Genus Streptococcus
- 1. Genus Streptococcus Dr Ravi Kant Agrawal, MVSc, PhD Senior Scientist (Veterinary Microbiology) Food Microbiology Laboratory Division of Livestock Products Technology ICAR-Indian Veterinary Research Institute Izatnagar 243122 (UP) India
- 2. Morphology Streptococcus is a genus of Gram-positive cocci or spherical bacteria, that belongs to the family Streptococcaceae, within the order Lactobacillales (lactic acid bacteria), in the phylum Firmicutes. Gram positive spherical or oval cocci arranged in chains or pairs. Chain formation is due to the cocci dividing in one plane only and the daughter cells failing to separate completely The name streptococci was given in 1877 by Viennese surgeon Albert Theodor Billroth (1829–1894). Streptos: easily twisted or coiled; coccus: berry) Individual coccus is 0.5-1.0 μm in diameter. They are non-motile and non-spore forming. Nutritionally fastidious Streptococci are catalase negative Facultative anaerobes but don’t use oxygen metabolically (create lactic acid) Longest chain is produced by Streptococcus salivarius (Commensal) Chains are longer in liquid than in solid media Some strains have capsule composed of hyaluronic acid (non-immunogenic).
- 3. Habitat Normal flora of upper respiratory tract in animals and human – Commensals and Saprophytes of decaying matter Some of them may be pathogens e.g. Streptococcus pyogenes causing pyogenic infections with a tendency to spread unlike staphylococcal infections It produces non-suppurative lesions, acute rheumatic fever and glomerulonephritis which occur as sequelae to infection
- 4. Classification Initial classification based on hemolysis on sheep blood agar plates: α (partial, reduction), β (complete), and γ (none). The cell wall structure of group A streptococci is among the most studied of any bacteria. The cell wall is composed of repeating units of N-acetylglucosamine and N-acetylmuramic acid, the standard peptidoglycan. Rebecca Lancefield (1895-1981) : in 1922 while working for her PhD thesis, Eighteen group- specific antigens were established on basis C Carbohydrate. 1930’s: Lancefield defines cell wall antigen groups Concentrated on virulent, β-hemolytic species Sherman: pyogenic, viridans, enterococci, lactic 1980’s: Enterococci get own genus Lactic acid Streptococci (Lancefield N): New genus Lactococcus Nutritionally variant Streptococci (require pyridoxal): Abiotrophia and Granulicatella Rebecca Craighill Lancefield (1895-1981)
- 5. Classification of Streptococci • Brown`s classification • Lancefield grouping • Griffith typing Brown`s classification Lancefield grouping V
- 6. Hemolysis
- 7. Hemolysis Example – Streptococcus viridans (Viridans = green) Streptococcus pneumoniae Example – enterococcus group
- 8. CLASSIFICATION: StreptococciAerobes & facultative anaerobes Obligate anaerobes Eg: PeptostreptococciBeta haemolytic Gamma haemolytic Eg: Enterococcus group Alpha haemolytic Eg: Viridans streptococci 20 Lancefield groups (ABCDEFGHKLMNOPQRSTUV)80 Griffith types (1,2,3,etc. up to 80) 02 requirement Haemolysis Serological Grouping (C carbohydrate antigen) Group A- Streptococcus pyogens Serological typing (M Protein)
- 9. Serology: Lancefield Classification • Streptococci classified into many groups from A-K & H-V • One or more species per group • Classification based on C- carbohydrate antigen of cell wall – Groupable streptococci • A, B and D (more frequent) • C, G and F (Less frequent) – Non-groupable streptococci • S. pneumoniae (pneumonia) • viridans streptococci – e.g. S. mutans – Causing dental carries Streptococci Group A S. pyogenes Group B S. agalactiae Group C S. equisimitis Group D Enterococcus Lanciefield classification Other groups (E-U)
- 10. Group A Streptococci (GAS) S. pyogenes: Cultural characteristics • Aerobes and facultative anaerobes • Optimum temperature: 37C • Needs enrichment with blood or serum - Growth occurs only in media containing fermentable carbohydrates or enriched with blood or serum i. Blood agar: Small (0.5-1.0 mm), circular, semi-transparent colonies Produce wide zone of β- hemolysis Growth and hemolysis are promoted by 5-10% CO2 Virulent strains, on fresh isolation form lesions, produce a ‘matt’ (finely granular) colony while avirulent strains form ‘glossy’ colonies Mucoid colonies are formed by strains that produce large capsules ii. Liquid media: Glucose or serum broth Growth occurs as a granular turbidity with a powdery deposit No pellicle is formed
- 11. CULTURE: Media used: 1. Non selective media:- Sheep blood agar 2. Selective media:- Crystal violet blood agar PNF medium (Horse blood agar containing polymyxin B sulphate, neomycin sulphate, and fusidic acid inhibited the growth of Staph. aureus, Ps. pyocyanea, Proteus mirabilis, E. coli, and Klebsiella pneumoniae but allowed good growth of, and haemolysis by, Str. pyogenes)
