Difficult airway
- 1. MANAGEMENT OF DIFFICULT AIRWAY ATUL KUMAR
- 2. DIFFICULT AIRWAY: DEFINITIONS DIFFICULT AIRWAY: A clinical situation in which a conventionally trained anaesthesiologist experiences difficulty with mask ventilation, difficulty with tracheal intubation or both Difficult airway: spectrum Difficult : Spontaneous/mask ventilation Laryngoscopy Tracheal intubation Tracheostomy.
- 3. DIFFICULT MASK VENTILATION – It is not possible for the unassisted anaesthesiologist to maintain SPO2>90% using 100% O2 and positive pressure mask ventilation in a patient whose SPO2 was > 90% before anaesthetic intervention and/or It is not possible for the unassisted anesthesiologist to prevent or reverse signs of inadequate ventilation during positive pressure mask ventilation. . Absent or inadequate chest movement. Absent breath sounds. Gastric air entry or dilatation. Cyanosis. Haemodynamic changes due to hypoxia or hypercarbia. Decreasing oxygen saturation. Absent or inadequate exhaled CO2 Signs of inadequate mask ventilation
- 4. Predictors of Difficult Mask Ventilation (mnemonic BONES ) Beard Obesity with BMI > 26 kg/m 2 No teeth Elderly > 55years Snorers patients having 2 or more of the above predictors likely to have difficult mask ventilation. DIFFICULT LARYNGOSCOPY- It is not possible to visualize any portion of the vocal cords with conventional laryngoscopy. DIFFICULT ENDOTRACHEAL INTUBATION : Using conventional laryngoscopy, it requires>3 attempts to insert an ETT and/or the insertion of an ETT requires> 10 min. using conventional laryngoscopy
- 5. BEST ATTEMPT LARYNGOSCOPY Laryngoscopy performed by reasonably experienced laryngoscopist with the pt in optimal sniff position having no significant muscle tone & the laryngoscopist has an option of change of blade type & length.
- 6. Degree of difficult mask ventilation Easy chin lift only ( zero) One person jaw thrust / mask seal. As above + oropharyngeal or nasopharyngeal airway or both. Two person jaw thrust / mask seal. Two person jaw thrust / mask seal + airway. Impossible mask ventilation despite maximal external effort & full use of airway (infinite)
- 7. Degree of difficult tracheal intubation Easy endotracheal intubation ( zero) One attempt, increasing lifting force. As above + use better sniff position Multiple attempts,external laryngeal pressure and multiple blades. As above + multiple attempt by the laryngoscopist. Impossible to intubate despite above maneuvers and using multiple blades. ( infinite)
- 8. Indication For Interruption Of Tracheal Intubation Intubation attempt if exceeds 30 seconds Cyanosis or pallor if develops Change in heart rhythm if occurs Patient if developed significant hypoxia.
- 9. Causes of difficult intubation Anaesthesiologist : Inadequate preoperative assessment Inadequate equipment preparation Inexperience Poor technique Equipment : Malfunction / Unavailability Patient : Congenital & acquired causes.
- 10. CAUSES OF DIFFICULT INTUBATION Pierre Robin Syndrome Micrographia, Macroglossia, Cleft soft palate Treacher Collins Syndrome Auricular & ocular defect, molar & mandibular hypoplasia. Goldenhar’s Syndrome Auricular and ocular defects, molar and mandibular hypoplasia; occipitalization of atlas. Down’s Syndrome Poorly developed or absent bridge of the nose, macroglossia Kilppel-Feil Syndrome Congenital fusion of a variable number of cervical vertebrae; restriction of neck movement.
- 11. ACQUIRED Infections Supraglottitis Croup Abscess Ludwig’s angina Laryngeal oedema Laryngeal oedema Distortion of the airway and trismus Distortion of the airway and trismus. Arthritis Larynx, Rheumatoid Arthritis Ankylosing spondylitis TMJ ankylosis, cricoarytenoid, deviation of restricted mobility of Cervical spine. Ankylosis of cervical spine, less commonly ankylosis of TMJ; lack of mobility of cervical spine. Tumour Benign Tumor Malignant Tumor Stenosis or distortion of the airway Fixation of larynx to adjacent tissues. Trauma Oedema of airway, unstable#, haematoma Obesity Short thick neck, sleep apnoea Acromegaly Macroglossia, Prognanthism Acute Burns Oedema of airway
- 12. Assessment of Difficult Airway History General physical examination Specific tests for assessment Difficult mask ventilation Difficult laryngoscopy Difficult surgical airway access Radiologic assessment
- 13. AIRWAY ANATOMY
- 15. History Congenital airway abnormalities: e.g. Pierre Robin, Klippel-Feil, Down’s syndromes Acquired Rheumatoid arthritis, Acromegaly, Benign and malignant tumors of tongue, larynx etc. Iatrogenic Oral/pharyngeal radiotherapy, Laryngeal/tracheal surgery, TMJ surgery. Reported previous anaesthetic problems Dental damage, Emergency tracheostomy, Med-alerts from the previous record etc.
