Fluidelectrolytes
- 1. Fluids, Electrolyte and Nutrition Management in Neonates Dr Varsha Atul Shah Consultant Neonatal and Devt Medicine
- 2. FEN Management in Neonates Essentials of life: – Food (Nutrition) – water (Fluid/electrolyte) – shelter (control of environment - temperature etc) Essentials of neonatal care: – Fluid, electrolyte, nutrition management (All babies) – Control of environment (All babies) – Respiratory /CVS/CNS management (some babies) – Infection management (some babies)
- 3. Why is FEN management important? Many babies in NICU need IV fluids They all don’t need the same IV fluids (either in quantity or composition) If wrong fluids are given, neonatal kidneys are not well equipped to handle them Serious morbidity can result from fluid and electrolyte imbalance
- 4. Fluids and Electrolytes Main priniciples: – Total body water (TBW) = Intracellular fluid (ICF) + Extracellular fluid (ECF) – Extracellular fluid (ECF) = Intravascular fluid (in vessels : plasma, lymph) + Interstitial fluid (between cells) Main goals: – Maintain appropriate ECF volume, – Maintain appropriate ECF and ICF osmolality and ionic concentrations
- 5. Things to consider: Normal changes in TBW, ECF All babies are born with an excess of TBW, mainly ECF, which needs to be removed – Adults are 60% water (20% ECF, 40% ICF) – Term neonates are 75% water (40% ECF, 35% ICF) : lose 5-10 % of weight in first week – Preterm neonates have more water (23 wks: 90%, 60% ECF, 30% ICF): lose 5-15% of weight in first week
- 6. Things to consider: Normal changes in Renal Function Adults can concentrate or dilute urine very well, depending on fluid status Neonates are not able to concentrate or dilute urine as well as adults - at risk for dehydration or fluid overload Renal function matures with increasing: – gestational age – postnatal age
- 7. Things to consider: Insensible water loss (IWL) “Insensible” water loss is water loss that is not obvious (makes sense?): through skin (2/3) or respiratory tract (1/3) – depends on gestational age (more preterm: more IWL) – depends on postnatal age (skin thickens with age: older is better --> less IWL) – also consider losses of other fluids: Stool (diarrhea/ostomy), NG/OG drainage, CSF (ventricular drainage), etc
- 8. Assessment of fluid and electrolyte status History: baby’s F&E status partially reflects mom’s F&E status (Excessive use of oxytocin, hypotonic IVF can cause hyponatremia) Physical Examination: – Weight: reflects TBW. Not very useful for intravascular volume (eg. Long term paralysis and peritonitis can lead to increased body weight and increased interstitial fluid but decreased intravascular volume. Moral : a puffy baby may or may not have adequate fluid where it counts: in his blood vessels)
- 9. Assessment of fluid and electrolyte status (contd.) Physical Examination (contd.) – Skin/Mucosa: Altered skin turgor, sunken AF, dry mucosa, edema etc are not sensitive indicators in babies – Cardiovascular: Tachycardia can result from too much (ECF excess in CHF) or too little ECF (hypovolemia) Delayed capillary refill can result from low cardiac output Hepatomegaly can occur with ECF excess Blood pressure changes very late
- 10. Assessment of fluid and electrolyte status (contd.) Lab evaluation: – Serum electrolytes and plasma osmolarity – Urine output – Urine electrolytes, specific gravity (not very useful if the baby is on diuretics - lasix etc), FENa – Blood urea, serum creatinine (values in the first few days reflect mom’s values, not baby’s) – ABG (low pH and bicarb may indicate poor perfusion)
- 11. Management of F&E Goal: Allow initial loss of ECT over first week (as reflected by wt loss), while maintaining normal intravascular volume and tonicity (as reflected by HR, UOP, lytes, pH). Subsequently, maintain water and electrolyte balance, including requirements for body growth. Individualize approach (no “cook book” is good enough!)
