HIVAIDS TX AND NURSINN- INTRO PART I.ppt
- 1. ® JAMES O.H is the Author many Books & Co-funder of DGCEO, Borad Director of DUGERI (www.dugeri.org) 1 STUDENT’S STUDY MATERIAL D & C IN HEALTH SCIENCES CONTENTS OF THIS BOOK ARE: HIV/AIDS MANAGEMENT, TREATMENT & NURSING INTRODUCTION TO COMMUNITY MEDICINE INTRODUCTION TO PRIMARY HEALTH CARE ANATOMY AND PHYSIOLOGY FIRST AID AND SCANE MANAGEMENT INTRODUCTION TO MEDICAL RECORD & INFORMATICS INTRODUCTION TO PUBLIC HEALTH INTRODUCTION HEALTH EDUCATION (2018- himofficer22@gmail.com O JAMES. H
- 2. Lesson objectives • Understand the global and local impact of the epidemic • Know about HIV/AIDS in adults, children, and families • Understand the Management and caring of PLHV • Understand the natural history of HIV infection • Understand the modes of HIV transmission • Understand HIV/AIDS opportunistic and related risks management • Understand HIV tests and ARTS • Etc Scope of the HIV/AIDS Pandemic Natural History and Transmission of HIV
- 3. Background of HIV/AIDS What was the first name given to HIV? When was HIV discovered in Uganda? What is the daily prevalence HIV rate among young people in Uganda? HIV-1 infection, initially described as slim disease was first recognized in Uganda in 1982, and is now a predominant health problem. Approximately 2.5 million Ugandans are now infected, largely through heterosexual transmission. In many areas half of adult deaths are now cause by HIV. In Uganda around 70 young people below 25 years contract HIV/AIDS every day in Uganda.
- 4. What is HIV? Human Immunodeficiency Virus H = Infects only Human beings I = Immunodeficiency, virus weakens the immune system and increases the risk of infection V = Virus that attacks the body Is A retrovirus that infects cells of human immune system and destroys or impairs the functions. Its a condition that attacks the body immune system, specifically the white blood cells called CD4 cells, weakening a persons immunity against opportunistic infections such as TB, and some cancer.
- 5. What is AIDS? Acquired Immune Deficiency Syndrome A = Acquired, not inherited I = Weakens the Immune system D = Creates a Deficiency of CD4+ cells in the immune system S = Syndrome, or a group of illnesses taking place at the same time
- 6. HIV and AIDS • When the immune system becomes weakened by HIV, the illness progresses to AIDS • Some blood tests, symptoms or certain infections indicate progression of HIV to AIDS
- 7. HIV-1 and HIV-2 types • HIV-1 and HIV-2 are • Transmitted through the same routes • Associated with similar opportunistic infections • HIV-1 is more common worldwide • HIV-2 is found in West Africa, Mozambique, and Angola
- 8. HIV-1 and HIV-2 • HIV-2 is less easily transmitted • HIV-2 is less pathogenic • Duration of HIV-2 infection is shorter • MTCT is relatively rare with HIV-2 • MTCT of HIV-2 has not been reported from India
- 9. V-VIRUS Is a microscopic pathogen made from a strip of genetic material and a prospective outer layer made of fatty acids. It is a parasitic organisms that cannot live on its own. It infects a host cell and causes changes. That divides or replicates There4 creating new viral particles. Virus has to infect a cell in order to survive. The eventually leaves its host and spreads to infect new cells in order to spread. Some viruses damage their host cell by forcing them to bust or replicate all the cell resources. The viruses that causes damage to their hosts are those that cause diseases. The symptoms of each disease caused by a virus depend on which cells in the body are damaged and the function they have.
- 10. Continue…….. HIV is a retrovirus. HIV belongs to a groups of viruses called retroviruses. This virus contains a genetic materials made from other RNA (Ribonucleic Acid) The most organisms, including people, have their genes from DNA (Deoxyribonucleic acids). HIV is called retrovirus, meaning Reverse virus because its process of replications is backwards compared to other organisms.