- 16. GENERAL EXAMINATION Adverse anatomical features : e.g. small mouth, receding chin, high arched palate, large tongue, morbid obesity Mechanical limitation : reduced mouth opening, post-radiotherapy fibrosis, poor cervical spine movement Poor dentition : Prominent/loose teeth Orthopaedic/orthodontic equipment . Patency of the nasal passage Basic categories Evaluation of tongue size relative to pharynx Mandibular space Assesment of glottic opening. Mobility of the joints TMJ Neck mobility AIRWAY EVALUATION
- 17. Airway assessment indices Individual indices. Group indices - Wilson’s score - Benumof’s analysis - Saghei & safavi test - Lemon assesment etc 3. Radiological indices
- 18. MALLAMPATI TEST Patient in sitting position Head in neutral position Maximal tongue protrusion No phonation SAMPSOON-YOUNG’S MODIFICATION ( 1987 ) added Class IV and correlated b/w ability to observe intraoral strucures and incidence of subsequent difficult intubations. Visualisation of any part of epiglottis during MMP test Associated with easy laryngoscopy Difficult airway possible large epiglottis hinder laryngoscopic view as well as ventilation CLASS ZERO MALLAMPATI
- 20. SIGNIFICANCE OF MMP SCORE Class III or IV : signifies that the angle between the base of tongue and laryngeal inlet is more acute and not conducive for easy laryngoscopy Limitations Poor interobserver reliability Limited accuracy Good predictor in pregnancy, obesity, acromegaly
- 21. EVALUATION OF MANDIBULAR SPACE THYROMENTAL DISTANCE (PATIL’S TEST) Distance from the tip of thyroid cartilage to the tip of inside of the mentum. Neck fully extended / mouth closed Significance Negative result – the larynx is reasonably anterior to the base of tongue > 6.5 cm-> No problem with laryngoscopy & intubation 6 – 6.5 cm -> Difficult laryngoscopy but possible < 6 cm -> Laryngoscopy may be impossible
- 22. Limitations Little reliability in prediction Variation according to height, ethnicity Modification to improve the accuracy Ratio of height to thyromental distance (RHTMD) Useful bedside screening test RHTMD > 23.5 – very sensitive predictor of difficult laryngoscopy Thyromental Distance PATIL’S TEST
- 23. HYO MENTAL DISTANCE Distance between mentum and hyoid bone Grade I : > 6cm Grade II: 4 – 6cm Grade III : < 4cm – Impossible laryngoscopy & Intubation
- 24. STERNOMENTAL DISTANCE (SAVVA TEST) Distance from the upper border of the manubrium to the tip of mentum, neck fully extended, mouth closed Minimal acceptable value – 12.5 cm Single best predictor of difficult laryngoscopy and intubation ( Has high sensitivity & specificity).
- 25. CORMACK - LEHANE Grading at direct laryngoscopy Grade 1: Full exposure of glottis (anterior + posterior commissure) Grade 2: Anterior commissure not visualised Grade3: Epiglottis only Grade 4: No glottic structure visible.