- 12. Biochemical reactions Catalase negative Bile insoluble Ferments sugars producing acid but no gas, faliure to ferment ribose PYR test positive: Hydrolyse pyrrolidonyl-beta- napthylamide (PYR) due to presence of peptidase, the resulting napthylamide produces a red colour upon the addition of 0.01% cinnamaldehyde reagent Bile insoluble Positive Negative PYR test Catalase
- 13. Resistance S. pyogenes is a delicate organism, easily destroyed by heat (54C for 30 min) Sensitive to bacitracin Has developed less resistance to drugs Dies in a few days in culture, unless stored at a low temperature (4C) preferably in Robertson’s cooked meat medium Rapidly inactivated by antiseptics and many antibiotics Fig. Zone of inhibition shown by S. pyogenes
- 14. Antigenic structure Capsular hyaluronic acid: • Non antigenic as hyaluronic acid is identical to that found in human connective tissue and hence bacteria can disguise themselves with an immunological self substance • Has weak anti-phagocytic activity but protects streptococci against immunological attacks
- 15. Antigenic structure A. Cell wall: 1. Outer layer: Protein and lipoteichoic acid 2. Middle layer: Group specific carbohydrate 3. Inner layer: Peptidoglycan (mucoprotein) Responsible for cell wall rigidity Enhances non-specific resistance (pyrogenic and thrombolytic activity) B. Group specific C-carbohydrates Serological grouping of streptococci is done on its basis Divided into 20 Lancefield groups (A to V) except I and J on the basis of group specific carbohydrates. All streptococci except viridans (α-hemolytic) group have a layer of carbohydrate
- 16. C. Proteins Present in outermost layer Produces surface protein antigens (F, M, T and R) Useful in serological typing of S. pyogenes M protein: Most virulent; heat and acid stable, but susceptible to tryptic digestion. 80 types identified. Griffith typing. T protein: Not virulent, acid labile, trypsin resistant. R protein: Not virulent Antigenic structure
- 17. Antigenic structure F-protein Recognizes host fibronectin, a matrix protein that is present in eukaryotic cells. Hence helps in attachment together with lipoteichoic acid and M protein M protein Most antigenic Covered with lipoteichoic acid that enable the organism to attach to epithelial cell M protein is heat and acid stable but susceptible to tryptic digestion On the basis of antigenic difference in M protein, S. pyogenes can be divided into about 100 types The most distal part of M protein shows extensive variability among strains hence individual may suffer from recurrent S. pyogenes infections with strains expressing different versions of M protein. Acts as a virulence factor by inhibiting phagocytosis T-Protein • Common to many M- types • Not associated with virulence and is not a protective antigen • It is strongly antigenic R protein • Non-type-specific and is associated with M- proteins of types 2,3 28 and 48 known as M-associated protein (MAP) • Not associated to virulence and not a protective antigen • Strongly antigenic
- 19. Virulence Factors: Toxins and enzymes Toxins 1. Hemolysins (Streptolysin O and S) 2. Erythrogenic toxin (Pyrogenic Exotoxin) Enzymes: 1. Streptokinase (Fibrinolysin) 2. Deoxyribonucleases (Streptodornase, DNAase) 3. Hyaluronidase 4.NADase 5.Serum opacity factor
- 20. Cytolytic toxins and other exo-enzymes produced by Streptococcus pyogenes
- 21. Hemolysins (Streptolysins) Produce complete disruption of RBC Contribute to tissue invasion and destruction There are two types of Streptolysins Streptolysin O: sensitive to oxygensensitive to oxygen Streptolysin S: insensitive to oxygeninsensitive to oxygen
- 22. Erythrogenic toxin • Also known as pyrogenic exotoxin/ Dick/ Scarlatinal toxin • Primary effect of the toxin is production of fever hence also called Streptococcal pyrogenic exotoxin (SPE) • Known as erythrogenic because its intradermal injection into susceptible individuals produced an erythematous reaction (Dick test) • DICK TEST- Used to identify susceptibility to scarlet fever • Three types of SPE (A,B,C) • Mediate production of rash e.g. (scarlet fever) • SUPERANTIGENS hence massive release of cytokines occur that leads to variety of clinical signs including inflammation, shock and organ failure Fig. Rash in scarlet fever
- 23. Streptokinase (Fibrinolysin) Two types of streptokinase (A and B) Antigenic protein Fibrinolysin facilitates spread of infection by breaking down the fibrin barrier around the lesions also known as spreading factor Promotes the lysis of human blood clot by converting plasminogen to plasmin It is given intravenously for the treatment of early myocardial infarction and other thromboembolic disorders
