national health programme.ppt
- 1. NATIONAL HEALTH PROGRAMME FOR CHILDREN IN INDIA BY MRS. MALAR KODI
- 2. Introduction Various national health programs are currently in operation for the improvement of child health and prevention of childhood diseases. There are mainly 6 national health programme
- 4. The Government of India launched the Reproductive and child health programme in15th October ,1997as per recommendations of international conference on population development in 1994..
- 5. Components
- 6. •
- 7. 3 Antenatal check up
- 9. Prevention and treatment of anemia
- 10. Early identification of maternal complication and referral
- 13. 3 post natal check up
- 14. Birth spacing
- 15. Child survival
- 17. Exclusive breast feeding and weaning
- 19. Mgt of ARI
- 20. Mgt of diarrhea
- 21. Adolescent health Counseling on family life and reproductive health Prevention of anemia Prevention of RTI and STD’S
- 22. Family welfare and planning Promotion of contraception to prevent unwanted pregnancies Safe services for MTP
- 23. RCH package RCH phase I RCH phase II
- 24. RCH phase 1 RCH I has integrated services with CSSM Newer intervention in RCH I: : Essential Obstetric care. 24 hour delivery services at PHC & CHC Emergency obstetric care. MTP services Prevention of RTI /STDs and AIDS District surveys
- 25. RCH Phase II RCH Phase II began from 1st April 2005 To reduce maternal Mortality To reduce child Mortality More focus on rural health care
- 26. Universal immunization programme The WHO launched global immunization program in 1978 India , known as expanded program on immunization (EPI), to Protect all children of the world against six killer diseases. EPI is now renamed as universal child immunization, as per declaration sponsored by UNICEF in India, it is called as universal immunization program(UIP) was launched in 1985, November, for the universal coverage of immunization to the eligible population.
- 28. Other vaccines Rabies vaccines Haemophilus influenza vaccines (Hib) Japanese encephalitis (JE) vaccines
- 29. Intensified pulse polio immunization campaign an pulse polio programme Pulse Polio is an immunization campaign established by the government of India in 1994 to eradicate poliomyelitis (polio) in India by vaccinating all children under age five against poliovirus. PULSE stands for "Post- resuscitation and Initial Utility in Life saving Efforts”
- 30. Every child (0-5 years of age) receives a dose of Oral Polio Vaccine (OPV), a live, attenuated virus which colonizes in the gastrointestinal tract. This virus competitively inhibits , disease-causing poliovirus. Not only does this prevent pernicious infection in the host, it precludes transmission of the poliovirus to other hosts. Since poliovirus cannot survive outside a host for more than two weeks, theoretically it would be eradicated, resulting in the eradication of poliomyelitis
- 31. Recent news Polio remains endemic in four countries – Afghanistan, India, Nigeria and Pakistan are suspected of having re- established transmission of poliovirus. There have not been any cases reported for 2011, and the number of cases for 2010 remains 42. Most of India is polio-free. Persistent transmission of poliovirus is localized in areas of western Uttar Pradesh and central Bihar.
- 32. Integrated child development services (ICDS)
- 33. "The Integrated Management of Childhood Illness (IMCI)" 1992 UNICEF and WHO
- 34. At present, the most important scheme in the field of child welfare is the ICDS scheme. In pursuance of the national policy for children, Govt of India, started ICDS program in 1975, under the minister of social and women welfare. It is designed for the both preventive and development effort through a integrated package services.
- 35. To improve the health and nutritional status of children in the age group 0-6 years, To lay the foundation for proper psychological, physical and social development of children, To reduce the incidence of mortality, morbidity, malnutrition and school drop-out, To enhance the capability of the mother to look after the normal health and nutritional need of the child through proper nutrition and health education
- 38. Delivery of services CDPO ( child development project officer)- in charge of ICDS projects Community development black officer(4 supervisor) supervisor or mukhyasevika (20-25 AWW) AWW [Anganwadi Workers -for 1000 population] Anganwadi Helpers (AWH)
- 39. Nutrition supply At present a combination 50g puffed rice, 15g jaggery and 25 gram sattu is given to beneficiaries which is a source of 300 calories and 8-10 grams of protein. At present, the procurement of this is done by the Deputy Commissioner through a contractor finalized through tender process .