- 12. Management of F&E (contd.) Total fluids required: – TFI = Maintenance requirements (IWL+Urine+Stool water) + growth – In the first few days, IWL is the largest component – Later, solute load increases (80-120 Cal/kg/day = 15-20 mOsm/kg/day => 60-80 ml/kg/day to excrete wastes) – Stool: 5-10 cc/kg/day – Growth: 20-25 cc/kg/day (since wt gain is 70% water)
- 13. Management of F&E (contd.) FLUIDS & ELECTROLYTES Guidelines for fluid therapy Fluids Term PreT ml/kg/d ml/kg/d D1 60 60 D2 90 80 D3 120 100 D4 150 120 D5 150 140 D6 150 150
- 14. Management of F&E (contd.) FLUIDS & ELECTROLYTES Guidelines for fluid therapy Full drip/NBM D1 – Dextrose + 10%CaG 5ml/kg D2 – Dextrose + 10%CaG 2 ml/kg (if N Ca) D3+ - add Na 2 mmol/kg + K 2 mmol/kg Use Calcium Chloride if on inotropes: D1 - Dextrose + 10%CaCl2 2 ml/kg D2 - Dextrose + 0.8 ml/kg (if N Ca) D3+ - add Na 2 mmol/kg + K 2 mmol/kg (1m 20%NaCl=3.4mmol; 1m 7.45%KCl=1mmol)
- 15. Management of F&E (contd.) FLUIDS & ELECTROLYTES Guidelines for fluid therapy •Usually 10% Dex •Preterm <1000g, use 5% Dex •SGA babies may need more fluids. Use 50th centile BW for GA as gauge. •Asphyxiated babies may need fluid restriction.
- 16. Maintenance electrolytes Sodium 2mmol/kg/d 1ml 20% NaCl = 3.4mmol Potassium 2mmol/kg/d1ml 7.45% KCl = 1mmol Calcium 1ml 10% Calcium gluconate = 0.23mmol Ca D1- 5ml/kg 10% Calcium gluconate D2 - 2ml/kg/d (if Ca level is Normal) If Baby on Inotropes: use 10% Ca Chloride D1 - 2 ml/kg; D2 - 0.8 ml/kg (if Ca is N)
- 17. Normal values for Electrolytes Sodium 135-145mmol/l Replacement (mmol) = 2/3 x (deficit from 140) x weight(kg) Potassium 3.5-6.0mmol/l Replacement (mmol) = 2/3 x (deficit from 5.0) x weight(kg)
- 18. Calcium Normal Calcilum 2.27 – 2.79mmol/l Correct if total Ca<2.0 mmol/l or ionic Ca<1.0 mmol/l: 5ml/kg/d 10%Ca Gluconate if on drip On feeds, give Ca Sandoz <2.5kg 2.5ml TDS ≥2.5kg 5ml BD
- 19. Magnesium Normal Magnesium 0.7-0.95 mmol/l Correct if: <0.7mmol/l (symptomatic) <0.55mmol/l (asymptomatic) IM 0.2ml/kg 50%MgSO4 (dilute to 25%)
- 20. Management of F&E (contd.) Factors modifying fluid requirement: – Maturity--> Mature skin --> reduces IWL – Elevated temperature (body/environment)--> increases IWL – Humidity: Higher humidity--> decreases IWL up to 30% (over skin and over respiratory mucosa) – Skin breakdown, skin defects (e.g. omphalocele)--> increases IWL (proportional to area) – Radiant warmer --> increases IWL by 50% – Phototherapy --> increases IWL by 50% – Plastic Heat Shield --> reduces IWL by 10-30%
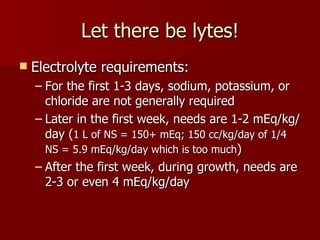
- 21. Let there be lytes! Electrolyte requirements: – For the first 1-3 days, sodium, potassium, or chloride are not generally required – Later in the first week, needs are 1-2 mEq/kg/ day (1 L of NS = 150+ mEq; 150 cc/kg/day of 1/4 NS = 5.9 mEq/kg/day which is too much) – After the first week, during growth, needs are 2-3 or even 4 mEq/kg/day
- 22. F&E in common neonatal conditions RDS: Adequate but not too much fluid. Excess leads to hyponatremia, risk of BPD. Too little leads to hypernatremia, dehydration BPD: Need more calories but fluids are usually restricted: hence the need for “rocket fuel”. If diuretics are used, w/f ‘lyte problems. May need extra calcium. PDA: Avoid fluid overload. If indocin is used, monitor urine output. Asphyxia: May have renal injury or SIADH. Restrict fluids initially, avoid potassium. May need fluid challenge if cause of oliguria is not clear.