- 27. ASSESSMENT OF TMJ FUNCTION TM joint exhibits 2 function. Rotation of the condyle in the s.cavity. Forward displacement of the condyle. First movement is responsible for 2-3cm mouth opening & the second is responsible for further 2-3cm mouth opening. Index finger is placed in front of the tragus & the thumb is placed in front of the the lower part of the mastoid process. patient is asked to open his mouth as wide as possible. Index finger in front of the tragus can be intented in its space and the thumb can feel the sliding movement of the condyle as the condyle of the mandible slides forward. SUBLUXATION OF THE MANDIBLE
- 28. INTER-INCISOR GAP Inter-incisor distance with maximal mouth opening Normal value > 5 cm / admits 3 fingers. Significance : Positive results: Easy insertion of a 3 cm deep flange of the laryngoscope blade < 3 cm: difficult laryngoscopy < 2 cm: difficult LMA insertion Affected by TMJ and upper cervical spine mobility
- 29. Significance- Class B and C: difficult laryngoscopy
- 30. UPPER LIP BITE /CATCH TEST Class I: Lower incisors can bite the upper lip above vermilion line Class II: can bite the upper lip below vermilion line Class III: cannot bite the upper lip Significance Assessment of mandibular movement and dental architecture Less inter observer variability
- 31. Evaluation of Neck Mobility Patient is asked to hold the head erect, facing directly to the front maximal head extension angle traversed by the occlusal surface of upper teeth( can also measured by goniometer). Minimum 35⁰ extension is possible at AOJ in normal individuals. Attlanto.Occipital.Extension
- 32. Grades 3 and 4 : Difficult laryngoscopy Grading of reduction in A.O.Extension Grade I : > 35° Grade II : 22-34° Grade III : 12-21° Grade IV : < 12° Grade Reduction of A.O.Extension 1 none 2 One third 3 Two third 4 complete
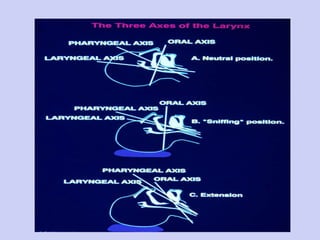
- 33. ASSESMENT OF A.O. EXTENSION can also be done by asking the patient to look at the floor and at wall after fully flexing and fixing the neck as shown Flexion movement of the cervical spine can be assessed by asking the patient to touch his manubrium sternii with his chin. If done, the above maneuver assures a neck flexion of 25- 35 degree. Flexion and the extension movement if within the normal range ,three axis ( oral,pharyngeal & laryngeal axis) can be brought into a straight line.
- 34. Warning sign of DELIKAN Place the index finger of each hand, one underneath the chin and one under the inferior occipital prominence with the head in neutral position. The patient is asked to fully extend the head on neck. If the finger under the chin is seen to be higher than the other, there would appear to be no difficulty with intubation. If level of both fingers remains same or the chin finger remains lower than the other, increased difficulty is predicted.
- 35. PALM PRINT & PRAYER SIGN Palm print sign: Patient’s fingers and palms painted with blue ink and pressed firmly against a white paper Grade 1- all phalangeal areas visible Grade 2- deficient interphalangeal areas of 4th and 5th digits Grade 3- deficient interphalangeal areas of 2nd to 5th digits Grade 4- only tips seen. Prayer sign. Limited-mobility joint syndrome (stiff-joint sydrome) 30-40% of Type I diabetics positive "prayer sign“. TM joint and C-spine (e.g. atlanto-occipital joint) may be involved
- 36. PRAYER SIGN A positive "prayer sign" can be elicited on examination with the patient unable to approximate the palmar surfaces of the phalangeal joints while pressing their hands together; this represents cervical spine immobility and the potential for a difficult endotracheal intubation.
- 37. Palm Print as a Predictor of Difficult Airway in DM
- 38. 1. SAGHEI & SAFAVI’S Weight Tongue protrusion Mouth opening Upper incisor length Mallampati class Head extension Any 3 indices if present - >80kg < 3.2cm <5cm >1.5cm >1 <70 degree Prolonged laryngoscopy Group indices
- 39. 2.“LEMON” Assessment L - Look externally (facial trauma, large incisors, beard, large tongue) E - Evaluate 3-3-2 rule 3 - Inter incisor gap 3 - Hyomental distance 2 - Distance between thyroid cartilage and floor of the mouth. M - MMP score O - Obstruction (epiglottitis, quinsy) N - Neck mobility .