- 24. Deoxyribonucleases (Streptodornase, DNAase) • Degrades DNA • Four antigenically distinct DNAases: A,B,C,D; B most antigenic • Capable of liquefying DNA accumulated in thick pus derived from nuclei of necrotic cells, hence the exudate is thin in streptococcal infections • Important therapeutically in liquefying localised collections of thick exudates (Empyema) • Demonstration of anti-DNAase B antibody in the diagnosis of S. pyogenes infections when ASO titres is low
- 25. Hyaluronidase • Breaks down hyaluronic acid of connective tissue and favors spread of infection • Antigenic and specific antibodies are formed • Degrades capsule • Others are proteinase, phosphatase, amylase, esterases, NADase, C5a peptidase, lipase, Serum opacity factor (SOP) etc.
- 26. Pathogenicity Produces pyrogenic infection with a tendency to spread locally, along lymphatics and through blood stream Disease caused can be: 1. Suppurative diseases: a. Respiratory infections b.Skin and soft tissue infections c. Genital infections 2. Non suppurative sequelae: a. Acute rheumatic fever b.Acute glomerulonephritis
- 27. Pathogenicity
- 28. Structural components of S. pyogenes that cross react with human tissues Structural components of S. pyogenes Human tissue with which it cross reacts Capsular hyaluronic acid Synovial fluid Cell wall protein Myocardium Cell wall carbohydrtes Cardiac valves Cytoplasmic membrane antigens Vascular intima Peptidoglycans Skin antigens
- 29. Streptococcal Diseases Suppurative Complications 1. Respiratory infections Primary site of invasion is throat causing SORE THROAT May be localized as tonsillitis or pharyngitis Lipoteichoic acid covering surface pili binds to the glycoprotein fibronectin on epithelial cells of pharynx From the throat, spreads to surrounding tissues leading to suppurative complications like Otitis media Mastoiditis Quinsy Suppurative adenitis Meningitis (rare) (it is an inflammation of the mucosal lining of the mastoid antrum and mastoid air cell system inside[1] the mastoid process. The mastoid process is the portion of the temporal bone of the skull that is behind the ear which contains open, air-containing spaces. (Peritonsillar abscess (PTA), also known as a quinsy, is pus due to an infection behind the tonsil). Adenitis is a general term for an inflammation of a gland tonsillitis pharyngitispharyngitis
- 30. 2. Skin and soft tissue infection • S. pyogenes causes subcutaneous infections ranging cellutitis to necrotising fascilitis • Include infections of wounds or burns, with a predilection to produce lymphangitis and cellulitis • Infection of minor abrasions may lead to fatal septicemia • S. pyogenes is also known as ‘FLESH EATING BACTERIA’ - extensive necrosis of subcutaneous and muscular tissue and adjacent fascia – causes Toxic shock like syndrome Quinsy Mastoiditis Pharyngitis Otitis media
- 31. a) Impetigo (Pyoderma) Pyo-purulent and derma-skin Caused by higher numbered M types S. pyrogen Superficial discrete crushed spot of less than one inch in diameter seen in children Lasts for 1-2 weeks and heals spontaneously without any scars b) Erysipelas Erythros: red and pella: skin Hypersensitivity reaction to Streptococcal antigen Causes acute spreading lesions involving superficial lymphatics Affected skin is red, swollen, indurated and sharply demarcated from surrounding healthy skin Rare and seen only in older patients Erysipelas Impetigo
- 32. c) Cellulitis and Necrotising fascilitis Involves deeper subcutaneous tissues Local inflammation and systemic signs like erysipelas are observed Necrotising faciitis : • M types 1 and 3 forming pyrogenic exotoxin A • High fatality • Flesh eating bacteria • Shock, DIC • Treatment with penicillin – not effective • Vancomycin – DOC in life threatening infections Effect of flesh eating bacteria Cellulitis Necrotising fascitis
- 33. 3. Genital infection • Both aerobic and anaerobic Streptococci are normal habitat of female genitalia • Causes puerperal sepsis with exogenous infection • Puerperal fever is caused due to endogenous infection with anaerobic Streptococci Other suppurative infections: Abscesses in brain, lungs, kidney and liver causing septicemia and pyemia
- 34. Non suppurative complications • After a latent period of 1-4 weeks • Followed by rheumatic fever and acute glomerulonephritis
- 35. a) Rheumatic fever • Complication of S. pyogenes pharyngitis due to specific M protein types • Characterized by aschoff nodules (sub cutaneous nodule) • Causes inflammatory myocardial lesion of connective tissue degeneration of heart valves • Results in chronic and progressive damage to heart valves, arthralgias to frank arthritis • Mimics epidemiologic character of streptococcal pharyngitis Aschoff bodies are nodules found in the hearts of individuals with rheumatic fever. They result from inflammation in the heart muscle and are characteristic of rheumatic heart disease.
