Copd and anaesthetic management
- 2. INTRODUCTION DEFINATION RISK FACTORS PATHOGENESIS PATHOPHYSIOLOGY CLINICAL FEATURES INVESTIGATION TREATMENT EXACERBATIONS PREPRATION FOR ANAESTHESIA ANESTHETIC TECHNIQUE
- 3. COPD is currently the fourth leading cause of death in the world COPD is projected to be the 3rd leading cause of death by 2020 More than 3 million people died of COPD in 2012 accounting for 6% of all deaths globally. CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- 4. Prevalence of COPD higher in smokers and ex-smokers compared to non-smokers Higher ≥ 40 year group compared to those < 40 Higher in men than women. Globally, the COPD burden is projected to increase in coming decades because of continued exposure to COPD risk factors and aging of the population
- 5. Definition: Disease state characterised by airflow limitation that is not fully reversible The airflow limitation is usually progressive and is associated with an abnormal inflammatory response of the lungs to noxious particles or gases, primarily caused by cigarette smoking CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- 6. Chronic Obstructive Pulmonary Disease (COPD) is a common, preventable and treatable disease that is characterized by persistent respiratory symptoms and airflow limitation that is due to airway and/or alveolar abnormalities usually caused by significant exposure to noxious particles or gases GOLD 2017 REPORT
- 8. Chronic Bronchitis: (Clinical Definition) Chronic productive cough for 3 months in each of 2 successive years in a patient in whom other causes of productive chronic cough have been excluded. Emphysema: (Pathological Definition) The presence of permanent enlargement of the airspaces distal to the terminal bronchioles, accompanied by destruction of their walls and without obvious fibrosis COPD
- 9. COPD: Risk factors Host factors: •Genetic factors: Eg. α1 Antitrypsin Deficiency •Gender : Prevalence more in males. ?Females more susceptible •Airway Hyperresponsiveness Exposures: •Smoking: Most Important Risk Factor •Passive/second hand ,smoking exposure •Occupation •Environmental pollution •Recurrent bronchopulmonary infections
- 10. PATHOGENESIS Tobacco smoke & other noxious gases Inflammatory response in airways Proteinase & Antiproteinase imbalance Oxidative Stress Alpha 1 antitrypsin def.
- 11. PATHOLOGY Pathological changes occur in 4 major areas of lungs:- Large airways Small airways Lung parenchyma Pulmonary vasculature
- 12. Large Airways: (cartilaginous airways >2mm of internal diameter) •Bronchial glands hypertrophy •Goblet cell metaplasia •Airway Wall Changes: •Inflammatory Cells Squamous metaplasia of the airway epithelium Increased smooth muscle and connective tissue Small airways (noncartilaginous airways<2mm internal diameter) •Bronchiolitis •Pathological extension of goblet cells and squamous metaplasia •Inflammatory cells •Fibrosis and increased deposition of collagen in the airway walls Excessive Mucus production Loss of cilia and ciliary dysfunction Airflow limitation and hyperinflation
- 13. Lung parenchyma (respiratory bronchioles, alveoli and capillaries) •Emphysema (abnormal enlargement of air spaces distal to terminal bronchioles) occurs in the parenchyma: 2 Types: Centrilobular and Panlobular •Early microscopic lesion progress to Bullae over time. •Results in significant loss of alveolar attachments, which contributes to peripheral airway collapse •Inflammatory cells Pulmonary Vasculature: •Thickening of the vessel wall and endothelial dysfunction •Increased vascular smooth muscle & inflammatory infiltration of the vessel wall •Collagen deposition and emphysematous destruction of the capillary bed Airflow limitation and hyperinflation •Pulmonary HTN •RV dysfunction (cor Pulmonale)
- 15. PATHOPHYSIOLOGY I. Airway obstruction The major site of obstruction is found in the smaller conducting airway (<2 mm in diameter). Processes contributing to obstruction in the small conducting airway include disruption of the epithelial barrier, interference with mucociliary clearance apparatus that results in accumulation of inflammatory mucous exudates in the small airway lumen, infiltration of the airway walls by inflammatory cells and deposition of connective tissue in the airway wall. Fibrosis surrounding the small airway appears to be a significant contributor. This remodelling and repair thickens the airway walls, reduces lumen calibre and restricts the normal increase in calibre produced by lung inflation.