- 42. To promote positive health To prevent diseases Early diagnosis, treatment and follow-up of defects Increasing health awareness in children about good and bad health To provide healthful environment
- 43. Component Of School Health Program School health services School health environment School health education
- 45. 1- Components of Appraisal History Observation Screening tests Laboratory investigations
- 46. Prevention and control of communicable diseases Early detection and correction of non- communicable diseases Early identification and education of children with special disabilities Emergency care and first aid services 2.Preventive Aspects
- 47. 3.Curative aspects School clinics provided by general practitioners (GP) Referral hospitals services
- 49. School health environment • School schedules, • Duration and timing of school day, • Amount and timing of homework……..etc. Psychosocial Environment • Classroom ventilation, lighting, furniture • Play facilities • Garbage disposal Physical Environment
- 51. Special nutritional program 1970 Mid-day meal program. 1957 Anemia prophylaxis program. 1970 National iodine deficiency disorders control program
- 53. OBJECTIVE To improve the nutritional status of preschool children, pregnant,and lactating mother of poor socio economic groups in urban slums,tribal area and drought prone rural area Child up to one year 200kcl and 8-10g protein/day child 1-6 years. 300 kcal 10-12g proteins/day women 500 kcal 25g protein/day
- 55. OBJECTIVES To raise the nutritional status of primary school children To improve attendance and enrolment in school. To prevent dropouts from primary school. Children belonging to backward classes, schedule caste, and scheduled tribe families are given priority.
- 56. PRINCIPLES:- Should be a substitute. 1/3 Total energy and ½ total protein Provided at the low cost It is easily prepared Locally available food Change menu frequently.
- 57. BENEFICIARY School children in the age group 6-11 year SERVICES provides 300 calories and 8-12 g protein/day for 200 days in year
- 58. ANEMIA CONTROL PROGRAM (1970) BENEFICIARY Pregnant women, Nursing mothers, Women acceptors to terminal methods and IUD. children 5 years Daily dose of iron and folic acid tablets women:80mg ferrous sulfate+0.5 mg folic acid. Children:180mg ferrous sulfate+0.1 mg folic acid.(2ml liquid )
- 59. NATIONAL IODINE DEFICIENCY DISORDERS CONTROL PROGRAM (1962) 1962: NGCP launched 1984 : The central council of health approved the Policy of Universal salt Iodization (USI): Private sector to produce iodized salt 1992: NGCP renamed as NIDDCP 1997: sale and storage of common salt banned
- 60. OBJECTIVES:- Surveys to assess the magnitude of the IDD. Supply of iodated salt in place of common salt Resurvey after every 5 years to assess the extent of iodine deficiency disorders and the Impact of iodated salt. Laboratory monitoring of iodated slat and urinary iodine excretion. Health education & publicity.
- 62. 1. National school health program. 1977 2. National mental health program 1982 3. National program for control of blindness 1963 4. National cancer control program 1975-1976 5. National diabetes control program 6. Child welfare program for disabled children 7. National water supply and sanitation program 1954 8. National family welfare program 1952 9. Minimum needs program 1974-1978 (5th five year plan)
- 64. AIMS AND OBJECTIVES Promotion of positive health Prevention of disease Timely diagnosis, treatment and follow up Health education to Inculcate awareness about good and bad health. Availability of healthful environment
- 65. COMPONENT Health appraisal Remedial measures and follow up Prevention of communicable disease Healthful environment Nutritional services First aid facilities Mental health Dental health Eye health Ear health Health education Education of handicapped children School health record
- 66. NATIONAL MENTAL HEALTH PROGRAM (1982) components 1. Treatment of Mentally ill 2. Rehabilitation 3. Prevention and promotion of positive mental health.
- 67. OBJECTIVES Provision of mental health services at district level. Improvements of facilities in mental hospitals. Training of trainers of PHC personnel in mental hospital Program for substance use disorder.