- 11. Transmission of HIV HIV is transmitted by • Direct contact with infected blood • Sexual contact: oral, anal, or vaginal • Direct contact with semen or vaginal and cervical secretions • HIV-infected mothers to infants during pregnancy, delivery, or breastfeeding
- 12. Transmission of HIV HIV is not transmitted by • Public baths • Handshakes • Work or school contact • Using telephones • Sharing cups, glasses, plates, or other utensils • Coughing, sneezing • Insect bites • Touching, hugging • Water, food • Kissing
- 13. Impact of Global HIV • Negative economic impact on countries • Overstrained healthcare systems • Decreasing life expectancy • Reversal of child survival gains • Increased numbers of orphans
- 14. HIV/AIDS Profile (Uganda) Describe the Uganda HIV/AIDS profile ?
- 15. Prevention of HIV Transmission • Strategies to prevent HIV transmission • Personal strategies • Public health strategies • Safe practices: no risk of HIV transmission • Risk reduction: reduces but does not eliminate risk
- 16. 1. Personal strategies Get tested for HIV. Talk to your partner about HIV testing and get tested before you have sex. Choose less risky sexual behaviors. HIV is mainly spread by having anal or vaginal sex without a condom or without taking medicines to prevent or treat HIV. Use condoms every time you have sex. Read this fact sheet from CDC on how to use condoms correctly. Limit your number of sexual partners. The more partners you have, the more likely you are to have a partner with poorly controlled HIV or to have a partner with a sexually transmitted disease (STD). Both of HIV. Get tested and treated for STDs. Insist that your partners get tested and treated, too. Having an STD can increase your risk of getting HIV or spreading it to others. Talk to your health care provider about pre-exposure prophylaxis (PrEP). PrEP is an HIV prevention option for people who do not have HIV but who are at risk of getting HIV. PrEP involves taking a specific HIV medicine every day to reduce the risk of getting HIV through sex or
- 17. Prevention of HIV Transmission…. HIV is mainly spread by having sex or sharing syringes and other injection equipment with someone who is infected with HIV. Substance use can contribute to these risks indirectly because alcohol and other drugs can lower people’s inhibitions and make them less likely to use condoms. 2. Public health strategies to prevent HIV transmission Screen all blood and blood products Follow universal precautions Educate in safer sex practices Identify and treat STIs/other infections Provide referral for treatment of drug dependence Apply the comprehensive PPTCT approach to prevent vertical transmission of HIV PPTCT is Prevention of Parent to Child Transmission
- 18. 3. RISK REDUCTION 1. Pre-Exposure Prophylaxis (PrEP) Pre-exposure prophylaxis (or PEP) is medicine taken to prevent getting HIV. PEP is highly effective for preventing HIV when taken as prescribed. PEP reduces the risk of getting HIV from sex by about 99%. PEP reduces the risk of getting HIV from injection drug use by at least 74%. PEP is less effective when not taken as prescribed. Since PEP only protects against HIV, condom use is still important for the protection against other STDs. Condom use is also important to help prevent HIV if PEP is not taken as prescribed.
- 19. Risk reduction continue…….. 2.Post-Exposure Prophylaxis (PEP) PEP is the use of antiretroviral drugs after a single high- risk event to stop HIV seroconversion. PEP must be started as soon as possible to be effective—and always within 72 hours of a possible exposure.
- 20. Continue…… 3. Condoms When used the right way every time, condoms are highly effective in preventing HIV and other sexually transmitted diseases (STDs). If condoms are paired with other option like PEP or ART, they provide even more protection.
- 21. The Right Way To Use A Male (External) Condom
- 22. Condom Dos and Don’ts Dos DO use a condom every time you have sex. DO put on a condom before having sex. DO read the package and check the expiration date. DO make sure there are no tears or defects. DO store condoms in a cool, dry place. DO use latex or polyurethane condoms. DO use water-based or silicone-based lubricant to prevent breakage.
- 23. Don’ts DON’T store condoms in your wallet as heat and friction can damage them. DON’T use nonoxynol-9 (a spermicide), as this can cause irritation. DON’T use oil-based products like baby oil, lotion, petroleum jelly, or cooking oil because they will cause the condom to break. DON’T use more than one condom at a time. DON’T reuse a condom.