- 16. Increased resistance of the small conducting airway and increased compliance of the lung as a result of emphysematous destruction, causes the prolonged time constant. This constant is reflected in measurements of the FEV1 and its ratio to forced vital capacity(FEV1/FVC),which are reliable screening tools because they are affected by both airway obstruction and emphysema
- 17. In COPD there is often “air trapping” (increased residual volume and increased ratio of residual volume to total lung capacity) and progressive hyperinflation (increased total lung capacity) late in the disease. Hyperinflation of the thorax during tidal breathing preserves maximum expiratory airflow, because as lung volume increases, elastic recoil pressure increases, and airways enlarge so that airway resistance decreases. Despite compensating for airway obstruction, hyperinflation can push the diaphragm into a flattened position with a number of adverse effects. II. Hyperinflation
- 18. First, by decreasing the zone of apposition between the diaphragm and the abdominal wall, positive abdominal pressure during inspiration is not applied as effectively to the chest wall, hindering rib cage movement and impairing inspiration. Second, because the muscle fibers of the flattened diaphragm are shorter than those of a more normally curved diaphragm, they are less capable of generating inspiratory pressures than normal. Third, the flattened diaphragm (with increased radius of curvature) must generate greater tension to develop the transpulmonary pressure required to produce tidal breathing.
- 19. Auto positive end expiratory pressure [Intrinsic positive end expiratory pressure (PEEPi)] Patients with severe COPD often breathe in a pattern that interrupts expiration before the alveolar pressure has decreased to atmospheric pressure This incomplete expiration is due to a combination of factors which include flow limitation, increased work of respiration and increased airway resistance This interruption leads to an increase of the end‐expiratory lung volume above the FRC. This PEEP in the alveoli at rest has been termed auto‐PEEP or PEEPi.
- 20. III. GAS EXCHANGE Non‐uniform ventilation and ventilation‐perfusion mismatch are characteristics of COPD, due to the heterogenous nature of the disease process within airway and lung parenchyma. Ventilation/ perfusion (V/Q) mismatching causes reduction in PaO2 but shunting is minimal. This finding explains the effectiveness of modest elevation of inspired oxygen in treating hypoxaemia due to COPD. Pao2 usually remains near normal until FEV1 is decreased to 50% of predicted and elevation of PaCO2 is not seen until FEV1 is <25%.
- 21. Hypercapnia, if present, reflects both V/Q mismatching and alveolar hypoventilation, the later resulting from both respiratory muscle dysfunction and increased ventilatory requirements. Pulmonary hypertension severe enough to cause corpulmonale and right heart failure is seen when there is marked decrease in FEV1 <25% along with chronic hypoxaemia PaO2 <55 mm Hg.
- 22. CLINICAL FEATURES Symptoms: Cough: Initially intermittent Present throughout the day Sputum: Tenacious & mucoid Purulent Infection Dyspnoea: Progressively worsens Persistant Physical Examination: Respiratory Signs •Barrel Chest •Pursed lip breathing •Adventitious Rhonchi/Wheeze Systemic Signs •Cyanosis •Neck vein enlargement •Peripheral edema •Liver enlargement •Loss of muscle mass
- 23. PINK PUFFER BLUE BLOATER
- 24. A "pink puffer" is a person where emphysema is the primary underlying pathology. Emphysema results from destruction of the airways distal to the terminal bronchiole which also includes the gradual destruction of the pulmonary capillary bed and thus decreased inability to oxygenate the blood. So, not only is there less surface area for gas exchange, there is also less vascular bed for gas exchange but less ventilation-perfusion mismatch than blue bloaters. PINK PUFFER
- 25. The body then has to compensate by hyperventilation (the "puffer" part). Their arterial blood gases (ABGs) actually are relatively normal because of this compensatory hyperventilation. Eventually, because of the low cardiac output, people afflicted with this disease develop muscle wasting and weight loss. They actually have less hypoxemia (compared to blue bloaters) and appear to have a "pink" complexion and hence "pink puffer"
- 26. A "blue bloater" is a person where the primary underlying lung pathology is chronic bronchitis. Chronic bronchitis is caused by excessive mucus production with airway obstruction resulting from hyperplasia of mucus-producing glands, goblet cell metaplasia, and chronic inflammation around bronchi. BLUE BLOATER
- 27. Unlike emphysema, the pulmonary capillary bed is undamaged. Instead, the body responds to the increased obstruction by decreasing ventilation and increasing cardiac output. There is a dreadful ventilation to perfusion mismatch leading to hypoxemia and polycythemia. In addition, they also have increased carbon dioxide retention (hypercapnia). Because of increasing obstruction, their residual lung volume gradually increases (the "bloating" part). They are hypoxemic/cyanotic because they actually have worse hypoxemia than pink puffers and this manifests as bluish lips and faces-the "blue" part.