- 36. b) Glomerulonephritis Caused by specific nephritogenic strains of group A streptococcus Characterized by acute inflammation of renal glomeruli with edema, hypertension, hematuria and proteinuria In contrast with rheumatic fever it is sequela of both pharyngeal and pyodermal streptococcal infection differing in nephrogenic M serotypes Mimics epidemiologic character of streptococcal infection Progressive, irreversible loss of renal function in young is common
- 37. Epidemiology Group A Streptococci causes transient asymptomatic colonization of oropharynx and skin Regulated by ability to mount specific immunity to M protein of colonizing strain and presence of competitive organism in oropharynx Pharyngitis is primarily disease of children (5-15 yrs.), infants and adults are also susceptible Pathogen spreads from respiratory droplets and direct contact especially in winter season Soft tissue infections are proceeded by initial skin colonization to superficial or deep tissue through a break in the skin Re-infection occur due to multiplicity of M protein serotypes
- 38. A) In acute suppurative infectionA) In acute suppurative infection Specimens to be collected: • Throat swab, • Pus, Pus swab • Tissue material, • Blood, • Swab from nose for detection of carriers. Transport media: Pike’s medium 2. Direct Microscopy: Gram-staining of pus can be examined Presence of Gram-positive cocci in chains can be indication. Direct microscopy with Gram stained smear is useful in case of pus & CSF, where cocci in chains are seen. This is of no value for specimen like sputum & genital swabs where mixed flora are normally present. LABORATORY DIAGNOSIS
- 39. Laboratory Diagnosis a. Throat swab culture: Detection of group A antigen b.Specific nucleic acid based test c. Elevation of anti-hyaluronidase antibodies (strong evidence) Culture: Swab from the affected area is collected and are either plated immediately or sent to laboratory in Pike’s medium. The specimen should be plated on blood agar and incubated at 37˚C anaerobically or under 5-10% CO2, as hemolysis develops better.
- 40. Bacitracin sensitivity Bacitracin sensitivity: Based on Maxted’s observation that they are more sensitive to bacitracin than other streptococci A filter paper disc of 0.04U is applied on the surface of an inoculated blood agar After incubation, a wide zone of inhibition is seen with S. pyrogenes but not with other streptococci Principle: – Bacitracin test is used for presumptive identification of group A – To distinguish between S. pyogenes (susceptible to B) & non group A such as S. agalactiae (Resistant to B) – Bacitracin will inhibit the growth of group A Strep. pyogenes giving zone of inhibition around the disk Procedure: – Inoculate BAP with heavy suspension of tested organism – Bacitracin disk (0.04 U) is applied to inoculated BAP – After incubation, any zone of inhibition around the disk is considered as susceptible
- 41. 4. Identification: Rapid diagnostic test kits are available for the detection of streptococcal group A antigen from throat swab f) Lancefield serogrouping: Based on ‘C’ carbohydrate antigen g) Serotyping: serotyping of S. pyogens is required only for epidemiological purposes. III) Antigen detection: ELISA & Agglutination tests are used for detection of S. pyogenes antigen from throat swabs
- 42. • Serological tests are useful • The tests are – 1. Anti Streptolysin O (ASO) test 2. Anti Deoxyribonuclease B (anti-DNAase B) test 3. Anti Hyaluronidase test 4. Streptozyme test B) In Non-suppurative complicationsB) In Non-suppurative complications
- 43. 5. Serology: Antistreptolysin O titration Standard test ASO titres higher than 200 are indicative of prior streptococcal infection. High levels are usually found in acute rheumatic fever but in glomerulonephritis, times are often low. Strep throat is now most often diagnosed quickly by a serological diagnostic test. One of the most common types is a latex particle agglutination test, where the latex particles are coated with specific Ab. against the prevailing Ag types of Group A Streptococcus. The swab from your throat is tested for the presence of these Ags by swirling in the tube of latex particles with specific Ab clumping being positive. ASO TITER greater than 1 in 180 Todd units is helpful in diagnosis of Rheumatic fever.
