A Venturi mask uses the Bernoulli principle. ✺ An anaesthetic face mask increases dead space. 83b Critical Care revision notes Dr.Sherif Badrawy
- 168. Clostridium difficile is a ? 84a Critical Care revision notes Dr.Sherif Badrawy
- 169. ✺ a spore-forming gram-positive anaerobic bacillus ✺ transmitted from patient to patient, usually via the hands of hospital personnel ✺ 40% of hospitalized patients can harbor C. difficile in their stool, most are asymptomatic 84b Critical Care revision notes Dr.Sherif Badrawy
- 170. Oral vancomycin is the treatment of choice for Clostridium difficile infection if ? 85a Critical Care revision notes Dr.Sherif Badrawy
- 171. High risk pts for serious complications such as toxic megacolon, perforation and death in case of recurrence. ✯ ↓GCS ✯ HD instability, dehydration ✯ age > 65 ✯ WBCs >20 ✯ creatinine >200 ✯ Confluent pseudomembranes, megacolon 85b Critical Care revision notes Dr.Sherif Badrawy
- 172. Dx of Clostridium difficile infection ? 86a Critical Care revision notes Dr.Sherif Badrawy
- 173. ✯ 【PCR】 ✯ Enzyme immunoassay (EIA) for C. difficile 【glutamate dehydrogenase】(GDH) ✯ (EIA) for C. difficile【 toxins A and B】 ✯ Cell culture cytotoxicity assay ✯ Selective anaerobic culture ✯ Colonoscopy or sigmoidoscopy and【biopsy】 86b Critical Care revision notes Dr.Sherif Badrawy
- 174. Which form of vancomycin is used in Rx of Clostridium difficile infection ? 87a Critical Care revision notes Dr.Sherif Badrawy
- 175. ❏ Oral vancomycin as resistance is rare and it reaches high concentrations in the colon. ❏ IV vancomycin is ineffective since it has poor penetration of the colon ❏ IV metronidazole is effective, however, and may be useful if an ileus preventing the enteral administration of drugs is present 87b Critical Care revision notes Dr.Sherif Badrawy
- 176. first-line therapy for uncomplicated C. difficile infection ? 88a Critical Care revision notes Dr.Sherif Badrawy
- 177. ✺ oral metronidazole ✺ effective and cheap but associated with a significant relapse rate of up to 25% in the first 10 days following cessation of therapy. 88b Critical Care revision notes Dr.Sherif Badrawy
- 178. Rule of Nasojejunal faecal replacement in Rx of Clostridium difficile infection ? 89a Critical Care revision notes Dr.Sherif Badrawy
- 179. Usen in Rx of chronic C. difficile infection, 【where it re-colonises the patient's colon with normal flora】. It has【 no place in the management of acute infection】. 89b Critical Care revision notes Dr.Sherif Badrawy
- 180. commonest adverse incident in the ICU? 90a Critical Care revision notes Dr.Sherif Badrawy
- 181. Line, drain and catheter dislodgement then Medication errors then Equipment failure. 90b Critical Care revision notes Dr.Sherif Badrawy
- 182. Flow-volume loop for Tracheomalacia 91a Critical Care revision notes Dr.Sherif Badrawy
- 183. ✯ characteristic pattern of variable intrathoracic obstruction【normal inspiratory limb and a flattened expiratory limb】. ✯ trachea to【collapse during expiration but remain patent during inspiration】. ✯ ischaemic injury to the trachea followed by chondritis necrosis of supporting tracheal cartilage. ✯ dt tracheostomy or prolonged transtracheal intubation 91b Critical Care revision notes Dr.Sherif Badrawy
- 184. The following support a diagnosis of SIADH ? 92a Critical Care revision notes Dr.Sherif Badrawy
- 185. a. Urine sodium less than 20mmol/l.【✘】➜ > 20 b. Correction by water restriction.【✔】 c. Pitting oedema.【✘】➜ euvolaemic d. Urine osmolality greater than plasma osmolality.【✔】 【SIADH is characterised by a low plasma sodium, high urinary sodium excretion and a predisposing cause】 92b Critical Care revision notes Dr.Sherif Badrawy
- 186. The following may be signs of 【hypomagnesaemia】: 93a Critical Care revision notes Dr.Sherif Badrawy
- 187. a. Trousseau's and Chvostek's signs.【✔】 b. Hyperreflexia.【✔】 c. Flushing.【✘】➜ a sign of hypermagnesaemia d. Ataxia.【✔】 93b Critical Care revision notes Dr.Sherif Badrawy
- 188. Regarding microshock: 94a Critical Care revision notes Dr.Sherif Badrawy
- 189. a. Risk of ventricular fibrillation is proportional to current density.【✔】 b. Microshock is unlikely with leakage currents at mains frequency (50Hz).【✘】 c. Microshock is unlikely with a leakage current of <50μA.【✔】 d. Type CF equipment is for cardiac use and has a floating circuit.【✔】 94b Critical Care revision notes Dr.Sherif Badrawy
- 190. Regarding the use of therapeutic hypothermia in cardiac arrest survivors: 95a Critical Care revision notes Dr.Sherif Badrawy
- 191. a. Level 1 evidence exists in out-of-hospital cardiac arrest patients with return of spontaneous circulation. 【✔】 b. Cooling should begin as soon as possible.【✔】 c. There is no significant difference in the incidence of arrhythmia compared with normothermic controls. 【✔】 d. Therapeutic hypothermia should be continued for at least 72 hours once instituted.【✘】 95b Critical Care revision notes Dr.Sherif Badrawy
- 192. RTA, fractures of right ribs 5-9 inclusive, with clear lung fields, pH 7.23, PCO2 8.5kPa (64mmHg), PO2 9.6kPa (73mmHg) (FiO2 0.8). 96a Critical Care revision notes Dr.Sherif Badrawy
- 193. a. A chest drain should be inserted immediately.【✘】 b. A CT thorax may provide additional diagnostic information.【✔】 c. Steroids are not indicated.【✔】(or prophylactic antibiotics) d. Ventilation in the right lateral position is likely to improve oxygenation【✘】 96b Critical Care revision notes Dr.Sherif Badrawy
- 194. pulmonary contusion in a trauma Pt ? 97a Critical Care revision notes Dr.Sherif Badrawy
- 195. ✯ trauma + shear stress, bursting forces and【pulmonary vascular damage with secondary alveolar haemorrhage】. ✯ Initial chest X-ray commonly ➜ clear lung fields, with 【opacities taking several hours to appear】. ✯ A CT scan has much > sensitivity ➜ evidence of pulmonary contusion immediately post-injury. ✯ Haemorrhage into the affected lung may continue for 24-48 hours, and【contusions resolve after about 7 days】 . 97b Critical Care revision notes Dr.Sherif Badrawy
- 196. RTA, Abdominal Seatbelt injury, Hb 11.5g/dL, amylase of 60IU/L & AST of 500IU/L. 98a Critical Care revision notes Dr.Sherif Badrawy
- 197. a. Mesenteric injury is a significant concern.【✔】 b. Pancreatic injury is excluded by a normal amylase.【✘】 c. The raised AST should increase suspicion of hepatic injury.【✔】 d. Hypotensive resuscitation should be employed.【✘】 98b Critical Care revision notes Dr.Sherif Badrawy
- 198. Compression from a seatbelt 99a Critical Care revision notes Dr.Sherif Badrawy
- 199. can cause subcapsular haematoma to solid organs, and can cause increased intraluminal pressure and rupture of hollow viscera 99b Critical Care revision notes Dr.Sherif Badrawy
- 200. RTA,GCS of 5 with extensor posturing, and dilated fixed pupils. A CT brain scan shows a 6mm midline shift and diffuse petechial haemorrhages. 100a Critical Care revision notes Dr.Sherif Badrawy
- 201. a. The GCS post-resuscitation has prognostic significance. 【✔】➜ the most important prognostic indicator. b. Midline shift of > 5mm on the CT scan carries a poor prognosis.【✔】 c. A 48-hour infusion of intravenous methylprednisolone is indicated.【✘】 d. The verbal response is the most prognostically useful component of the GCS.【✘】➜ motor component is the most useful 100b Critical Care revision notes Dr.Sherif Badrawy
- 202. The following findings in cerebrospinal fluid are characteristic of the Guillain-Barré syndrome: 101a Critical Care revision notes Dr.Sherif Badrawy
- 203. a. Pleocytosis.【✘】 b. CSF glucose >2/3 of plasma glucose.【✔】 c. Protein >0.5g/L.【✔】 d. Oligoclonal bands.【✘】➜ multiple sclerosis 【Typical CSF in GBS are↑protein (normal range is 0.2-0.4g/L), normal glucose and no ↑WBCs (↑WBCs should cast doubt on the diagnosis)】. 101b Critical Care revision notes Dr.Sherif Badrawy
- 204. CSF characteristic of the Guillain-Barré syndrome: 102a Critical Care revision notes Dr.Sherif Badrawy
- 205. elevated protein normal glucose and no elevation of WBCs (an elevated WBCs should doubt the diagnosis). Oligoclonal bands are characteristic of (but not specific to) demyelinating disease. 102b Critical Care revision notes Dr.Sherif Badrawy
- 206. A 78-y seizure 5 days postcarotid endarterectomy. It spontaneously terminates but on recovery he complains of a severe left-sided 'pounding' headache and a weak right arm. His BP is 205/110mmHg. 103a Critical Care revision notes Dr.Sherif Badrawy
- 207. a. A CT brain scan is not required. 【✘】➜to exclude stroke b. His blood pressure should be reduced by pharmacological means.【✔】 c. Glyceryl trinitrate is the agent of choice. 【✘】 d. A heparin infusion should be started immediately.【✘】 103b Critical Care revision notes Dr.Sherif Badrawy
- 208. The history of seizure, headache and neurological deficit post-endarterectomy suggests 104a Critical Care revision notes Dr.Sherif Badrawy
- 209. ✯ cerebral hyperperfusion syndrome ✯ blood flow is restored to part of the brain where previously it was poor, and normal autoregulatory mechanisms are ineffective ✯ peak ➜ day 5 post-op ✯ requires drug treatment (unlike ischaemic stroke where BP is generally left untreated in the acute phase). ✯ labetalol or clonidine are preferred to nitrates ✯ If left unRx ➜ cerebral oedema and haemorrhagic stroke 104b Critical Care revision notes Dr.Sherif Badrawy
- 210. Regarding sites of vascular access: 105a Critical Care revision notes Dr.Sherif Badrawy
- 211. a. The brachial artery lies between the biceps brachii tendon and the ulnar nerve.【✘】 b. The femoral nerve travels in the femoral canal with the femoral vein and artery.【✘】➜ outside the sheath c. The carotid sheath contains the internal jugular vein, carotid artery and vagus nerve.【✔】 d. The long saphenous vein can be cannulated 2cm posterior and superior to the medial malleolus【✘】➜ anterior and superior 105b Critical Care revision notes Dr.Sherif Badrawy
- 212. Regarding the intensive care management of patients with blunt traumatic brain injury: 106a Critical Care revision notes Dr.Sherif Badrawy
- 213. a. Hyperglycaemia has no bearing on neurological outcome.【✘】➜ glycaemic control improve survival and neurological outcome b. The incidence of deep vein thrombosis is less than 10% in isolated head injury.【✔】 c. Prophylactic anticoagulation for thromboprophylaxis should begin in the first 24h.【✘】➜ after 72h d. Prophylactic hypothermia is a standard of care in the management of these patients.【✘】➜ no statistically significant reduction in mortality 106b Critical Care revision notes Dr.Sherif Badrawy
- 214. RTA, significant abdominal injuries, liver lacerations and diffuse small vessel bleeding, abdomen is packed and the patient is transferred to the ICU, continuous bleeding, regarding the use of recombinant factor VIIa (rFVIIa) 107a Critical Care revision notes Dr.Sherif Badrawy
- 215. a. rFVIIa is not licensed for use in this situation.【✔】➜ licensed for haemophilia A and B b. rFVIIa has been shown to reduce blood transfusion requirements in【blunt trauma】.【✔】➜ This benefit was not shown in patients with penetrating trauma c. Use of rFVIIa is proven to reduce mortality in blunt trauma.【✘】 d. The action of rFVIIa is independent of platelet number and function.【✘】 107b Critical Care revision notes Dr.Sherif Badrawy
- 216. RTA, emergency splenectomy, external fixation of a pelvic fracture and external fixation of a femoral shaft fracture.ATLS grade III shock, ABG lactate of 6.4mmol/L, on arrival in the ICU this has reduced to 3.5mmol/L 108a Critical Care revision notes Dr.Sherif Badrawy
- 217. a. This man has a Type A lactic acidosis.【✔】➜ Type B is dt inability of the organs to metabolise a lactate load b. Lactate is of prognostic significance in trauma patients.【✔】 c. Venous blood can be used for lactate analysis. 【✔】 d. Outlook will be poor if lactate remains above 2mmol/L after 48h.【✔】 108b Critical Care revision notes Dr.Sherif Badrawy
- 218. enclosed space with a burning coal fire. GCS 13 saturation of 96% on high-flow oxygen a brief tonic-clonic seizure which self-terminates ABG pH 7.36, PO2 40.6kPa (308mmHg), PCO2 4.4kPa (33mmHg),calculated SaO2 99%. 109a Critical Care revision notes Dr.Sherif Badrawy
- 219. a. The history and findings are consistent with carbon monoxide poisoning.【✔】 b. There is evidence of a saturation gap.【✘】 c. Oxygen therapy should be titrated down to a lower PaO2.【✘】➜ A standard pulse oximeter measures only two wavelengths of light and falsely interprets COHb as oxyhaemoglobin, overestimating the true arterial oxygen saturation d. Hyperbaric oxygen therapy is contraindicated.【✘】 109b Critical Care revision notes Dr.Sherif Badrawy
- 220. the 'saturation gap' 110a Critical Care revision notes Dr.Sherif Badrawy
- 221. ✯ In Co poisoning True SaO2 can be measured using a co-oximeter which uses multiple wavelengths of light. If measured in this case, true SaO2 would be very low when compared with the falsely elevated SpO2 ✯ SaO2 provided in this question is calculated, however, this is not seen. 110b Critical Care revision notes Dr.Sherif Badrawy
- 222. The following assumptions are made when determining stroke volume using an oesophageal Doppler probe: 111a Critical Care revision notes Dr.Sherif Badrawy
- 223. a. 70% of total cardiac output passes the probe. 【✔】 b. The ascending aorta runs parallel to the oesophagus.【✘】➜ The descending aorta c. The diameter of the aorta is constant throughout systole.【✔】 d. Haematocrit is unchanged between measurements.【✘】➜ haematocrit has no bearing on SV determination. 111b Critical Care revision notes Dr.Sherif Badrawy
- 224. Concerning the measurement of cardiac output by thermodilution techniques: 112a Critical Care revision notes Dr.Sherif Badrawy
- 225. a. A pulmonary artery catheter is required.【✘】➜ only a central line and an arterial cannula b. Cardiac output is inversely proportional to the area under the temperature-time curve.【✔】 c. A small volume of injectate will underestimate cardiac output.【✘】 d. 'Cold' injectate should be at 12-15°C.【✘】➜ ice- cold, the closer the temperature is to blood temperature, the less precise the measurement 112b Critical Care revision notes Dr.Sherif Badrawy
- 226. Regarding the management of carbon monoxide poisoning: 113a Critical Care revision notes Dr.Sherif Badrawy
- 227. a. The half-life of CoHb in air is about 4 hours.【✔】 b. A CoHb level of 60% is commonly lethal.【✔】 c. An otherwise fit and well patient with a CoHb level of 50% will have an arterial oxygen content of approximately 5 mlO2/100ml when breathing 100% oxygen.【✘】 d. Untreated pneumothorax is an absolute CI to hyperbaric oxygen therapy.【✔】 113b Critical Care revision notes Dr.Sherif Badrawy
- 228. The following information can be derived from the arterial pressure waveform: 114a Critical Care revision notes Dr.Sherif Badrawy
- 229. a. Stroke volume from the area under the entire waveform.【✘】➜ from the area under the systolic portion of the arterial waveform b. Myocardial afterload from dP/dt.【✘】➜ The rate of rise in pressure per unit time (dP/dt) is an index of contractility. c. Hypovolaemia from a high dicrotic notch.【✘】➜ low dicrotic notch and a narrow waveform d. Vasodilatation from a steep diastolic rate of decay. 【✔】 114b Critical Care revision notes Dr.Sherif Badrawy
- 230. Regarding the physical principles behind pulse oximetry: 115a Critical Care revision notes Dr.Sherif Badrawy
- 231. a. Light is transmitted through the measurement site at 3Hz.【✘】➜ (30Hz) b. Light is transmitted at wavelengths of 660nm (red) and 940nm (infrared).【✔】 c. The isobestic point indicates an SpO2 of 50%.【✘】 d. The Hagen-Poiseuille law underpins the physics involved.【✘】 115b Critical Care revision notes Dr.Sherif Badrawy
- 232. The pulse oximeter measures ? 116a Critical Care revision notes Dr.Sherif Badrawy
- 233. ✯ the absorbance of red and infrared light transmitted through tissues ✯ Oxyhaemoglobin absorbs more infrared light (940nm) and allows more red light (660nm) to pass through (and vice versa for deoxyhaemoglobin). 116b Critical Care revision notes Dr.Sherif Badrawy
- 234. The isobestic point is 117a Critical Care revision notes Dr.Sherif Badrawy
- 235. the 【wavelength of light】at which absorption is the same for oxy- and deoxy Hb (805nm) regardless of the oxygen saturation of the blood. a reference point for some types of pulse oximeter. 117b Critical Care revision notes Dr.Sherif Badrawy
- 236. 43-y SOB, pleuritic chest pain and haemoptysis.Sat 87% on air, RR is 45, HR is 156, BP is 80/55 Echo moderate RV dilatation, PAP 60mmHg. 118a Critical Care revision notes Dr.Sherif Badrawy
- 237. a. Pulmonary embolism is a likely diagnosis.【✔】 b. The mortality rate is around 1% with this clinical picture.【✘】 c. 【Thrombolysis】 has been shown to reduce the risk of death for such patients.【✘】➜ 【Improve RV function but not to reduce the risk of death】 d. A left ventricular heave is a likely finding on examination【✘】➜ RV affected not LV. 118b Critical Care revision notes Dr.Sherif Badrawy
- 238. The capnograph trace below could be explained by: 119a Critical Care revision notes Dr.Sherif Badrawy
- 239. a. Oesophageal intubation.【✔】 b. Endobronchial intubation.【✘】 c. Massive haemorrhage.【✔】 d. Hyperventilation.【✘】 119b Critical Care revision notes Dr.Sherif Badrawy
- 240. Regarding the following intracranial pressure trace: 120a Critical Care revision notes Dr.Sherif Badrawy
- 241. a. P1 represents transmitted arterial pulsation.【✔】 b. P2 exceeds P1 as intracranial compliance falls.【✔】 c. P3 represents the dicrotic notch.【✔】 d. P1, P2 and P3 are Lundberg waves.【✘】 120b Critical Care revision notes Dr.Sherif Badrawy
- 242. intracranial pressure trace 121a Critical Care revision notes Dr.Sherif Badrawy
- 243. ✪ P1 ➜【transmitted arterial pulsation】 (the percussion wave); ✪ P2 related to ➜ 【brain compliance】 (the tidal wave) and ↑as brain compliance ↓ ✪ P3 dt the 【closure of the aortic valve】 (the dicrotic wave). ✪ Lundberg waves ➜ longer, time-dependent patterns of pressure waves in patients with ↑ICP 121b Critical Care revision notes Dr.Sherif Badrawy
- 244. Regarding the aetiology of massive haemoptysis: 122a Critical Care revision notes Dr.Sherif Badrawy
- 245. a. It more commonly originates from the bronchial than the pulmonary circulation.【✔】In 【90% , bleeding from the bronchial circulation】 b. Chest X-ray identifies the source of bleeding in a minority of cases.【✘】identifies the source of bleeding in 64-80% of cases but CT is even more c. The presence of a nasal septal perforation may suggest Behcet's syndrome.【✘】Wegener's granulomatosis d. Pulmonary-renal syndromes are the commonest cause. 【✘】【Bronchiectasis, tuberculosis and lung cancer】 122b Critical Care revision notes Dr.Sherif Badrawy
- 246. Massive haemoptysis is 123a Critical Care revision notes Dr.Sherif Badrawy
- 247. blood loss of 【100-1000ml in a 24-h】 period from the respiratory tract 123b Critical Care revision notes Dr.Sherif Badrawy
- 248. a patient just admitted to the ICU: sodium 145mmol/L, potassium 3.5mmol/L, urea 17mmol/L (BUN 48mg/dL), creatinine 170μmol/L (1.9mg/dL), bicarbonate 8mmol/L, chloride 105mmol/L, glucose 30mmol/L (550mg/dL). Regarding this patient: 124a Critical Care revision notes Dr.Sherif Badrawy
- 249. a. The anion gap is raised.【✔】 b. The serum osmolality is raised.【✔】 c. The biochemical picture is consistent with 【gastric outflow obstruction】. 【✘】causes a 【hypochloraemic metabolic alkalosis due to loss of HCL】. d. Excessive administration of 0.9% saline can cause this biochemical picture.【✘】 124b Critical Care revision notes Dr.Sherif Badrawy
- 250. Concerning aortic dissection: 125a Critical Care revision notes Dr.Sherif Badrawy
- 251. a. Medical management is the preferred option in uncomplicated Stanford Type B dissection.【✔】 b. Medical management includes noradrenaline infusion to maintain renal perfusion pressure.【✘】 c. The commonest site of origin is the descending aorta.【✘】 【ascending aorta】 d.【A TEE is the Ix of choice in patients too unstable for angiography】.【✔】 125b Critical Care revision notes Dr.Sherif Badrawy
- 252. Regarding the Injury Severity Score (ISS): 126a Critical Care revision notes Dr.Sherif Badrawy
- 253. a. It is comprised of anatomical and physiological data.【✘】 b. The maximum score is 75.【✔】 c. Head injury carries the highest weighting.【✘】 d. Six body regions are defined.【✔】 (head, face, chest, abdomen, extremities [including pelvis], external). 126b Critical Care revision notes Dr.Sherif Badrawy
- 254. limitations of the Injury Severity Score (ISS) 127a Critical Care revision notes Dr.Sherif Badrawy
- 255. A patient with several wounds to the same body region can only score once for that region; in such a case the ISS may underestimate the severity of their injuries. 127b Critical Care revision notes Dr.Sherif Badrawy