- 28. Comparative features of COPD
- 29. INVESTIGATIONS:- 1.PULMONARY FUNCTION TEST: Diagnosis Assessment of severity Following progress Decreased FEV1/FVC Decreased FEF(25-75%) Increased RV
- 31. Normal Trace Showing FEV1 and FVC 1 2 3 4 5 6 1 2 3 4 Volume,liters Time, sec FVC5 1 FEV1 = 4L FVC = 5L FEV1/FVC = 0.8
- 32. Spirometry: Obstructive Disease Volume,liters Time, seconds 5 4 3 2 1 1 2 3 4 5 6 FEV1 = 1.8L FVC = 3.2L FEV1/FVC = 0.56 Normal Obstructive
- 33. Time, seconds FEV1 = 1.9L FVC = 2.0L FEV1/FVC = 0.95 1 2 3 4 5 6 5 4 3 2 1 Spirometry: Restrictive Disease Normal Restrictive Volume,liters
- 34. Measurement Normal Obstructive Restrictive FVC (L) 80% of TLC (4800) FEV1 (L) 80% of FVC FEV1/FVC(%) 75- 85% N to N to FEV25%- 75%(L/sec) 4-5 L/ sec N to Slope of FV curve TLC 6000 ml N to RV 1500 mL RV/TLC(%) 0.25 N
- 35. GOLD Criteria for COPD Severity
- 36. Arterial blood gases and oximetry may demonstrate resting or exertional hypoxemia Arterial blood gases provide additional information about alveolar ventilation and acid-base status by measuring arterial Pco2 and pH. The change in pH with Pco2 is 0.08 units/10 mmHg acutely and 0.03 units/10 mmHg in the chronic state The arterial blood gas is an important component of the evaluation of patients presenting with symptoms of an exacerbation. 2.ARTERIAL BLOOD GAS ANALYSIS
- 37. 3. CHEST RADIOGRAPH: Obvious bullae, paucity of parenchymal markings, or hyper- lucency suggests the presence of emphysema Increased lung volumes and flattening of the diaphragm suggest hyperinflation but do not provide information about chronicity of the changes
- 38. 4. CT SCAN:- Computed tomography (CT) scan is the current definitive test for establishing the presence or absence of emphysema
- 39. 5.ECG Signs of RVH: RAD p Pulmonale in Lead II Predominant R wave in V1-3 RS pattern in precordial leads
- 40. 6.Alpha-1 antitrypsin deficiency (AATD) AATD screening The World Health Organization recommends that all patients with a diagnosis of COPD should be screened once especially in areas with high AATD prevalence. AATD patients are typically < 45 years with panlobular basal emphysema Delay in diagnosis in older AATD patients presents as more typical distribution of emphysema (centrilobular apical). A low concentration (< 20% normal) is highly suggestive of homozygous deficiency.