- 68. NATIONAL PROGRAM FOR CONTROL OF BLINDNESS (1976)
- 69. 1963: Started as National Trachoma Control Program 1976: Renamed as National Program for prevention of Visual Impairment and Control of Blindness 1982: Blindness included in 20-point program
- 70. OBJECTIVES Dissemination of information about eye care. Augmentation of ophthalmic services so that eye care is promptly availed off. Establishment of a permanent infrastructure of community oriented eye health care.
- 71. BENIFICERY :- 6month -5 year children STREATGY Administration of vit A dose at a regular 6 monthinterval VIT AADMINISTRATIONSCHEDUALE 6-11 month:-100000 IU 1-5 year:-200000 IU /6 months Child must receive total 9 does VITAMIN A DEFICIENCY CONTROL PROGRAM (1970)
- 72. PREVENT VIT-A DEFICIENCY THROUGH Promotion of breastfeeding and feeding of colostrums. Encourage the intake of green leafy vegetable and yellow colored fruit. Increase the coverage of with measles (depletes vitamin A stores)
- 73. NATIONAL CANCER CONTROL PROGRAM 1975-76: National Cancer Control Program launched 1984-86: Strategy revised and stress laid on primary prevention and early detection of cancer cases. 1991-92: District Cancer Control Program started 2000-01: Modified District Cancer Control Program initiated 2004 : Evaluation of NCCP by NIHFW 2005 : Program revised after evaluation
- 74. GOAL ANDOBJECTIVE Primary prevention of cancers by health education. Secondary prevention i.e. early detection and diagnosis of common cancer of cervix, mouth, breast and tobacco related cancer by screening method. Tertiary prevention strengthening of the existing institutions of comprehensive therapy including palliative therapy.
- 75. Prevention of tobacco related cancer. Prevention of cancer of uterine cervix. Strengthening of diagnostic and treatment equipment for cancer at medical colleges and major hospitals.
- 76. THE SCHEMES UNDER THE REVISED PROGRAM ARE Regional cancer centre scheme Oncology wing development scheme District cancer control program Decentralized NGO scheme Research and training
- 77. NATIONAL DIABETES CONTROL PROGRAM(7 FYP) • OBJECTIVES Identification of high risk subjects at an early stage and imparting appropriate health education. Early diagnosis and management of cases Prevention, arrest or slowing of acute and chronic metabolic as well as chronic cardiovascular, renal and ocular complication of the disease. Rehabilitation of the partially or totally handicapped diabetic people.
- 78. CHILD WELFARE PROGRAM FOR DISABLED CHILDREN DISABILITY IN FIVE YEAR PLANS 1FYP -Launched a small unit by the ministry of education for the visually impaired in 1947. 2 FYP- under ministry of education a National Advisory Council for the physically challenged started. 3FYP-attention was given to rural areas and facilitated training and rehabilitation of the physically challenged. Cont……
- 79. 4FYP-more emphasis was given to preventive work. 6FYP-national policies were made around for provision of community oriented disability prevention and rehabilitation services to promote self reliance.
- 80. NATIONAL WATER SUPPLY AND SANITATION PROGRAM 1954 OBJECTIVE providing safe water supply and adequate drainage facilities for the entire urban and rural population of the country. Cont……
- 81. SWAJALDHARA (2002) Swajaldhara is a community led participatory program, which AIMS providing safe drinking water in rural areas, with full ownership of the community, building awareness among the village community on the management of drinking water projects, promote better hygiene practices encouraging water conservation practices along with rainwater harvesting.
- 82. MINIMUM NEEDS PROGRAM (1974-78-5 FYP) OBJECTIVES To improve the living standards of the people. It is the expression of the commitment of the government for the “social and economic development of the community particularly the underprivileged and underserved population.” Cont……
- 83. COMPONENTS: Rural health Rural water supply Rural electrification Elementary education Adult education Nutrition Environment improvement of urban slums Houses for landless laborers.