- 256. The following are good predictors of increased hospital mortality in patients with COPD requiring MV 128a Critical Care revision notes Dr.Sherif Badrawy
- 257. a. Mechanical ventilation lasting >72h. 【✔】 b. An FEV1 <30% predicted prior to ICU admission.【✘】 c. One failed extubation attempt.【✔】 d. Presence of comorbidities.【✔】 128b Critical Care revision notes Dr.Sherif Badrawy
- 258. Facts about predictors of increased hospital mortality in patients with COPD requiring MV 129a Critical Care revision notes Dr.Sherif Badrawy
- 259. ✪ Interestingly, survival rates were also much better in patients with a previous episode of mechanical ventilation ✪ FEV1 is an important predictor of long- term survival, but does not predict short- term outcome in COPD patients requiring MV 129b Critical Care revision notes Dr.Sherif Badrawy
- 260. Regarding therapeutic interventions for massive haemoptysis: 130a Critical Care revision notes Dr.Sherif Badrawy
- 261. a. Bronchial artery embolisation is successful in the majority of cases.【✔】➜ 75-90% of patients b. Emergency lung resection carries a 60% mortality.【✘】 c. Bronchoscopic lavage with epinephrine 1:10000 may be useful.【✔】 d. Rigid bronchoscopy has no place in this situation.【✘】➜ has a role but cannot visualise the periphery of the tracheobronchial tree. 130b Critical Care revision notes Dr.Sherif Badrawy
- 262. (PEEP) in patients with (ARDS): 131a Critical Care revision notes Dr.Sherif Badrawy
- 263. a. High PEEP (>12cmH2O) reduces ICU mortality compared with low PEEP (5-12cmH2O).【✘】 b. PEEP should be set below the lower inflection point on the pressure-volume curve.【✘】 c. High PEEP improves the PaO2/FiO2 ratio compared with low PEEP. 【✔】 d. PEEP causes atelectrauma.【✘】 131b Critical Care revision notes Dr.Sherif Badrawy
- 264. Regarding atrial fibrillation: 132a Critical Care revision notes Dr.Sherif Badrawy
- 265. a. Maximum cardiac output occurs with ventricular rate controlled to 50bpm.【✘】➜ the optimum ventricular rate is around 90bpm at rest b. The atria are normally responsible for 40-50% of ventricular filling.【✘】➜ 15-30% c. Valvular heart disease is the commonest cause.【✘】➜ IHD d. 'Atrial stunning' commonly occurs after successful cardioversion.【✔】➜ Atrial mechanical function usually improves over the first 24 hours. 132b Critical Care revision notes Dr.Sherif Badrawy
- 266. The following are absolute contraindications to the use of an intra- aortic balloon pump: 133a Critical Care revision notes Dr.Sherif Badrawy
- 267. a. Clinically significant aortic stenosis. 【✘】➜ clinically significant AR b. Refractory angina.【✘】 c. Aortic dissection.【✔】 d. Severe peripheral vascular disease. 【✘】➜ a relative CI, Also Morbid obesity & AAA. 133b Critical Care revision notes Dr.Sherif Badrawy
- 268. 77-y M, in HDU, a new right-sided homonymous hemianopia and dysphasia HR of 85bpm, BP of 190/105 mmHg, SpO2 of 96% on room air. A CT brain scan is unremarkable. Appropriate initial management includes: 134a Critical Care revision notes Dr.Sherif Badrawy
- 269. a. Aspirin 300mg.【✔】➜ clinical evidence of a stroke ➜ ↓recurrence of stroke b. Clopidogrel 300mg.【✘】 c. Treatment dose of low-molecular-weight heparin.【✘】 d. Labetalol.【✘】 134b Critical Care revision notes Dr.Sherif Badrawy
- 270. Anticoagulation in the acute phase of ischaemic stroke 135a Critical Care revision notes Dr.Sherif Badrawy
- 271. Anticoagulation has no benefit in the acute phase of ischaemic stroke (except in special cases such as venous sinus thrombosis) and should not be given 135b Critical Care revision notes Dr.Sherif Badrawy
- 272. Hypertension in acute stroke 136a Critical Care revision notes Dr.Sherif Badrawy
- 273. should not be actively lowered unless pressures of 220mmHg (systolic) or 120mmHg (diastolic) are reached. If thrombolysis is considered, lower thresholds for treatment exist (185mmHg systolic, 110mmHg diastolic) 136b Critical Care revision notes Dr.Sherif Badrawy
- 274. The following features favour a diagnosis of encephalopathy over encephalitis in a patient presenting with an altered sensorium: 137a Critical Care revision notes Dr.Sherif Badrawy
- 275. a. Meningism.【✘】 b. Normal cerebrospinal fluid analysis. 【✔】 c. Gradual steady deterioration in mental status.【✔】 d. Seizures.【✘】 137b Critical Care revision notes Dr.Sherif Badrawy
- 276. commonest cause of acute encephalitis 138a Critical Care revision notes Dr.Sherif Badrawy
- 277. Herpes simplex 138b Critical Care revision notes Dr.Sherif Badrawy
- 278. The following interventions are effective in reducing the incidence of acute renal failure in selected populations: 139a Critical Care revision notes Dr.Sherif Badrawy
- 279. a. Low dose dopamine infusion (2μg/kg/min).【✘】 b. Mannitol.【✘】 c. Normal saline infusion prior to administration of radiocontrast media. 【✔】 d. N-acetylcysteine prior to administration of radiocontrast media.【✔】 139b Critical Care revision notes Dr.Sherif Badrawy
- 280. IV drug abuser is admitted to the ICU.itchy, and feeling lethargic and unwell. She is sleepy but arousable, and is incoherent and extremely confused. Asterixis is present. Serology confirms acute hepatitis B infection; the prothrombin time is 70 seconds. 140a Critical Care revision notes Dr.Sherif Badrawy
- 281. a. This patient has grade III hepatic encephalopathy.【✔】 b. The clotting deficit should be corrected with fresh frozen plasma.【✘】➜ should not be corrected in the absence of bleeding or invasive procedures c. Survival rates for this condition without liver transplant are around 60%.【✘】➜ Mortality without liver transplantation is around 90% for fulminant hepatic failure d. Cerebral oedema is a likely cause of the confusional state 【✔】➜ best assessed with ICP monitoring (after CT brain scan to exclude other causes) 140b Critical Care revision notes Dr.Sherif Badrawy
- 282. Regarding acalculous cholecystitis in the ICU patient: 141a Critical Care revision notes Dr.Sherif Badrawy
- 283. a. It has a high mortality.【✔】➜ mortality up to 40% b. The incidence is around 0.2%.【✔】 c. Gram negative biliary tract sepsis is the initiating cause.【✘】 d. U/S is highly sensitive and specific for the condition.【✘】➜ only moderate, CT has greater diagnostic accuracy 141b Critical Care revision notes Dr.Sherif Badrawy
- 284. 45-y admitted to the ICU with signs of sepsis. c/o of a painful, swollen knee for the last 3 d no history of trauma no previous history of joint problems or other medical problems, apyrexial, ESR of 72mm/h. A diagnosis of septic arthritis is considered. 142a Critical Care revision notes Dr.Sherif Badrawy
- 285. a. Septic arthritis is unlikely in the absence of pyrexia.【✘】 b. An elevated ESR is a sensitive indicator of septic arthritis.【✔】 c. Plain radiography is often diagnostic. 【✘】 d. A negative Gram stain of joint fluid aspirate excludes the diagnosis.【✘】 142b Critical Care revision notes Dr.Sherif Badrawy
- 286. Regarding the RIFLE criteria classification system for acute renal failure: 143a Critical Care revision notes Dr.Sherif Badrawy
- 287. a. The 'E' in 'RIFLE' represents end-stage kidney disease.【✔】 b. Kidney failure can be diagnosed based on urine output alone.【✔】 c. Criteria for risk of kidney injury are specific but not sensitive.【✘】 d. Serum creatinine is accepted as an index of glomerular function.【✔】 143b Critical Care revision notes Dr.Sherif Badrawy
- 288. RIFLE criteria 144a Critical Care revision notes Dr.Sherif Badrawy
- 289. 144b Critical Care revision notes Dr.Sherif Badrawy
- 290. The following drugs require altered dosing in patients with advanced liver cirrhosis: 145a Critical Care revision notes Dr.Sherif Badrawy
- 291. a. Midazolam.【✔】 b. Remifentanil.【✘】 c. Atracurium.【✘】➜ Hofmann elimination (a non-enzymatic process which occurs at physiological pH and temperature) d. Propofol.【✔】➜ conjugated in the liver with glucuronides and sulphates before excretion in urine 145b Critical Care revision notes Dr.Sherif Badrawy
- 292. When commencing renal replacement therapy, the following properties predict significantly increased clearance of a drug compared with the anuric state: 146a Critical Care revision notes Dr.Sherif Badrawy
- 293. a. Low protein-binding.【✔】 b. Low volume of distribution.【✔】 c. High non-renal clearance.【✘】 d. High molecular weight.【✘】 146b Critical Care revision notes Dr.Sherif Badrawy
- 294. The following are common features of 3,4- methylenedioxymethamphetamine ('ecstasy') poisoning: 147a Critical Care revision notes Dr.Sherif Badrawy
- 295. a. Rhabdomyolysis.【✔】 b. Hypernatraemia.【✘】➜ Hyponatraemia dt excessive sodium loss in sweat, excessive water intake and enhanced ADH c. Hyperthermia.【✔】 d. Non-cardiogenic pulmonary oedema. 【✘】 147b Critical Care revision notes Dr.Sherif Badrawy
- 296. Other complications of ('ecstasy') poisoning 148a Critical Care revision notes Dr.Sherif Badrawy
- 297. hypertension, tachyarrhythmias and, rarely, stroke (haemorrhagic or thrombotic) and hepatotoxicity. 148b Critical Care revision notes Dr.Sherif Badrawy
- 298. Regarding obstetric-related deaths in the developed world: 149a Critical Care revision notes Dr.Sherif Badrawy
- 299. a. More mothers die from indirect causes (pre-existing disease exacerbated by pregnancy) than direct causes (bleeding, preeclampsia, etc.).【✔】 b. Haemorrhage is the leading direct cause of obstetric death.【✘】 c. Inability to intubate the patient is the leading cause of anaesthetic related deaths.【✘】 d. Psychiatric disease is the commonest indirect cause of death.【✘】 149b Critical Care revision notes Dr.Sherif Badrawy
- 300. MCC of obstetric deaths ? 150a Critical Care revision notes Dr.Sherif Badrawy
- 301. MCC is cardiac disease exacerbated by pregnancy (an indirect cause), MC direct cause of death is thromboembolic disease, followed by hypertensive disease of pregnancy and then haemorrhage. Psychiatric disease is the second most common indirect cause of death 150b Critical Care revision notes Dr.Sherif Badrawy
- 302. A patient with severe pre-eclampsia becomes unwell in the peripartum period with blurred vision, clonus and a BP of 180/120mmHg. The following are appropriate initial antihypertensive treatments: 151a Critical Care revision notes Dr.Sherif Badrawy
- 303. a. Labetalol.【✔】 b. Hydralazine.【✔】 c. Nitroprusside.【✘】 d. Metolazone.【✘】 151b Critical Care revision notes Dr.Sherif Badrawy
- 304. previously fit pregnant woman, mildly unwell in the third trimester, palmar erythema, ALP 100IU/L, albumin 35g/L, ALT 35IU/L. 152a Critical Care revision notes Dr.Sherif Badrawy
- 305. a. Obstructive jaundice is likely to be present. 【✘】 b. There is evidence of pre-existing liver disease.【✘】 c. Albumin is normally low in pregnancy (compared with non-pregnant values).【✔】 d. Aminotransferases are normally elevated in the third trimester.【✘】➜ ALP rise in normal pregnancy 152b Critical Care revision notes Dr.Sherif Badrawy
- 306. Regarding noradrenaline (norepinephrine): 153a Critical Care revision notes Dr.Sherif Badrawy
- 307. a. A typical dose range would be 5-10μg/kg/min. 【✘】➜ 0.05- 0.5µg/kg/min b. It is a metabolite of adrenaline (epinephrine). 【✘】➜ formed from dopamine & metabolised to adrenaline c. It causes coronary artery vasodilatation increasing coronary blood flow.【✔】 d. It increases contractility of the pregnant uterus.【✔】 153b Critical Care revision notes Dr.Sherif Badrawy
- 308. A postoperative patient, HDU, morphine infusion 2mg/hour., still in pain following surgery, and the nursing staff ask you to adjust the morphine regime. 154a Critical Care revision notes Dr.Sherif Badrawy
- 309. a. Doubling the rate to 4mg/h will take about half an hour to have significant effect.【✘】If a drug is infused it takes about five half-lives to reach a steady state b. The half-life of morphine is around 2-3 hours.【✔】 c. If the clearance of morphine is halved by renal impairment, its half life will double.【✔】 d. The volume of distribution of morphine is around 0.5L/kg.【✘】 154b Critical Care revision notes Dr.Sherif Badrawy
- 310. The following data can be obtained from transpulmonary thermodilution: 155a Critical Care revision notes Dr.Sherif Badrawy
- 311. a. Cardiac output.【✔】 b. An estimate of preload.【✔】 c. An estimate of pulmonary oedema. 【✔】 d. An estimate of total circulating blood volume.【✘】 155b Critical Care revision notes Dr.Sherif Badrawy
- 312. Transpulmonary thermodilution concept ? 156a Critical Care revision notes Dr.Sherif Badrawy
- 313. ✪ the delivery of a bolus of 15-20ml of cold fluid (<8°C) through a CVC with temperature-time measurement at an arterial site (usually femoral) with a thermistor- tipped arterial cannula. The temperature-time curve produced gives an estimate of COP according to a modified form of the Stewart-Hamilton equation. ✪ global end-diastolic volume [GEDV] an estimate of preload which may be a better predictor of fluid requirements than CVP ✪ extravascular lung water EVLW is a measure of pulmonary oedema guide diuretic therapy a more sensitive marker of pulmonary oedema than chest X- ray. ✪ Total intrathoracic blood volume can be estimated by transpulmonary thermodilution, but not total circulating blood volume. 156b Critical Care revision notes Dr.Sherif Badrawy
- 314. Regarding pressure ulcers in the ICU: 157a Critical Care revision notes Dr.Sherif Badrawy
- 315. a. A high Waterlow score is associated with an increased risk of pressure ulcer development.【✔】 b. Nursing workload increases by 50% if a pressure ulcer is present.【✔】➜ since dressing changes and positioning manoeuvres are time-consuming c. Pressure ulcers bear little relation to in-hospital mortality.【✘】 d. Patients with a pressure ulcer should be repositioned every 8 hours.【✘】➜ every 2 hours 157b Critical Care revision notes Dr.Sherif Badrawy
- 316. Regarding the management of risk in the ICU and the techniques available for analysing risk factors: 158a Critical Care revision notes Dr.Sherif Badrawy
- 317. a. The vast majority of clinical adverse incidents are dt a lack of technical skills in the medical staff.【✘】50% dt non-technical skill deficit b. Root cause analysis should be applied to all minor incidents in order to prevent future major incidents.【✘】 c. Observational studies using simulated patients are useful for assessing non-technical skills.【✔】 d. Attitudinal studies may not accurately reflect real life performance.【✔】 158b Critical Care revision notes Dr.Sherif Badrawy
- 318. Root cause analysis ? 159a Critical Care revision notes Dr.Sherif Badrawy
- 319. ✾ detailed examination of all the technical and non-technical factors associated with an adverse incident ✾ extremely time consuming and should be reserved for serious critical incidents. 159b Critical Care revision notes Dr.Sherif Badrawy
- 320. Regarding tracheal stenosis as a complication of tracheostomy: 160a Critical Care revision notes Dr.Sherif Badrawy
- 321. a. MC occurs at the site of the tracheostomy tube cuff. 【✘】➜ at the level of the stoma or directly above it b. It is a much more common complication than tracheomalacia.【✔】➜ Tracheomalacia is a very rare complication of tracheostomy. c. Patients rarely show symptoms in the first 3 months following decannulation.【✘】➜ present within 2 month d. Stridor is an early sign.【✘】➜ Stridor is a late sign, and signifies advanced stenosis (<5-10mm airway diameter). 160b Critical Care revision notes Dr.Sherif Badrawy
- 322. MC complication of tracheostomy 161a Critical Care revision notes Dr.Sherif Badrawy
- 323. ✪ Tracheal stenosis ✪ symptoms may be non-specific ✪ Risk factors ➜ prolonged ETT, stomal site infection, old age, sepsis, oversized cannulae, excessive tube motion and prolonged placement ✪ asymptomatic until 75% airway narrowing has occurred 161b Critical Care revision notes Dr.Sherif Badrawy
- 324. tracheo-innominate artery fistula as a complication of tracheostomy 162a Critical Care revision notes Dr.Sherif Badrawy
- 325. ✪ rare but almost universally fatal complication of tracheostomy. ✪ The innominate artery crosses the trachea at the level of the ninth tracheal ring, and therefore risk is increased with a low cannula placement. ✪ bleeding, massive haemoptysis and near- 100% mortality. 162b Critical Care revision notes Dr.Sherif Badrawy
- 326. Tracheomalacia as a complication of tracheostomy 163a Critical Care revision notes Dr.Sherif Badrawy
- 327. ✪ ischaemic injury to the trachea followed by chondritis and subsequent destruction and necrosis of tracheal cartilage. As with tracheal stenosis, symptoms may be non- specific. ✪ Flow-volume loops may show a variable intrathoracic obstruction (expiratory collapse of the trachea). 163b Critical Care revision notes Dr.Sherif Badrawy
- 328. CP of refeeding syndrome ? 164a Critical Care revision notes Dr.Sherif Badrawy
- 329. ✪ may occur with either enteral or parenteral nutrition. ✪ ↓serum phosphate ➜ arrhythmias, HF, Wernicke's encephalopathy, leukocyte and platelet dysfunction rhabdomyolysis, renal failure and myopathy. All abnormalities are dt hypophosphataemia, which is a consequence of ↑insulin [insulin causes cellular uptake of phosphate ➜ hypophosphataemia]. ✪ ↑insulin is dt switch from a starvation state to CHO metabolism. 164b Critical Care revision notes Dr.Sherif Badrawy
- 330. Rx of refeeding syndrome ? 165a Critical Care revision notes Dr.Sherif Badrawy
- 331. prophylactic thiamine and intravenous phosphate replacement if <0.5mmol/L or symptomatic 165b Critical Care revision notes Dr.Sherif Badrawy
- 332. Third degree heart block , Asymptomatic, the heart rate is <40bpm, Pacing ? 166a Critical Care revision notes Dr.Sherif Badrawy
- 333. CHB is an accepted indication for transvenous pacing even in the absence of symptoms if the HR is <40bpm 166b Critical Care revision notes Dr.Sherif Badrawy
- 334. The lowest pH in the first 24h post-arrest correlates with mortality when 167a Critical Care revision notes Dr.Sherif Badrawy
- 335. it is below 7.25, presumably reflecting the duration of the arrest and the quality of organ function in the post-resuscitation phase. 167b Critical Care revision notes Dr.Sherif Badrawy
- 336. Regarding cardiac tamponade 168a Critical Care revision notes Dr.Sherif Badrawy
- 337. ✪ It is more common in penetrating than blunt trauma. ✪ The jugular venous pressure may be normal. ✪ A fall of >10mmHg in systolic BP during inspiration defines pulsus paradoxus. ✪ ECG findings of electrical alternans is pathognomonic of cardiac tamponade. ✪ In chronic tamponade enlargement of the cardiac silhouette but not in acute cases low compliance of the pericardium leads to rapid tamponade 168b Critical Care revision notes Dr.Sherif Badrawy
- 338. Regarding the fluid resuscitation of the trauma patient 169a Critical Care revision notes Dr.Sherif Badrawy
- 339. a. Resuscitation with large volumes of crystalloid increases the incidence of abdominal compartment syndrome. b. No evidence that Hypertonic saline increase survival compared with crystalloid. c. Arterial base deficit is a better indicator of adequacy of fluid resuscitation than urine output. d. Serum lactate is a better indicator of adequacy of fluid resuscitation than urine output. e. Rate of clearance of base deficit is correlated with survival. 169b Critical Care revision notes Dr.Sherif Badrawy
- 340. J waves (with hypothermia) represents 170a Critical Care revision notes Dr.Sherif Badrawy
- 341. abnormality in the earliest phase of ventricular repolarisation 170b Critical Care revision notes Dr.Sherif Badrawy
- 342. Classification of Post-traumatic seizure (PTS) 171a Critical Care revision notes Dr.Sherif Badrawy
- 343. ✪ early (within 7 days of injury) or late (after 7 days).Prophylactic phenytoin is effective in preventing early (<7 days) but not late (>7 days) PTS. ✪ Routine seizure prophylaxis is reasonable in high-risk cases but should be stopped after 7 days unless a specific indication for continued therapy exists 171b Critical Care revision notes Dr.Sherif Badrawy
- 344. Risk factors for Post-traumatic seizure (PTS) 172a Critical Care revision notes Dr.Sherif Badrawy
- 345. GCS <10, SDH, EDH or ICH, depressed skull fracture and penetrating head injury 172b Critical Care revision notes Dr.Sherif Badrawy
- 346. The incidence of thromboembolic problems in patients treated with rFVIIa is 173a Critical Care revision notes Dr.Sherif Badrawy
- 347. ✪ 1% in haemophiliacs, and 1.4% in cases of non-haemophilia coagulopathy. ✪ given in large, supra-physiological doses for major haemorrhage (an off-label indication) 173b Critical Care revision notes Dr.Sherif Badrawy
- 348. patient with major burns 174a Critical Care revision notes Dr.Sherif Badrawy