- 23. Common ‘lyte problems Sodium: – Hyponatremia (<130 mEq/L; worry if <125) – Hypernatremia (>150 mEq/L; worry if >150) Potassium: – Hypokalemia (<3.5 mEq/L; worry if <3.0) – Hyperkalemia > 6 mEq/L (non-hemolyzed) (worry if >6.5 or if ECG changes ) Calcium: – Hypocalcemia (total<7 mg/dL; i<4) – Hypercalcemia (total>11; i>5)
- 24. Sodium stuff : Hyponatremia Sodium levels often reflect fluid status rather than sodium intake ECF Excess Excess IVF, CHF, Restrict fluids Sepsis, Paralysis ECF Normal Excess IVF, SIADH, Restrict fluids Pain, Opiates ECF Deficit Diuretics, CAH, NEC Increase (third spacing) sodium intake
- 25. Sodium stuff : Hypernatremia Hypernatremia is usually due to excessive IWL in first few days in VLBW infants (micropremies). Increase fluid intake and decrease IWL. Rarely due to excessive hypertonic fluids (sod bicarb in babies with PPHN). Decrease sodium intake.
- 26. Potassium stuff Potassium is mostly intracellular: blood levels do not usually indicate total-body potassium pH affects K+: 0.1 pH change=>0.3-0.6 K+ change (More acid, more K; less acid, less K) ECG affected by both HypoK and HyperK: – Hypok:flat T, prolonged QT, U waves – HyperK: peaked T waves, widened QRS, bradycardia, tachycardia, SVT, V tach, V fib
- 27. Hypo- and Hyper-K Hypokalemia: – Leads to arrhythmias, ileus, lethargy – Due to chronic diuretic use, NG drainage – Treat by giving more potassium slowly Hyperkalemia: – Increased K release from cells following IVH, asphyxia, trauma, IV hemolysis – Decreased K excretion with renal failure, CAH – Medication error very common
- 28. Management of Hyperkalemia Stop all fluids with potassium Calcium gluconate 1-2 cc/kg (10%) IV Sodium bicarbonate 1-2 mEq/kg IV Glucose-insulin combination Lasix (increases excretion over hours) Kayexelate 1 g/kg PR (not with sorbitol! Not to give PO for premies!) Dialysis/ Exchange transfusion
- 29. Calcium stuff At birth, levels are 10-11 mg/dL. Drop normally over 1-2 days to 7.5-8.5 in term babies. Hypocalcemia: – Early onset (first 3 days):Premies, IDM, Asphyxia If asymptomatic, >6.5: Wait it out. Supplement calcium if <6.5 – Late onset (usually end of first week)”High Phosphate” type: Hypoparathyroidism, maternal anticonvulsants, vit. D deficiency etc. Reduce renal phosphate load
- 30. Things we aren’t going to discuss (i.e.) homework: Acid-base disorders: Acidosis or Alkalosis, Metabolic or Respiratory or Mixed Hypercalcemia Magnesium disorders Metabolic disorders Methods of feeding: Continuous vs. Intermittent; TP vs OG vs NG vs NJ; Trophic feeds; Complications of TPN (We can discuss these, if time permits)
- 31. Common fluid problems Oliguria : UOP< 1cc/kg/hr. Prerenal, Renal, or Postrenal causes. Most normal term babies pee by 24-48 hrs. Don’t wait that long in sick l’il babies! Check Baby, urine, FBP. Try fluid challenge, then lasix. Get USG if no response Dehydration: Wt loss, oliguria+, urine sp. gravity >1.012. Correct deficits, then maintenance + ongoing losses Fluid overload: Wt gain, often hyponatremia. Fluid+ sodium restriction