- 40. 3. WILSON SCORING SYSTEM 5 factors - Weight, upper cervical spine mobility, jaw movement, receding mandible, buck teeth Each factor: score 0-2 Total score < 5 – Easy laryngoscopy. 6 to 7 - Moderate difficulty. > 7 - Severe difficulty. IID – Interincisor Gap SL – Maximal Forward Protrusion of Lower incisors beyond upper incisors. Parameter Risk 0 1 2 Weight (kg) < 90 90 – 110 > 110 Head & neck movement > 90 = 90 < 90 IID (cm) SL > 5 > 0 = 5 = 0 < 5 < 0 Receding mandible None Moderate severe Buck teeth None Moderate severe
- 41. 4. BENUMOF’S 11 PARAMETER ANALYSIS Parameter Upper inciors length Buck teeth Subluxation Interincisor gap Palate configuration Mallampati class Minimum acceptable value <1.5cm Absent Yes >3cm No arching/narrowness <2 7. TM distance 8. SMS compliance 9. Neck thickness 10. Length of neck 11. Head /neck mvt > 5cm Soft to palpation. Qualitative ( >33cm DI) >8cm Normal range 2 for mandibular space 3 for neck examination. 4-2-2-3 rule 4 for tooth 2 for inside of mouth
- 42. Rule of 1-2-3 1 finger breadth for subluxation of mandible. 2 finger breatdh for adequacy of mouth opening. 3 finger breathd for hyomental distance. In emergency situation, above test can be rapidly performed within 15sec to assess the TMJ function,mouth opening and SM Space. Significant difficulty in 2 or more of these components requires detailed examination. 4 finger breath for thyromental distance 5 movements- ability to flex the neck upto the manubrium sterni, extension at the AOJ, rotation of the head along with right & left movement of the head to touch the shoulder. Rule of 1-2-3-4-5 3 finger in the interdental space. 3 finger between mentum and hyoid bone. 3 finger between thyroid cartilage & sternum. Significant difficulty in 2 or more of these components requires detailed examination. RULE OF THREE`S
- 43. 1. X-Ray neck (lateral view) : Occiput - C1 spinous process distance< 5mm. Increase in posterior mandible depth > 2.5cm. Ratio of effective mandibular length to its posterior depth <3.6. Tracheal compression. RADIOGRAPHIC PREDICTORS
- 44. 2. CT Scan: Tumors of floor of mouth, pharynx, larynx Cervical spine trauma, inflammation Mediastinal mass 3. Helical CT (3D-reconstruction): Exact location and degree of airway compression Flow volume loop Acoustic response measurement Ultra sound guided CT / MRI Flexible bronchoscope ADVANCED INDICES
- 45. ASA TASK FORCE ON MANAGEMENT OF DIFFICULT AIRWAY Basic preparation Inform Ascertain help Preoxygenation Supplemental oxygenation throughout Portable storage unit Rigid laryngoscope blades ETTs ETT guides/bougie LMAs FOI equipments Retrograde intubation kit Emergency non invasive airway ventilation device. Emergency invasive airway access Exhaled CO2 detector
- 46. Plan “A”: (ALTERNATE) Different length of blade Different type of blade Different position Bougie or lightwand guided Call for help Best attempt laryngoscopy Plans “A”, “B” and “C” What are we going to do if we don’t get the Tube placement??
- 47. Plan “B”: (BVM and other ventilation Techniques ) Can we Ventilate with a BVM? (Consider two NPA’s or a OPA, gentle Ventilation) Two person ventilation? LMA an Option? Or other supraglottic airway ? ILMA? Combi-Tube? Retrograde Intubation? we should have an assistant at this stage
- 48. What do we do when faced with a Can’t Intubate,Can’t Ventilate situation? Plan “C” Needle, Surgical cricothyroidectomy TTJV Tracheostomy Try to wake up the patient from the time we fail intubation.