- 349. a. Aggressive high calorie feeding (>200% of resting requirement) increase mortality. b. Enteral feeding is preferred to parenteral. c. Protein requirement is 1.5-2g/kg/day. d. Nutritional supplementation with glutamine is of no proven benefit. e. Hyperglycaemia should be treated aggressively. 174b Critical Care revision notes Dr.Sherif Badrawy
- 350. Protein binding of thyroid hormones 175a Critical Care revision notes Dr.Sherif Badrawy
- 351. T4 is 99.97% protein-bound, T3 99.7%. 175b Critical Care revision notes Dr.Sherif Badrawy
- 352. Factors ↓peripheral conversion of T4 to T3 ? 176a Critical Care revision notes Dr.Sherif Badrawy
- 353. critical illness, fasting, malnutrition and by drugs including propylthiouracil, corticosteroids, propranolol and amiodarone. 176b Critical Care revision notes Dr.Sherif Badrawy
- 354. Effect of Dopamine and somatostatin on TRH ? 177a Critical Care revision notes Dr.Sherif Badrawy
- 355. both inhibit TRH release 177b Critical Care revision notes Dr.Sherif Badrawy
- 356. treatment of choice for ESBL-producing organisms ? 178a Critical Care revision notes Dr.Sherif Badrawy
- 357. carbapenems 178b Critical Care revision notes Dr.Sherif Badrawy
- 358. MCC of ESBL producing organisms ? 179a Critical Care revision notes Dr.Sherif Badrawy
- 359. gram-negative bacilli, of which Klebsiella pneumoniae is the commonest. 179b Critical Care revision notes Dr.Sherif Badrawy
- 360. What's flow time corrected (FTc) in oesophageal Doppler measurements ? 180a Critical Care revision notes Dr.Sherif Badrawy
- 361. FTc is a marker of afterload (a low FTc indicates a high afterload). Since hypovolaemia causes an increase in systemic vascular resistance, FTc is also an indirect marker of preload and is often used for this purpose. However, other conditions such as hypothermia, cardiac failure and vasopressor therapy may similarly increase afterload (reducing FTc) despite adequate or excessive preload. 180b Critical Care revision notes Dr.Sherif Badrawy
- 362. Normal value of flow time corrected (FTc) in oesophageal Doppler measurements ? 181a Critical Care revision notes Dr.Sherif Badrawy
- 363. ✪ an FTc of ~340ms is considered 'normal', this should not be a target of fluid Rx. As with all forms of COP monitoring, trends are > important than absolute values. If a fluid bolus ➜ ↑FTc and a significant (>10%) ↑in SV, this suggests > volume is required. ✪ If there is little change, giving further fluid may be harmful. FTc gives no information regarding cardiac contractility (peak velocity is more useful in this respect). 181b Critical Care revision notes Dr.Sherif Badrawy
- 364. markers of the adequacy of the circulation? 182a Critical Care revision notes Dr.Sherif Badrawy
- 365. ❁ Arterial lactate. ❁ Venous lactate. ❁ Base deficit. ❁ Central venous oxygen saturation. ❁ While a low PAOP may indicate hypovolaemia, it is a poor predictor of the adequacy of circulating volume, and bears little relation to the adequacy of tissue perfusion. 182b Critical Care revision notes Dr.Sherif Badrawy
- 366. When Hypotension is a problem with opiates ? 183a Critical Care revision notes Dr.Sherif Badrawy
- 367. when patients have been inadequately fluid-resuscitated, since the sympathetic tone maintaining blood pressure is damped by their administration. 183b Critical Care revision notes Dr.Sherif Badrawy
- 368. Fentanyl is useful in the ICU because of its very short context sensitive half-life, True or False ? 184a Critical Care revision notes Dr.Sherif Badrawy
- 369. Although fentanyl has a short offset following a bolus dose, it has a much longer context-sensitive half- life (around 300 minutes after an 8-hour infusion, and a similar offset time to morphine after infusion for 24 hours). 184b Critical Care revision notes Dr.Sherif Badrawy
- 370. best lead for monitoring rhythm disturbances ? 185a Critical Care revision notes Dr.Sherif Badrawy
- 371. Lead II since its axis parallels the electrical axis of the heart, giving the best visualisation of the P wave. 185b Critical Care revision notes Dr.Sherif Badrawy
- 372. most sensitive detector of left ventricular ischaemia ? 186a Critical Care revision notes Dr.Sherif Badrawy
- 373. Lead V5 186b Critical Care revision notes Dr.Sherif Badrawy
- 374. An oesophageal lead is used in the detection of which ischaemia ? 187a Critical Care revision notes Dr.Sherif Badrawy
- 375. posterior ischaemia 187b Critical Care revision notes Dr.Sherif Badrawy
- 376. A low probability V/Q scan effectively rules out a PE, True or False ? 188a Critical Care revision notes Dr.Sherif Badrawy
- 377. False, V/Q scans are reported as high, intermediate, low probability or normal. While a normal scan reliably excludes a PE, a low probability scan does not and requires further imaging unless the clinical probability is also low. 188b Critical Care revision notes Dr.Sherif Badrawy
- 378. DD bw pulmonary angiography spiral CT in Dx PE ? 189a Critical Care revision notes Dr.Sherif Badrawy
- 379. Although pulmonary angiography is the gold standard, spiral CT is highly sensitive for lobar or segmental PE; it may miss subsegmental PE. 189b Critical Care revision notes Dr.Sherif Badrawy
- 380. Use of Echocardiography in PE ? 190a Critical Care revision notes Dr.Sherif Badrawy
- 381. ❁ shocked ICU patient in whom PE is being considered as the cause of the HD compromise. ❁ the absence of RV dysfunction or overload excludes Dx. Echo is not sensitive for detecting subsegmental PE. 190b Critical Care revision notes Dr.Sherif Badrawy
- 382. Definition of Pseudohypoxaemia or 'leukocyte larceny' ? 191a Critical Care revision notes Dr.Sherif Badrawy
- 383. a spuriously low PaO2 in the ABG of patients with a very high WBCs. dt consumption of dissolved O2 in the sample by the metabolically active leukoblasts. Immediate analysis of a sample placed on ice will give a higher and more representative PaO2. 191b Critical Care revision notes Dr.Sherif Badrawy
- 384. intracranial pressure monitoring devices 192a Critical Care revision notes Dr.Sherif Badrawy
- 385. ❁ An intraventricular catheter is the gold standard. ❁ A Camino bolt cannot be re-zeroed once sited ❁ Infection rates are low with intraparenchymal strain gauge monitors. ❁ Parenchymal ICP monitoring > accurate than subdural, extradural and subarachnoid monitoring ❁ The pressure transducer for an intraventricular catheter should be kept at the level of the foramen of Munro 192b Critical Care revision notes Dr.Sherif Badrawy
- 386. critical care management of patients with cystic fibrosis 193a Critical Care revision notes Dr.Sherif Badrawy
- 387. The outcome for respiratory failure requiring MV is poor even in younger patients. 193b Critical Care revision notes Dr.Sherif Badrawy
- 388. Drugs given via the ETT during CPR ? 194a Critical Care revision notes Dr.Sherif Badrawy
- 389. ❁ Epinephrine. ❁ Atropine. ❁ Naloxone. ❁ Lidocaine. 194b Critical Care revision notes Dr.Sherif Badrawy
- 390. PaCO2 and pH are better predictors of the need for mechanical ventilation than PaO2 in COPD Pts ? 195a Critical Care revision notes Dr.Sherif Badrawy
- 391. True 195b Critical Care revision notes Dr.Sherif Badrawy
- 392. flow-volume loop of a 40-year-old man best described by a diagnosis of: 196a Critical Care revision notes Dr.Sherif Badrawy
- 393. Restrictive disease. 196b Critical Care revision notes Dr.Sherif Badrawy
- 394. volume/time graphic on a mechanical ventilator suggests 197a Critical Care revision notes Dr.Sherif Badrawy
- 395. ❁ Dynamichyperinflation isoccurring. ❁ waveform doesnot return to baseline on each occasion, and becomesprogressively higher ❁ Disconnect breathing circuit for a few secondsallowstrapped gasto escape returning the waveform to baseline 197b Critical Care revision notes Dr.Sherif Badrawy
- 396. management of atrial fibrillation 198a Critical Care revision notes Dr.Sherif Badrawy
- 397. ❁ The risk of thromboembolic complications is similar with electrical or chemical cardioversion. ❁ Digoxin is an ineffective rate control in the critically ill patient.(ineffective in hyperadrenergic states) ❁ Successful cardioversion is more likely in atrial fibrillation of short duration. ❁ Beta-blockers should not be used as first-line therapy in patients with decompensated heart failure ❁ Rhythm control has no long-term mortality benefit compared with rate control 198b Critical Care revision notes Dr.Sherif Badrawy
- 398. Which ONE of the following confers the greatest mortality benefit when used appropriately in the management of STEMI ? a. Aspirin. b. Gylceryl trinitrate. c. Atenolol. d. Oxygen. e. Thrombolysis. 199a Critical Care revision notes Dr.Sherif Badrawy
- 399. ❁ Aspirin. ❁ a better answer than thrombolysis. ❁ aspirin in a dose of 162-325mg. This should be given within 24 hours of STEMI, but has not been shown to be as time- critical as thrombolysis. 199b Critical Care revision notes Dr.Sherif Badrawy
- 400. What's this form ? 200a Critical Care revision notes Dr.Sherif Badrawy
- 401. Arterial pressure waveform intra-aortic balloon counterpulsation with a 1:2 ratio. 200b Critical Care revision notes Dr.Sherif Badrawy
- 402. Mechanism of intra-aortic balloon counterpulsation 201a Critical Care revision notes Dr.Sherif Badrawy
- 403. The cylindrical balloon sits 【distal to the left subclavian artery】 and 【inflates at the start of diastole】, 【gauged by the dicrotic notch on the arterial trace】. It remains inflated throughout diastole, the augmented pressure wave ↑coronary perfusion pressure. 【It deflates during isovolumetric contraction】, before ejection of blood from the left ventricle begins.The fall in afterload produced by this deflation reduces cardiac work and O2 consumption.a modest ↑in COP is seen. 201b Critical Care revision notes Dr.Sherif Badrawy
- 404. An ischaemic stroke patient, If the patient is a candidate for thrombolysis, should we give aspirin ? 202a Critical Care revision notes Dr.Sherif Badrawy
- 405. NO, Aspirin should be given to all ischaemic stroke patients who are not candidates for thrombolysis 202b Critical Care revision notes Dr.Sherif Badrawy
- 406. Electromyelography showing an incremental increase in compound muscle action potential response with high rates of repetitive stimulation is in keeping with 203a Critical Care revision notes Dr.Sherif Badrawy
- 407. Lambert-Eaton myasthenic syndrome 203b Critical Care revision notes Dr.Sherif Badrawy
- 408. Fasciculations are characteristic of 204a Critical Care revision notes Dr.Sherif Badrawy
- 409. lower motor neurone pathology and are classically seen in patients with motor neurone disease 204b Critical Care revision notes Dr.Sherif Badrawy
- 410. Pentoxyphylline in Rx of rhabdomyolysis 205a Critical Care revision notes Dr.Sherif Badrawy
- 411. Pentoxyphylline is a free radical scavenger which have theoretical but largely unproven benefits in Rx of rhabdomyolysis 205b Critical Care revision notes Dr.Sherif Badrawy
- 412. risk factors for the development of stress-related mucosal damage 206a Critical Care revision notes Dr.Sherif Badrawy
- 413. ✲ Mechanical ventilation. ✲ Burns. ✲ Coagulopathy. ✲ Hypotension. 206b Critical Care revision notes Dr.Sherif Badrawy
- 414. 85-year-old nursing home resident is admitted to the hospital with a painful, swollen right knee joint, antibiotic therapy ? 207a Critical Care revision notes Dr.Sherif Badrawy
- 415. ✲ Vancomycin + cefuroxime. ✲ Patient's at risk of MRSA ➜ nursing home residents and recent inpatients ➜ should be treated with vancomycin and a 2nd or 3rd generation cephalosporin 207b Critical Care revision notes Dr.Sherif Badrawy
- 416. regard to balloon tamponade with a Sengstaken or Minnesota tube 208a Critical Care revision notes Dr.Sherif Badrawy
- 417. ✲ Acute bleeding is controlled in 90% of cases ✲ further bleeding is common following balloon deflation 50% of cases). ✲ tube should be inserted to at least 【45cm before inflation】 of the gastric balloon to prevent inflation in the oesophagus. ✲ A volume of 【300-500ml fluid】 is required to fully inflate the gastric balloon. ✲ Maximum traction should not exceed 1kg. 208b Critical Care revision notes Dr.Sherif Badrawy
- 418. Which drug will not have ↑clearance with CRRT compared with the anuric state a. Vancomycin. b. Gentamicin. c. Atenolol. d. Amiodarone. e. Lithium. 209a Critical Care revision notes Dr.Sherif Badrawy
- 419. d. Amiodarone. Amiodarone has a very large Vd, is eliminated in bile and is highly protein- bound and is therefore not significantly eliminated by RRT. 209b Critical Care revision notes Dr.Sherif Badrawy
- 420. For a drug to be significantly cleared by renal replacement therapy, it must 210a Critical Care revision notes Dr.Sherif Badrawy
- 421. have low protein binding (only the free fraction is filtered). It must have a low non- renal clearance, It must have a low volume of distribution 210b Critical Care revision notes Dr.Sherif Badrawy
- 422. Active cooling should be initiated if 211a Critical Care revision notes Dr.Sherif Badrawy
- 423. ✲ the core temperature exceeds 40°C. ✲ Dantrolene has been used for the treatment of hyperthermia in 'ecstasy' Toxicity 211b Critical Care revision notes Dr.Sherif Badrawy
- 424. SIRS & Sepsis definition 212a Critical Care revision notes Dr.Sherif Badrawy
- 425. 212b Critical Care revision notes Dr.Sherif Badrawy
- 426. Acute fatty liver of pregnancy 213a Critical Care revision notes Dr.Sherif Badrawy
- 427. ✲ occurs in the third trimester ✲ dt enzymatic defect in fatty acid oxidation ➜ microvesicular fatty infiltration of hepatocytes in the absence of significant inflammation or necrosis. ✲ may co-exist with pre-eclampsia ✲ ↑↑jaundice, ↑transaminases (<1000IU/L), derangement of coagulation, Hypoglycaemia, hepatic encephalopathy 213b Critical Care revision notes Dr.Sherif Badrawy
- 428. DD bw Acute fatty liver of pregnancy & HELLP 214a Critical Care revision notes Dr.Sherif Badrawy
- 429. marked elevations of bilirubin, hypoglycaemia and severe coagulopathy in AFLP 214b Critical Care revision notes Dr.Sherif Badrawy
- 430. DD bw Acute fatty liver of pregnancy & Cholestasis of pregnancy 215a Critical Care revision notes Dr.Sherif Badrawy
- 431. Cholestasis of pregnancy rarely causes a bilirubin level of >100µmol/L and does not cause a coagulopathy. 215b Critical Care revision notes Dr.Sherif Badrawy
- 432. Morphine properties 216a Critical Care revision notes Dr.Sherif Badrawy
- 433. ✲ undergoes extensive first pass metabolism ➜ only 25- 30% of an oral dose reaches the systemic circulation. ✲ metabolised in the liver to morphine 3-glucuronide and morphine 6-glucuronide; the latter has a potency over ten- fold greater than morphine. ✲ It inhibits neurotransmission in the CNS ✲ Peak effect takes 10-30 minutes from the time of IV injection ✲ Respiratory depression manifests predominantly as a fall in RR rather than tidal volume 216b Critical Care revision notes Dr.Sherif Badrawy
- 434. amiodarone properties 217a Critical Care revision notes Dr.Sherif Badrawy
- 435. ✲ It is 98% protein-bound. ✲ It does not require dose adjustment in renal failure. ✲ It has effect on heart rate even if the patient is in sinus rhythm.[causes a 15% reduction in heart rate of patients in sinus rhythm] ✲ It has a volume of distribution up to 70L/kg. ✲ It potentiates the effect of warfarin. 217b Critical Care revision notes Dr.Sherif Badrawy
- 436. The following ventilator graphic is best described by 218a Critical Care revision notes Dr.Sherif Badrawy
- 437. Volume-controlled ventilation with pressure support 218b Critical Care revision notes Dr.Sherif Badrawy
- 438. Facts about CVVH 219a Critical Care revision notes Dr.Sherif Badrawy
- 439. ✲ Replacement fluids usually contain lactate which is metabolised by the liver to bicarbonate, replacing the endogenous bicarbonate ion that is freely filtered during CVVH. ✲ Excessive infusion of lactate-buffered solution may cause metabolic alkalosis if liver is functioning normally ✲ Lactate-buffered solutions are usually avoided in liver failure ✲ Bicarbonate-buffered solutions have a short shelf-life ✲ Pre-dilution (adding replacement fluid prior to passage through the filter) ↓HCT of the filtered blood and may ↓filter clotting. 219b Critical Care revision notes Dr.Sherif Badrawy
- 440. CP of Persistent vegetative state. 220a Critical Care revision notes Dr.Sherif Badrawy
- 441. ✲ for over 1 month a patient who is 'wakeful without awareness'. ✲ eye opening and closing mirroring the sleep- wake cycle, HD stable & non-purposeful movements, no capacity to recognise or interact with the world. ✲ dt severe disruption to the cerebral cortex, but with intact brainstem and thalamic function a diagnostic rather than a prognostic label 220b Critical Care revision notes Dr.Sherif Badrawy
- 442. 'permanent vegetative state' 221a Critical Care revision notes Dr.Sherif Badrawy
- 443. Same CP after 12 months 221b Critical Care revision notes Dr.Sherif Badrawy
- 444. A minimally conscious state 222a Critical Care revision notes Dr.Sherif Badrawy
- 445. ✲ retain some degree of awareness ✲ may be able to obey a simple command and have limited interaction with their environment (e.g. social smiling, mood disturbance). 222b Critical Care revision notes Dr.Sherif Badrawy
- 446. Brainstem death 223a Critical Care revision notes Dr.Sherif Badrawy
- 447. ✲ loss of all cranial nerve reflexes, and loss of cardio-respiratory homeostasis. ✲ It is assumed that all higher mental function has ceased also; such patients are neither wakeful nor aware. 223b Critical Care revision notes Dr.Sherif Badrawy
- 448. locked-in syndrome 224a Critical Care revision notes Dr.Sherif Badrawy
- 449. ✲ Awareness is preserved ✲ caused by an insult at the 【level of the midbrain】, such as central pontine myelinosis or basilar artery thrombosis ✲ Quadriplegia and loss of function of the lower cranial nerves may leave the patient almost totally void of means of interaction with the world, despite full awareness. ✲ Vertical eye movements and blinking may be preserved 224b Critical Care revision notes Dr.Sherif Badrawy
- 450. The following drugs are recognised causes of hypokalaemia: 225a Critical Care revision notes Dr.Sherif Badrawy
- 451. a. Gentamicin.【✔】➜ dt renal potassium wasting b. Triamterene.【✘】➜ potassium-sparing diuretic c. Piperacillin.【✔】➜ dt renal potassium wasting d. Metolazone.【✔】➜ inhibits Na+ and Cl- absorption in the early DCT ➜ > K+ loss in the urine 225b Critical Care revision notes Dr.Sherif Badrawy
- 452. Regarding electrical injury: 226a Critical Care revision notes Dr.Sherif Badrawy
- 453. a. Skin resistance is 100 times greater when dry than when wet.【✔】➜ 100,000 Ohms when dry, but just 1000 Ohms when wet. b. Ventricular fibrillation occurs at a lower current than asystole.【✔】 c. A current of >50mA is required to cause microshock. 【✘】➜ can be caused by currents as small as 50mA if directly applied to the heart (e.g. saline filled catheter or pacing wire). d. A current of 1A is sufficient to cause deep burns and neurological injury.【✔】 226b Critical Care revision notes Dr.Sherif Badrawy
- 454. The following are accepted indications for permanent transvenous pacing: 227a Critical Care revision notes Dr.Sherif Badrawy
- 455. a. Symptomatic second degree heart block. 【✔】 b. Asymptomatic third degree heart block with documented pauses of >3 seconds.【✔】 c. Sinus node dysfunction with documented symptomatic bradycardia.【✔】 d. Asymptomatic third degree heart block with a heart rate <40bpm.【✔】 227b Critical Care revision notes Dr.Sherif Badrawy
- 456. a Pt s/p PEA cardiac arrest admitted to ICU, 28 minutes of CPR, five doses of IV epinephrine 1mg before ROSC, GCS of 3 and no pupillary reaction to light, but is making spontaneous respiratory effort. 228a Critical Care revision notes Dr.Sherif Badrawy
- 457. a. Her prognosis would be better if her arrest rhythm were ventricular fibrillation.【✔】➜ PEA/asystole, anoxic time >5 minutes and CPR time of >25 minutes all predict poor neurological outcome but not suitable as prognostic markers b. The length of her resuscitation time before return of spontaneous circulation is not compatible with survival.【✘】 c. If she has absent pupillary reflexes at 72h further treatment is futile.【✔】 d. Brain swelling on a CT scan accurately predicts poor outcome.【✘】 228b Critical Care revision notes Dr.Sherif Badrawy
- 458. a stab wound to the upper abdomen.small puncture wound under the left costal margin. BP is 80/40mmHg, HR is 130bpm and RR is 30 b/m.neck veins are distended. Chest X-ray shows no evidence of pneumothorax or haemothorax. ECG RBBB and T wave inversion in lead V1. FAST scan shows the presence of pericardial fluid. 229a Critical Care revision notes Dr.Sherif Badrawy