- 29. Natural History of HIV Infection DR. S.K CHATURVEDI
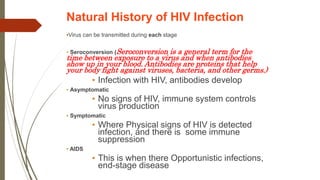
- 30. Natural History of HIV Infection •Virus can be transmitted during each stage • Seroconversion (Seroconversion is a general term for the time between exposure to a virus and when antibodies show up in your blood. Antibodies are proteins that help your body fight against viruses, bacteria, and other germs.) • Infection with HIV, antibodies develop • Asymptomatic • No signs of HIV, immune system controls virus production • Symptomatic • Where Physical signs of HIV is detected infection, and there is some immune suppression • AIDS • This is when there Opportunistic infections, end-stage disease
- 31. Natural History of HIV Infection Immune suppression • HIV attacks white blood cells,called CD4 cells, that protect body from illness • Over time, the body’s ability to fight common infections is lost • Opportunistic infections occur Mr. James –himofficer22@gmail.com 256 (0) 392 553 317, (KRAWFORD INTERNATIONAL INSTITUTE )
- 32. HIV Disease Progression of HIV disease is measured by: CD4+ count Degree of immune suppression Lower CD4+ count means decreasing immunity Viral load Amount of virus in the blood Higher viral load means more immune suppression Mr. James –himofficer22@gmail.com 256 (0) 392 553 317, (KRAWFORD INTERNATIONAL INSTITUTE )
- 33. Direct infection of organ systems • HIV can directly infect the: • Brain (HIV dementia) • Gut (wasting) • Heart (cardiomyopathy) Mr. James –himofficer22@gmail.com 256 (0) 392 553 317, (KRAWFORD INTERNATIONAL INSTITUTE )
- 34. HIV Disease contiu Severity of illness is determined by amount of virus in the body (increasing viral load) and the degree of immune suppression (decreasing CD4+ counts) Higher the viral load, the sooner immune suppression occurs Mr. James –himofficer22@gmail.com 256 (0) 392 553 317, (KRAWFORD INTERNATIONAL INSTITUTE )
- 35. Progression of HIV Infection HIGH viral load (number of copies of HIV in the blood) LOW CD4 count (type of white blood cell) Increasing clinical symptoms (such as opportunistic infections) Mr. James –himofficer22@gmail.com 256 (0) 392 553 317, (KRAWFORD INTERNATIONAL INSTITUTE )
- 36. HIV Disease: Summary • HIV multiplies inside the CD4+ cells, destroying them • As CD4+ cell count decreases and viral load increases, the immune defences are weakened • HIV-infected people become vulnerable to opportunistic infections • HIV is a chronic viral infection with no known cure • Without ARV treatment, HIV progresses to symptomatic disease and AIDS Mr. James –himofficer22@gmail.com 256 (0) 392 553 317, (KRAWFORD INTERNATIONAL INSTITUTE )
- 37. Key Points HIV is a global pandemic and the number of people living with HIV continues to increase worldwide. HIV epidemic is especially severe in resource-constrained settings HIV is a virus that destroys the immune system, leading to opportunistic infections. The progression from initial infection with HIV to end-stage AIDS varies from person to person and can take more than 10 years. Mr. James –himofficer22@gmail.com 256 (0) 392 553 317, (KRAWFORD INTERNATIONAL INSTITUTE )
- 38. Key Points (continued) The most common main route of transmission worldwide is heterosexual transmission. Women of childbearing age are at particular risk for acquiring HIV through unprotected sex HIV-positive women who are pregnant are at risk of passing HIV infection to their newborn. Risk of HIV transmission from mother-to-child can be greatly reduced through effective PMTCT programs Mr. James –himofficer22@gmail.com 256 (0) 392 553 317, (KRAWFORD INTERNATIONAL INSTITUTE )
- 39. HIV Treatment A approaches and Care Antiretroviral therapy (ART) reduces HIV-related morbidity and mortality at all stages of HIV infection and reduces HIV transmission. When taken consistently as prescribed, ART can suppress viral load, maintain high CD4 cell counts, prevent AIDS, prolong survival, and reduce risk of transmitting HIV to others, all of which are important treatment goals. Current treatment guidelines recommend ART for all people with HIV, regardless of CD4 cell count. ART should be started as soon as possible after diagnosis and should be accompanied by patient education regarding the benefits and risks of ART and the importance of adherence to ART. Mr. James –himofficer22@gmail.com 256 (0) 392 553 317, (KRAWFORD INTERNATIONAL INSTITUTE )
- 40. ART Initiation Health care providers play a crucial role in helping patients initiate ART, including describing the benefits of early initiation of ART, offering and prescribing ART, helping to manage long-term ART use, and providing information on other interventions that can reduce HIV transmission risk. By engaging patients in brief conversations at every office visit, providers can emphasize the benefits of consistent, long-term adherence to their prescribed ART regimen and the potential consequences of nonadherence. One way health care providers can enhance communication is to ask their patients open-ended questions during their office visits. These questions can help providers better understand the patient’s views, barriers, and ability to adhere to their treatment regimen. Mr. James –himofficer22@gmail.com 256 (0) 392 553 317, (KRAWFORD INTERNATIONAL INSTITUTE )
- 41. Here are some examples of questions providers can ask patients about initiating ART: • “What have you heard about HIV medicines?” • “What are the most important results you hope to get from treatment?” • “What are your concerns about HIV medicines?”
