Open fracture management
- 1. OPEN FRACTURE MANAGEMENT BY DR ANIL KUMAR P(junior resident) MODERATOR : DR NAGAKUMAR J S PROFESSOR DEPT OF ORTHOPAEDICS SDUMC
- 2. Definition • Open fracture by definition is communication between external environment and the fracture. • A soft tissue injury complicated by a broken bone.
- 3. • Egyptians 1sttime recognised he need for coverage over fracture wounds to minimise morbidity. • Hippocrates favoured the debridementof purulent material. • Ambroise Parèalso favoured the debridement asthe mainstay of treatment ofopen HISTORY
- 4. • Desault (coined the term ‘debridement) in18th century reiterated this belief by advising debridement of dead necroticmaterial. • Still in the 19thcentury, prior to aseptic technique & antibiotics, emergency amputation wasthe life saving measureafter open fracture.
- 5. • Lastcentury, high mortality with openfractures of longbones • WWI, mortality of open femur fractures>70% • Bythe WWI the main principle of treatmentwas debridement and stabilization & all healing by secondary intention. • 1939 Trueta “closed treatment of warfractures” – Included open wound treatment and thenenclosure of the extremity ina cast – “Greatest danger of infection lay in muscle, not bone”
- 6. • During the WW-II useof local antibioticslike sulfonamides wasstarted for wound treatment. •Useof penicillinon the battlefield quicklyreduced the rate of woundsepsis.
- 7. • Advances shifted the focus Preservation of life and limb preservation of function and prevention of complications • However, amputation rates still exceed 50% in the most severe open tibial fractures associated with vascular injury.
- 8. Epidemiology • Highest rate of fractures are seen in tibia followed femur • Diaphyseal > metaphyseal • Generally aresult of high energy mechanisms which cause greater soft tissue disruption that leaves the wound more susceptible to infection by contaminatingbacteria. • Most Common Causes of Death in the United States Among Individuals 25 to 44 Years Old
- 9. • Fracture pattern • Local factors – Amount of foreign debris and contaminant material – Extent of soft tissue and bonedevitalization. • Systemicfractures – Host nutrition – Medications – Nicotine abuse Prognosis
- 10. COMPONENTS OF OPENFRACTURE 10 • Fracture • Soft-tissue damage • Neurovascularcompromise • Contamination.
- 11. Open fracture classification • Allows comparison of results • Provides guidelines on prognosis and treatment – Fracture healing, infection and amputation rate correlate with the degree of soft tissue injury • Gustilo upgraded to Gustilo and Anderson • AO open fracture classification
- 14. 14
- 15. 15
- 16. 16
- 17. 17
- 18. Nerve Sensate No major nerve 1 injury Dorsal Deep peroneal 2 nerve Plantar partial Tibial nerveinjury 3 Plantar complete Sciaticnerve 4 Ischemia None Good to fair pulses, 0 no ischemia Mild Decreasedpulses 1 perfusion Moderate Prolongedcapillary2 refill,Doppler pulses fill Severe Pulseless, cool, 3 ischemic,no doppler SoftTissue GradeI Minimal 0 contamination GradeII Moderatesoft 1 tissue injury, low velocity GradeIIIA Moderatecrush 2 injury, high velocity with Considerable contamination GradeIIIB Massivecrush 3 injury severe contamination Skeletal Spiral or oblique 0 fracture Transverse 1 fracture-minimal contamination Moderate 2 displacement and communitionwith high velocity Segmental 3 fracture, severe communition,bony loss Shock Normotensive 0 Transient 1 hypotensive Persistent 2 hypotensive 18
- 19. • Gradesof soft tissue injury correlates withinfection and fracture healing Grade 1 2 3A 3B 3C Infection Rates 0-2% 2-7% 10-25% 10-50% 25-50% Fracture Healing (weeks) 21-28 28-28 30-35 30-35 Amputation Rate 50%
- 20. Tscherne Classification for Open Tibial Fractures • This system includes soft- tissue damage and compartment syndrome, which are not included in other grading schemes
- 21. AO-ASIF Soft-Tissue Injury Classification • The AO-ASIF(Association for the Study of Internal Fixation) group added to their extensive fracture classification a soft-tissue classification scheme that closely follows that of Tscherne and Gotzen. • This classification includes both closed and open injuries, musculotendinous injury, and neurovascular injury
- 22. Proposed Classification of Open Fractures (OTA 2010) This new classification uses five categories of assessment: skin injury, muscle injury, arterial injury, contamination, and bone loss. This provides a systemic approach to classification at the time of arrival before treatment has occurred.