- 459. a. TTE is the diagnostic technique of choice when considering traumatic cardiac tamponade as a Dx ? 【✔】➜ fast and sensitive in the right hands b. A CT scan of the thorax should be performed immediately to confirm the suspected diagnosis.【✘】 c. Rapid fluid infusion should be avoided to prevent RHF. 【✘】 d. Removal of at least 300ml fluid is required to materially improve the clinical condition.【✘】➜ Removal of as little as 30ml fluid may give dramatic improvement 229b Critical Care revision notes Dr.Sherif Badrawy
- 460. RTA, ? seatbelt injury, HD unstable, +ve DPL, bilateral closed femoral fractures, OR for emergency laparotomy 230a Critical Care revision notes Dr.Sherif Badrawy
- 461. a. Definitive surgery must be performed before transfer to the intensive care unit.【✘】➜ coagulopathy, hypothermia and metabolic acidosis are great risks to the pt ↑by prolonged surgery. initial surgery should be damage control only b. Surgical stabilisation of the femoral fractures should be deferred until a later date.【✘】 c. Hollow viscus injury must be dealt with immediately.【✔】 d. The abdomen must be closed to prevent overwhelming sepsis.【✘】➜ Abdominal closure may provoke abdominal compartment syndrome which has ↑mortality 230b Critical Care revision notes Dr.Sherif Badrawy
- 462. What's damage control surgery ? 231a Critical Care revision notes Dr.Sherif Badrawy
- 463. packing a bleeding liver rather than formal resection, debridement of a pancreatic injury rather than pancreaticoduodenectomy, or resecting non-viable bowel and stapling the ends rather than attempting primary re- anastomosis. 231b Critical Care revision notes Dr.Sherif Badrawy
- 464. Regarding the use of mannitol for the treatment of raised intracranial pressure: 232a Critical Care revision notes Dr.Sherif Badrawy
- 465. a. A typical dose is 250-500ml of 20% mannitol as an IV bolus.【✔】 b. Intravascular volume depletion is a side effect.【✔】 c. It increases calculated plasma osmolality.【✘】 d. It has a rapid effect.【✔】 232b Critical Care revision notes Dr.Sherif Badrawy
- 466. Immediate management for a patient suspected of having anaphylaxis includes: 233a Critical Care revision notes Dr.Sherif Badrawy
- 467. a. High-flow oxygen.【✔】 b. Intravenous hydrocortisone 100-200mg. 【✘】➜ a 2ndry management but is not time-critical c. Epinephrine 0.5mg IV bolus.【✘】➜ Epinephrine should be given IM d. Lie the patient flat and raise their legs. 【✔】 233b Critical Care revision notes Dr.Sherif Badrawy
- 468. crushing central chest pain.ECG shows 2mm ST elevation in leads II, III and aVf. hypotensive, with a BP of 80/50mmHg and ↑JVP, lungs are clear to auscultation, ↑ST in lead V4R. 234a Critical Care revision notes Dr.Sherif Badrawy
- 469. a. A nitrate infusion should be started to relieve the chest pain.【✘】➜ may precipitate profound hypotension b. A fluid challenge of 500-1000ml should be given.【✔】 c. A posterior myocardial infarction is the likely diagnosis. 【✘】➜ right ventricular infarction [↑ST in lead V4R is highly sensitive and specific for RV infarction]. d. Thrombolysis is contraindicated.【✘】 234b Critical Care revision notes Dr.Sherif Badrawy
- 470. RTA, a liver laceration, During laparotomy extensive bleeding + 15-unit blood transfusion, MV, ICU, progressively worsening lung compliance and hypoxaemia (PaO2 9kPa [68mmHg] on 80% FIO2), over the next few hours. Chest X-ray shows widespread fluffy infiltrates; the PAOP is 15mmHg. 235a Critical Care revision notes Dr.Sherif Badrawy
- 471. a. The chest X-ray may be consistent with pulmonary oedema.【✔】 b. Diuretic therapy is indicated.【✘】 c. Corticosteroids are indicated.【✘】 d. Sufficient information is available to diagnose TRALI.【✔】 235b Critical Care revision notes Dr.Sherif Badrawy
- 472. Regarding the cerebral monitoring of patients with traumatic brain injury: 236a Critical Care revision notes Dr.Sherif Badrawy
- 473. a. Intracranial pressure is a good surrogate measure of cerebral metabolism.【✘】➜ a crude means of estimating cerebral metabolism and blood flow b. A jugular bulb SjvO2 of <50% has prognostic significance. 【✔】➜ > doubles mortality, A high mean SjvO2 (>75%) also carries a poor prognosis since dead brain tissue does not extract oxygen. c. The greater the SjvO2 the better the neurological outcome. 【✘】 d. A low arterio-jugular oxygen content difference (AJDO2) implies a poor outcome.【✔】 236b Critical Care revision notes Dr.Sherif Badrawy
- 474. ICP correlates with survival ? 237a Critical Care revision notes Dr.Sherif Badrawy
- 475. With severe head injury and ICP <20mmHg, expected mortality is 18%; this rises to 45% >20mmHg, 74% >40mmHg, and 100% >60mmHg 237b Critical Care revision notes Dr.Sherif Badrawy
- 476. Recombinant factor VIIa is licensed for use in the following scenarios: 238a Critical Care revision notes Dr.Sherif Badrawy
- 477. a. Second-line treatment of bleeding in major blunt trauma.【✘】 b. Emergency reversal of the anticoagulant effects of pentasaccarides (e.g. fondaparinux). 【✘】 c. Prophylaxis against bleeding for procedures in patients with liver disease.【✘】 d. Treatment of major obstetric haemorrhage. 【✘】 238b Critical Care revision notes Dr.Sherif Badrawy
- 478. Recombinant factor VIIa is licensed for treatment of ? 239a Critical Care revision notes Dr.Sherif Badrawy
- 479. ✲ bleeding in haemophiliacs with antibodies to Factor XIII or IX, and also for patients with acquired Factor VII deficiency ✲ surgical bleeding prophylaxis in these patient groups. ✲ used off-label for many indications including those listed in the question. 239b Critical Care revision notes Dr.Sherif Badrawy
- 480. Regarding the physiology of the patient with major burns: 240a Critical Care revision notes Dr.Sherif Badrawy
- 481. a. Cardiac output is increased in the immediate post-burn period.【✘】COP usu ↓immediately following injury dt sympathetic activation ➜ ↑systemic and pulmonary vascular resistance. b. A hypermetabolic state begins in the first 6 hours post-burn. 【✘】➜ A hypometabolic ('ebb') phase is usual in the first few days following a burn injury c. Acidic drugs have an increased free fraction in the plasma. 【✔】dt ↓Albumin levels. d. Sensitivity to non-depolarising muscle relaxants is increased.【✘】➜ reduced from around 1 week post-burn. 240b Critical Care revision notes Dr.Sherif Badrawy
- 482. Definition of A hypometabolic ('ebb') phase ? 241a Critical Care revision notes Dr.Sherif Badrawy
- 483. It' is usual in the first few days following a burn injury (or any major systemic insult), with the hypermetabolic phase supervening around 3 days post-burn. 241b Critical Care revision notes Dr.Sherif Badrawy
- 484. Regarding MRSA infection: 242a Critical Care revision notes Dr.Sherif Badrawy
- 485. a. Around half of all Staphylococcus aureus infections are methicillin resistant.【✔】 b. MRSA infection rates are inversely related to nursing staffing levels.【✔】 c. MRSA bacteraemia carries about a 15% mortality.【✔】 d. Active surveillance culture of patients is an effective means of reducing MRSA infection rates.【✔】➜ as most patients are colonised with rather than infected by MRSA 242b Critical Care revision notes Dr.Sherif Badrawy
- 486. PAOP overestimates LVEDP in the following conditions: 243a Critical Care revision notes Dr.Sherif Badrawy
- 487. a. Mitral stenosis.【✔】➜ dt ↑Left atrial pressure b. Mitral regurgitation.【✔】➜ dt ↑Left atrial pressure c. Massive pulmonary embolism.【✔】 d. Catheter tip outside West zone III.【✔】 243b Critical Care revision notes Dr.Sherif Badrawy
- 488. The following are effective methods of predicting an increase in cardiac output in response to a fluid challenge: 244a Critical Care revision notes Dr.Sherif Badrawy
- 489. a. Passive leg raising to 10° with oesophageal Doppler monitoring.【✘】➜ elevated to >30° ➜ ↑COP after 30s measured by oesophageal Doppler probe if the patient is preload-responsive. b. Pulmonary artery occlusion pressure.【✘】➜ a poor predictor of LVEDP & preload-responsivness. c. A large 'swing' on the arterial line trace in a mechanically ventilated patient.【✔】 d. A fall of 3mmHg in central venous pressure during unimpeded inspiration in a spontaneously breathing patient. 【✔】 244b Critical Care revision notes Dr.Sherif Badrawy
- 490. pulse pressure variation predicting an increase in cardiac output in response to a fluid challenge 245a Critical Care revision notes Dr.Sherif Badrawy
- 491. A pulse pressure variation of >13% ➜ a sensitive and specific predictor of ↑COP in response to a fluid bolus. 245b Critical Care revision notes Dr.Sherif Badrawy
- 492. 65-y, M, trapped in a burning building for 1 hour before extrication, ataxic and listless with a GCS of 12, RR of 30, HD stable, PaO2 44kPa (334mmHg), PaCO2 3.5kPa (26.6mmHg), SaO2 99% and lactate 10.5mmol/L, CoHb on co-oximetry is 10.4%. He has a brief seizure. 246a Critical Care revision notes Dr.Sherif Badrawy
- 493. a. This patient has severe carbon monoxide poisoning.【✘】➜ CoHb level of 10% is insufficient to explain a GCS of 12 and a seizure (smokers may have CoHb levels of up to 10% with no symptoms) b. A normal lactate would rule out cyanide poisoning completely. 【✔】 c. Treatment for suspected cyanide toxicity should not be delayed until laboratory blood cyanide levels are available.【✔】 d. Sodium nitroprusside may be appropriate treatment for this man.【✘】➜ sodium thiosulphate, hydroxycobalamin and sodium nitrite are used for Rx, Sodium nitroprusside is a cause of cyanide toxicity. 246b Critical Care revision notes Dr.Sherif Badrawy
- 494. The following are accepted indications for administering sedative medication to a mechanically ventilated intensive care patient: 247a Critical Care revision notes Dr.Sherif Badrawy
- 495. a. To manage alcohol withdrawal.【✔】 b. To reduce oxygen consumption.【✔】 c. To reduce the long-term incidence of psychological sequalae.【✘】 d. To provide amnesia covering periods of neuromuscular blockade.【✔】 247b Critical Care revision notes Dr.Sherif Badrawy
- 496. A 67-year-old lady with chronic bronchitis and emphysema is ventilated on the ICU and has the following capnograph trace: 248a Critical Care revision notes Dr.Sherif Badrawy
- 497. a.The slope of phase IIissteeper than normal.【✘】➜ Phase IIIisthe plateau phase, which in thiscase hasa steeper slope than normal b.The abnormalwaveform isexplained by late emptying of alveoliwith higher V/Q ratios.【✘】➜ low V/Q ratio empty later in expiration than those that are wellventilated. c.The end-tidalCO2 reflectsalveoliwith the largest time constants.【✔】 d.Endobronchialintubation doesnot produce thispicture.【✔】 248b Critical Care revision notes Dr.Sherif Badrawy
- 498. The following are true of thrombolytic therapy for pulmonary embolism: 249a Critical Care revision notes Dr.Sherif Badrawy
- 499. a. There is a 15% risk of clinically significant bleeding.【✘】➜ 3% with TPA. b. The S1Q3T3 pattern on the ECG is an indication for thrombolysis.【✘】 c. Right ventricular function is often improved. 【✔】 d. Systemic hypotension is an absolute contraindication to thrombolysis.【✘】 249b Critical Care revision notes Dr.Sherif Badrawy
- 500. Regarding delirium in the intensive care patient: 250a Critical Care revision notes Dr.Sherif Badrawy
- 501. a. It is an independent predictor of ↑mortality.【✔】 b. It is experienced by 30-40% of MV patients.【✘】➜ 80% of MV patients. c. The Confusion Assessment Method for ICU patients (CAM-ICU) delirium assessment tool can be used in patients unable to communicate verbally.【✔】 d. An acute change in mental state is sufficient to make a Dx of ICU delirium using the CAM-ICU system.【✘】 250b Critical Care revision notes Dr.Sherif Badrawy
- 502. Types of Delirium in the ICU 251a Critical Care revision notes Dr.Sherif Badrawy
- 503. recognised in agitated, combative patients or hypoactive Delirium ➜ > common, under-recognised and possibly associated with worse outcomes. 251b Critical Care revision notes Dr.Sherif Badrawy
- 504. Definition of Delirium in the ICU 252a Critical Care revision notes Dr.Sherif Badrawy
- 505. acute change or fluctuation in the course of a patient's mental status, plus inattention and either disorganised thinking or an altered level of consciousness 252b Critical Care revision notes Dr.Sherif Badrawy
- 506. Concerning Doppler ultrasound: 253a Critical Care revision notes Dr.Sherif Badrawy
- 507. a. The Doppler effect states that observed frequency ↑as the source moves closer to the observer.【✔】 b. In colour flow Doppler, a red colour indicates arterial blood flow.【✘】➜ represent direction of a given jet c. For blood flow measurement the probe should ideally be perpendicular to the direction of flow.【✘】➜ should be as near parallel to the direction of blood flow as possible d. Blood flow velocity is proportional to the cosine of q (theta) according to the Doppler equation.【✔】 253b Critical Care revision notes Dr.Sherif Badrawy
- 508. 44-y, F, acute pancreatitis, ALI, VAP after 8 days, antibiotics started. 254a Critical Care revision notes Dr.Sherif Badrawy
- 509. a. Dx should be confirmed microbiologically prior to antibiotic treatment.【✘】 b. Tracheobronchial aspiration has a high negative predictive value.【✔】➜ provided empirical antibiotics have not been started c. Quantitative cultures (e.g. protected specimen brushings) have a high specificity for VAP.【✘】➜ not very specific d. Levofloxacin is a suitable antibiotic if empirical treatment is warranted.【✘】 254b Critical Care revision notes Dr.Sherif Badrawy
- 510. Late onset VAP ? 255a Critical Care revision notes Dr.Sherif Badrawy
- 511. onset at least 5 days after hospital admission. 255b Critical Care revision notes Dr.Sherif Badrawy
- 512. Regarding the measurement of lung compliance in MV patients: 256a Critical Care revision notes Dr.Sherif Badrawy
- 513. a. Static compliance calculation requires knowledge of plateau pressure and PEEP.【✔】 b. Dynamic compliance calculation requires knowledge of plateau pressure and PEEP.【✘】 c. Static compliance is greater than dynamic compliance for the same patient.【✔】 d. Bronchospasm has more effect on dynamic compliance than static.【✔】 256b Critical Care revision notes Dr.Sherif Badrawy
- 514. In a patient with known WPW syndrome, who presents with fast AF, appropriate pharmacotherapy includes: 257a Critical Care revision notes Dr.Sherif Badrawy
- 515. a. Procainamide.【✔】 b. Digoxin.【✘】 c. Verapamil.【✘】 d. Flecainide.【✔】 257b Critical Care revision notes Dr.Sherif Badrawy
- 516. 72-y, F, recent onset fast AF, CCU admission, severe abdominal pain and looks generally unwell, abdomen is soft and minimally tender, no guarding, ABG profound metabolic acidaemia. Appropriate initial steps include : 258a Critical Care revision notes Dr.Sherif Badrawy
- 517. a. Obtaining a surgical opinion as this lady may need an urgent laparotomy.【✔】➜ ?acute mesenteric ischaemia b. Give intravenous morphine and observe overnight while fluid resuscitating.【✘】 c. Urgent abdominal ultrasound.【✘】➜ Mesenteric angiography is the investigation of choice,but should not delay laparotomy if clinical suspicion is high, since operative delay ↑mortality. d. Thrombolysis.【✘】 258b Critical Care revision notes Dr.Sherif Badrawy
- 518. The following physiological observations are commonly seen in patients with an acute exacerbation of COPD: 259a Critical Care revision notes Dr.Sherif Badrawy
- 519. a. Reduced respiratory compliance.【✔】 b. Increased pulmonary vascular resistance.【✔】 c. Increased resistive load.【✔】 d. Increased mechanical efficiency of the diaphragm.【✘】 259b Critical Care revision notes Dr.Sherif Badrawy
- 520. 23-y, F, sudden SOB, Hx of asthma on salbutamol inhaler, unable to talk in sentences, HR 120bpm (sinus tachycardia).SaO2 100% on NRBM 15L/min O2, flow-volume loop 260a Critical Care revision notes Dr.Sherif Badrawy
- 521. a. The inspiratory limb of the flow-volume loop is normal.【✘】 b. The flow-volume loop is consistent with bronchospasm.【✘】 c. Steroids and bronchodilators should be administered.【✘】 d. Awake fibreoptic intubation is indicated.【✘】 260b Critical Care revision notes Dr.Sherif Badrawy
- 522. Significance of this flow-volume loop 261a Critical Care revision notes Dr.Sherif Badrawy
- 523. ✵ vocalcord dysfunction (VCD) inspiratory limb isflattened but the expiratory limb isnormalwith no 'dip' suggestive of bronchospasm, ✵ commonly mistaken for acute severe asthma, leading to unnecessary intubation and ventilation, ✵ MC in young adult femalesand hasan association with psychiatricdisease. ✵ Dx isconfirmed by indirect laryngoscopy ➜ complete adduction of the anterio 2/3 of VCsduring inspiration with a 'glotticchink' posteriorly. ✵ Rx isSpeech therapy and/or psychotherapy 261b Critical Care revision notes Dr.Sherif Badrawy
- 524. Regarding the use of synchronised DC cardioversion for new onset atrial fibrillation in ICU surgical patients: 262a Critical Care revision notes Dr.Sherif Badrawy
- 525. a. Sinus rhythm is initially restored in over 95% of cases.【✘】➜ just 35% b. Successful DC cardioversion of new onset AF is less likely in medical than surgical patients.【✘】 c. Most successfully cardioverted patients maintain sinus rhythm in the first 48 hours.【✘】 d. Successful cardioversion is unlikely if the first two shocks are unsuccessful.【✔】 262b Critical Care revision notes Dr.Sherif Badrawy
- 526. The following favour a strategy of primary angioplasty over thrombolysis in patients with an acute STEMI: 263a Critical Care revision notes Dr.Sherif Badrawy
- 527. a. Cardiogenic shock.【✔】 b. Late presentation (onset of symptoms >3h ago).【✔】 c. 'Door-to-balloon time' likely to exceed 90 minutes.【✘】 d. Diagnosis of STEMI in doubt.【✔】 263b Critical Care revision notes Dr.Sherif Badrawy
- 528. 44-y,M, dilated cardiomyopathy, cardiogenic shock while on the waiting list for a heart transplant, refractory to maximal medical Rx, left ventricular assist device (LVAD) is considered. 264a Critical Care revision notes Dr.Sherif Badrawy
- 529. a. Blood flow produced by an LVAD may be pulsatile or non-pulsatile.【✔】 b. The LVAD takes blood from the RV or vena cava and pumps it into the aorta.【✘】 c. An LVAD will increase COP much > IABCP. 【✔】 d. This patient could be maintained on a LVAD for several months.【✔】typically used as a bridge to transplantation in those with a HF 264b Critical Care revision notes Dr.Sherif Badrawy
- 530. 58-y ,M, dense left hemiparesis, suddenly 2 hours ago. BP is 175/105mmHg, CT brain no evidence of haemorrhage. Thrombolysis is considered. 265a Critical Care revision notes Dr.Sherif Badrawy
- 531. a. Thrombolysis reduces death and dependency rates in carefully selected stroke patients.【✔】 b. Thrombolysis must be given within 12 hours of presentation for the greatest benefit.【✘】 c. Haemorrhagic transformation is not significantly greater with thrombolysis than placebo.【✘】 d. There is no CI to thrombolytic therapy from the information given.【✔】 265b Critical Care revision notes Dr.Sherif Badrawy
- 532. 28-y, acute confusion, headache for the past 2 days, low grade fever, disorientated and has a mild left-sided hemiparesis, no Hx of recent foreign travel, examination is unremarkable except for the presence of a cold sore 266a Critical Care revision notes Dr.Sherif Badrawy
- 533. a. Lumbar puncture is the initial investigation of choice.【✘】Altered sensorium and focal neurological deficit argue against Dx of viral meningitis. b. Viral meningitis is the most likely diagnosis.【✘】 c. Empirical acyclovir is mandatory.【✔】 d. CT brain scan is not a useful investigation in this case.【✘】➜ useful, rules out other pathologies 266b Critical Care revision notes Dr.Sherif Badrawy
- 534. mortality of Untreated Herpes simplex encephalitis 267a Critical Care revision notes Dr.Sherif Badrawy
- 535. ✵ 70%, mandating immediate intravenous acyclovir on suspicion of the diagnosis. ✵ Even with treatment, mortality is 20-30% 267b Critical Care revision notes Dr.Sherif Badrawy
- 536. Regarding ARF on the ICU: 268a Critical Care revision notes Dr.Sherif Badrawy
- 537. a. Hypovolaemia is the commonest ppt factor in pts with established ARF.【✘】➜ sepsis was the commonest factor b. Mortality is not significantly different between ICU patients with and without ARF.【✘】 c. The prevalence of ARF requiring RRT in ICU pts is about 45%.【✘】 d. The vast majority (86%) of ARF survivors are dialysis- independent on hospital discharge.【✔】 268b Critical Care revision notes Dr.Sherif Badrawy
- 538. Regarding stress ulceration in ICU patients: 269a Critical Care revision notes Dr.Sherif Badrawy
- 539. a. Stress-related mucosal damage usually takes 3-5 days to develop.【✘】➜ evident after 24 hours. b. The incidence of clinically important gastrointestinal bleeding in ICU patients is 1.5%.【✔】 c. Bleeding from stress ulcers is associated with significantly increased ICU mortality.【✔】 d. Acid suppression is an effective intervention.【✔】 269b Critical Care revision notes Dr.Sherif Badrawy