- 41. 7.Bronchodilator Reversibility Testing Provides the best achievable FEV1 (and FVC) Can be done on first visit if no diagnosis has been made Best done as a planned procedure: pre- and post- bronchodilator tests require a minimum of 15 minutes
- 42. Preparation Tests should be performed when patients are clinically stable and free from respiratory infection Patients should not have taken: inhaled short-acting bronchodilators in the previous six hours long-acting bronchodilator in the previous 12 hours sustained-release theophylline in the previous 24 hours
- 43. Spirometry FEV1 should be measured (minimum twice, within 5% or 150ml) before a bronchodilator is given The bronchodilator should be given by metered dose inhaler through a spacer device or by nebulizer to be certain it has been inhaled The bronchodilator dose should be selected to be high on the dose/response curve
- 44. Spirometry (continued) Possible dosage protocols: 400 µg β2-agonist, or 80-160 µg anticholinergic, or the two combined FEV1 should be measured again: 15 minutes after a short-acting bronchodilator 45 minutes after the combination
- 45. Results An increase in FEV1 that is both greater than 200 ml and 12% above the pre- bronchodilator FEV1 (baseline value) is considered significant
- 46. Flow Volume Curve Expiratory flow rate L/sec Volume (L) FVC Maximum expiratory flow (PEF) Inspiratory flow rate L/sec RVTLC
- 47. Flow Volume Curve Patterns Obstructive and Restrictive Obstructive Severe obstructive Restrictive Volume (L) Expiratoryflowrate Expiratoryflowrate Expiratoryflowrate Volume (L) Volume (L) Steeple pattern, reduced peak flow, rapid fall off Normal shape, normal peak flow, reduced volume Reduced peak flow, scooped out mid-curve
- 49. Combined Assessment of COPD: provides a rubric for combining these assessments to improve management of COPD. • Symptoms: Less Symptoms =(mMRC 0-1 or CAT < 10)=patient is (A) or (C) More Symptoms=(mMRC ≥ 2 or CAT ≥ 10)=patient is (B) or (D) • AirflowLimitation: Low Risk =(GOLD 1 or 2)=patient is (A) or (B) High Risk=(GOLD 3 or 4)=patient is (C) or (D) • Exacerbations: Low Risk: ≤ 1 per year and no hospitalization for exacerbation: patient is (A) or (B) High Risk: ≥ 2 per year or ≥ 1 with hospitalization: patient is (C) or (D) 8. Combined Assessment of COPD:-
- 52. ABCD Assessment Tool Example Consider two patients: Both patients with FEV1 < 30% of predicted Both with CAT scores of 18 But, one with 0 exacerbations in the past year and the other with 3 exacerbations in the past year. Both would have been labelled GOLD D in the prior classification scheme. With the new proposed scheme, the subject with 3 exacerbations in the past year would be labelled GOLD grade 4, group D. The other patient, who has had no exacerbations, would be classified as GOLD grade 4, group B.
- 53. TREATMENT Modifying natural history of Disease: Smoking cessation Long term oxygen therapy Symptomatic: Bronchodilators Antibiotics Others Lung Volume Reduction surgery
- 54. Treatment: Smoking Cessation Need: Most important cause of COPD Major risk factor for atherosclerotic vascular disease, cancer, peptic ulcer and osteoporosis. Quitting smoking slows progressive loss of lung function & reduces symptoms Motivation, Counselling & behavioural support Nicotine replacement Patches chewing gum Inhaler nasal spray lozenges Bupriopion
- 55. Effects of smoking: Respiratory Effects: The irritant smoke decreases ciliary motility and increases sputum production. Thus these patients have a high volume of sputum and decreased ability to clear it effectively Exposure to smoke increases synthesis and release of elastolytic enzymes from alveolar macrophages,causes damage to lung parenchyma Further damage to the lung tissue is probably caused by reactive metabolites of oxygen,such as hydroxyl radicles and hydrogen peroxide,which are usually used by the macrophages to kill microorganisms
- 56. Early in the disease , mild V/Q mismatch,bronchitis and airway hyperactivity are the primary problems. Later these problems are accompained by the hallmarks of COPD:Gas trapping, flattened diaphragmatic configuration(which decreases the diaphragm’s efficiency), and barrel chest deformity Cardiac Effects: Risk factor for development of cardiovascular disease CO decreases Oxygen delivery & increases myocardial work Catecholamine release, coronary vasoconstriction Decreased exercise capacity Other Systems Impairs wound healing