- 42. How does antiretroviral therapy work? Antiretroviral therapy reduces the amount of HIV in the body. When a person takes them consistently, antiretroviral drugs are very effective at limiting the impact of the virus. Although inequities exist by region and population, advances in antiretroviral therapy have made it possible for many people with HIV to live a comparable life span to those without HIV. This therapy helps keep the body healthy and prevent infections. Specifically, successful antiretroviral therapy prevents people from developing advanced HIV and makes it impossible to transmit the virus to others. The Centers for Disease Control and Protection (CDC)Trusted Source recommend that all people with HIV take antiretroviral therapy, regardless of how long they have had the virus or their current state of health. Antiretroviral therapy has become more potent, less toxic, and easier to use than in the past. It produces fewer and less severe side effects than before. This article describes various antiretroviral drugs, how they work, and their possible side effects. It also provides information about beginning treatment.
- 43. HIV is a retrovirus that targets the immune system, which is the system that fights off infection and disease. The virus damages or destroys white blood cells called CD4 cells. This makes it difficult for the body to fight off illness. Antiretroviral therapy prevents the virus from multiplying, which reduces the amount of HIV in the body. This gives the immune system a chance to produce more CD4 cells. Although antiretroviral therapy cannot completely remove HIV from the body, it keeps the immune system strong enough to combat infections and some HIV- related cancers. The aim of antiretroviral therapy is to reduce the amount of HIV in the blood to very low levels. Viral suppressionTrusted Source occurs when the count reaches fewer than 200 copies of the virus per milliliter of blood. When the viral load is so low that it is undetectable, it no longer damages the immune system, and there is no risk of transmitting the virus to others. This is known as “undetectable = untransmittable.”
- 44. There are many benefits to ART, including improved health and reduced risk of HIV transmission – but adherence is key! The success of ART is contingent on adherence to achieve and maintain viral suppression. Here are some examples of questions providers can ask patients to assess their ongoing adherence to ART: “How has it been going taking your HIV medicines?” “What seems to get in the way of taking your medicines?” “Have you missed any doses of your medication and if so, what was going on at that time?” Once the conversation has started, health care providers may find that patients are encountering barriers to adherence. Below is a list of common barriers and ways providers can address them through routine conversations during patient visits. ART Adherence and Viral Suppression Mr. James –himofficer22@gmail.com 256 (0) 392 553 317, (KRAWFORD INTERNATIONAL INSTITUTE )
- 45. Types of antiretroviral drug Antiretroviral therapy involves taking a combination of drugs each day. An HIV treatment regimen usually involves at least three different drugs from at least two different drug classes. The following are the different categories of antiretroviral drug: 1. Nucleoside reverse transcriptase inhibitors (NRTIs) NRTIs block the action of an enzyme called viral reverse transcriptase, which is necessary for HIV to replicate. Some examples of NRTIs include: • abacavir (Ziagen) • emtricitabine (Emtriva) • lamivudine (Epivir) • stavudine (Stavudine) • tenofovir disoproxil fumarate (Viread) • zidovudine (Retrovir) Mr. James –himofficer22@gmail.com 256 (0) 392 553 317, (KRAWFORD INTERNATIONAL INSTITUTE )
- 46. Non-nucleoside reverse transcriptase inhibitors (NNRTIs) 2. Non-nucleoside reverse transcriptase inhibitors (NNRTIs) NNRTIs work similarly to NRTIs. The only difference is that they act on different sites of the enzyme. Some examples of these antiretroviral medications include: • doravirine (Pifeltro) • efavirenz (Sustiva) • etravirine (Intelence) • nevirapine (Viramune) • rilpivirine (Edurant) Mr. James –himofficer22@gmail.com 256 (0) 392 553 317, (KRAWFORD INTERNATIONAL INSTITUTE )