- 44. 5. Serology: Antideoxyribonuclease B (anti-DNAase B) Commonly used Titres higher than 300 are taken Streptozyme test: A passive slide hemagglutination test using erthyrocytes sensitised with a crude preparation of streptococci It is a convenient, sensitive and specific screening test.
- 45. Treatment, prevention and control DRUGS USED: • For streptococcal pharyngitis: Oral penicillin V or amoxicillin • Oral cephalosporin or macrolides can be used for penicillin sensitive patients • For severe, systemic infection: Combined use of intravenous penicillin with protein synthesis inhibiting antibiotics (clindamycin) is recommended • Streptococcal pyogenes have developed resistance over tetracyclines and sulfonamides, newer macrolides • Antimicrobial drugs has no effect on glomerulonephritis and rheumatic fever
- 46. Prophylaxis • Rheumatic fever requires long term antibiotic prophylaxis to prevent recurrence of disease • Penicillin is used in patients who have developed early signs of rheumatic fever • For acute glomerulonephritis no need of antibiotic therapy and prophylactic therapy (no re-infection) • For patients with serious soft tissue infection, drainage and aggressive surgical debridement must be initiated
- 47. Group B beta hemolytic Streptococci Streptococcus agalactiae • Infect newborns - Neonatal infection • Source – Infection acquired through maternal vagina during birth • Group B Streptococci (GBS) – puerperal sepsis, pneumonia • Presents as meningitis, pneumonia or septicemia • Most common cause of neonatal meningitis • Diagnostic markers – Hippurate hydrolysis, CAMP test
- 48. CAMP test • Christie, Atkins and Munch-Peterson • When S. agalactiae is inoculated perpendicular to a streak of S. aureus grown on blood agar an accentuated zone of hemolysis occurs
- 49. CAMP test Principle: Group B streptococci produce extracellular protein (CAMP factor) CAMP act synergistically with Staphylococcus aureus β-lysin to cause lysis of RBCs Procedure: Single streak of Streptococcus to be tested and a Staph. aureus are made perpendicular to each other 3-5 mm distance was left between two streaks After incubation, a positive result appear as an arrowhead shaped zone of complete hemolysis S. agalactiae is CAMP test positive while non group B streptococci are negative
- 50. CAMP TEST S. aureus (Spingomyelinase C) Group B Streptococcus (CAMP Factor) Group A Streptococcus Enhanced Zone of Hemolysis
- 51. Hippurate Test Hippurase NEG Streptococcus agalactiae not added Hippurase POS Grp B Streptococci added
- 52. Streptococcal Mastitis S. agalactiae (B), S, dysgalactiae (C) and S. uberis are main causes. S. pyogenes (A) and S. zooepidemicus (C) are less commonly isolated. S. agalactiae colonizes in milk ducts and produces persistent infection with intermittent bouts of acute mastitis. S. dysgalactiae found in buccal cavity and genitalia and on the skin of the mammary gland causes acute mastitis. S. uberis a normal inhabitant of skin, tonsils and vaginal mucosa is a major cause of clinical mastitis, usually without systemic signs. Hemolysis CAMP test Aesculin hydrolysis (Edwards Medium) Growth on MacConkey agar Lancefield Group S. agalactiae β (α, γ) + - - B S. dysgalactiae α - - - C S. uberis α - + - Not assigned E. faecalis α - + + D
- 53. Group C beta hemolytic Streptococci Streptococcus equi • S. equi ssp equi causes Stangles in Horses. • Highly contagious disease of horses. • Febrile disease (>1010 C) involving the upper respiratory tract with abscessation of regional lymph nodes. • Horses of all ages are susceptible however, most common in young horses. • Assembling horses at sales, shows and races increases risk of infection. • Transmission is via purulent exudates from the upper respiratory tract or from discharging abscesses. • A chronic convalescent carrier state can develop with bacteria present in the guttural pouch. • An atypical mild form where S. equi are present in small purulent foci has been described. • Infected animals may shed S. equi for at least 04 weeks after development of clinical signs.