- 84. NATIONAL FAMILY WELFARE PROGRAM (1952) 1951, 100% Centrally Sponsored, concurrent list First country in the world 1961 Family Welfare Dept.- created in 3rd FYP 4th FYP - integration of Family Planning services with MCH services MTP Act introduced 1972 5th FYP(1975-80) The ministry of Family Planning was renamed “Family Welfare”
- 86. Mid day meal program The Mid Day Meal is the world’s largest school feeding programme Mid Day Meal in schools has a long history in India. In 1925, a Mid Day Meal Programme was introduced for disadvantaged children in Madras Municipal Corporation To improving nutritional levels among children, the National Programme of Nutritional Support to Primary Education (NP-NSPE) was launched as a Centrally Sponsored Scheme on 15th August 1995,
- 87. Special nutrition programme (SNP) The programme was launched in the country in 1970-71. It provides supplementary feeding of about 300 calories and 10 grams of protein to preschool children and about 500 calories and 25 grams of protein to expect at and nursing mothers for six days a week. This programme was operated under Minimum Need Programme.
- 88. Beside this 6 national health programme following programme are directly or indirectly helping for child and welfare
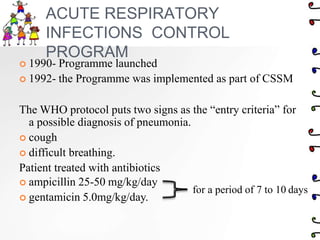
- 89. ACUTE RESPIRATORY INFECTIONS CONTROL PROGRAM 1990- Programme launched 1992- the Programme was implemented as part of CSSM The WHO protocol puts two signs as the “entry criteria” for a possible diagnosis of pneumonia. cough difficult breathing. Patient treated with antibiotics ampicillin 25-50 mg/kg/day gentamicin 5.0mg/kg/day. for a period of 7 to 10 days
- 91. National leprosy eradication program(1992 & 1998) 1955 - Government of India launched National Leprosy Control Programme 1983 - Launched National Leprosy Eradication Programme and introduced MDT for treatment 2005 - India achieved elimination of leprosy at National Level in December’ 05
- 92. NATIONAL LEPROSY CONTROL PROGRAM 1955 SERVICES Provide domiciliary treatment (MDT) Provide services through mobile leprosy treatment units with the help of PHCstaff. Organize health education deformity and ulcer care and medical rehabilitation services.
- 93. National anti malaria programme Strategy: The strategy of control includes early case detection and prompt treatment, Selective use of insecticides, Promotion of personal prophylaxis, Capacity building and epidemic preparedness.
- 95. National AIDS control programme
- 96. NATIONAL AIDS CONTROL PROGRAM (1987) 1987-NACP 1991 –NACP PHASE 1 1992 -National AIDS control organization 1999 –NACP PHASE 2 2011 –NACP PHASE 3
- 97. Objective Prevent infections care, support and treatment . Strengthen- infrastructure, systems and human resources Strengthen the Strategic Information Management System
- 98. STRATEGY Surveillance of HIV infection as indicated by serum positivity. Surveillance of aids cases showing clinical signs & symptoms. Disease control strategies are targeted at three main modes of spread Sexual activity . Self injection by drug addicts HIV infected blood transfusion
- 99. STRATEGY Surveillance of HIV infection as indicated by serum positivity. Surveillance of aids cases showing clinical signs & symptoms. Disease control strategies are targeted at three main modes of spread Sexual activity . Self injection by drug addicts HIV infected blood transfusion
- 100. Training programs for paramedical & general practitioners to enhance their capability of effective STD diagnosis. Counseling for HIV & AIDS patients Cheap availability of good quality condoms. Licensing of blood banks, encouraging voluntary blood donation & screening of blood for HIV, malaria, hepatitis B & C to be mandatory for all.