- 47. 3. Protease inhibitors (PIs) PIs impede another viral enzyme, called HIV protease. HIV requires protease to replicate. Some types of PI include: • atazanavir (Reyataz) • darunavir (Prezista) • fosamprenavir (Lexiva, Telzir) • indinavir (Crixivan) • lopinavir/ritonavir (Kaletra) • ritonavir (Norvir) • saquinavir (Invirase) • tipranavir (Aptivus) Mr. James –himofficer22@gmail.com 256 (0) 392 553 317, (KRAWFORD INTERNATIONAL INSTITUTE )
- 48. 4. Entry inhibitors As the name suggests, these drugs prevent the virus from entering the targeted cells. To penetrate immune cells, HIV must fuse to the cells’ receptors, and these drugs work to stop this from happening. People often take entry inhibitors when other treatments have not worked. Some examples currently in use include enfuvirtide (Fuzeon) and, maraviroc (Selzentry). Mr. James –himofficer22@gmail.com 256 (0) 392 553 317, (KRAWFORD INTERNATIONAL INSTITUTE )
- 49. 5. Integrase inhibitors HIV uses a protein called integrase to send its genetic material into the cells that it targets. Integrase inhibitors block this action. Mr. James –himofficer22@gmail.com 256 (0) 392 553 317, (KRAWFORD INTERNATIONAL INSTITUTE )
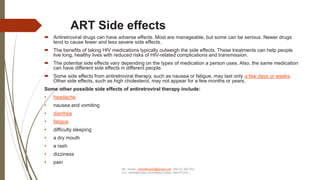
- 50. ART Side effects Antiretroviral drugs can have adverse effects. Most are manageable, but some can be serious. Newer drugs tend to cause fewer and less severe side effects. The benefits of taking HIV medications typically outweigh the side effects. These treatments can help people live long, healthy lives with reduced risks of HIV-related complications and transmission. The potential side effects vary depending on the types of medication a person uses. Also, the same medication can have different side effects in different people. Some side effects from antiretroviral therapy, such as nausea or fatigue, may last only a few days or weeks. Other side effects, such as high cholesterol, may not appear for a few months or years. Some other possible side effects of antiretroviral therapy include: • headache • nausea and vomiting • diarrhea • fatigue • difficulty sleeping • a dry mouth • a rash • dizziness • pain Mr. James –himofficer22@gmail.com 256 (0) 392 553 317, (KRAWFORD INTERNATIONAL INSTITUTE )
- 51. If someone experiences severe side effects or side effects that do not go away, they can talk to their healthcare provider about changing dosages or drug combinations to find the one that works best for them. It is important to avoid stopping medication without talking to a healthcare provider first, as breaks in therapy can allow the virus to multiply rapidly, which increases the person’s risk of getting sick. Some long-term side effects may include: • depression • diabetes • heart disease • insomnia • kidney damage • liver damage • nerve damage • weak bones, or osteoporosis • higher levels of fat in the blood Mr. James –himofficer22@gmail.com 256 (0) 392 553 317, (KRAWFORD INTERNATIONAL INSTITUTE )
- 52. Side effects that indicate a more serious complication and may require urgent care include: • extreme fatigue • nausea • fever • persistent vomiting • a rash People who experience swelling of the face, throat, or tongue require emergency treatment. If this occurs, a person should call an ambulance or go to the nearest emergency room. Mr. James –himofficer22@gmail.com 256 (0) 392 553 317, (KRAWFORD INTERNATIONAL INSTITUTE )
- 53. Managing the side effects A healthcare provider can give advice and other forms of support to people experiencing side effects from HIV treatment. If the symptoms are severe or ongoing, they may recommend alternative medications. It helps for people to discuss their lifestyle, needs, preferences, and current health status with their healthcare provider, who can take these into account when prescribing a treatment plan. When to start antiretroviral therapy The CDC Trusted Source recommend that all people with HIV take antiretroviral therapy, regardless of how long they have had the virus or their current health status. This includes the following groups: • people in the early stages of HIV • people who are pregnant or breastfeeding • people with stage 3 HIV • people with HIV-related infections or cancers Ideally, a person should begin antiretroviral therapy on the day they receive a diagnosis of HIV, or as soon as possible after this. This gives people the best chance of reducing their viral load and risk of complications. If a person does not receive effective treatment, the virus typically develops into the most advanced stage, stage 3 HIV, within 10 years. At this stage, the immune system is badly damaged, which can lead to opportunistic infections or certain types of cancer. Mr. James –himofficer22@gmail.com 256 (0) 392 553 317, (KRAWFORD INTERNATIONAL INSTITUTE )