- 54. Strangles • Incubation Period: 3-6 days • There is high fever, depression and anorexia followed by an occulo-nasal discharge that becomes purulent. • The lymph nodes of head and neck are swollen and painful. • Characteristically sub-mandibular lymph nodes are affected and they eventually rupture discharging purulent highly infectious pus. • Guttural pouch empyema is a common finding • Morbidity up to 100% and mortality less than 5% • Death occurs due to complications like pneumonia, neurological involvement, asphyxia due to pressure on pharynx from enlarges lymph nodes or purpura hemorrhagica (caused by bleeding from capillaries which results in red spots on the skin and mucous membranes together with oedema (swelling) of the limbs and the head). • Bastard Strangles: in which abscessation develops in many organs, is a serious complication in about 1% of affected animals.
- 55. Clinical Signs
- 56. Diagnosis Clinical signs and history of recent exposure to suspected animals Colonies are mucoid, up to 4.0 mm in diameter, surrounded by a wide zone of beta-hemolysis S. equisimillis and S. zooepidemicus, which causes mild upper respiratory tract infections, must be differentiated from S. equi by sugar fermentation tests in peptone water containing serum. Trehalose Sorbitol Lactose Maltose S. equi - - - + S. equisimilis + - V + S. zooepidemicus - + + +(-)
- 57. Treatment Treatment Penicillin to in-contact and infected horses is recommended Antibiotics are of limited use when abscesses have developed. Control: Clinically suspected animals should be isolated. Horses should be isolated for 10 days when first introduced or returning to herd Predisposing factors liking overcrowding and mixing of different age groups should be avoided. After outbreak, building and equipment should be disinfected. Prophylaxis: Inactivated vaccine is available in some countries
- 58. Group C beta hemolytic Streptococci Streptococci equisimilis • Upper respiratory infections • Endocarditis, osteomyelitis, brain abscess • Treat with penicillin and gentamicin • Penicillin tolerance • Source of streptokinase used for thrombolytic therapy in patients
- 59. Classified into 2 groups: 1. Non enterococcal group: containing S. suis, S. bovis and S. equinus. 2.The enterococcus group: which have been reclassified as a separate genus called Enterococcus, containing- E. faecalis, E. faecium and E. durans. Group D Streptococci:
- 60. S. suis is recognized as cause of significant losses in pig industry. Causes meningitis, arthritis, septicemia and bronchopneumonia in pigs of all ages with sporadic cases of endocarditis, neonatal deaths and abortion. Belong to Lancefield group D. Symptomatic carrier pigs harbour S. suis in tonsillar tissue. Disease outbreaks most common in intensively reared pigs due to overcrowding, poor ventilation and other stress factors. Sows carrying organisms may infect their litters leading to neonatal deaths or carrier state animals Respiratory disease may occur in conjunction with Mycoplasma and Pasteurella spp. S. suis may infect cattle, small ruminants, horses and cats. Infections occurs in human directly involved in pig husbandry or processing. Control: These bacteria tend to become endemic in herd and eradication not feasible. Improved husbandry practices Prophylactic Penicillins may be given to sows 01 week prior to farrowing and to piglets during first 02 weeks of life- in herds experiencing neonatal deaths and meningitis at weaning S. suis
- 61. Formerly Streptococcus - GROUP D STREPTOCOCCI Enterococcus faecalis Enterococcus faecium Enterococcus durans Most commonMost common species in faecalisspecies in faecalis Group D carbohydrate cell wall antigen Present in intestine, genital tract and saliva - Normal inhabitant Normal gut floraNormal gut flora Enterococcus
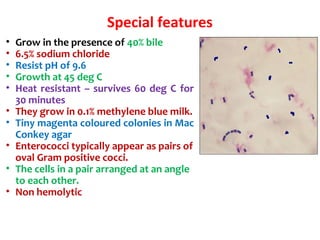
- 62. Special features • Grow in the presence of 40% bile • 6.5% sodium chloride • Resist pH of 9.6 • Growth at 45 deg C • Heat resistant – survives 60 deg C for 30 minutes • They grow in 0.1% methylene blue milk. • Tiny magenta coloured colonies in Mac Conkey agar • Enterococci typically appear as pairs of oval Gram positive cocci. • The cells in a pair arranged at an angle to each other. • Non hemolytic
