Epistaxis
- 2. Epistaxis Is an acute haemorrhage from the nostril, nasal cavity or nasopharynx. Another name for nose-bleeding. Fairly common and seen in all ages. Presents as an emergency Is a sign not a disease per se.
- 3. Why bleeding from the nose? It is a highly vascularised organ to provide required heating and humidification of incoming air. Vasculature runs just under mucosa (pseudo-stratified ciliated columnar epithelium) Arterial to venous anastomoses
- 4. Blood supply of the nose The nose is supplied by both the external and the internal carotid systems, on both the septum and the lateral walls. Nasal septum – Internal carotid system Supplied by the anterior and posterior ethmoidal arteries, both being branches of the ophthalmic artery.
- 5. Blood supply of the nose Cont….. – External carotid system: Sphenopalatine artery (branch of maxillary artery), gives nasopalatine and posterior nasal septal branches. Septal branch of greater palatine artery (branch of maxillary artery) Septal branch of superior labial artery (branch of facial artery)
- 6. Cont… Lateral walls – Internal carotid system Anterior ethmoidal branches of ophthalmic artery Posterior ethmoidal – External carotid system Posterior lateral nasal → from sphenopalatine artery Greater palatine artery → from maxillary artery Nasal branch of anterior → from infraorbital br. Of superior dental maxillary artery Branches of facial artery to nasal vestibule
- 7. Little’s area It is situated on the anterior inferior part of the nasal septum just above the vestibule. Four arteries- anterior ethmoidal, septal branch of superior labial, septal branch of sphenopalatine and the greater palatine anastomose here to form a vascular plexus called the Kiesselbach’s plexus. This area is exposed to drying effect of inspiratory current and to finger nail trauma and is the usual site for epistaxis in children and young adults Retrocolumellar vein: – This vein runs vertically downwards just behind the columella, crosses the floor of nose and joints venous plexus on the lateral nasal wall. This is a common site of venous bleeding in young people.
- 8. Blood supply of the nose
- 9. Aetiology Classified as: A) Local B) Systemic and C) Idiopathic
- 10. A) Local causes 1. Trauma- finger nail trauma, injuries of the nose, fractures of the middle third of the face and base of skull, hard blowing and violent sneezing.
- 11. Local causes 2. Infections and allergies Acute: viral rhinitis, nasal diphtheria, acute sinusitis. Chronic: all crust forming diseases, atrophic rhinitis, rhinitis sicca, tuberculosis, syphilis septal perforation, granulomatous lession of the nose, e.g. rhinosporidosis
- 12. Local causes… 3. Foreign body – Non-living: any neglected foreign body, rhinolith – Living: maggots, leeches 4. Neoplasm of the nose and paranasal sinuses – Benign: haemangioma and papilloma – Malignant: carcinoma or sarcoma 5. Atmospheric changes: high altitudes, sudden decompression (Caisson’s disease) 6. Deviated nasal septum
- 13. Local causes... Nasopharynx 1. Adenoiditis 2. Juvenile angiofibroma 3. Malignant tumours Carcinoma of the nasopharynx angiofibroma
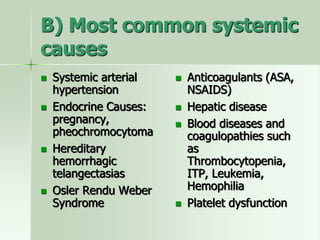
- 14. B) Most common systemic causes Systemic arterial hypertension Endocrine Causes: pregnancy, pheochromocytoma Hereditary hemorrhagic telangectasias Osler Rendu Weber Syndrome Anticoagulants (ASA, NSAIDS) Hepatic disease Blood diseases and coagulopathies such as Thrombocytopenia, ITP, Leukemia, Hemophilia Platelet dysfunction
- 15. C) Idiopathic Many times the cause of epistaxis is not clear.
- 16. Sites of epistaxis 1. Little’s area in 90% of the cases 2. Above the level of middle turbinate 3. Below the level of middle turbinate 4. Posterior part of nasal cavity 5. Diffuse, both from septum and lateral nasal wall 6. Nasopharynx
- 17. Classification of epistaxis Anterior epistaxis Blood comes out through the nostrils Posterior epistaxis – Blood flows back into the throat. – Coffee coloured vomitus
- 18. The differences between anterior and posterior epistaxis Anterior Posterior Incidence and site More common Mostly from the little’s area or anterior part of lateral wall. Less common Mostly from posterior part of nasal cavity. Age Mostly occurs in children and young adults. Occurs after 40 years of age. Cause Mostly trauma or by nasal mucosal dryness. Spontaneous; often due to hypertension or arteriosclerosis. Bleeding Usually mild and can be controlled by local pressure or anterior pack. Bleeding is severe and requires hospitalisation; postnasal pack often required.