- 101. National surveillance programme for communicable diseases
- 102. National vector borne disease control programme
- 103. 2003- (NVBDCP) is an umbrella programme for prevention and control of Vector borne diseases. 1. Malaria 2. Dengue 3. Chikungunya 4. Japanese Encephalitis 5. Kala-Azar 6. Filaria (Lymphatic Filariasis)
- 104. NATIONAL MALARIA ERADICATION PROGRAM (1953) 1953 National Malaria Control Programme 1958 National Malaria Eradication Programme 1977 Modified Plan of Operation (MPO). 1995 Implementation of Malaria Action Plan 1997 Enhanced Malaria Control Project in tribal districts of the State (World Bank Assisted) 2000 National Anti Malaria Programme
- 105. OBJECTIV ES To prevent death due to malaria Agricultural and industrial production to be maintained by undertaking intensive anti- malarial measures in such areas.Early case detection and promote treatment. Vector control by house to house spray in rural areas with appropriate insecticide and by recurrent anti larval measures in urban areas. Health education and community participation. Reduction in the period of sickness
- 106. NATIONAL FILARIA CONTROL PROGRAM (1995) ACTIVITES Delimitations of the problem in unsurved areas. Control in urban area through: (a)recurrent anti larval measures (b)anti parasitic measures Control in rural areas through detection and treatment of microfilaria carriers/persons.
- 107. Anti-larval measures which include weekly spray of approval larvacides and biological control through larvivorous fishes. Source reduction through environmental and water management Anti parasitic measure-diagnosis and treatment. community awareness through education Annual single dose (preventive)mass drug administration of DEC (Diethylcarbamazine citrate tablets)
- 108. KALA AZAR CONTROL PROGRAM (1991) STRATEGY Interruption of transmission for reducing vector population by undertaking indoor residual insecticidal spray twice annually. Early diagnosis and complete treatment of kala- Azar cases. Information education and communication for community awareness and community involvement.
- 109. PREVENTION AND CONTROL OF DENGUE HEMORRHAGIC FEVER STRATEGY Surveillance for disease and vectors. Early diagnosis and prompt case management Vector control through community participation and social mobilization. Capacity building.
- 110. National iodine deficiency control program
- 114. GOALS Reduction in IMR and MMR Universal access to public health services Prevention and control of communicable and non communicable diseases. Access to integrated comprehensive primary health care.
- 115. Population stabilization, gender and demographic balance. Revitalize local health traditions and mainstream AYUSH Promotion of healthy life styles
- 116. STRATEGIES enhance capacity of panchayti raj institutions to own, control and manage public health services. Promote access to improve health care at house hold level through the ASHA Health plan for each village through village health committee of the panchayat Strengthening sub-centre through an untied fund to enable local planning and action and more multi-purpose workers.
- 117. Prepared by the district health Mission, including drinking water, sanitation and hygiene and nutrition. Technical support to National, State Block and district levels traditions. Reorienting medical education to support rural health issues including regulation of medical care and medical ethics. Mainstreaming AYUSH revitalization local health.
- 120. National water supply and sanitation programme
- 121. National diarrheal disease control programme
- 122. CONTROL OF DIARRHEAL DISEASE (CDD) PROGRAM (1971) STRATEGY : To train medical and other health personnel in standard case management of diarrhea. Promote standard case management practices amongst private practitioners. Instruct mother in home management of diarrhea and recognition sign which signal immediate care. Make available the ORS (oral rehydration salts) packets free of cost
- 123. TREATME NT The rational treatment of diarrhea consists in prevention of dehydration in a by oral rehydration therapy(ORS) Breastfeeding should be continued. In dysentery given cotrimoxazole in addition to ORS. If unsatisfactory response, nalidixic acid is given for five days. Any program for diarrheal disease control must include provision of portable water.
- 124. Parent must be educated regarding storage of water and food in clear utensils, continue of breastfeeding, using of only freshly prepared weaning foods washing of hands with soap before handling food.
- 125. Currentissues





































![Delivery of services
CDPO ( child development project officer)- in
charge of ICDS projects
Community development black officer(4 supervisor)
supervisor or mukhyasevika (20-25 AWW)
AWW [Anganwadi Workers -for 1000 population]
Anganwadi Helpers (AWH)](https://image.slidesharecdn.com/nationalhealthprogramme-221110095600-e4494e69/85/national-health-programme-ppt-38-320.jpg)