- 32. Nutrition Goals: Normal growth and development (as compared to intrauterine growth for preterm neonates, or as compared to growth charts for term neonates) Nutrient requirements: Energy (Cals) Carbohydrate Water Minerals Protein Vitamins Fat Trace elements
- 33. E=energy required Energy { E = mc 2 m =mass of baby c = cry loudness } Energy needs: depend upon age, weight, maturation, caloric intake, growth rate, activity, thermal environment, and nature of feeds. Growing premies: (Cal/kg/day) – Resting expenditure: 50 – Minimal activity: 4-5 – Occasional cold stress: 10 – Fecal loss (10-15%): 15 – Growth (4.5 Cal/g +): 45 125
- 34. Energy Stressed and sick infants need more energy (e.g. sepsis, surgery) Babies on parenteral nutrition need less energy (less fecal loss of nutrients, no loss for absorption): 70-90 Cal/kg/day+ 2.4-2.8 g/kg/day Protein adequate for growth Count non-protein calories only! Protein to be preferred used for growth, not energy 65% from carbohydrates, 35% from lipids ideal >165-180 Cal/kg/day not useful
- 35. Calculations To calculate a neonate’s F,E,& N: – First calculate the amount of fluid (Water) – Then calculate how you plan to give it: Parenteral (IV) or Enteral (OG/PO) – Then calculate the amount of energy required – Decide how to provide the energy: amount and nature of carbohydrates and lipids – Provide proteins, vitamins, trace elements
- 36. Calculations: practical hints for TPN Do not starve babies! The ones who don’t complain are the ones who need it the most. Use birthweight to calculate intake till birthweight regained, then use daily wt Start TPN on 2nd or 3rd day if the baby will not be on full feeds by a week Start with proteins (1 g/kg/d) and increase slowly. After a few days (3rd or 4th day), add lipids (0.5 kg/kg/ d) Aim for 90-100 Cal/kg/day with 2.5-3 g/kg/d Protein (NPC/N of 150-200)
- 37. Carbohydrate IV: – Dextrose 3.4 Cal/g = 34 Cal/100 cc of D10W. – Tiny babies are less able to tolerate dextrose. If < 1 kg, start at 6 mg/kg/min. If 1-1.5 kg, start at 8 mg/kg/min. – If blood levels >150-180 mg/dL, glucosuria=> osmotic diuresis, dehydration – Insulin can control hyperglycemia – Hyper- or hypo-glycemia => early sign of sepsis – Avoid Dextrose>12.5% through peripheral IV
- 38. Carbohydrate Enteral: – Human milk/ 20 Cal/oz formula = 67 Cal/100 cc – Lactose is carbohydrate in human milk and term formula. Soy and lactose free formula have sucrose, maltodextrins and glucose polymers – Preterm formula has 50% lactose and 50% glucose polymers (lactase level lower in premies, but glycosidases active) 80Cal/100cc – Lactose provides 40-45% of calories in human milk and term formula
- 39. Fat Parenteral: – 20% Intralipid (made from Soybean) better than 10% – High caloric density (2 Cal/cc vs 0.34 for D10W) – Start low, go slow (0.5-3 g/kg/day) – Avoid higher amounts in sepsis, jaundice, severe lung disease – Maintain triglyceride levels of < 150 mg/dL. Decrease infusion if >200-300 mg/dL.