- 50. MANAGEMENT OF DIFFICULT INTUBATION : Correct position of the patient - A pillow (10 cm) should be placed under the head but not under the shoulders. - Morton and colleagues (1989) defined this position as lower neck flexion 35 o and extension of the plane of face 15 o (both angles relative to horizontal plane)
- 52. SIMPLE TECHNIQUES : Pressure on cricothyroid/thyroid cartilage or External laryngeal manipulation. - Knill postulated Backward, Upward and Rightward pressure known as BURP to the thyroid cartilage when the larynx is anterioly placed for improving the view. Stylet : - Elongated metal or plastic rod with a smooth surface and no sharp edges over which an ETT can be passed. - Should be stiff and flexible enough to change the shape and curve of the ETT. - Facilitate intubation by directing the tube tip towards the glottis. Guedel Airways : Gum elastic Bougie or Tube changers.-used by Sir Robert Macintosh (1943) - Elongated;flexible,soft and smooth rods over which the ETT can be passed but these can not alter the shape of ETT. - Useful when the posterior portion of the larynx is barely visible for the epiglottis can not be elevated. It is important to bend the distal end forward after it has been passed through the tracheal tube. The bougie can then be advanced blindly towards the cords and then the tube can be rail-roaded over the bougie. - Hollow bougies are also available for attachment to oxygen
- 53. “ BURP” & “External Laryngeal Manipulation” B ackward, U pward, R ightward P ressure: manipulation of the trachea 90% of the time the best view will be obtained by pressing over the thyroid cartilage Differs from the Sellick Maneuver
- 54. v) Magill forceps : Double angled forceps have grasping ends in the axis of ETT and handle at the right angle. vi) Tube bender forceps (Aillon forceps) : These have unequal limbs which can bend the distal end of the ETT in the desired direction. vii) Flexible lumen finder (Flexguide) : It is designed to be used with right hand after insertion through the ETT. It has a handle thumb ring, inner rod and notched outer tube. The distal tip of the tube can be manoeuvred with the help of the proximal thumb ring. Schroeder Stylet : ix) Laryngoscope blade and handles : Bozzoni invented first laryngoscope in 1805. In 1907 Jackson designed a U-shaped laryngoscope with the aim to divert force away from upper teeth. Two commonly used designs – the curved ( Macintosh ) and the straight ( Miller ) blades. It is essential that the force applied to the laryngoscope handle is directed along the long axis of handle.
- 55. Specialised curved blades 1- Left handed Macintosh blade - for left handed laryngoscopists - For anatomical abnormalities on the right side of the face mouth and oral cavity. 2- Improved vision Macintosh blade 3- Polio Blade – The angle between the blade and the handle is made obtuse. - It is useful in situations when the antero-posterior diameter of the chest is such that insertion of the laryngoscope into the mouth is difficult or impossible.
- 56. Laryngoscope with “stunted” or short handle : useful in obese patients and in patients with large breast. Oxiport Macintosh : It has an oxygen port in the blade allowing oxygen insufflation during intubation attempts. Tull Macintosh : This blade has a suction port. Siker blade : has stainless steel mirrored surface which permits visualisation of an “anterior” larynx. It gives an inverted image. Huffman Prism : Images are real. - Prism should be placed in warm water for 30 sec on anti-fog solution to prevent fogging
- 57. 9. Bullard Laryngoscope : This is a fiber-optic laryngoscope with a built in rigid 90 0 curved blade. It is battery operated Eye piece is attached to the main body of the scope at 45 0 angle. - Useful in mid-facial hypoplasia syndrome and unstable cervical spines.
- 58. McCoy levering Laryngoscope – The tip of the Macintosh blade is hinged (approx. 2.5 cm from the blade tip) and the angle of the hinged portion can be altered by a lever attached to the handle. Shucman-Pro Levering Laryngoscope
- 59. 11. Upsher fibrecoptic laryngoscope – combines fibreoptic round the corner viewing with maneuverability. - The tip of blade is advanced until it comes to rest close to the cords. The tube sits in the semi-enclosed space in the blade. - The variable focus eye piece enables the operator to obtain uninterrupted view of the procedure. The eye piece can be attached to T.V. Camera for teaching purposes.
- 60. 12. Belscope – Long angulated blade with 45 0 bend at midpoint and a detachable prism. - It minimizes damage to teeth, due to angulation – the blade stays away from upper teeth. - It gives a good view of larynx when the macintosh blade gives grade 3 view. 13. Specialised straight blades Racz-Allen blade, Choi blade, Belscope blade, Bainton blade, Guedel blade, Bennett blade, Whitehead blade, Flagg blade, Eversole blade, Snow blade. WU SCOPE
- 61. Glidescope L with video intubating system Truview evo2 Laryngoscope
- 62. AIRTRACH Indirect rigid laryngoscopy Minimum mouth opening required Less hemodynamic stimulation compared to conventional L
- 63. Utilises the paraglossal technique of intubation BONFILS retromolar intubation fibrescope is a 5mm optical, distally curved stylet which can accommodate a 6mm or larger ET tube Permits continous oxygen insufflation Light supplied via remote Xenon source Can be attached to a module with image display
- 64. BLIND NASAL INTUBATION : can be performed in anaesthetised or awake patients. - Position - sniffing the morning air position - A well lubricated nasal tube is gently passed through the most patent nostril. The nasal mucous membrane should be constricted by the use of vasoconstrictor (xylometazoline or any other nasal decongestant). The bevel of the tube should be pointing laterally so as to avoid trauma to choncha. The opposite nostril should be occluded with the mouth shut and the chin lifted forward. The tube is then advanced while listening to the breath sounds, manipulation of thyroid cartilage and at times of head facilitates the alignment of the tube. At times acute flexion of neck may be required if the obstruction occurs during passage of the tube. The tip of the tube may get placed at five positions – 1- Into the trachea 2. Against the anterior commissure 3. In the vallecula at the base of tongue. 4. Laterally into pyriform recess. 5. In the Oesophagus.