- 19. Pathogenesis The pathogenesis of epistaxis is quite various: 1. Local causes; – local traumas (usually a blunt trauma, e.g. a punch, possibly accompanied by a nasal fracture) – exposition to environmental irritants → severe local inflammatory reaction → some local changes, such as vasodilatation, increased permeability, increased blood flow and increased blood pressure → an increased risk of capillary ruptures – frequent use of nasal sprays, in particular corticosteroid nasal sprays reduce inflammation, but they enhance protein catabolism → an increased capillary fragility
- 20. Pathogenesis cont…. 2. Systemic causes; Hypertension → increased risk of capillary ruptures vitamin C deficiency (required for the synthesis of collagen, an important component of connective tissue) → defective connective tissue → fragile capillaries, resulting in abnormal bleeding heart failure (particularly, right-sided failure) → an increase in systemic venous pressure and also in systemic capillary pressure → raises the risk of capillary ruptures
- 21. Cont…. Hyperthermia → an extreme peripheral vasodilatation (in order to increase heat dissipation)→ raised risk of capillary ruptures alcohol → inhibits the vasomotor centre → a persistent peripheral vasodilatation in case of chronic abuse → an increased risk of capillary ruptures Impaired system of coagulation → decreased ability to stop bleeding when a blood vessel is broken.
- 22. Clinical presentation Bleeding from the nose (continuous or intermittent) Haemoptysis Haematemesis Anxiety Shock in severe cases
- 23. Complications Severe bleeding Hypoxia Sinusitis Otitis media Necrosis of the colemulla or nasal ala Haemorrhagic anaemia Possibility of airway obstruction Shock Septal hematoma or abscess Septal perforation
- 24. First aid Trotter’s procedure Make the patient sit up, pinch nose, open mouth and breath. Ice or cold application on the bridges of the nose. Pinching the nose for a minute.
- 25. Diagnosis Laboratory investigations are not usually necessary, although they may be required in certain specific circumstances: – Haematocrit or FBC is obtained if there is concern about anaemia from excessive blood loss or clotting abnormality – Coagulation studies (PT, activated partial thromboplastin time, platelet function tests) are only required in the presence of atypical persistence, recurrence, or recalcitrance to treatment – Urea, serum creatinine, and LFTs are usually only performed if there is concern about the patient's general medical condition. Impaired liver function may result in impaired clotting.
- 26. Cont… Imaging is also not normally necessary but is indicated, following control of bleeding, in specific circumstances: – If a tumour is suspected, MRI of the head is obtained, it has the ability to differentiate between soft tissue of neoplasm versus fluid (e.g., blood or mucus) – CT scan of the paranasal sinuses is the imaging modality of choice when epistaxis is secondary to facial trauma, but it is often unable to differentiate sinusitis from neoplasm
- 27. Cont…. Further specialist investigations for acute epistaxis – Nasal endoscopy and nasopharyngoscopy are indicated when an obvious epistaxis is not seen. – They also provide the opportunity for therapeutic intervention in the form of endonasal cautery or laser ablation.
- 28. Management In any case of epistaxis, it is important to know : 1. Mode of onset. 2. Duration and frequency of bleeding. 3. Amount of blood loss. 4. Side of nose from where bleeding is occurring. 5. Whether bleeding is of anterior or posterior type. 6. Any known bleeding tendency in the patient or family. 7. History of known medical ailment (hypertension, leukaemias, mitral valve disease, cirrhosis, nephritis). 8. History of drug intake ( e.g. analgesics, anticoagulant)
- 29. Treatment of anterior epistaxis Cauterization 1. Chemical Silver Nitrate stick, chromic acid bead. 2. Electrical Use of an electric rod to stop bleeding.
- 30. Anterior nasal packing If bleeding is profuse and/or the site of bleeding is difficult to localise, anterior packing should be done. Ribbon gauze soaked with liquid paraffin One or both cavities may need to be packed. Can be removed after 24 hours if bleeding has stopped. If it has to be kept for 2 to 3 days; systemic antibiotics should be given to prevent sinus infection and toxic shock syndrome
- 32. Treatment of posterior epistaxis Balloon-type epistaxis devices often easiest Foley catheter or other traditional posterior packs
- 33. Posterior nasal packs and balloon device
- 34. Vessel ligation External carotid. Ligation of external carotid artery above the origin of superior thyroid artery. Maxillary artery. Ligation in uncontrollable posterior epistaxis. Ethmoidal arteries. In anteriosuperior bleeding above the middle turbinate.
- 35. Systemic management Antihypertensives Fresh blood transfusion Antibiotics Sedatives
- 36. General measures in epistaxis Make the patient sit up with a back rest and record any blood loss taking place through spitting or vomiting. Reassure the patient. Mild sedation should be given. Keep check on pulse, BP and respiration. Antibiotics may be given to prevent sinusitis, if pack is to be kept beyond 24 hours. Intermittent oxygen may be required in patients with bilateral packs because of increased pulmonary resistance from nasopulmonary reflex. Investigate and treat the patient for any underlying local or general cause.
- 37. Preventive measures Keep allergic rhinitis under control. Use saline nasal spray frequently to cleanse and moisturize the nose. Avoid forceful nose blowing Avoid digital manipulation of the nose with fingers or other objects Use saline-based gel intranasally for mucosal dryness Consider using a humidifier in the bedroom Keep vasoconstricting spray at home to use only prn (pro re nata) epistaxis
- 38. Bibliography Myers T (ed). (2009), Mosby’s Dictionary of Medicine, Nursing and Health Professions, 8th Edn, Canada, Elsevier Mosby Shier.D., Butler. J. and Lewis.R. Hole’s Anatomy and Physiology. (12th edition).New York. McGraw- Hill Publisher Kumar V., Abbas A.K., Fausto N. and Aster J. C. (2010). Robins and Cotran Pathologic Basis of Disease. (8th edn). Philadelphia. Saunders Elsevier.