- 57. Smoking cessation and time course of beneficial Effects Time after smoking Physiological Effects 12-24 Hrs Fall in CO & Nicotine levels 48-72 Hrs COHb levels normalise Airway function improves 1-2 Weeks Decreased sputum production 4-6 Weeks PFTs improve 6-8 Weeks Normalisation of Immune function 8-12 Weeks Decreased overall post operative morbidity
- 58. Smoking patients should be advised to smoking 2 months prior to elective operations to maximize the effects of smoking cessation, or for at least 4 weeks to benefit from improved mucociliary function and some reduction in post pulmonary complications. If patient cannot stop smoking for 4 to 8 weeks preoperatively, it is controversial whether they should be advised to stop smoking 24 hours preoperatively. A 24 hour smoking absitnence would allow carboxyhemoglobin levels to fall to normal but may increase the risk of post pulmonary complications
- 59. LONG TERM OXYGEN THERAPY Long-term oxygen therapy(home oxygen therapy) is recommended if the Pao2 <55 mmHg, the hematocrit >55% or there is evidence of cor pulmonale The goal of supplemental oxygen administration is to achieve a Pao2 between 60 and 80 mmHg. This goal can usually be accomplished by delivering oxygen through a nasal cannula at 2L/min. The flow rate of oxygen is titrated as neeeded according to arterial blood gas or pulse oximetry measurements Relief of arterial hypoxemia with supplemental oxygen administration is more effective than any known drug therapy in decreasing pulmonary vascular resistance and pulmonary hypertension and in preventing erythrocytosis
- 61. Symptomatic Measures Bronchodilators: Beta Agonists Anticholinergics Bronchodilators are the mainstay of drug therapy for COPD. Bronchodilators cause only a small increase in FEV1 but may alleviate symptoms by decreasing hyperinflation and dyspnea. COPD is more effectively treated by anticholinergic drugs than by beta2 agonists. Corticosteroids N-Acetyl Cysteine α1 Antitrypsin augmentation Others:Vaccination(influenza vaccine,pneumococcal vaccine)
- 63. COPD: Exacerbations Definition: Exacerbations are episodes of increased dyspnea and cough and change in the amount and character of sputum. They may or may not be accompanied by other signs of illness, including fever, myalgias, and sore throat. Precipitating Causes: Infections: Bacterial, Viral Air pollution exposure Non compliance with LTOT
- 64. ►Classified as: Mild (treated with SABDs only) Moderate (treated with SABDs plus antibiotics and/or oral corticosteroids) or Severe (patient requires hospitalization or visits the emergency room). Severe exacerbations may also be associated with acute respiratory failure. Assessment of Exacerbation Risk
- 65. Treatment Supplemental Oxygen (if SPO2 < 90%) Bronchodilators: Nebulised Beta Agonists, Ipratropium with spacer/MDI Corticosteroids Inhaled, Oral Antibiotics: If change in sputum characteristics Based on local antibiotic resistance Amoxycillin/Clavulamate, Respiratory Flouroquinolones Ventillatory support: NIV, Invasive ventillation
- 67. Anaesthetic Considerations in patients with COPD undergoing surgery: Patient Factors: Advanced age Poor general condition, nutritional status Co morbid conditions HTN Diabetes Heart Disease Obesity Sleep Apnea
- 68. Anaesthetic Considerations in patients with COPD undergoing surgery: Problems due to Disease Exacerbation of Bronchial inflammation d/t Airway instrumentation preoperative airway infection surgery induced immunosuppression increased work of breathing Increased post operative pulmonary complications
- 69. Anaesthetic Considerations in patients with COPD undergoing surgery: Problems due to Anaesthesia: GA decreases lung volumes, promotes V/Q mismatch FRC reduced during anaesthesia Anaesthetic drugs blunt Ventilatory responses to hypoxia & CO2 Postoperative Atelectasis & hypoxemia Postoperative pain limits coughing & lung expansion Problems due to Surgery: Site : most important predictor of Post op complications Duration: > 3 hours Position
- 70. Pre-operative assessment: History: Smoking Cough: Type, Progression, Recent RTI Sputum: Quantity, color, blood Dyspnea Exercise intolerance Occupation, Allergies Symptoms of cardiac or respiratory failure