- 40. Fat Enteral: – Approximately 50% of the calories are derived from fat. >60% may lead to ketosis. – Medium-chain triglycerides (MCT) are absorbed directly. Preterm formula have more MCT for this reason. – At least 3% of the total energy should be supplied as EFA
- 41. Protein Term infants need 1.8-2.2 g/kg/day Preterm (VLBW) infants need 3-3.5 g/kg/day (IV or enteral), ELBW 3-4g/kg/day Restrict stressed infants or infants with cholestasis to 1.5 g/kg/day Start early - VLBW neonates may need 1.5-2 g/kg/day by 72 hours Very high protein intakes (>5-6 g/kg/day) may be dangerous Maintain NP Calorie/Protein ratio (at least 25-30:1)
- 42. Minerals (other than Na,K, Cl) Calcium & Phosphorus: – Third trimester Ca accretion (120-150mg/kg/day) and PO4 (75-85 mg/kg/day) is more than available in human milk. Hence, HMF is essential. Premie formula has sufficient Ca/PO4. Ratio should be 1:7:1 by wt. Magnesium: sufficient in human milk & formula Iron: Feed Fe-fortified formula. Start Fe in breast fed term infants at 4 months of age, and in premies once full feeds are reached. (Does not prevent Anemia of Prematurity )
- 43. Vitamins Fat soluble vitamins: A, D, E, K Water soluble vitamins: Vitamins B1,B2, B6, B12, Biotin, Niacin, Pantothenate, Folic acid, Vitamin C All neonates should get vit K at birth Term neonates: No vitamin supplement required, except perhaps vit D Preterm: Start vitamin supplements once full feeds established if on human milk without HMF. No need if on human milk with HMF, or preterm infant formula (except: add vit D if on SSC24).
- 44. Trace elements Zinc, Copper, Selenium, Chromium, manganese, Molybdenum, Iodine Most preterm formulas contain sufficient amounts Fluoride supplementation not required in neonatal period
- 45. Special formula Soy formula: – Not recommended for premies: impaired mineral and protein absorption; low vitamin content – Used if galactosemia, CMPI, secondary lactose intolerance following gastroenteritis Alfare: (Alimentum is similar, but with sucrose) – Hydrolyzed casein; 50% MCT; glucose polymers – Used if malabsorption or short bowel syndrome Portagen: – Casein; 75% glucose polymers+25% sucrose; 85% MCT – Useful for persistent chylothorax. Can cause EFA def.
- 46. Special formula (contd.) Similac PM 60/40: – Low sodium and phosphate; high Ca/PO4 ratio – Used in renal failure, hypoparathyroidism Similac 27: – High energy with more Protein, Ca/Po4, Lytes – Used for fluid restricted infants: CHF, BPD Nutramigen: – Hypoallergenic, lactose and sucrose free – Used for protein allergies, lactose intolerance
- 47. MILK FEEDS F/S(M) 0.67cal/ml F/S(P) 0.8cal/ml EBM 0.67cal/ml Neosure 0.73cal/ml Alfare 0.7cal/ml
- 48. Supplements MCT oil (8cal/ml) Start when iv lipids taken off Max 2ml/kg Start as ¼ml alt feed; ↑ ¼ml/feed after 2-3 days S-26 HMF: max 2 sachets /100ml EBM 0.13cal/ml Similac HMF: max 4 satchets/100ml EBM 0.15cal/ml For EBM, start fortification as half fortification when EBM reaches 100ml/kg and ≥ a week old ↑ Full fortification after 2-3 days
- 49. Iron and Multivitamin Ferrum: start when started on recormon and feeds started & tolerated or <1500g /not on recormon – on D21 5-6mg/kg (1ml Fe=20drops=50mg) Multivitamins: start when off TPN 1ml om