- 63. Source & mode of infection: 1. Endogenous: from colonized site. 2. Exogenous: through direct or indirect contact. Common infections: 1. Urinary tract infection 2. Wound infection 3. Bacteremia 4. Intra-abdominal abscesses 5. Biliary tract infection 6. Sub acute bacterial endocarditis Clinical significance
- 64. Laboratory diagnosis Specimens collected: Urine, blood, pus & exudates. Methods of examination: 1. Direct microscopy- by doing Gram’s smear. 2. Culture- Blood agar and MacConkey’s agar is used. Identification: • Gram’s stain • Catalase Negative • Mannitol, sucrose, sorbitol fermentation • Bile Esculin hydrolysis • Non-hemolytic on blood agar • Intrinsically resistant to cephalosporins Treatment: • Strains resistant to penicillin & other antibiotics occur frequently. • Penicillin + Aminoglycosides • Vancomycin is the alternative drug to penicillin: Vancomycin resistant is also seen- VRE - terminal D-ala replaced by D-lactateterminal D-ala replaced by D-lactate
- 65. Viridans group • Streptococci normally resident in the mouth and upper respiratory tract • Alpha hemolysis on blood agar • Cannot be categorized under Lancefield antigenic groups Types: 1. S. mitis 2. S. mutans 3. S. salivarius 4.S. sanguis • Causes dental caries • Tooth extraction – seeding into blood stream - endocarditis – hence give prophylactic antibiotics
- 66. Streptococcus pneumoniae (pneumococcus) Morphology: • Lancet shaped (one end broad, other pointed) • Capsulated • Diplococci S. pneumoniae: lancet-shaped diplococcus
- 67. Growth characteristics • Alpha hemolysis on blood agar • On further incubation, the colonies become flat with raised edges and central elevation resembling carrom coins Example – Streptococcus viridans (Viridans = green) Streptococcus pneumoniae
- 68. Biochemical reactions • Hiss serum water – fermentation of inulin • Bile solubility
- 69. Resistance • Pneumococcus is sensitive to optochin – used for typing • Resistance to penicillin • May be resistant to third gen ceph also – third generation cephalosporin like ceftriaxone
- 70. Capsule
- 71. Pathogenicity and virulence • Capsule • Toxins – pneumolysin • C reactive protein
- 73. Pneumolysin • Membrane damaging toxin • Cytotoxic activity
- 74. C reactive protein • Abnormal immunoglobulin against C protein of S. pneumoniae appears in serum of patients • Also seen in acute phase of infections and inflammations • CRP titre is tested in acute infections
- 75. Epidemiology • Source – respiratory tract of humans • Spread – droplets • Carriers – pharynx • Low immunity is responsible for fulminant infections – RSV infection, pulmonary congestion, stress, malnutrition, alcoholism – Splenectomy – Sickle cell disease
- 76. 76 Diseases caused • Middle ear – otitis media • Para nasal sinuses – sinusitis • Respiratory tract – pneumonia, bronchitis, empyema • Meningitis is secondary to otitis media, penumonia, sinusitis and conjunctivitis
- 77. Laboratory diagnosis Sample Pneumonia - Sputum Septicemia - blood culture Otitis media - fluid from middle ear Meningitis - CSF Method – Gram stain, microscopy – Culture Latex agglutination for pneumococcal antigen in serum of patients
- 78. Differentiation between α-hemolytic streptococci • The following definitive tests used to differentiate between S. pneumoniae & viridans streptococci Optochin Test Bile Solubility Test Inulin Fermentation
- 79. Optochin Susceptibility Test Principle: – Optochin (OP) test is presumptive test that is used to identify S. pneumoniae – S. pneumoniae is inhibited by Optochin reagent (<5 µg/ml) giving a inhibition zone ≥14 mm in diameter. Procedure: – BAP inoculated with organism to be tested – OP disk is placed on the center of inoculated BAP – After incubation at 37oC for 18 hrs, accurately measure the diameter of the inhibition zone by the ruler – ≥14 mm zone of inhibition around the disk is considered as positive and ≤13 mm is considered negative • S. pneumoniae is positive (S) while S. viridans is negative (R) Optochin susceptible S. pneumoniae Optochin resistant S. viridans