- 540. 35-y, M, RTA, emergency laparotomy, on MV in ICU, jaundiced with a bilirubin of 62mmol/L, The following would support a diagnosis of 'ICU jaundice': 270a Critical Care revision notes Dr.Sherif Badrawy
- 541. a. Dilatation of the biliary tree on ultrasound. 【✘】 b. Grade III or IV encephalopathy.【✘】 c. An AST level of 1500U/L.【✘】➜ 'ICU jaundice' = ↑bilirubin +normal liver enzymes, ↑AST level would raise the possibility of ischaemic hepatitis. d. Intrahepatic cholestasis on liver histology. 【✔】 270b Critical Care revision notes Dr.Sherif Badrawy
- 542. The following are common findings in a patient with profound myxoedema: 271a Critical Care revision notes Dr.Sherif Badrawy
- 543. a. Coma.【✘】➜ few patients are comatose. Altered mentation, depression and slowing of thought are common b. Hyponatraemia.【✔】➜ c. Elevated creatine kinase.【✔】➜ dt thyroid myopathy d. Low/undetectable thyrotrophin.【✘】➜ Thyrotrophin (TSH) is usually very high to drive thyroid hormone production, except in rare cases of pituitary hypothyroidism 271b Critical Care revision notes Dr.Sherif Badrawy
- 544. Regarding the detection of impaired renal function in critically ill patients: 272a Critical Care revision notes Dr.Sherif Badrawy
- 545. a. The Cockroft-Gault formula requires a urinary creatinine value.【✘】 b. A normal serum creatinine measurement indicates normal renal function in critically ill patients.【✘】➜ muscle mass is reduced in this population, even with poor renal clearance, creatinine is not elevated above the normal range c. Measurement of the GFR requires a 24-hour urine collection.【✘】 d. Calculated GFR correlates well with measured GFR. 【✘】 272b Critical Care revision notes Dr.Sherif Badrawy
- 546. Regarding tight glycaemic control in critically ill patients: 273a Critical Care revision notes Dr.Sherif Badrawy
- 547. a. Maintenance of normoglycaemia is of no benefit in medical ICU patients.【✘】➜ there's mortality benefit b. Beneficial effects of tight glucose control in surgical patients relate to the dose of insulin used rather than the glucose levels per se.【✘】 c. Patients with a longer ICU stay (>5 days) benefit the most.【✔】 d. Hypoglycaemic episodes are more likely with enteral than with parenteral feeding.【✔】 273b Critical Care revision notes Dr.Sherif Badrawy
- 548. The following are elements of the 6-hour sepsis resuscitation care bundle as advocated by the Surviving Sepsis Campaign group: [two 'sepsis care bundles' to be implemented within 6 and 24 hours of the recognition of a septic patient] 274a Critical Care revision notes Dr.Sherif Badrawy
- 549. a. Serum lactate measurement.【✔】 b. Administration of recombinant human activated protein C.【✘】 c. Achievement of a central venous oxygen saturation of >70%.【✔】 d. Administration of broad spectrum antibiotics within the first 3 hours.【✘】➜ within 1 hour 274b Critical Care revision notes Dr.Sherif Badrawy
- 550. 46-y, F, suspected CAP, temperature 38.3°C, BP 85/40, RR 24, HR 105, CXR consolidation in the left lower zone, green sputum, Initial blood cultures are negative, ABG (on 60% oxygen via high-flow mask) pH 7.32, PaCO2 3.8kPa (28.9mmHg), PaO2 8.9kPa (67.6mmHg), base excess -7.3mmol/L and lactate 3.4mmol/L (30mg/dL). A fluid challenge is given. 275a Critical Care revision notes Dr.Sherif Badrawy
- 551. a. The SIRS is present.【✔】 b. Sepsis cannot be diagnosed without a positive blood culture.【✘】 c. Severe sepsis is present.【✔】 d. Septic shock is present.【✘】 275b Critical Care revision notes Dr.Sherif Badrawy
- 552. Regarding the use of HFOV in adult patients with the ARDS compared with conventional MV: 276a Critical Care revision notes Dr.Sherif Badrawy
- 553. a. Mean airway pressure is usually higher.【✔】➜ Peak Aw P is reduced compared with conventional ventilation, but end-expiratory lung volume is higher and mean Aw P is usually higher. b. Early improvement in oxygenation is typical.【✔】➜ not sustained beyond the first 24 h c. Mortality is significantly reduced in surgical patients. 【✘】 d. Less arterial CO2 is eliminated.【✔】 276b Critical Care revision notes Dr.Sherif Badrawy
- 554. Regarding amniotic fluid embolism: 277a Critical Care revision notes Dr.Sherif Badrawy
- 555. a. Hypoxia is most commonly due to bronchospasm. 【✘】➜ dt V/Q mismatch, pulmonary oedema dt LV dysfunction , or bronchospasm b. The diagnosis should be questioned in the absence of hypotension.【✔】 c. DIC occurs in 5-10% of patients.【✘】➜ occurs in 83% of patients d. The majority of survivors have a permanent neurological deficit.【✔】 277b Critical Care revision notes Dr.Sherif Badrawy
- 556. Regarding the pharmacology of NSAIDs : 278a Critical Care revision notes Dr.Sherif Badrawy
- 557. a. Bronchospasm may be ppt by ↑bradykinin production.【✘】 b. ↓thromboxane A2 synthesis ↓platelet aggregation. 【✔】 c. NSAIDs are excreted unchanged in the urine.【✘】 d. NSAIDs have ↓protein binding and a ↑volume of distribution.【✘】➜ highly protein bound and may displace warfarin from its albumin binding site,↓volume of distribution. 278b Critical Care revision notes Dr.Sherif Badrawy
- 558. Regarding amiodarone toxicity: 279a Critical Care revision notes Dr.Sherif Badrawy
- 559. a. Corneal microdeposits are rare.【✘】➜ MC complication of amiodarone, occurring in over 90% of patients b. Pulmonary toxicity does not occur with short-term therapy.【✘】➜ may occur acutely in the ICU patient, immunologically-mediated hypersensitivity, > common in pts with pre-existing lung disease & in Pts undergoing cardiac surgery c. Elevation of hepatic transaminases is common.【✔】 d. Neurotoxicity is a dose-related problem.【✔】 279b Critical Care revision notes Dr.Sherif Badrawy
- 560. Regarding the use of lithium dilution to measure cardiac output in the ICU: 280a Critical Care revision notes Dr.Sherif Badrawy
- 561. a. It cannot be used in patients taking lithium carbonate.【✔】➜ alters the background concentration in the plasma and causes an overestimation of COP. b. It cannot be used in patients who have previously received atracurium.【✘】 c. Anaemia affects the measurement.【✔】 d. Central venous access is not required. 【✔】➜ central or peripheral line 280b Critical Care revision notes Dr.Sherif Badrawy
- 562. A patient on the ICU develops ARF ➜ haemofiltration. The following measures will increase the efficiency of solute clearance: 281a Critical Care revision notes Dr.Sherif Badrawy
- 563. a. Increasing blood flow rate.【✔】 b. Pre-dilution instead of post-dilution. 【✘】 c. Increasing the surface area of the filter. 【✔】 d. Using arteriovenous rather than venovenous renal replacement.【✘】 281b Critical Care revision notes Dr.Sherif Badrawy
- 564. The following factors are associated with a greater likelihood of a critical incident occurring during a patient's care on the ICU: 282a Critical Care revision notes Dr.Sherif Badrawy
- 565. a. High severity of illness.【✔】 b. Long stay.【✔】 c. Higher level of care.【✔】 d. Renal replacement therapy.【✔】 282b Critical Care revision notes Dr.Sherif Badrawy
- 566. 35-y, F, insulin overdose, ICU, MV, no sedation for the last month but shows no interaction or apparent awareness despite periods of eye opening, A CT brain scan and metabolic screening show no reversible features. A diagnosis of persistent vegetative state is considered.rule out this diagnosis by: 283a Critical Care revision notes Dr.Sherif Badrawy
- 567. a. Intact sleep-wake cycle.【✘】 b. Bowel and bladder incontinence.【✘】 c. Spontaneous movements.【✘】 d. Social smiling.【✔】 283b Critical Care revision notes Dr.Sherif Badrawy
- 568. Indications of steroids in Rx hypercalcaemia ? 284a Critical Care revision notes Dr.Sherif Badrawy
- 569. Steroids are ineffective in hypercalcaemia of malignancy but are effective in granulomatous causes such as sarcoidosis. 284b Critical Care revision notes Dr.Sherif Badrawy
- 570. severe pre-eclampsia, In the ICU 1 day post partum with confusion, weakness, flushing and bradyarrhythmia , ECG shows prolongation of the PR and QT intervals. 285a Critical Care revision notes Dr.Sherif Badrawy
- 571. Hypermagnesaemia flaccid paralysis reflect a very high serum magnesium level of >5mmol/L 285b Critical Care revision notes Dr.Sherif Badrawy
- 572. MCC of Hypermagnesaemia 286a Critical Care revision notes Dr.Sherif Badrawy
- 573. excessive iatrogenic administration 286b Critical Care revision notes Dr.Sherif Badrawy
- 574. consequences of therapeutic (32-34°C) hypothermia 287a Critical Care revision notes Dr.Sherif Badrawy
- 575. ✽ A 7% fall in cerebral metabolic rate for each 1°C fall in temperature, decreasing intracranial blood volume and improving CPP. ✽ ↓reabsorption of solutes by the kidney. 'cold diuresis' ✽ Hyperglycaemia dt ↓insulin secretion from the pancreas ✽ ↑incidence of VAP. ✽ Prolonged PT. 287b Critical Care revision notes Dr.Sherif Badrawy
- 576. In trauma pt, The primary survey should include the following points EXCEPT: a. Use of airway adjuncts if indicated. b. Control of external haemorrhage. c. Cervical spine assessment. d. Pupillary light reflex determination. e. Percussion of the chest. 288a Critical Care revision notes Dr.Sherif Badrawy
- 577. c. Cervical spine assessment. Although the cervical spine should be maintained in neutral alignment throughout the primary survey, a cervical spine fracture is not immediately life-threatening and should be assessed radiographically and clinically as part of the secondary survey. 288b Critical Care revision notes Dr.Sherif Badrawy
- 578. In penetrating abdominal injury, Peritonitis in a HD stable patient is an indication for laparotomy ? 289a Critical Care revision notes Dr.Sherif Badrawy
- 579. Yes, Peritonitis may reflect leakage of digestive tract contents from a hollow viscus and is an indication for laparotomy. 289b Critical Care revision notes Dr.Sherif Badrawy
- 580. The most commonly injured organ in penetrating stab wounds is ? 290a Critical Care revision notes Dr.Sherif Badrawy
- 581. the liver (40%), small bowel (30%), diaphragm (20%) and colon (15%). 290b Critical Care revision notes Dr.Sherif Badrawy
- 582. A negative FAST scan has a high negative predictive value for injury requiring laparotomy ? 291a Critical Care revision notes Dr.Sherif Badrawy
- 583. No, negative FAST scan has a negative predictive value for laparotomy of only 60%; it may miss free intraperitoneal blood, and will not reliably identify injuries to structures such as the diaphragm and bowel. 291b Critical Care revision notes Dr.Sherif Badrawy
- 584. features of the abdominal compartment syndrome? [a combination of intra-abdominal hypertension and end-organ dysfunction, with reversal of this organ dysfunction on relief of the pressure]. 292a Critical Care revision notes Dr.Sherif Badrawy
- 585. ✯ occurs with pressures > 20mmHg ✯ ↑pulmonary vascular resistance dt hypoxic VC & ↑intrathoracic pressures ✯ ↓pulmonary artery occlusion pressure. ✯ ↓COP dt compression of venous return from the IVC and hepatic portal vein. ✯ Oliguria. ✯ ↑intracranial pressure. 292b Critical Care revision notes Dr.Sherif Badrawy
- 586. The presence of mildly raised CSF protein, normal CSF glucose and oligoclonal bands, pseudobulbar palsy (including dysarthria) and internuclear ophthalmoplegia manifesting as occulomotor signs. is strongly supportive of a diagnosis of ? 293a Critical Care revision notes Dr.Sherif Badrawy
- 587. multiple sclerosis (MS). 293b Critical Care revision notes Dr.Sherif Badrawy
- 588. Oligoclonal bands are ? 294a Critical Care revision notes Dr.Sherif Badrawy
- 589. distinct electrophoretic patterns dt ↑IgG by plasma cells and are present in the CSF of 85% of patients with multiple sclerosis. Also present in SLE, neurosarcoidosis, CNS lymphoma and subacute sclerosing panencephalitis 294b Critical Care revision notes Dr.Sherif Badrawy
- 590. Srquence of drugs given in status epilepticus ? 295a Critical Care revision notes Dr.Sherif Badrawy
- 591. ✯ prehospital care➜ rectal diazepam or buccal midazolam ➜ hospital care➜ lorazepam ➜ repeated after 10-20 minutes ➜ phenytoin or phosphenytoin ➜ Phenobarbitone ➜ refractory cases ➜ induction of general anaesthesia ➜ propofol, midazolam or thiopentone. 295b Critical Care revision notes Dr.Sherif Badrawy
- 592. management of status epilepticus in adults ? 296a Critical Care revision notes Dr.Sherif Badrawy
- 593. ✯ Buccal midazolam 10mg is an alternative to rectal diazepam. ✯ Phenytoin should be given at a rate < 50mg/minute can ppt arrhythmias if given faster.(or phosphenytoin at a dose of 15-20mg phenytoin equivalents/kg). ✯ Lorazepam is preferred to diazepam if intravenous access is present. ✯ Ideally serum levels should be measured to guide thiopentone infusion. ✯ 'Thiopentone coma' should be titrated to burst suppression on the EEG. 296b Critical Care revision notes Dr.Sherif Badrawy
- 594. toxic megacolon CP ? 297a Critical Care revision notes Dr.Sherif Badrawy
- 595. ✯ Enteral loss of potassium and fluid ➜ volume depletion hypokalaemia and a metabolic alkalosis which carries a poor prognosis ✯ Anaemia dt blood loss per rectum with a lowered haematocrit ✯ Leukocytosis with left shift ➜ as a component of the inflammatory response 297b Critical Care revision notes Dr.Sherif Badrawy
- 596. ICP monitoring in patients with traumatic brain injury 298a Critical Care revision notes Dr.Sherif Badrawy
- 597. ✯ Outcome is improved in patients who respond to ICP- lowering therapies ✯ Haematoma requiring surgical evacuation occurs in 0.5% of cases of ICP measurement, most commonly with ventriculostomy catheter insertion ✯ A normal CT brain scan is associated with a reduced risk of raised ICP in comatose TBI pts, but is not highly sensitive; the incidence was 13% in one series (vs.~60% with an abnormal CT). 298b Critical Care revision notes Dr.Sherif Badrawy
- 598. Regarding unstable fractures of the pelvis 299a Critical Care revision notes Dr.Sherif Badrawy
- 599. ✯ The commonest cause of serious pelvic injury is MVC, followed by falls from height. ✯ Mortality 30%-45%, bleeding being the major cause. ✯ Serious pelvic injury is correlated with intra-abdominal injury which should be actively excluded. ✯ Arterial embolisation may be indicated in selected cases; although most pelvic bleeding is venous, arterial embolisation may stop arterial bleeding, while fixation of the pelvic ring allows venous bleeding to tamponade itself 299b Critical Care revision notes Dr.Sherif Badrawy
- 600. minute volume in the anaesthetic management of a patient with major burns 300a Critical Care revision notes Dr.Sherif Badrawy
- 601. ✯ A high ventilator minute volume will be required dt ↑CO2 production will be a feature of the hypermetabolic phase, and therefore minute volume will need to be ↑if normocapnia is to be maintained. 300b Critical Care revision notes Dr.Sherif Badrawy
- 602. Fick principle in the calculation of cardiac output formula 301a Critical Care revision notes Dr.Sherif Badrawy
- 603. ✯ Cardiac output (Q) = VO2/Arterial O2 content - mixed venous O2 content ✯ CaO2 [Arterial O2 content] = 1.39 x [Hb] x (SaO2/100) + 0.023 x PaO2 (Hb in g/dL, PaO2 in kPa) 301b Critical Care revision notes Dr.Sherif Badrawy
- 604. 42-y, F, admitted to the ICU generally unwell 1 week following abdominal surgery.oliguric, hypotensive (BP 80/35mmHg) and tachycardic (HR 130bpm).oesophageal Doppler probe, flow time (corrected) 380ms, peak velocity 110cm/s, stroke volume 90ml, would you give IV fluid ? 302a Critical Care revision notes Dr.Sherif Badrawy
- 605. ✯ This patient is in shock, oesophageal Doppler shows a raised flow time corrected (FTc), reflecting low SVR. ✯ Typical value for FTc is 330-360 ms ✯ A supra-normal FTc (>340ms) does not necessarily mean the patient is adequately volume loaded ✯ A fluid challenge should be given and the stroke volume response assessed ✯ Peak velocity (reflecting contractility) is at the upper end of normal for this age (there is a linear decline from ≅120cm/s at 20 years old to ≅60cm/s at 90 years old ✯ In massive pulmonary embolism COP is↓dt impaired LV filling, and FTc would be low dt compensatory systemic VC to maintain BP. 302b Critical Care revision notes Dr.Sherif Badrawy
- 606. Regarding electrical temperature measurement 303a Critical Care revision notes Dr.Sherif Badrawy
- 607. ✯ The resistance of a platinum thermometer increases linearly with increasing temperature. ✯ A thermocouple can measure temperatures up to 1600°C. ✯ A radiation thermometer utilises Planck's law. ✯ A thermistor is a type of semiconductor 303b Critical Care revision notes Dr.Sherif Badrawy
- 608. 78-y,F, MV on the ICU with diffuse brain injury following a fall, significant renal impairment, sick sinus syndrome for which he is awaiting implantation of a permanent pacemaker, proven allergy to egg protein. Which of the following sedative agents would be most suitable a. Midazolam. b. Propofol. c. Etomidate. d. Clonidine. e. Ketamine. 304a Critical Care revision notes Dr.Sherif Badrawy
- 609. ✯ Midazolam ➜ Not suitable, active metabolite accumulates in renal impairment, especially in the elderly. ✯ Etomidate ➜ Not suitable, cause adrenal suppression and should not be used as maintenance sedation in the ICU. ✯ Clonidine ➜ Not suitable,α-2 agonist with sedative and analgesic-sparing properties. an attractive agent dt lack of respiratory depression, it can cause significant hypotension and bradycardia, a poor choice given this patient's cardiac history. ✯ Ketamine ➜ Not suitable,↑ICP, CI in head injury Rx. ✯ Propofol ➜ suitable, Pts with anaphylactic egg allergy react to one of three egg proteins (ovoalbumin, ovomucoid and conalbumin) whereas the propofol lipid vehicle contains purified egg phosphatide (lecithin) which is not known to be allergenic. 304b Critical Care revision notes Dr.Sherif Badrawy
- 610. 28-y, F, elective femoral hernia repair is anaesthetised with propofol, atracurium and Sevoflurane, ETT, 30 minutes into the procedure, progressively more difficult to ventilate. Her BP falls to 60/40mmHg, her HR is 150bpm and widespread bronchospasm is heard on auscultation, Dx ? 305a Critical Care revision notes Dr.Sherif Badrawy
- 611. ✯ Latex allergy. ✯ an IgE mediated anaphylaxis, Symptoms, usually occur some time (20-30 mins) following exposure, unlike drug anaphylaxis which occurs immediately following intravenous injections. It is more common in those routinely exposed to latex (e.g. healthcare workers) and those with a variety of food allergies including avocado, chestnut and kiwi. ✯ Patients with spina bifida and cerebral palsy probably dt repeated urinary catheterisation. ✯ Rx same as that for drug anaphylaxis + all latex products should be removed. 305b Critical Care revision notes Dr.Sherif Badrawy
- 612. Rx of ICU delirium 306a Critical Care revision notes Dr.Sherif Badrawy
- 613. ✯ Pharmacological IV haloperidol 0.5-10mg. ✯ Benzodiazepines are not considered first-line therapy unless to treat a benzodiazepine or alcohol withdrawal delirium ✯ Non-pharmacological maintenance of a normal sleep- wake cycle as far as possible (lights off at night), orientation of the patient (clock on the wall), ensuring spectacles and hearing aids are available if required, and eliminating organic drivers of delirium such as pain and hypoxia. 306b Critical Care revision notes Dr.Sherif Badrawy
- 614. Lundberg waves for ICP monitoring 307a Critical Care revision notes Dr.Sherif Badrawy
- 615. ✯ three types of abnormal ICP waves found in cases of ↑CP ✯ occur over a period of time and should not be confused with the three peaks of the normal intracranial pressure waveform seen in normal individuals and related to the arterial waveform. 307b Critical Care revision notes Dr.Sherif Badrawy
- 616. the three peaks of the normal intracranial pressure waveform 308a Critical Care revision notes Dr.Sherif Badrawy
- 617. 308b Critical Care revision notes Dr.Sherif Badrawy
- 618. P1 WAVE of the normal intracranial pressure waveform 309a Critical Care revision notes Dr.Sherif Badrawy
- 619. 309b Critical Care revision notes Dr.Sherif Badrawy
- 620. P2 & P3 WAVES of the normal intracranial pressure waveform 310a Critical Care revision notes Dr.Sherif Badrawy
- 621. 310b Critical Care revision notes Dr.Sherif Badrawy
- 622. Lundberg waves for ICP monitoring ➜ Type A waves 311a Critical Care revision notes Dr.Sherif Badrawy
- 623. ✯ Type A (plateau waves) are largest in amplitude (50-100mmHg above baseline ICP) and duration (5-20 minutes). ✯ cerebral vasodilatation in response to critically low cerebral perfusion ➜ This dilatation ➜ ↑ICP, compromising cerebral perfusion. 311b Critical Care revision notes Dr.Sherif Badrawy
- 624. Lundberg waves for ICP monitoring ➜ Type B waves 312a Critical Care revision notes Dr.Sherif Badrawy