- 65. Awake Intubation
- 66. SPECIALIZED TECHNIQUE : 1. Light wand : it has battery handle and copper stylet (about 45 cms) covered in white plastic. As it enters trachea, transilluminated light is seen as bright, circumscribed below cricoid cartilage if it enters esophagus, light is not easily seen. - Once position of light wand is confirmed then the tube is threaded and guided through it.
- 67. Principle Internal reflection - Beam of light entering one end of glass rod will repeated internally reflex off the walls of rod, eventually emerging from other end. Optical lenses – Light that is internally reflected is completely blurred. it is focused with a series of optical lenses. Gold standard for anticipated difficult intubation – any age, any position. Requires good experience. 2. Bronchoscopes : Both rigid and fibreoptic bronchoscopes have been used as an aid to intubation. Flexible fibreoptic intubation . It consists of – A. Insertion tube – Flexible part extending from control section to distal tip of scope. B. Control section – Contain the tip control knob which controls movement of insertion tube. C. Eye piece section. D. Light transmission cord – from external light source to hand of fiberscope. E. Light source.
- 68. ADJUNCTS TO DIFFICULT AIRWAY MANAGEMENT – 1. Nasopharyngeal airway 2. Oesophageal Obturator Airway –By Don Michael and Gordon in 1968. Consist of two parts first 30 cms plastic oesophageal tube occluded at distal end. There are perforation in the tube which are intended to be located in hypopharynx. A large balloon is located at distal end to create a seal in the oesophagus. Second part of the device is face mask with ap inflatable cuff designed to make a tight seal with the face. After lubrication tube is inserted blindly without laryngoscope. Connell’s Nasopharyngeal Airway Esophageal Obturator Airway
- 69. 3. Patils syracuse oral airway- allows fibreoptic intubation 4. Ovassapian fiberoptic intubating airway – Accommodates tracheal tube upto 9 mm diameter. 5. COPA (Cuffed Oropharyngeal airway )- Disposable device that combines a guided airway with an inflatable distal high volume lowpressure cuff and a proximal 15mm adapter. - distal tip should be behind base of tongue
- 70. 6. Pharyngo-tracheal lumen airway - it is double lumen tube consisting of a long tube with a distal cuff (15 cc) designed to be inflated in esophagus and shorter tube that protrudes through the larger tube and past alarge proximal cuff (100 cc) to ventillate the lungs.
- 71. 7. Oesophageal tracheal combi tube (OTC) : - Disposable double lumen tube with a low volume inflatable distal cuff and a larger proximal cuff. - Distal cuff => Oesophagus Proximal cuff => Oropharynx - Ventilation is possible witheither tracheal or esophageal intubation. If it enters oesophagus (common) – Ventilation is through multiple proximal apertures situated above distal cuff. Both cuffs have to be inflated. - If it enters trachea –ventillation is through distal lumen as with a standard tracheal tube.
- 72. LMA classic (standard LMA)
- 73. LMA PROSEAL & LMA SUPREME
- 74. - LMA unique (disposable)
- 75. Is a non cuffed supraglottic device with the shape of the LMA Disposable made of gel ,softer has a gastric drain (ProSeal LMA-like) bite block and an epiglottis blocker 10. I GEL
- 76. 11. Pharyngeal airway Xpress – Curved tube with anatomically shaped gilled distal tip, large oropharyngeal cuff and an open hooded window that allows ventilation. More effective seal than LMA. “ Pharyngeal Express” Airway
- 77. new type of SLA device that does not have a cuff, rather, it has a preformed plastic that fits anatomically to the shape of the pharynx. This device allows one to give positive pressure ventilation to the patient without cuff. This device also contains a chamber (about 50 mls) as storage for regurgitant fluids to collect. 12 .