- 71. Body Habitus:-Obesity/ Malnourished Active infection Sputum- change in quantity, nature Fever Crepitations Respiratory failure Hypercapnia Hypoxia Cyanosis Cor Pulmonale and Right heart failure Dependant edema tender enlarged liver Pulmonary hypertension Loud P2 Right Parasternal heave Tricuspid regurgitation Pre-operative assessment: Examination
- 72. Preoperative Assessment: Investigations Complete Blood count Serum Electrolytes Blood Sugar ECG Arterial Blood Gases Diagnostic Radiology Chest X Ray Spiral CT Preoperative Pulmonary Function Tests-specific and nonspecific tests
- 73. Pre-operative preparation Cessation of smoking Dilation of airways Loosening & Removal of secretions Eradication of infection Recognition of Cor Pulmonale and treatment Improve strength of skeletal muscles – nutrition, exercise Correct electrolyte imbalance Familiarization with respiratory therapy, education, motivation & facilitation of patient care
- 74. Anticholinergics: Block muscarinic receptors Onset of action within 30 Min Ipratropium – MDI:- 17 mcg/puff, 200 puffs/ canister -2-3 puffs every 6hours NEBULIZER:- 0.25mg/ml(0.025%)- 0.25mg every 6hours Ipratropium bromide is generally preferred to the short- acting beta-2-agonists as a first-line agent because of its longer duration of action and absence of sympathomimetic side effects Tiotropium - long lasting Side Effects: Dry Mouth, metallic taste Caution in Prostatism & Glaucoma
- 75. Beta Agonists: Act by increasing cAMP Specific β2 agonist – Salbutamol : oral 2-4 mg/ 0.25 – 0.5 mg i.m /s.c 100-200 μg inhalation muscle tremors, palpitations, throat irritation Terbutaline : oral 5 mg/ 0.25 mg s.c./ 250 μg inhalation Salmeterol : Long acting (12 hrs) 50 μg BD- 200 μg BD
- 76. Methylxathines Mode of Action – inhibition of phospodiesterase,↑ cAMP, cGMP – Bronchodilatation Adenosine receptor antagonism ↑ Ca release from SR Intravenous (Aminophylline, Theophyllin) loading – 5mg/kg Maintenace – 0.5mg/kg/h
- 77. Inhaled Corticosteroids: Anti-inflammatory Restore responsiveness to β2 agonist Reduce severity and frequency of exacerbations Do not alter rate of decline of FEV1 Beclomethasone, Budesonide, Fluticasone
- 79. Choice of anaesthesia depends on the 1. Patient factors(clinical state) 2. Surgical factors(type and duration of procedure)
- 80. Concerns in Regional Anesthesia Neuraxial Techniques: •No significant effect on Respiratory function: Level above T6 not recommended •No interference with airway Avoids bronchospasm •No danger of pneumothorax from N2O Peripheral Nerve Blocks: •Suitable for peripheral limb surgeries •Minimal respiratory effects •Supraclavicular techniques contraindicated in severe pulmonary disease •Interscalene block remains a concern due to ipsilateral phrenic nerve paralysis and loss of sympathetic tone due to stellate ganglion block resulting in bronchospasm
- 81. Concerns in Regional Anesthesia •Thoracic epidural anesthesia using low concentrations of local anaesthetic agents and low doses of opiates suppresses both the afferent nociceptive inputs and the efferent sympathetic output thus preserving the respiratory muscular activity and the HPV response. It also improve ventilatory mechanics resulting in decreased airway resistance, lower work of breathing and better preservation of inspiratory and expiratory capacities allowing lung recruitment manoeuvres and voluntary drainage of secretions
- 82. Concerns in General Anesthesia General anesthetic agents, opiates, myorelaxants as well as mechanical ventilation are known to interfere with the respiratory system The combined effects of the supine position, GA and thoracic/abdominal incision produce an immediate decline in lung volumes with atelectasis formation in the most dependent parts of the lung Pre-oxygenation should be used in any patient who is hypoxic on air before induction. In patients with severe COPD and hypoxia, CPAP during induction may be used to improve the efficacy of pre-oxygenation and reduce the development of atelectasis