- 625. ✯ an amplitude of up to 50mmHg, and a duration of <2 minutes. ✯ reflect reduced intracranial complianc 312b Critical Care revision notes Dr.Sherif Badrawy
- 626. Lundberg waves for ICP monitoring ➜ Type C waves 313a Critical Care revision notes Dr.Sherif Badrawy
- 627. ✯ a duration of approximately 5 minutes and an amplitude of <20mmHg. ✯ can be pathological can also be seen in normal individuals and are of less clinical significance than type A and B waves 313b Critical Care revision notes Dr.Sherif Badrawy
- 628. The normal D-dimer excludes a diagnosis of pulmonary embolism, True ? 314a Critical Care revision notes Dr.Sherif Badrawy
- 629. No, A positive D-dimer result is 96-98% sensitive, meaning that false negatives are possible though rare, and further investigation should be pursued if clinical suspicion is high. 314b Critical Care revision notes Dr.Sherif Badrawy
- 630. Etiology of Malignant hyperthermia 315a Critical Care revision notes Dr.Sherif Badrawy
- 631. ✯ a rare disorder of calcium homeostasis in skeletal muscle caused by a defect in the ryanodine receptor. ✯ Suxamethonium and volatile anaesthetic ➜ trigger ↑↑ release of calcium from sarcoplasmic reticulum ➜ generalised excessive muscle contraction in susceptible individuals. 315b Critical Care revision notes Dr.Sherif Badrawy
- 632. physiology of proning 316a Critical Care revision notes Dr.Sherif Badrawy
- 633. ✯ Perfusion is thought to remain largely dorsal in the prone position (i.e. not greatly affected by gravity). ✯ Ventilation is more homogenously distributed. ✯ A reduction in physiological shunt occurs dt improvement in V/Q matching ✯ Compression of dorsal lung regions by the heart is reduced. ✯ Anterior chest wall compliance is decreased. 316b Critical Care revision notes Dr.Sherif Badrawy
- 634. Precautions in Pts with severe aortic stenosis 317a Critical Care revision notes Dr.Sherif Badrawy
- 635. ✯ LV is hypertrophied and poorly compliant, and will require a high preload and high filling pressures. ✯ Swift cardioversion of any atrial fibrillation that develops,as The 'atrial kick' is of greater importance to help fill the stiff left ventricle ✯ Intra-aortic balloon counterpulsation, inflates in diastole improving coronary perfusion, it's CI in severe AR since it increases the regurgitant fraction. ✯ Use of vasopressors to elevate systemic vascular resistance ✯ Dieuretics are used with caution since a drop in preload can severely compromise 317b Critical Care revision notes Dr.Sherif Badrawy
- 636. CT brain in Cerebral venous sinus thrombosis 318a Critical Care revision notes Dr.Sherif Badrawy
- 637. 'empty delta sign' a triangular area of enhancement is seen on multiple contiguous transverse CT images in the region of the superior sagittal sinus. However, a CT scan is entirely normal in 10-20% of cases. 318b Critical Care revision notes Dr.Sherif Badrawy
- 638. CP of Cerebral venous sinus thrombosis 319a Critical Care revision notes Dr.Sherif Badrawy
- 639. ✯ Nine in ten people with sinus thrombosis have a headache; this tends to worsen over the period of several days, but may also develop suddenly (thunderclap headache), may be the only symptom of cerebral venous sinus thrombosis ✯ symptoms of stroke: inability to move one or more limbs, weakness on one side of the face or difficulty speaking. This does not necessarily affect one side of the body as in the more common "arterial" stroke. ✯ 40% have seizures, affecting only one part of the body and unilateral, occasionally generalised 319b Critical Care revision notes Dr.Sherif Badrawy
- 640. Type of Pt of Cerebral venous sinus thrombosis 320a Critical Care revision notes Dr.Sherif Badrawy
- 641. The condition is more likely in young women, especially in the puerperium, and is also associated with any hypercoagulable state Systemic or localised infections may also precipitate the condition. 320b Critical Care revision notes Dr.Sherif Badrawy
- 642. Rx of Cerebral venous sinus thrombosis 321a Critical Care revision notes Dr.Sherif Badrawy
- 643. Therapeutic anticoagulation is indicated even in the presence of venous infarction 321b Critical Care revision notes Dr.Sherif Badrawy
- 644. CP of critical illness polyneuromyopathy ? 322a Critical Care revision notes Dr.Sherif Badrawy
- 645. ✯ Ventilation for >7 days. ✯ A flaccid quadriparesis is a common presentation ✯ Elevated serum creatinine kinase. ✯ Four twitches of equal height with train-of- four nerve stimulation, If fade or a reduced count is present this should raise suspicion of residual neuromuscular blockade 322b Critical Care revision notes Dr.Sherif Badrawy
- 646. antimicrobial treatment in a catheterised ICU patient suspected UTI 323a Critical Care revision notes Dr.Sherif Badrawy
- 647. ✯ Candida in urine culture ➜ NO Rx unless isolated from multiple sites,consider Rx if high levels are present (> (10)4cfu/ml), signs of infection are present, and no other source of infection is apparent. ✯ Pyuria [>10 WBCs/ml urine]. alone not mandate antibiotic Rx, search for urinary pathogens. Non-infectious causes of pyuria as recent antibiotic Rx, systemic inflammatory conditions, nephrolithiasis and drugs [CST]. ✯ Urine culture >(10)3 CFU/ml bacteria ➜ antibiotic Rx only in the presence of clinical indicators of infection and may represent simple colonisation if such indicators are absent. ✯ Positive urine dipstick for leukocyte esterase and/or nitrate ➜ further Ix, it is not sufficiently specific to justify antibiotic Rx in the absence of supporting evidence of UTI. 323b Critical Care revision notes Dr.Sherif Badrawy
- 648. How to r/o Budd chiari syndrome ? 324a Critical Care revision notes Dr.Sherif Badrawy
- 649. Doppler ultrasonography. but the gold standard is hepatic venography. 324b Critical Care revision notes Dr.Sherif Badrawy
- 650. SAAG 325a Critical Care revision notes Dr.Sherif Badrawy
- 651. 325b Critical Care revision notes Dr.Sherif Badrawy
- 652. cocaine toxicity Rx 326a Critical Care revision notes Dr.Sherif Badrawy
- 653. ✯ a benzodiazepine ameliorates both the cerebral and CVS manifestations ✯ alpha-blockade is preferable to beta- blockade to avoid unopposed alpha stimulation ➜ ↟BP. 326b Critical Care revision notes Dr.Sherif Badrawy
- 654. Gamma-hydroxybutyrate [derived from GABA] 327a Critical Care revision notes Dr.Sherif Badrawy
- 655. ✯ popular recreational drug ✯ also a muscle-bulking agent used by bodybuilders ✯ Toxicity ➜ euphoria in small doses ➜ hypothermia, bradycardia, ↓GCS and emesis. ✯ effects of overdose lasts only for several hours 327b Critical Care revision notes Dr.Sherif Badrawy
- 656. Ecstasy poisoning 328a Critical Care revision notes Dr.Sherif Badrawy
- 657. ✯ tachycardia and hyperpyrexia NOT bradycardia & hypothermia. 328b Critical Care revision notes Dr.Sherif Badrawy
- 658. Ketamine poisoning as a recreational drug 329a Critical Care revision notes Dr.Sherif Badrawy
- 659. ✯ loss of awareness with preservation of airway and cardiovascular reflexes ✯ hypertension, tachycardia in large doses. 329b Critical Care revision notes Dr.Sherif Badrawy
- 660. parameters are directly set by the operator of HFOV 330a Critical Care revision notes Dr.Sherif Badrawy
- 661. ✯ Frequency. ✯ I:E ratio. ✯ Driving pressure. ✯ Mean airway pressure. ✯ Tidal volume is provided by oscillations of pressure around the mean value (delta P). directly related to the driving pressure, and inversely related to the frequency 330b Critical Care revision notes Dr.Sherif Badrawy
- 662. HELLP Syndrome 331a Critical Care revision notes Dr.Sherif Badrawy
- 663. ✯ Schistocytes are seen on the blood film. ✯ LDH is elevated ✯ Delivery of the foetus is the mainstay of treatment. ✯ Hypoglycaemia and acute liver failure are uncommon. ✯ Not always in association with preeclampsia. 20% of cases of HELLP have no antecedent history of HTN or proteinuria. 331b Critical Care revision notes Dr.Sherif Badrawy
- 664. Aspirin effect on cyclo-oxygenase 332a Critical Care revision notes Dr.Sherif Badrawy
- 665. ✯ Aspirin has greater effect on platelet cyclo- oxygenase than endothelial cyclo-oxygenase in low doses ➜ ↓thromboxane A2 production and platelet aggregation. ✯ Aspirin irreversibly inhibits platelet cyclo-oxygenase. ✯ Even in high doses aspirin is a less effective analgesic agent than most NSAIDS. ✯ All NSAIDs can displace warfarin from its albumin binding site, promoting anticoagulation 332b Critical Care revision notes Dr.Sherif Badrawy
- 666. Regarding the hepatic clearance of drugs 333a Critical Care revision notes Dr.Sherif Badrawy
- 667. ✯ Drugs with a high extraction ratio exhibit flow-dependent metabolism. ✯ Enzyme induction significantly increases clearance of drugs with a low extraction ratio. ✯ Phenytoin has a low extraction ratio. ✯ A drug with a high extraction ratio will have low bioavailability. 333b Critical Care revision notes Dr.Sherif Badrawy
- 668. sickle cell disease, How to prevent sickling crises 334a Critical Care revision notes Dr.Sherif Badrawy
- 669. ✯ Good hydration. ✯ correction of acidosis, ✯ excellent analgesia ✯ Exchange transfusion to maintain HbS levels of <30%. ✯ Maintenance of normothermia ✯ Avoidance of hypoxaemia. ✯ Chest physiotherapy. 334b Critical Care revision notes Dr.Sherif Badrawy
- 670. Rx of Clostridium difficile diarrhoea 335a Critical Care revision notes Dr.Sherif Badrawy
- 671. ✯ uncomplicated cases oral metronidazole DOCH, effective and cheap ✯ Stop the antibiotic associated with the outbreak [quinolones, clindamycin and cephalosporins] ✯ ileus is present ➜ oral metronidazole or vancomycin is ineffective ➜ Use IV metronidazole [IV vancomycin is of no use since it does not penetrate the large bowel in sufficient dose] ✯ Probiotics ➜ weak evidence ✯ IV immunoglobulin ➜ effective in small case series, for refractory cases if antibiotic therapy is unsuccessful. It is not a first-line treatment 335b Critical Care revision notes Dr.Sherif Badrawy
- 672. Notes on Antifungal Rx 336a Critical Care revision notes Dr.Sherif Badrawy
- 673. ✯ Voriconazole ➜ QT prolongation in susceptible individuals [patient on amiodarone] ✯ Amphotericin B ➜ wide spectrum of activity, effective against most Candida ➜ renal impairment ✯ Fluconazole ➜ effective against C. albicans but less so against other forms of Candida including C. glabrata which is resistant in 60% ✯ Nystatin ➜ Rx of C. albicans of the skin and mm, but not for systemic candidiasis ✯ Caspofungin ➜ a broad spectrum of activity suitable for invasive Candida and Aspergillus 336b Critical Care revision notes Dr.Sherif Badrawy
- 674. Definition of Autonomy 337a Critical Care revision notes Dr.Sherif Badrawy
- 675. respect for the patient's wishes and attitudes regarding the treatment they wish to receive 337b Critical Care revision notes Dr.Sherif Badrawy
- 676. Definition of Non-maleficence 338a Critical Care revision notes Dr.Sherif Badrawy
- 677. the duty of the physician not to do harm to the patient or members of the healthcare team or wider community. 338b Critical Care revision notes Dr.Sherif Badrawy
- 678. Definition of Beneficence 339a Critical Care revision notes Dr.Sherif Badrawy
- 679. the duty of the healthcare team to 'do good' to the patient by effecting a cure, relieving suffering and generally acting in their best interests. 339b Critical Care revision notes Dr.Sherif Badrawy
- 680. Definition of Utility 340a Critical Care revision notes Dr.Sherif Badrawy
- 681. the principle of doing the greatest good for the greatest number of patients with the resources available; [ the obligation to provide a net balance of benefits over harms with limited resources], a subset of beneficence 340b Critical Care revision notes Dr.Sherif Badrawy
- 682. Definition of Justice 341a Critical Care revision notes Dr.Sherif Badrawy
- 683. the obligation to distribute benefits and harms fairly. 341b Critical Care revision notes Dr.Sherif Badrawy
- 684. Definition of Paternalism 342a Critical Care revision notes Dr.Sherif Badrawy
- 685. implies that 'the doctor knows best' for the pt. While this may be true in some contexts (e.g. which antibiotic is appropriate for the pt's infection), in the wider sense it contradicts the principle of pt autonomy. The physician has a duty to act as the pt would wish him to act rather than imposing his own beliefs. Giving a blood transfusion to a devout Jehovah's Witness would be an extreme example of paternalism. 342b Critical Care revision notes Dr.Sherif Badrawy
- 686. Regarding the refeeding syndrome: 343a Critical Care revision notes Dr.Sherif Badrawy
- 687. a. It occurs solely as a consequence of parenteral nutrition.【✘】➜ both enteral and parenteral nutrition b. It develops around day 4 following reinstatement of nutrition.【✔】 c. Thiamine and B vitamins should be given prior to commencing feeding after a prolonged period of poor nutrition.【✔】➜ as patients are at risk of Wernicke's encephalopathy d. It is a consequence of low insulin levels.【✘】➜ High insulin levels. 343b Critical Care revision notes Dr.Sherif Badrawy
- 688. 46-y, M, electrocution, maintaining an airway, has a palpable pulse but is extending to pain and has fixed and dilated pupils. His ECG is normal. A small burn wound is found over the left forearm. 344a Critical Care revision notes Dr.Sherif Badrawy
- 689. a. The neurological prognosis is hopeless.【✘】 b. A normal ECG makes ongoing cardiac problems unlikely.【✔】 c. The small entry wound makes significant tissue damage unlikely.【✘】 d. Wet skin has 50% less impedance to current flow than dry skin.【✘】➜ Wet skin has an impedance of around 100 times less than dry skin greater current to flow for a given voltage with consequently greater tissue damage 344b Critical Care revision notes Dr.Sherif Badrawy
- 690. 50-y, M, Out of the hospital Cardiac Arrest, defibrillation on the arrival of the paramedics, ROSC after 12 minutes, fixed and dilated pupils and a GCS 5, with flexion to pain, ICU & MV. 345a Critical Care revision notes Dr.Sherif Badrawy
- 691. a. His neurological prognosis is hopeless.【✘】➜ Initial neurological presentation is a poor predictor of outcome following ROSC neurological function are considered unreliable in the first 72h post-ROSC. b. He should be actively cooled to 32-34°C.【✔】 c. His age has a bearing on his survival chances.【✔】 d. Patients admitted to ICU following out-of-hospital cardiac arrest have less than a 10% chance of survival to hospital discharge.【✘】➜ around 30% 345b Critical Care revision notes Dr.Sherif Badrawy
- 692. FAST scanning in the emergency assessment of blunt abdominal trauma: 346a Critical Care revision notes Dr.Sherif Badrawy
- 693. a. Visualisation of the pericardium is a key view. 【✔】➜ subxiphoid view b. Free intraperitoneal fluid volumes in excess of 500ml are reliably detected.【✔】 c. It is moderately sensitive for detecting encapsulated solid organ injury.【✔】 d. Hollow viscus injury is detected in 60-70% of cases. 【✘】➜ rarely detects injury to a hollow viscus even in experienced hands. 346b Critical Care revision notes Dr.Sherif Badrawy
- 694. 34-y, M, a stab wound to the abdomen, RR of 30, HR of 130, BP of 65/40, A 3cm entry wound in the epigastric area, firm abdomen with guarding. 347a Critical Care revision notes Dr.Sherif Badrawy
- 695. a. Chest X-ray is mandatory.【✔】➜ A stab wound could easily cause tension pneumothorax or cardiac tamponade exclude clinically, then radiologically. b. Complete head to toe exposure should be part of the primary survey.【✔】 c. If a FAST scan is normal, laparotomy should be deferred.【✘】 d. a fluid bolus should be given to this pt as soon as vascular access is obtained.【✔】 347b Critical Care revision notes Dr.Sherif Badrawy
- 696. The following are causes of the abdominal compartment syndrome: 348a Critical Care revision notes Dr.Sherif Badrawy
- 697. a. High volume crystalloid resuscitation. 【✔】 b. Pancreatitis.【✔】 c. Blunt abdominal trauma.【✔】 d. Laparostomy.【✘】 348b Critical Care revision notes Dr.Sherif Badrawy
- 698. Etiology of Abdominal compartment syndrome 349a Critical Care revision notes Dr.Sherif Badrawy
- 699. can be primary (due to an intra-abdominal cause, e.g. pancreatitis, haemorrhage, trauma, perforation), or secondary to high- volume fluid resuscitation, extensive burns or sepsis (any condition where capillary leak can cause large volumes of fluid to be sequestered in the abdominal compartment). 349b Critical Care revision notes Dr.Sherif Badrawy
- 700. The following are causes of elevated protein in cerebrospinal fluid: 350a Critical Care revision notes Dr.Sherif Badrawy
- 701. a. Brain tumour.【✔】 b. Seizure.【✔】 c. Bacterial meningitis.【✔】 d. Neurosyphilis.【✔】 350b Critical Care revision notes Dr.Sherif Badrawy
- 702. Other causes of elevated CSF protein 351a Critical Care revision notes Dr.Sherif Badrawy
- 703. The previous + abscess, haemorrhage, demyelinating disease and Guillain-Barré syndrome. 351b Critical Care revision notes Dr.Sherif Badrawy
- 704. normal range of CSF protein 352a Critical Care revision notes Dr.Sherif Badrawy
- 705. is around 0.2-0.4g/L. CSF protein is extremely non-specific 352b Critical Care revision notes Dr.Sherif Badrawy
- 706. causes of low CSF protein 353a Critical Care revision notes Dr.Sherif Badrawy
- 707. a chronic dural leak or repeated lumbar punctures, and water intoxication. Hypoproteinaemia is not a cause 353b Critical Care revision notes Dr.Sherif Badrawy
- 708. 28-y ,M, mixed overdose, Rx with antidepressant tablets, HR of 145bpm, BP of 210/150, 39.7°C, extremely agitated and has muscular rigidity and clonus; no extrapyramidal features. 【history is highly suggestive of the serotonin syndrome, SSRI, antidepressants and ecstasy could cause this】 354a Critical Care revision notes Dr.Sherif Badrawy
- 709. a. MDMA ('ecstasy') should be considered as a possible cause.【✔】 b. Benzodiazepine therapy is CI for this patient. 【✘】 c. ETT & MV may be indicated.【✔】 d. A 5-hydroxytryptamine agonist may have a role in treatment of this patient.【✘】➜ A 5- HT2A antagonist cyproheptadine. 354b Critical Care revision notes Dr.Sherif Badrawy
- 710. 58-y, F, recovering from CAP, received ceftriaxone 2 wks ago, abdominal distension, fever and profuse watery diarrhoea, Tachycardia, dehydrated, abdominal X-ray shows distended loops of large bowel (10cm). 355a Critical Care revision notes Dr.Sherif Badrawy
- 711. a. This condition carries a mortality of 50%.【✘】➜ Mortality around 5%. b. Colonoscopy is the investigation of choice.【✘】 c. Initial treatment should include oral clindamycin. 【✘】 d. An urgent surgical opinion should be obtained. 【✔】➜ a surgical emergency and may complicate any form of colitis including IBD and ischaemia. 355b Critical Care revision notes Dr.Sherif Badrawy
- 712. The following interventions have been shown to reduce mortality in patients with septic shock: 356a Critical Care revision notes Dr.Sherif Badrawy
- 713. a. Antithrombin III.【✘】 b. Activated protein C.【✘】 c. Anti-TNF-a antibody.【✘】 d. High dose methylprednisolone.【✘】 356b Critical Care revision notes Dr.Sherif Badrawy
- 714. 37-y, M, crushed against a wall by a truck, significant abdominal injuries, hypovolaemic shock, ATLS® class III, laparotomy, splenectomy,retroperitoneal bleeding, 18 units PRBCs, ICU ➜ 6 units PRBCs, HCT 23%, platelets 30, fibrinogen 0.4g/L, INR 6.2. 357a Critical Care revision notes Dr.Sherif Badrawy
- 715. a. Recombinant factor VIIa should be given immediately. 【✘】➜ correction of platelets, fibrinogen, hypothermia, acidosis and ionised calcium to minimum levels is a pre- requisite for its use. b. Class III shock implies blood loss of over 2L.【✘】➜ 1.5- 2L. c. It is not mandatory to give vitamin K immediately. 【✔】➜ of little benefit as a dilutional coagulopathy dt massive transfusion rather than a primary synthetic problem. d. His temperature should be checked【✔】 357b Critical Care revision notes Dr.Sherif Badrawy
- 716. 41-y, M, RTA, shock, pelvis is unstable, disrupted pelvic ring on X-ray, ETT, OR, remains in shock despite 3L crystalloid and 1L gelofusine, HCT 28%, PT 28s. 358a Critical Care revision notes Dr.Sherif Badrawy
- 717. a. The presence of a coagulopathy worsens the prognosis. 【✔】 b. HCT is an insensitive indicator of the need for surgical intervention.【✔】 c. A high level of PEEP should be used in theatre to prevent lung derecruitment.【✘】➜ should be minimised until bleeding controlled. d. Immediate mechanical stabilization of the pelvic ring is indicated.【✔】 358b Critical Care revision notes Dr.Sherif Badrawy
- 718. 76-y, M, house fire, hospital 4 hours later, ETT, Carbonaceous sputum from ETT, MV, burns across his entire torso ant., face, backs of both arms. 359a Critical Care revision notes Dr.Sherif Badrawy