- 80. Bile Solubility test Principle: – S. pneumoniae produce a self- lysing enzyme to inhibit the growth – The presence of bile salt accelerate this process Procedure: – Add ten parts (10 ml) of the broth culture of the organism to be tested to one part (1 ml) of 2% Na deoxycholate (bile) into the test tube – Negative control is made by adding saline instead of bile to the culture – Incubate at 37oC for 15 min – Record the result after 15 min Results: – Positive test appears as clearing in the presence of bile while negative test appears as turbid – S. pneumoniae soluble in bile whereas S. viridans insoluble
- 81. Differentiation between β-hemolytic streptococci Hemolysis Bacitracin sensitivity CAMP test S. pyogenes β Susceptible Negative S. agalactiae β Resistant Positive Hemolysis Optochin sensitivit y Bile solubility Inulin Fermentation S. pneumoniae α Sensitive (≥ 14 mm) Soluble Not ferment Viridans strep α Resistant (≤13 mm) Insoluble Ferment Differentiation between α-hemolytic streptococci
- 82. Outline of differentiation between Gram-Positive cocci e.g. S. epidermidis
- 83. Treatment • Penicillin • Amoxycillin • ceftriaxone/ceftazidime • Vancomycin
- 84. Prophylaxis • Pneumococcal conjugate vaccine is available • Given to splenectomy patients, sickle cell anemia patients and susceptible individuals
- 85. Classification of Streptococci from Humans Species Lancefield Hemolytic Comments S. pyogenes A β Scarlet Fever, Septic Sore throat, Rheumatic fever, Glomerulonephritis S. agalactiae B β (α, γ) Chronic Mastitis S. dysgalactiae C α (β, γ) Acute mastitis S. equisimilis C α (β, γ) Abscesses, Endometritis, Mastitis S. equi C β Strangles, suppurative conditions, purpura haemorrhagica S. equi subsp zooepidemicus C β Bovine mastitis S. suis D α, β septicaemia; meningitis, arthritis, bronchopneumonia & infrequent human meningitis
- 86. Zoonotic Streptococcus Species Species Lancefield Hemol ysis Comments S. bovis species group D α, γ Viridans; associated with colon cancer; IE S. mutans group not useful α, γ, rarely β Viridans; dental caries and IE S. salivarius group not useful α, γ Viridans; opportunistic S. mitis group not useful α Viridans; IE, opportunistic S. anginosus group A, C, F, G, or no detectable α, β, γ Viridans; formerly known as S. milleri; 3 species S. anginosus, S. constellatus, and S. intermedius; purulent infections S. canis G β Dogs; infrequent human pathogen S. iniae None detectable β Fish; SSTI, sepsis
- 87. Group F beta hemolytic Streptococci Streptococcus MG • Grow poorly on blood agar • Minute streptococci • Streptococcus MG – alphalytic strain – isolated from Primary atypical pneumonia
- 88. Minute colony streptococciMinute colony streptococci Various groups/ hemolysis (e.g. group A)Various groups/ hemolysis (e.g. group A) – genetically distinct from large colony (e.g. S. pyogenes)genetically distinct from large colony (e.g. S. pyogenes) – no rheumatic feverno rheumatic fever Large colonyLarge colony Minute colonyMinute colony
- 89. Thanks Acknowledgement: All the material/presentations available online on the subject are duly acknowledged. Disclaimer: The author bear no responsibility with regard to the source and authenticity of the content. Questions???
- 90. Thanks Acknowledgement: All the presentations available online on the subject are duly acknowledged. Disclaimer: The author bear no responsibility with regard to the source and authenticity of the content.





























![Streptococcal Diseases
Suppurative Complications
1. Respiratory infections
Primary site of invasion is throat causing SORE THROAT
May be localized as tonsillitis or pharyngitis
Lipoteichoic acid covering surface pili binds to the glycoprotein
fibronectin on epithelial cells of pharynx
From the throat, spreads to surrounding tissues leading to suppurative
complications like
Otitis media
Mastoiditis
Quinsy
Suppurative adenitis
Meningitis (rare)
(it is an inflammation of the mucosal lining of the mastoid antrum and mastoid air cell system
inside[1]
the mastoid process. The mastoid process is the portion of the temporal bone of the skull
that is behind the ear which contains open, air-containing spaces.
(Peritonsillar abscess (PTA), also known as a quinsy, is pus due to an infection behind the
tonsil).
Adenitis is a general term for an inflammation of a gland
tonsillitis pharyngitispharyngitis](https://image.slidesharecdn.com/genusstreptococcus-190604025329/85/Genus-Streptococcus-29-320.jpg)