- 54. Research tends to suggest that receiving prompt treatment reduces the risk of transmission, disease progression, and complications. However, it can be challenging to follow a daily treatment plan consistently for many reasons. These include: • access to and affordability of medications • stigma and discrimination in the healthcare system • mental health and substance use issues • pill fear or pill fatigue If a person is having trouble following their treatment regimen consistently, it is best that they talk to their healthcare provider as soon as possible to work out a plan to stay healthy. HIV.gov provides information about covering the costs of HIV treatment and tips for following an antiretroviral therapy regimen. Barriers of treatment and approaches to solution Mr. James –himofficer22@gmail.com 256 (0) 392 553 317, (KRAWFORD INTERNATIONAL INSTITUTE )
- 55. Barrier(s) Approach to Address the Barrier(s) Patient beliefs and behaviors, such as not taking their medications when they “feel well.” •Explain the importance of consistent ART adherence even when they feel well or their viral load is already undetectable, and the decrease in transmission risk when viral suppression is achieved. Cognitive or organizational barriers, such as lack of logistic skills and comprehension level. •Offer advice about and tools for adherence, such as weekly pill boxes, dose reminder alarms, and linking dosing to daily events/activities. Use a feedback strategy (such as “tell me what you just heard”) to help patients avoid confusion about new medicines, dosing schedule, and/or changed regimen. Treatment competence or the overall ability to adhere to a potentially complicated and long-term regimen. •Involve patients in decision making, including selection of the ART regimen, if options exist. •Ensure patients understand the treatment plan, including drug regimen, dosing schedule, and dietary restrictions. •Prepare patients for situations or changes in routine that could trigger nonadherence or short-term interruption, such as side effects, illicit drug use, or running out of HIV medication. •Encourage patients to keep one or two days worth of medication on hand in case of emergency to avoid missed doses. •Encourage patients to recruit friends and/or family members to help with adherence. Comorbid conditions – such as diabetes, dyslipidemia, hypertension, and viral hepatitis – that may further complicate the treatment plan design and the ability of the patient to adhere to the plan. •Regularly review the total treatment plan, and simplify regiment if possible with consideration for patients’ lifestyles and comorbidities. •Anticipate (and plan to manage) possible drug-drug interactions. Regimen-related barriers, including fear of treatment, fear of treatment-related side effects, and confusion about doses. •Offer ART regimens that are highly effective and simple to take (e.g., once daily single-tablet dosing, few if any dietary restrictions). •Explain that treatment has improved and is easier to take and better tolerated today than ever before. •Encourage patients to recruit friends and/or family members to help with adherence. Short-term side effects that can occur when patients start or change ART regimens, such as nausea, fatigue, disturbed sleep or dreaming. •Alert patients that some people have side effects but that they are usually mild, short-lived, and can be managed. •Explain which side effects may occur with the ART they are taking. •Anticipate (and plan to manage) these side effects. •Instruct patients that if they experience these or other side effects, they should seek help before stopping their ART regimen.