- 719. a. He has burns to approximately 45% of his body surface area. 【✘】➜ ~ 36% BSA b. A reasonable fluid regime would be 4ml/kg/% body surface area burns over the next 24 h.【✘】 c. Use of suxamethonium would be dangerous in this situation.【✘】➜ life-threatening hyperkalaemia about 10 days post-burn, It is safe at the time of the injury d. O2 Rx should be titrated initially to maintain PaO2 around 10kPa (76 mmHg).【✘】➜ CO poisoning. Arterial PaO2 may not reflect blood oxygen carriage, and 100% O2 is warranted. 359b Critical Care revision notes Dr.Sherif Badrawy
- 720. rule of 9 in burn 360a Critical Care revision notes Dr.Sherif Badrawy
- 721. 360b Critical Care revision notes Dr.Sherif Badrawy
- 722. rule of 9 in children 361a Critical Care revision notes Dr.Sherif Badrawy
- 723. 361b Critical Care revision notes Dr.Sherif Badrawy
- 724. 44-y, M, HAP, Sputum and blood C&S ESBL Klebsiella, empirical antibiotic 362a Critical Care revision notes Dr.Sherif Badrawy
- 725. a. Cefotaxime and gentamicin.【✘】 b. Piperacillin/tazobactam.【✘】 c. Imipenem.【✔】DOCH, good in vitro and in vivo effect against ESBL-producers. d. Ciprofloxacin.【✘】 362b Critical Care revision notes Dr.Sherif Badrawy
- 726. 66-y, M, SOB, X-ray pulmonary oedema, ETT, MV, BP 185/120, HR 115, SpO2 92% on 80% FIO2, oesophageal Doppler probe ➜ flow time corrected (FTc) 270ms, peak velocity 35cm/s, stroke volume 40ml, fluid challenge of 250ml colloid over 10 minutes. Repeat readings : FTc 275ms, peak velocity 33cm/s, stroke volume 39ml 363a Critical Care revision notes Dr.Sherif Badrawy
- 727. a. A further fluid bolus should be given.【✘】 b. A nitrate infusion is appropriate.【✔】 c. Frusemide is appropriate.【✔】 d. Cardiac contractility is normal for a man of this age. 【✘】 NB:FTc is low dt ↑SVR ➜ Hx suggesting HF (not all cases of reduced FTc are due to hypovolaemia)lack of response to a fluid challenge (no significant↑SV, ↓peak velocity) suggesting that this patient is fluid-overloaded. 363b Critical Care revision notes Dr.Sherif Badrawy
- 728. Regarding the arterial pressure wave in the hypovolaemic mechanically ventilated patient: 364a Critical Care revision notes Dr.Sherif Badrawy
- 729. a. Changes in pulse pressure across the respiratory cycle better reflect hypovolaemia than changes in systolic pressure.【✔】 b. Pulse pressure is inversely proportional to stroke volume.【✘】 c. The maximum fall in systolic pressure coincides temporally with the peak inspiratory pressure.【✘】 d. The arterial pressure waveform is an unreliable guide to fluid requirement in arrhythmias.【✔】 364b Critical Care revision notes Dr.Sherif Badrawy
- 730. Regarding the physics of direct arterial blood pressure measurement: 365a Critical Care revision notes Dr.Sherif Badrawy
- 731. a. The catheter connecting the arterial cannula to the transducer should be short, stiff and narrow to reduce resonance.【✘】 b. Bubbles and clots cause damping.【✔】 c. The resonant frequency of the system should be greater than 30Hz.【✔】 d. The primary harmonic of the system is 100Hz. 【✘】 365b Critical Care revision notes Dr.Sherif Badrawy
- 732. Regarding the assessment of sedation on the ICU: 366a Critical Care revision notes Dr.Sherif Badrawy
- 733. a. A score of 3-4 is desirable on the Richmond agitation and sedation scale.【✘】 b. The commonest form of delirium in the ICU patient is characterised by hyperarousal and agitation.【✘】➜ hypoactive form c. The Ramsay scale does not assess patient agitation. 【✔】➜ It is primarily a test of rousability d. The GCS is not useful for the assessment of sedation.【✔】 366b Critical Care revision notes Dr.Sherif Badrawy
- 734. The Richmond agitation and sedation scale 367a Critical Care revision notes Dr.Sherif Badrawy
- 735. scored from +4 (combative and violent) to - 5 (unrousable). A score of 0 (alert and calm) is desirable. 367b Critical Care revision notes Dr.Sherif Badrawy
- 736. The Ramsay sedation scale 368a Critical Care revision notes Dr.Sherif Badrawy
- 737. A score from 1 (anxious and restless) to 6 (unresponsive) is given, with 3-4 being optimal. 368b Critical Care revision notes Dr.Sherif Badrawy
- 738. Effects of excessive heparinisation of an ABG sample on the measured values may include: 369a Critical Care revision notes Dr.Sherif Badrawy
- 739. a. Elevated PaCO2.【✘】 b. Reduced PaCO2.【✔】 c. Elevated PaO2.【✔】 d. Reduced bicarbonate.【✔】 369b Critical Care revision notes Dr.Sherif Badrawy
- 740. 48-y, M, homeless, unresponsive on the street, signs of malnutrition, temperature of 28°C, HR of 42, GCS 5. 370a Critical Care revision notes Dr.Sherif Badrawy
- 741. a. Passive re-warming should be commenced limiting temperature rise to 1°C per hour.【✘】 b. Intubation should be avoided as it may cause ventricular fibrillation.【✘】 c. IV thiamine should be administered urgently.【✔】 d. If VF occurs, DC cardioversion should not be attempted until the core temperature is above 30°C.【✘】➜ Cardioversion can be attempted < 30°C, but if a perfusing rhythm is not restored after 3 shocks no further attempts until core temperature > 30°C. 370b Critical Care revision notes Dr.Sherif Badrawy
- 742. Pt in HDU, acting strangely, normally a nursing home resident and now appears agitated and confused, features favour a diagnosis of delirium as opposed to dementia: 371a Critical Care revision notes Dr.Sherif Badrawy
- 743. a. Global cognitive impairment.【✘】➜ Focal cognitive impairment is in keeping with delirium, whereas global impairment suggests dementia b. An insidious onset of symptoms.【✘】➜ acute with delirium (hours), insidious with dementia. c. Inattention.【✔】 d. Psychotic symptoms.【✔】 371b Critical Care revision notes Dr.Sherif Badrawy
- 744. delirium vs dementia 372a Critical Care revision notes Dr.Sherif Badrawy
- 745. 372b Critical Care revision notes Dr.Sherif Badrawy
- 746. Regarding acute epiglottitis in adults: 373a Critical Care revision notes Dr.Sherif Badrawy
- 747. a. It is more common than in children.【✔】 b. Haemophilus influenzae has been largely eradicated as a cause.【✘】 c. Amoxycillin with clavulanic acid is appropriate empirical therapy.【✔】 d. Patients usually appear systemically well. 【✘】➜ usually toxic and unwell with a high fever. 373b Critical Care revision notes Dr.Sherif Badrawy
- 748. 75-y, M, SDH 6 days ago, ETT, MV, massive PE, confirmed by CTPA, IVC filter is considered. 374a Critical Care revision notes Dr.Sherif Badrawy
- 749. a. Thrombolysis is absolutely CI.【✔】 b. Once placed the filter cannot safely be removed.【✘】 c. IVC filters are effective in reducing the incidence of further PE.【✔】 d. IVC filters do not improve survival.【✔】 374b Critical Care revision notes Dr.Sherif Badrawy
- 750. 28-y, RTA, severe TBI, ICU, evacuated SDH, ICP 40 mmHg. Appropriate Rx to buy time while awaiting a CT brain 375a Critical Care revision notes Dr.Sherif Badrawy
- 751. a. Dobutamine infusion.【✘】 b. Frusemide.【✔】➜ acceptable but mannitol is MC used c. Hyperventilation to a PaCO2 of 3.5kPa (27mmHg). 【✔】➜ a PaCO2 < 4.0kPa (30mmHg) not recommended for the routine Rx of head injury , dt cerebral artery VC and may worsen brain ischaemia. However, as an acute Rx ➜↓ICP ➜ buy time until definitive Rx. d. Thiopentone bolus.【✔】 375b Critical Care revision notes Dr.Sherif Badrawy
- 752. The following capnograph trace on a ventilated patient is consistent with: 376a Critical Care revision notes Dr.Sherif Badrawy
- 753. a.Endobronchialintubation following patient repositioning.【✘】➜ A rapid fallin the end-tidalCO2 over the course of a few breaths➜ a fallin COP ➜ ↑physiologicaldead space (↑V/Q ratio). b.Air embolism.【✔】 c.Incipient cardiacarrest.【✔】 d.Bronchospasm.【✘】➜ waveform'llbe rising to a peak rather than being 'flat-topped' 376b Critical Care revision notes Dr.Sherif Badrawy
- 754. 75-y, F, 5 days after anterior MI, SOB, chest X- ray ➜ pulmonary venous congestion. neck veins distended. A systolic murmur on auscultation. BP 80/65, PAC ➜ PAO2 Sat 88%, PAP 50/23mmHg. The following are true:88% is 【PAO2 Sat 88% is much higher than would normally be expected (mixed venous oxygen saturation should be around 70%)】 377a Critical Care revision notes Dr.Sherif Badrawy
- 755. a. This lady probably has papillary muscle rupture. 【✘】➜ VSD ➜ Lt to Rt shunt, usu within a week of MI b. This lady is likely to need urgent surgery.【✔】➜ 30- day survival is 24% with medical Rx and 47% when Rx surgically. c. ECG is the key investigation.【✘】➜ Ix of choice is Doppler echo ➜ excludes papillary muscle rupture. d. Urgent needle thoracocentesis is the treatment of choice.【✘】➜ Rx of choice for cardiac tamponade 377b Critical Care revision notes Dr.Sherif Badrawy
- 756. 55-y, M, massive haemoptysis [500ml blood over a 3-h], several minor episodes of haemoptysis over the last few months, BP 90/70, HR of 100, SpO2 of 85% on 15L/min oxygen NRBM, 378a Critical Care revision notes Dr.Sherif Badrawy
- 757. a. IV access and rapid fluid challenge is the first priority. 【✘】➜ The 1st priority is to secure the airway and improve O2. b. A double-lumen tube is mandatory if tracheal intubation is required.【✘】 c. Fibreoptic bronchoscopy may be useful in this case. 【✔】➜ may be difficult dt blood but should be attempted by an experienced operator, Dx & Rx. d. If a bleeding source is lateralised, the patient should be ventilated with that side dependent.【✔】➜ to prevent blood from contaminating the other lung. 378b Critical Care revision notes Dr.Sherif Badrawy
- 758. The following therapeutic manoeuvres improve survival in the ARDS: 379a Critical Care revision notes Dr.Sherif Badrawy
- 759. a. High levels of PEEP >15cm H2O.【✘】 b. Proning for >8 hours per day.【✘】 c. Low tidal volume ventilation (6ml/kg predicted body weight).【✔】➜ and limiting plateau pressure d. Alveolar recruitment manoeuvres.【✘】 379b Critical Care revision notes Dr.Sherif Badrawy
- 760. Regarding atrial fibrillation in the postoperative period: 380a Critical Care revision notes Dr.Sherif Badrawy
- 761. a. Overall incidence is low (<1%) in non- cardiothoracic surgery.【✔】 b. It most commonly occurs in the first 3 postoperative days.【✔】 c. It resolves spontaneously in most patients. 【✔】 d. It occurs in 80-90% of patients following coronary artery bypass grafting.【✘】 380b Critical Care revision notes Dr.Sherif Badrawy
- 762. 67-y, M, CCU, central chest pain, like his usual angina but more severe, pain came on at rest and has lasted for 3 h, ECG 1mm ST depression in the lateral leads, CK normal on admission 381a Critical Care revision notes Dr.Sherif Badrawy
- 763. a. A diagnosis of ACS can be made.【✔】 b. Aspirin and clopidogrel should be administered.【✔】 c. A glycoprotein IIb/IIIa inhibitor is not indicated.【✘】 d. PCI is only beneficial in the presence of STEMI.【✘】 381b Critical Care revision notes Dr.Sherif Badrawy
- 764. 66-y, CCU, severe cardiogenic shock, ECG significant ↓ST anterior leads, cold and clammy, BP of 80/60, HR 120 (sinus tachy), unrecordable Sao2, X-ray ➜ pulmonary oedema, Despite appropriate inotropic support his condition fails to improve over the next few hours 382a Critical Care revision notes Dr.Sherif Badrawy
- 765. a. MI is the MCC of cardiogenic shock. 【✔】 b. MV is CI as it will further impair COP. 【✘】 c. CPAP ↓preload.【✔】 d. CPAP ↓afterload.【✔】 382b Critical Care revision notes Dr.Sherif Badrawy
- 766. 49-y, M, painful left-sided ophthalmoplegia following a recent sinusitis,chemosis, slight proptosis, ↓visual acuity, Dx of cavernous sinus thrombosis is considered. 383a Critical Care revision notes Dr.Sherif Badrawy
- 767. a. CT brain scan is likely to be a useful Ix in this case. 【✔】➜ MRI occasionally if CT fails to make Dx. b. IV empirical antibiotics are indicated.【✔】 ➜ location of the cavernous sinuses and their extensive venous connections vulnerable to septic thrombi [MCC Staphylococcus aureus] c. Mortality is 80-100%.【✘】This is In the pre-antibiotic era, now ~20% with appropriate antimicrobial Rx. d. Cavernous sinus thrombosis is the MCC of cerebral venous sinus thrombosis.【✘】 383b Critical Care revision notes Dr.Sherif Badrawy
- 768. The following are risk factors for the development of critical illness polyneuromyopathy: 384a Critical Care revision notes Dr.Sherif Badrawy
- 769. a. Sepsis.【✔】 b. Corticosteroids.【✔】 c. Neuromuscular blocking agents.【✔】 d. Poor glycaemic control.【✔】 NB : ✾ MV >4-7 days ✾ Nerve conduction ➜ show evidence of denervation. ✾ muscle biopsy ➜ shows evidence of myopathy. 384b Critical Care revision notes Dr.Sherif Badrawy
- 770. Regarding urinalysis: 385a Critical Care revision notes Dr.Sherif Badrawy
- 771. a. Red cell casts are always pathological.【✔】 b. A negative nitrite dipstick effectively excludes the presence of bacteria in the urine.【✘】➜ Although 90% of common urinary pathogens are nitrite-forming, [NOT Pseudomonas, Staph albus, Staph saprophyticus, Strept faecalis] c. Hyaline casts are suggestive of bacterial endocarditis. 【✘】➜ Tamm-Horsfall glycoprotein, common in healthy individuals. d. White cell casts are a normal finding.【✘】➜ proliferative GN, AIN & acute PN. 385b Critical Care revision notes Dr.Sherif Badrawy
- 772. Regarding pharmacological prophylaxis of stress ulceration in the ICU: 386a Critical Care revision notes Dr.Sherif Badrawy
- 773. a. Sucralfate neutralises gastric pH.【✘】 b. PPI are superior to H2-blockers in preventing clinically significant bleeding. 【✘】 c. Tolerance occurs to ranitidine.【✔】 d. Antacids are effective with twice-daily dosing.【✘】 386b Critical Care revision notes Dr.Sherif Badrawy
- 774. 74-y, M, biliary tract sepsis, ICU, Over 3 days ➜ marked abdominal distension, X- ray ➜ dilatation of the large bowel, features favour Dx acute intestinal pseudo- obstruction [Ogilvie's syndrome] over mechanical obstruction: 387a Critical Care revision notes Dr.Sherif Badrawy
- 775. a. The presence of air in the rectosigmoid colon on plain radiography.【✔】 b. A maximum colonic diameter of 10cm on plain radiography.【✘】 c. Free passage of contrast during a contrast enema study.【✔】 d. The presence of bowel sounds on auscultation.【✘】 387b Critical Care revision notes Dr.Sherif Badrawy
- 776. Renal failure may cause alterations in the following pharmacokinetic properties of a drug: 388a Critical Care revision notes Dr.Sherif Badrawy
- 777. a. Absorption.【✔】 b. Distribution.【✔】 c. Metabolism.【✔】 d. Excretion.【✔】 388b Critical Care revision notes Dr.Sherif Badrawy
- 778. Pt has liver cirrhosis, major upper GI bleeding dt oesophageal varices, ICU for resuscitation, acute pharmacological management 389a Critical Care revision notes Dr.Sherif Badrawy
- 779. a. Glypressin.【✔】➜ improve survival and be as effective as balloon tamponade for bleeding control b. Propranolol.【✘】➜ prophylaxis rather than treatment of an acute bleed. c. Somatostatin.【✔】➜ selective splanchnic VC & ↓portal pressure d. Isosorbide mononitrate.【✘】 389b Critical Care revision notes Dr.Sherif Badrawy
- 780. 65-y, F, exploratory laparotomy and right hemicolectomy. With regard to her nutrition: 390a Critical Care revision notes Dr.Sherif Badrawy
- 781. a. Parenteral feeding should be instituted only if enteral feeding has been unsuccessful over a 72-hour period.【✘】 b. Mortality is 20% higher in parenterally fed ICU patients compared with enteral feeding.【✘】 c. Delayed feeding is associated with poorer ICU outcome.【✔】 d. Parenteral feeding is associated with a higher risk of infectious complications.【✔】 390b Critical Care revision notes Dr.Sherif Badrawy
- 782. The following are elements of the 24-h sepsis mgmnt bundle as advocated by the Surviving Sepsis Campaign group: 391a Critical Care revision notes Dr.Sherif Badrawy
- 783. a. Administration of recombinant human activated protein C for eligible patients.【✘】 b. Methylprednisolone 1g q.d.s. for patients requiring vasopressors.【✘】➜ hydrocortisone 200-300mg/day c. Maintain glucose <12.4mmol/L (225mg/dL).【✘】➜ between 3.8-8.3mmol/L d. Maintain a plateau pressure of <30cmH2O for mechanically ventilated patients.【✔】 391b Critical Care revision notes Dr.Sherif Badrawy
- 784. Regarding high frequency oscillatory ventilation (HFOV): 392a Critical Care revision notes Dr.Sherif Badrawy
- 785. a. O2 can be improved by ↑mean airway pressure.【✔】➜ by greater splinting open of alveoli (with reduced shunt). b. Expiration is passive.【✘】➜ Expiration is active (the diaphragm moves both 'in' and 'out'). c. Frequency of ventilation is typically 50-100 breaths per minute.【✘】➜ ~300 breaths/min d. CO2 elimination can ↑ by reducing the frequency of ventilation.【✔】➜ by either increasing DP or decreasing the frequency 392b Critical Care revision notes Dr.Sherif Badrawy
- 786. The following forms of shock may be present in amniotic fluid embolism: 393a Critical Care revision notes Dr.Sherif Badrawy
- 787. a. Distributive.【✔】 b. Cardiogenic.【✔】 c. Obstructive.【✔】 d. Haemorrhagic.【✔】 393b Critical Care revision notes Dr.Sherif Badrawy
- 788. Types of shock in amniotic fluid embolism 394a Critical Care revision notes Dr.Sherif Badrawy
- 789. ❂ Obstructive shock and cardiogenic shock ➜ predominate early ❂ Obstructive ➜ dt PA VC dt exposure to immunologically active substances ❂ Cardiogenic ➜ dt LV dysfunction. ❂ Distributive ➜ later dt SIRS ➜ capillary leak ❂ Haemorrhagic ➜ dt DIC ➜ life-threatening Hge 394b Critical Care revision notes Dr.Sherif Badrawy
- 790. NSAIDs, selective for COX-2 isoenzyme: 395a Critical Care revision notes Dr.Sherif Badrawy
- 791. a. They significantly↓risk of GI bleeding compared with non-selective NSAIDs.【✔】 b. They cause ↑thromboxane A2 production compared with non-selective NSAIDs.【✔】 c. Rofecoxib > doubles the risk of MI compared with placebo.【✔】➜ ↓prostacyclin in vascular endothelium (which has VD and antiplatelet activity) & ↑thromboxane A2 (pro-aggregatory platelet effects). d. They are < effective analgesics than non-selective NSAIDs.【✘】➜ efficacy of COX-2 agents is among the highest of all NSAIDs. 395b Critical Care revision notes Dr.Sherif Badrawy
- 792. Regarding pharmacokinetics: 396a Critical Care revision notes Dr.Sherif Badrawy
- 793. a. A T1/2 is half the total time taken for the drug to be completely cleared from the plasma.【✘】➜ time taken for its conc to fall by 50%. b. Vd is calculated from plasma conc x dose following an IV bolus of a drug.【✔】 c. Clearance is usually expressed in ml/kg/min.【✘】➜ expressed as ml/min. d. Zero order kinetics implies enzyme saturation.【✔】 396b Critical Care revision notes Dr.Sherif Badrawy
- 794. Which is more potent, Fentanyl or alfentanil ? 397a Critical Care revision notes Dr.Sherif Badrawy
- 795. Fentanyl is more potent than alfentanil (same efficacy with a lower dose) 397b Critical Care revision notes Dr.Sherif Badrawy
- 796. 44-y, M, abdominal sepsis, ICU, renal function deteriorates, requires RRT 398a Critical Care revision notes Dr.Sherif Badrawy
- 797. a. RRT is associated with excess in-hospital mortality.【✔】 b. ARF requiring RRT is an independent risk factor for ↑mortality.【✔】 c. Bleeding complications are MCC of death in ICU pts with ARF.【✘】➜ infection is the MCC here. d. Hospital mortality is around 15% in ICU pts requiring RRT.【✘】 398b Critical Care revision notes Dr.Sherif Badrawy
- 798. A patient on the ICU develops candidaemia following a prolonged period of MV dt abdominal sepsis, C. albicans is isolated in blood and urine cultures. The following are likely to be effective antifungal agents: 399a Critical Care revision notes Dr.Sherif Badrawy
- 799. a. Voriconazole.【✔】 b. Fluconazole.【✔】 c. Caspofungin.【✔】 d. Amphotericin B.【✔】 ✷ NB: continue Rx until 14 days after -ve blood cultures 399b Critical Care revision notes Dr.Sherif Badrawy
- 800. The following are recognised complications of prone positioning in the anaesthetised patient: 400a Critical Care revision notes Dr.Sherif Badrawy
- 801. a. Stroke.【✔】head rotation ➜ vertebral or carotid artery occlusion b. Weakness of hand grip.【✔】➜ dt injury to the brachial plexus (esp with arm extended) c. Macroglossia.【✔】➜ dt ↑venous pressure [excessive flexion of neck ➜ kinking of IJV] d. Blindness.【✔】➜ dt retinal ischaemia dt ↑IOP ➜ ↓intra-orbital perfusion pressure 400b Critical Care revision notes Dr.Sherif Badrawy
- 802. Regarding the persistent vegetative state: 401a Critical Care revision notes Dr.Sherif Badrawy
- 803. a. Prognosis is worse if the cause is metabolic than if it is traumatic.【✔】 b. The GCS is a useful assessment tool.【✘】 c. Neuroimaging is usually normal.【✘】 ➜ widespread cortical and thalamic atrophy in PVS pts progresses with time. d. Life expectancy is normal if appropriate supportive care is provided.【✘】 ➜ mortality of the PVS is 70% at 3 years influenced by complications as pressure sores and infections. 401b Critical Care revision notes Dr.Sherif Badrawy




















