- 83. Upper airway instrumentation( e.g tracheal intubation) may trigger vagally-mediated reflex bronchoconstriction thereby promoting the expiratory collapse of the peripheral airways with incomplete lung alveolar emptying To atteunate the bronchoconstrictive reflex due to endotracheal intubation or suctioning, prophylactic treatment with lidocaine(IV or inhaled) and/or a beta2-adrenergic agonist are recommended in COPD patients with bronchospastic response Volatile anaesthetics are useful for maintenance of anaesthesia due to their excellent bronchodilating properties with the possible exception of desflurane. Desflurane may cause irritation of the bronchi and increased airway resistance so there may be an advantage to choosing a less irritating agent such as sevoflurane for induction and emergence in cases of severe airway reactivity
- 84. Emergence from anesthesia with inhalational agents can be prolonged significantly ,especially in patients with significant airway obstruction, because air trapping also traps inhalational agents as they flood out of the body’s compartments into the lungs Nitrous oxide can be administered in combination with a volatile anesthetic. When nitrous oxide is used, there is the potential for passage of this gas into pulmonary bullae. is could lead to enlargement or even rupture of the bullae, resulting in development of a pneumothorax. Another potential disadvantage of nitrous oxide is the limitation on the inspired oxygen concentration that it imposes
- 85. Opioids may be less useful than inhaled anesthetics for maintenance of anesthesia in patients with COPD because they can be associated with prolonged ventilatory depression as a result of their slow rate of metabolism or elimination An endotracheal tube bypasses most of the natural airway humidification system, so humidification of inspired gases and use of low gas flows are needed to keep airway secretions moist
- 86. General anesthesia exceeding 2.5–4 hours has been identified as a strong predictor of PPCs .Indeed, prolonged exposure to general anesthetics alters the immune defenses and gas exchange capacity mainly by depressing the alveolar macrophage function, interfering with surfactant production, slowing of the muco-ciliary clearance and increasing the permeability of the alveolar-capillary barrier Management of ventilation during general anaesthesia should be aimed at reducing the dynamic hyperinflation, PEEPi, and air trapping. Harmful effects of air trapping include hypotension, barotrauma and volume trauma to the lungs, hypercapnia, and acidosis
- 87. Measures to reduce air trapping include use of smaller tidal volumes and lower respiratory rates, with more time for expiration Shortening the inspiratory time increases the peak inspiratory flow thereby facilitating better ventilation of all alveoli Tidal volumes of 6 to 8 mL/kg combined with slow inspiratory flow rates minimize the likelihood of turbulent air flow and help maintain optimal ventilation/perfusion matching Slow respiratory rates (6 to 10 breaths per minute) provide sufficient time for complete exhalation to occur, which is particularly important if air trapping is to be minimized. Slow rates also allow sufficient time for venous return and are less likely to be associated with undesirable degrees of hyperventilation
- 88. Application of external PEEP has been shown to decrease the effort of triggering breaths in patients breathing spontaneously on assisted modes of ventilation. Even during controlled ventilation, external PEEP that is less than or equal to PEEPi, is not found to significantly increase the alveolar pressure Pressure controlled ventilation, by virtue of its decelerating flow reduces peak inspiratory pressure and allows for more uniform distribution of tidal volume and improvement of static and dynamic compliance
- 89. Residual neuromuscular blockade persisting after anesthesia emergence has been incriminated in deficient coughing, depressed hypoxic ventilatory drive and “silent” inhalation of gastric contents Restrictive fluid administration decreases risk of pulmonary oedema, it has been accepted in thoracic surgery and showed good outcomes after major abdominal interventions
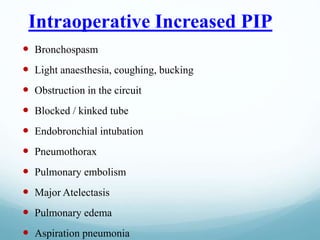
- 90. Intraoperative Increased PIP Bronchospasm Light anaesthesia, coughing, bucking Obstruction in the circuit Blocked / kinked tube Endobronchial intubation Pneumothorax Pulmonary embolism Major Atelectasis Pulmonary edema Aspiration pneumonia