- 56. Psychosocial barriers, such as mental health issues (e.g., depression, perceived low quality of live), drug or alcohol abuse, negative attitudes or beliefs about HIV, and lack of social support. •When possible, refer patients to patient navigators for help with receiving essential support services related to mental health, substance use, and other support resources (e.g., psychologists, addiction specialists, support groups, adherence counselors, case managers) •Remind patients not to share their ART with anyone. •Encourage patients to recruit friends and/or family members to help with adherence. Mr. James –himofficer22@gmail.com 256 (0) 392 553 317, (KRAWFORD INTERNATIONAL INSTITUTE )
- 57. HOW TO EVALUATE PATIENT FOR ART INITIATION HIV Treatment and Follow-up Patients who are diagnosed with HIV are referred to the HIV clinic for care and treatment. Those who are eligible for ART receive at least 3 counselling sessions, in accordance with the national treatment guidelines to prepare them to start ART which is a lifelong commitment. The first follow-up visit is scheduled 2 weeks after ART initiation to monitor response to the prescribed regimen including drug toxicity and side-effects. Thereafter monthly visits are scheduled. Patients that are stable are given longer (usually 2 months) appointment times, which 5 is unusual for adolescents and young adults because of their challenges with adherence. The clinic visits are scheduled to coincide with the ARV drugs refills. During each visit, patients undergo a comprehensive clinical assessment that includes a physical examination and virological testing as described in the national guidelines. The parameters assessed included ARV drug regimen and adherence to medication; potential side effects; weight and height; TB status and presence of other OIs; loss of function; clinical disease stage; laboratory investigations and whether the patient had been hospitalized since the last clinic visit. CD4 count tests are done every six months and viral load testing is done 6 months after initiating treatment and annually thereafter. Patient records are routinely updated at every clinic visit including those that are lostto-follow-up (LTFU), transferred in from other clinics/out to other clinics, or have died. Most deaths are reported by relatives, community health workers and volunteers. Since there is no death registry, for this study, we used the recorded date of death in the medical record. Mr. James –himofficer22@gmail.com 256 (0) 392 553 317, (KRAWFORD INTERNATIONAL INSTITUTE )
- 58. ADHERENCE SUPPORT Adherence support interventions should be provided to people on ART. The following interventions have demonstrated benefit in improving adherence and viral suppression; Peer support system: This enables clients to learn from each other’s experiences and to cope better with the disease. A peer is a person who shares similar characteristics with a particular group of people. In HIV care, peers include mentor mothers in the eMTCT program, adolescent peers, expert clients and other peers as patients and caregivers usually relate better to peers .Peer support can be provided either in form of peer counseling or Peer support groups. Mr. James –himofficer22@gmail.com 256 (0) 392 553 317, (KRAWFORD INTERNATIONAL INSTITUTE )
- 59. • Mobile phone calls and text messages: These should be used with the patient or caregiver consent. The patient or caregiver should provide the appropriate phone numbers to avoid accidental disclosure when messages are sent to a wrong person. • Reminder devices like calendars, pill boxes, cell phone alarm sand diaries can be used by clients. • Behavioral skills training and medication adherence training: These include module-based interventions and those designed to improve life skills, attitudes, behavior and knowledge. • Fixed-dose combinations and once-daily regimens: When available, health-care workers should prescribe fixed dose combinations because they reduce the pill burden. If once daily regimens are available and recommended, they should be used. • Use of treatment buddies(supporters):This is an individual identified by the client to take on the role of a treatment supporter. This person reminds/gives the client their medication whenever it is time and also reminds them of their refill dates. • Peer-led dialogues: These include group discussions among clients. They could discuss the challenges they face and come up with possible solutions.
- 60. ADHERENCE PREPARATION Preparing people to start antiretroviral therapy (ART) is an important step to achieving ART success. Healthcare providers should initiate a detailed discussion about the willingness and readiness of patients to initiate ART. However, the choice to accept or decline ART ultimately lies with the person or his or her caregiver. If they choose to defer initiation, ART can be offered again at subsequent visits. Defer- put off, postponed……….. Health workers should provide information on circumstances where delays in starting ART can have negative consequences, particularly for people with tuberculosis (TB), advanced immune suppression, and/or who are at high risk of death. The healthcare team should use the 5As principles for chronic care as a guide to offer pre-ART adherence counseling and psychosocial support. These are Assess, Advise, Assist, Agree and Arrange Mr. James –himofficer22@gmail.com 256 (0) 392 553 317, (KRAWFORD INTERNATIONAL INSTITUTE )