![♧ the fourth power of the radius [NOT to
the square of the radius]
♧ & inversely proportional to the viscosity
of the fluid and the length of the tube
27b
Critical Care revision notes
Dr.Sherif Badrawy](https://image.slidesharecdn.com/criticalcare-revision-notes-160212144759/85/Critical-care-revision-notes-55-320.jpg)

![NO, Used if intravenous access is not
possible, though the
tougher bony cortex makes this difficult
[tibia, sternum and iliac crest]
28b
Critical Care revision notes
Dr.Sherif Badrawy](https://image.slidesharecdn.com/criticalcare-revision-notes-160212144759/85/Critical-care-revision-notes-57-320.jpg)

















































































































































































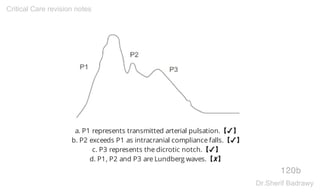











![a. It is comprised of anatomical and
physiological data.【✘】
b. The maximum score is 75.【✔】
c. Head injury carries the highest
weighting.【✘】
d. Six body regions are defined.【✔】
(head, face, chest, abdomen, extremities
[including pelvis], external).
126b
Critical Care revision notes
Dr.Sherif Badrawy](https://image.slidesharecdn.com/criticalcare-revision-notes-160212144759/85/Critical-care-revision-notes-253-320.jpg)



























































![✪ the delivery of a bolus of 15-20ml of cold fluid (<8°C) through a CVC with
temperature-time measurement at an arterial site (usually femoral) with a
thermistor- tipped arterial cannula. The temperature-time curve produced
gives an estimate of COP according to a modified form of the Stewart-Hamilton
equation.
✪ global end-diastolic volume [GEDV] an estimate of preload which may be a
better predictor of fluid requirements than CVP
✪ extravascular lung water EVLW is a measure of pulmonary oedema guide
diuretic therapy a more sensitive marker of pulmonary oedema than chest X-
ray.
✪ Total intrathoracic blood volume can be estimated by transpulmonary
thermodilution, but not total circulating blood volume.
156b
Critical Care revision notes
Dr.Sherif Badrawy](https://image.slidesharecdn.com/criticalcare-revision-notes-160212144759/85/Critical-care-revision-notes-313-320.jpg)














![✪ may occur with either enteral or parenteral nutrition.
✪ ↓serum phosphate ➜ arrhythmias, HF, Wernicke's
encephalopathy, leukocyte and platelet dysfunction
rhabdomyolysis, renal failure and myopathy. All
abnormalities are dt hypophosphataemia, which is a
consequence of ↑insulin [insulin causes cellular uptake of
phosphate ➜ hypophosphataemia].
✪ ↑insulin is dt switch from a starvation state to CHO
metabolism.
164b
Critical Care revision notes
Dr.Sherif Badrawy](https://image.slidesharecdn.com/criticalcare-revision-notes-160212144759/85/Critical-care-revision-notes-329-320.jpg)































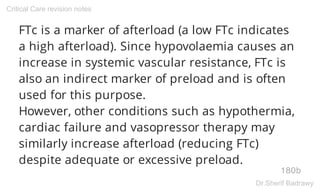




































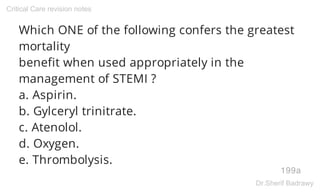




































![✲ It is 98% protein-bound.
✲ It does not require dose adjustment in renal
failure.
✲ It has effect on heart rate even if the patient
is in sinus rhythm.[causes a 15% reduction in
heart rate of patients in sinus rhythm]
✲ It has a volume of distribution up to 70L/kg.
✲ It potentiates the effect of warfarin.
217b
Critical Care revision notes
Dr.Sherif Badrawy](https://image.slidesharecdn.com/criticalcare-revision-notes-160212144759/85/Critical-care-revision-notes-435-320.jpg)















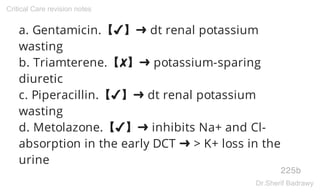

















![a. A nitrate infusion should be started to relieve the chest
pain.【✘】➜ may precipitate profound hypotension
b. A fluid challenge of 500-1000ml should be given.【✔】
c. A posterior myocardial infarction is the likely diagnosis.
【✘】➜ right ventricular infarction [↑ST in lead V4R is
highly sensitive and specific for RV infarction].
d. Thrombolysis is contraindicated.【✘】
234b
Critical Care revision notes
Dr.Sherif Badrawy](https://image.slidesharecdn.com/criticalcare-revision-notes-160212144759/85/Critical-care-revision-notes-469-320.jpg)
![RTA, a liver laceration, During laparotomy
extensive bleeding + 15-unit blood transfusion,
MV, ICU, progressively worsening lung
compliance and hypoxaemia
(PaO2 9kPa [68mmHg] on 80% FIO2), over the
next few hours. Chest X-ray shows widespread
fluffy
infiltrates; the PAOP is 15mmHg.
235a
Critical Care revision notes
Dr.Sherif Badrawy](https://image.slidesharecdn.com/criticalcare-revision-notes-160212144759/85/Critical-care-revision-notes-470-320.jpg)



















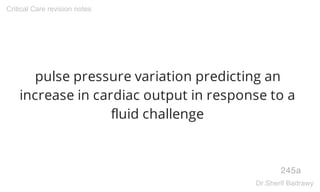
















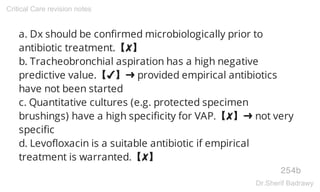






































![The following are elements of the 6-hour
sepsis resuscitation care bundle as
advocated by the Surviving Sepsis
Campaign group: [two 'sepsis care
bundles' to be implemented within 6 and
24 hours of the recognition of a septic
patient]
274a
Critical Care revision notes
Dr.Sherif Badrawy](https://image.slidesharecdn.com/criticalcare-revision-notes-160212144759/85/Critical-care-revision-notes-548-320.jpg)



































![features of the abdominal compartment
syndrome?
[a combination of intra-abdominal
hypertension and end-organ dysfunction,
with reversal of this organ dysfunction on
relief of the pressure].
292a
Critical Care revision notes
Dr.Sherif Badrawy](https://image.slidesharecdn.com/criticalcare-revision-notes-160212144759/85/Critical-care-revision-notes-584-320.jpg)


















![✯ Cardiac output (Q) = VO2/Arterial O2
content - mixed venous O2 content
✯ CaO2 [Arterial O2 content] =
1.39 x [Hb] x (SaO2/100) + 0.023 x PaO2
(Hb in g/dL, PaO2 in kPa)
301b
Critical Care revision notes
Dr.Sherif Badrawy](https://image.slidesharecdn.com/criticalcare-revision-notes-160212144759/85/Critical-care-revision-notes-603-320.jpg)










































![✯ Candida in urine culture ➜ NO Rx unless isolated from multiple
sites,consider Rx if high levels are present (> (10)4cfu/ml), signs of infection are
present, and no other source of infection is apparent.
✯ Pyuria [>10 WBCs/ml urine]. alone not mandate antibiotic Rx, search for
urinary pathogens. Non-infectious causes of pyuria as recent antibiotic Rx,
systemic inflammatory conditions, nephrolithiasis and drugs [CST].
✯ Urine culture >(10)3 CFU/ml bacteria ➜ antibiotic Rx only in the presence of
clinical indicators of infection and may represent simple colonisation if such
indicators are absent.
✯ Positive urine dipstick for leukocyte esterase and/or nitrate ➜ further Ix, it is
not sufficiently specific to justify antibiotic Rx in the absence of supporting
evidence of UTI.
323b
Critical Care revision notes
Dr.Sherif Badrawy](https://image.slidesharecdn.com/criticalcare-revision-notes-160212144759/85/Critical-care-revision-notes-647-320.jpg)






![Gamma-hydroxybutyrate [derived from
GABA]
327a
Critical Care revision notes
Dr.Sherif Badrawy](https://image.slidesharecdn.com/criticalcare-revision-notes-160212144759/85/Critical-care-revision-notes-654-320.jpg)
















![✯ uncomplicated cases oral metronidazole DOCH, effective
and cheap
✯ Stop the antibiotic associated with the outbreak
[quinolones, clindamycin and cephalosporins]
✯ ileus is present ➜ oral metronidazole or vancomycin is
ineffective ➜ Use IV metronidazole [IV vancomycin is of no use
since it does not penetrate the large bowel in sufficient dose]
✯ Probiotics ➜ weak evidence
✯ IV immunoglobulin ➜ effective in small case series, for
refractory cases if antibiotic therapy is unsuccessful. It is not a
first-line treatment
335b
Critical Care revision notes
Dr.Sherif Badrawy](https://image.slidesharecdn.com/criticalcare-revision-notes-160212144759/85/Critical-care-revision-notes-671-320.jpg)

![✯ Voriconazole ➜ QT prolongation in susceptible individuals
[patient on amiodarone]
✯ Amphotericin B ➜ wide spectrum of activity, effective
against most Candida ➜ renal impairment
✯ Fluconazole ➜ effective against C. albicans but less so
against other forms of Candida including C. glabrata which is
resistant in 60%
✯ Nystatin ➜ Rx of C. albicans of the skin and mm, but not for
systemic candidiasis
✯ Caspofungin ➜ a broad spectrum of activity suitable for
invasive Candida and Aspergillus
336b
Critical Care revision notes
Dr.Sherif Badrawy](https://image.slidesharecdn.com/criticalcare-revision-notes-160212144759/85/Critical-care-revision-notes-673-320.jpg)







![the principle of doing the greatest good for
the greatest number of patients with the
resources available; [ the obligation to
provide a net balance of benefits over
harms with limited resources], a subset of
beneficence
340b
Critical Care revision notes
Dr.Sherif Badrawy](https://image.slidesharecdn.com/criticalcare-revision-notes-160212144759/85/Critical-care-revision-notes-681-320.jpg)






































































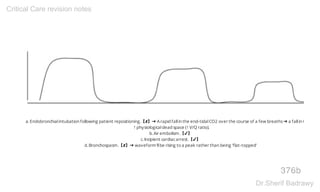


![55-y, M, massive haemoptysis [500ml blood
over a 3-h], several minor episodes of
haemoptysis over the last few months, BP
90/70, HR of 100, SpO2 of 85% on 15L/min
oxygen NRBM,
378a
Critical Care revision notes
Dr.Sherif Badrawy](https://image.slidesharecdn.com/criticalcare-revision-notes-160212144759/85/Critical-care-revision-notes-756-320.jpg)










![a. CT brain scan is likely to be a useful Ix in this case.
【✔】➜ MRI occasionally if CT fails to make Dx.
b. IV empirical antibiotics are indicated.【✔】 ➜ location of
the cavernous sinuses and their extensive venous
connections vulnerable to septic thrombi [MCC
Staphylococcus aureus]
c. Mortality is 80-100%.【✘】This is In the pre-antibiotic
era, now ~20% with appropriate antimicrobial Rx.
d. Cavernous sinus thrombosis is the MCC of cerebral
venous sinus thrombosis.【✘】
383b
Critical Care revision notes
Dr.Sherif Badrawy](https://image.slidesharecdn.com/criticalcare-revision-notes-160212144759/85/Critical-care-revision-notes-767-320.jpg)



![a. Red cell casts are always pathological.【✔】
b. A negative nitrite dipstick effectively excludes the
presence of bacteria in the urine.【✘】➜ Although 90% of
common urinary pathogens are nitrite-forming, [NOT
Pseudomonas, Staph albus, Staph saprophyticus,
Strept faecalis]
c. Hyaline casts are suggestive of bacterial endocarditis.
【✘】➜ Tamm-Horsfall glycoprotein, common in healthy
individuals.
d. White cell casts are a normal finding.【✘】➜
proliferative GN, AIN & acute PN.
385b
Critical Care revision notes
Dr.Sherif Badrawy](https://image.slidesharecdn.com/criticalcare-revision-notes-160212144759/85/Critical-care-revision-notes-771-320.jpg)


![74-y, M, biliary tract sepsis, ICU, Over 3
days ➜ marked abdominal distension, X-
ray ➜ dilatation of the large bowel,
features favour Dx acute intestinal pseudo-
obstruction [Ogilvie's syndrome] over
mechanical obstruction:
387a
Critical Care revision notes
Dr.Sherif Badrawy](https://image.slidesharecdn.com/criticalcare-revision-notes-160212144759/85/Critical-care-revision-notes-774-320.jpg)


























![a. Stroke.【✔】head rotation ➜ vertebral or
carotid artery occlusion
b. Weakness of hand grip.【✔】➜ dt injury to
the brachial plexus (esp with arm extended)
c. Macroglossia.【✔】➜ dt ↑venous pressure
[excessive flexion of neck ➜ kinking of IJV]
d. Blindness.【✔】➜ dt retinal ischaemia dt
↑IOP ➜ ↓intra-orbital perfusion pressure
400b
Critical Care revision notes
Dr.Sherif Badrawy](https://image.slidesharecdn.com/criticalcare-revision-notes-160212144759/85/Critical-care-revision-notes-801-320.jpg)