- 78. Transtracheal Techniques : - Usually a small IV cannula (14/16) is required. It is advisable to keep this fitted with usual 15 mm connector of 3.5 mm endotracheal tube. - The patients should be positioned to achieve maximum extension of neck. Thyroid and cricoid cartilages are identified and the skin overlying the cricothyroid membrane is fixed. A 14 IV needle is inserted through the membrane into the trachea and directed towards carina. The correct intratracheal position is verified by free aspiration of air through a syringe containing saline. - Begin with 5 psi and increase in increments of 5 psi until adequate chest excursion occurs. - No more than 25 psi and no more than half a second inspiratory time. Emergency tracheostomy : - It is always better to oxygenate the patient via transtracheal I.V. cannula while also performing tracheostomy. - Percutaneous dilatational tracheostomy (PCDT) takes time and is usually not recommended where urgency is there –
- 79. Minitracheostomy is preferred. A single vertical incision 3-5 mm in length over cricothyroid membrane is made and then through obturator the 4 mm uncuffed tracheal tube is guided. Compared with I.V. cannula the minitrach has larger diameter and is better for jet ventilation and even for assisted spontaneous respiration for a short period. MINI TRACHEOSTOMY
- 81. Cricothyrotomy Quicktrach I Standard-Set Available for adults (I.D. 4mm children (I.D. 2mm) and infants (I.D. 1.5mm) Quicktrach II with cuff Set with cuff Thin cuff seals trachea and allows efficient ventilation with aspiration protection. Stopper and safety clip reduce the risk of posterior tracheal wall injury. Anatomically shaped cannula adjusts to the trachea due to “memory effect”. Available for adults (I.D. 4mm)
- 82. Confirm the airway Technology Based ETCO2 (monitor) EDD (bulb) Colormetric (cap) Pulse Ox change METHODS OF CONFIRMATION Traditional Direct Visualization Lung Sounds Tube Condensation
- 83. Causes of difficult intubation in PREGNANCY 1….. MMP Class 3 or 4 2….Supraglottic and glottic areas oedema. 3….Large breasts. 4….Full dentition. 5….Mucosal congestion of nose, pharynx,etc. 6….Enlargement of tongue. 7….Fat deposition in oropharyngeal region. 8….Elevation of hyoid bone. 9…..Weight gain. 10…Improperly applied cricoid pressure. 11…Improperly applied hip wedge causes decreased chin – chest distance.
- 84. Difficult airway : OBESITY Difficult spontaneous ventilation in obstructive sleep apnea BMI > 26 – predicts difficult mask ventilation Difficult intubation predictors- MMP Score >3 Neck circumference > 16 inches
- 85. Positioning for morbidly obese patient
- 86. Whelan - Calicott position
- 87. AIRWAY MANAGEMENT IN TRAUMA RSI involves 4 experienced personnel AMPLE history Allergies Medication Past medical history time of Last meal Events leading No definition of safe cervical spine movement Equipment option depend on operator experience & skill Manual in-line stabilization Airway interventions requiring less neck movement Jaw-thrust (ventilation) Adjunctive device ILMA, combitube Cricothyrotomy Least movement (0.1 mm) with fibre optic nasal intubation CERVICAL SPINE INJURY: MANAGEMENT OPTIONS
- 88. Airway management in trauma
- 89. EXTUBATION STRATEGIES Cuff leak test Performed in a spontaneously ventilating patient at risk of obstruction after extubation. Circuit disconnected occlusion of ETT end and deflation of cuff ability to breath around the ETT. Conventional awake extubation Extubation over a bougie. Extubation over a fibreoptic bronchoscope. Endotracheal ventilation and exchange catheters e.g. Cook’s airway exchange catheter Tracheal tube exchanger
- 90. Do`s in the management of difficult airway Use antisialogue in premedication. Aspiration prophylaxis. ET of assorted size. LMA of assorted size. Tracheostomy set. Check special airway equipment. Keep help of senior anaesthesiologist. Preoxygenate patient / End tidal CO2 device.
- 91. Dont`s in the management of difficult airway Dont produce deep plane of anaesthesia. Dont use technique that you are not familiar. Avoid multiple attempts. Dont render the patient apnoeic, unless you are certain that mask ventilation can be maintained
- 92. THANK YOU