- 91. Bronchospasm during anaesthesia usually manifests as prolonged expiration Expiratory wheeze may be auscultated in the chest or heard in the breathing circuit due to movement of the gas through narrowed airway Breath sounds may be reduced or absent. With intermittent positive pressure ventilation, peak airway pressures are increased, tidal volumes reduced, or both. In severe bronchospasm, wheeze may be quiet or absent due to cessation of movement of air Intraoperative bronchospasm
- 92. With capnography, narrowed airway and prolonged expiration result in a delayed rise in end‐tidal carbon dioxide, producing a characteristic ‘shark fin’ appearance
- 93. Intraoperatively, bronchospasm occurs most commonly during the induction and maintenance stages of anaesthesia and is less often encountered in the emergence and recovery stages Bronchospasm during the induction stage is most commonly caused by airway irritation, often related to intubation. During the maintenance stage of anaesthesia, bronchospasm may result from an anaphylactic or serious allergic reaction. Following endotracheal intubation, wheezing is more likely to occur when barbiturates are used as anaesthetic induction agents, compared with propofol, ketamine or volatile anaesthetics
- 94. Management of intraoperative bronchospa Increase FiO2 Deepen anaesthesia Commonest cause is surgical stimulation under light anaesthesia Relieve mechanical stimulation endotracheal suction Stop surgery β2 agonists – Nebulisation or MDI s/c Terbutaline, iv Adrenaline intravenous Aminophyline:-5mg/kg IV over 20min then 0.5mg/kg/h infusion Intravenous corticosteroid(hydrocortosone 200mg) indicated if severe bronchospasm
- 95. Post Operative Pulmonary Complications: Include: Atelectasis Aspiration pneumonitis Ventilation associated pneumonia Deep vein thrombosis and pulmonary embolism
- 97. Post operative care Mechanical Ventilation: Indications: Severe COPD undergoing major surgery FEV1/FVC<70% Preop PaCO2 > 50mm Hg FiO2 & Ventillator settings adjusted to maintain PaO2 60- 100 mm Hg & PaCO2 in range that maintains pH at7.35- 7.45 Continue Bronchodilators Oxygen therapy Lung Expansion maneuvers
- 100. Post Operative Pulmonary Complications: Post Operative Analgesia: Opioids Paravertebral/Intercostal N Blocks Epidural Analgesia LA Opioids
- 101. Post Operative Pulmonary Complications: Lung Expansion maneuvers: Incentive spirometry Deep breathing exercises Chest Physiotherapy & postural drainage Intermittant Positive Pressure Ventilation CPAP, BiPAP Early Ambulation
- 102. Summary: COPD is a progressive disease with increasing irreversible airway obstruction. Cigarette smoking is the most important causative factor for COPD Smoking cessation & LTOT are the only measures capable of altering the natural history of COPD. COPD is not a contraindication for any particular anaesthsia technique if patients have been appropriately stabilised. COPD patients are prone to develop intraoperative and postoperative pulmonary complications. Preoperative optimisation should include control of infection and wheezing. Postoperative lung expansion maneuvers and adequate post op analgesia have been proven to decrease incidence of post op complications.
- 103. REFERENCES 1) Harrison’s principles of internal medicine-19th edition 2) Robbins Basic Pathology- 9th edition 3) Stoelting’s Anesthesia and coexisting diseases- 2nd south asia edition 4) Clinical anesthesia-Barash, 7th edition 5) COPD: Perioperative management, M.E.J. Anesth 2008 6) Post Operative Pulmonary Complications, IJA April 2006 7) Perioperative Management of patients with COPD: Review, IJ COPD 8) Anaesthesia for patient with chronic obstructive pulmonary disease. Indian J Anaesth 2015 9) http://goldcopd.org
- 104. THANK YOU
- 105. World COPD Day November 16, 2016 http://goldcopd.org/world-copd-day/



















![Auto positive end expiratory pressure [Intrinsic positive end
expiratory pressure (PEEPi)]
Patients with severe COPD often breathe in a pattern
that interrupts expiration before the alveolar pressure has
decreased to atmospheric pressure
This incomplete expiration is due to a combination of
factors which include flow limitation, increased work of
respiration and increased airway resistance
This interruption leads to an increase of the
end‐expiratory lung volume above the FRC. This PEEP
in the alveoli at rest has been termed auto‐PEEP or
PEEPi.](https://image.slidesharecdn.com/copd-170824165721/85/Copd-and-anaesthetic-management-19-320.jpg)