- 61. Guide Components Assess Goal: To assess patients’ knowledge of HIV,ARVs and potential barriers to adherence •Knowledge about HIV and ARVs •Myths and misconceptions about HIV and ARVs •Potential barriers to adherence •Patient psychosocial concerns and needs that may hinder adherence to ART •Patient willingness and commitment to take medicines correctly •Patient readiness to honor subsequent appointment for treatment support •Patient’s support systems at family and community level •Disclosure status and implications Advise (information giving) Goal: To provide the patient with knowledge about HIV/ARVs to enable them decide to initiate treatment (Table 40) •Give information about HIV and ARVs •Provide information on adherence to ART. Include information on the 5 Rs (taking the right medicine, at the right time, right dose, right way, and right frequency) •Demonstrate how the ARV sare taken •Provide information about side effects of ARVs, improved quality of life while on ART, changes that may occur in a person’s life once on treatment •Explain the benefits of disclosure and support systems to adherence •Explain to the patient how often they will be monitored once on treatment; other ways of assessing adherence and response to treatment including pill counts •Emphasize the importance of attending all the clinic appointments for review and support •Discuss the Positive Health, Dignity, and Prevention package •Explain the implication of not adhering to ARV treatment 5As for adherence preparation support Mr. James –himofficer22@gmail.com 256 (0) 392 553 317, (KRAWFORD INTERNATIONAL INSTITUTE )
- 62. Guide Components • Explain what VL test is and the meaning of suppressed and unsuppressed viral load Assist Goal: To support client identify possible barriers and consider different options of dealing with the barriers. The client: •Evaluates the possible barriers to adherence and how to overcome them •Identifies the support systems that will enable the client to take his drugs and to regularly come to the facility such as treatment supporter, social support groups •Consider to disclose to a trusted person of their choice such as a treatment supporter, social support group, etc. Agree on Goal: To guide the client to develop a realistic individual adherence plan. The client considers and where possible documents; •An adherence plan(Table 41) •Family and community support systems (expert client in the community) •Possibility of home visit and consent •Possibility of testing other family members including sexual partner and children •Assess client’s readiness to start ART (see Table 42: ART readiness assessment form)
- 63. Arrange for • The patient to see a clinician for ARV prescription if they are ready to start ART • Follow-up adherence counseling and psychosocial support sessions o At one month for patients who have initiated ART o At agreed time but probably a week for those who were not ready for ART at theinitial visit • The patient to join psychosocial support groups and use support systems • Follow-up appointments (home visiting where appropriate, phone call reminders and text messages Guide Components where appropriate) •Monthly counseling sessions for drug adherence. •Reviewing the action plans at every encounter •When to bring other family members for testing •Supported disclosure where it has not happened Mr. James –himofficer22@gmail.com 256 (0) 392 553 317, (KRAWFORD INTERNATIONAL INSTITUTE )
- 64. INTENSIVE ADHERENCE COUNSELING AND SUPPORT FOR PATIENTS WITH DETECTABLE VIRAL LOAD Introduction Intensive Adherence Counseling and support refers to a targeted and structured counseling and support intervention offered to patients with a non-suppressed viral load (patients with viral load >1000 copies/ml). IAC is offered systematically and routinely as per scheduled appointments. IAC helps a client develop a comprehensive plan for adhering to ARVs by identifying their barriers to adherence, gaining insight of the barriers ,exploring possible ways to overcome barriers and making a plan to adhere to medicine. Provision of IAC requires a multidisciplinary team including clinicians, nurses, counselors, family members ,peers, etc. It may also require consultations from experts or referrals to address the issues related to stigma, disclosure, mental health and nutrition. How to offer IAC The 5As counseling framework applies to provision of intensive adherence counseling and psychosocial support. Key messages at every step are summarized below in Table 45 Mr. James –himofficer22@gmail.com 256 (0) 392 553 317, (KRAWFORD INTERNATIONAL INSTITUTE )
- 65. 5As for adherence support for people with non-suppressed viral load Guide Components IAC Session 1 Assess • Explain purpose of session and Disclose VL test results to client and explain meaning of suppressed and non-suppressed VL o Explain reasons for non-suppressed VL results (nonadherence to drugs or drugs may not be working well) o Discuss implications of non-suppressed results to the client • Determine adherence levels Calculate the adherence score using the adherence Guide Components percentage formula • Assess client’s barriers to adherence o Use the adherence assessment checklist to ascertain client’s adherence practices. o Identify barriers to client’s adherence (arising from the assessment)
- 66. Advise • Identify information gaps from assessment o Educate client in relation to specific barriers identified • Review benefits of good adherence o Assess client’s knowledge of benefits o Provide correct and complete information on • Discuss consequences of non-adherence o Assess clients knowledge on the dangers of nonadherence o Educate client on the consequences of nonadherence Assist • Evaluate the underlying causes of the identified barriers • Prioritize the barriers • Identify possible root causes of each barrier (where applicable) • Identify client specific strategies to overcome identified barriers • Discuss possible options to address key barriers • Provide information about available support systems e.g. CBOs, peer support groups etc • Discuss the pros and cons of each strategy/option Agree on • Agree on client’s action points to address the key barriers and Identify appropriate strategies Provide relevant and necessary information • Evaluate each action point using the 5 Ws and 1H o What, where, when, who, which , how? • Document agreed upon action points on the IAC session form • Develop and document a new adherence plan on the IAC