- 23. • Number of other trauma scoring systems have been proposed, including • The trauma score (TS), • Revised trauma score (RTS), • Injury severity score (ISS), • Modified abbreviated injury severity scale (MISS), • Pediatric trauma score (PTS), • Nerve injury, ischemia, soft-tissue injury, skeletal injury, shock, and age of patient score (NISSSA), and the • Hanover fracture scale-97 (HFS-97)
- 24. Common bacteria encountered with open fractures • Blunt Trauma, LowEnergy trauma • Farm Wounds • Fresh Water SeaWater wounds • War Wounds, • High Energy gun shot wounds Staph,Strept Clostridia Pseudomonas,Aeromonas Aeromonas, Vibrios GramNegative
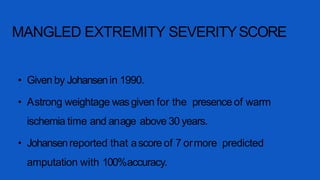
- 25. MANGLED EXTREMITY SEVERITYSCORE • Given by Johansenin 1990. • Astrong weightage wasgiven for the presence of warm ischemia time and anage above 30 years. • Johansenreported that ascore of 7 ormore predicted amputation with 100%accuracy.
- 27. Ganga Hospital Open InjurySeverity Score • GHOISS was proposed by Rajasekaran in 2006 as a score specifically to assess severe Grade IIIB limb injuries without a vascular injury.
- 28. 23
- 30. • Injuries with ascoreof 14 and below should be attemptedfor salvage, 17 and above should be consideredfor primary amputation, in between(15,16) must be assessedbyan experienced team on acase-to-casebasis.
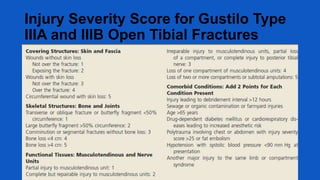
- 31. Injury Severity Score for Gustilo Type IIIA and IIIB Open Tibial Fractures
- 32. Management
- 33. Goalsof treatment • • • 1. preserve life 2. preserve limb 3. preserve function – Prevent infection – Fracture stabilization – Soft tissue coverage
- 34. Stagesof care for openfractures
- 35. Initial assessment traumatized • Important components in assessing extremity are 1. History and mechanism of injury 2. Neurovascular status 3. Sizeof skin wound 4. Muscle crush or loss 5. Periosteal stripping or boneloss 6. Fracture pattern, fragmentation 7. Contamination 8. Compartment syndrome.
- 37. Irrigation • Supplements systemic debridement by removing foreign material anddecreasing bacterial load. • Simpulse irrigation system(HPPL-high pressure pulsatile lavage). • Pressure must be lessthan 50psiunits. Fracturetype Volof fluid usedfor irrigation Type I 3 L Type 2 6L Type 3 9L
- 38. Irrigation NS normally used for irrigation. Antibiotic solution has no advantage than soap for irrigation. Surfactant(non sterile soap): same effectiveness, less tissue damage and more economical.
- 44. Timing of debridement and irrigation • Most guidelines recommenddebridement within 6 hrs and If clean Primaryclosure. • Serial debridement may be necessaryevery 24-72hrs ifdebrima is delayed until the wound viability isensured. • If clean within 2-3 daysdelayed Primary Closure. • Later Secondary closure (Flaps)or healingby Secondary intentions (scarring )
- 46. ANTIBIOTICS AND INFECTION • 24-70% of open fractures are contaminated with bacteria • 14-15% of open complicated fracture with infection in the absence of antibiotic prophylaxis
- 48. Antibiotics • Localantibiotics:-In gustilo type III fractures additional useof local aminoglycoside impregnated polymethylmethacrylate(PMMA) beads reduces overall infection rate.
- 50. Tetanus prophylaxis • Tetanus Toxoid(TT),dose is 0.5ml i.m. regardless of age. • Immunoglobulin:- 75IU <5yrs of age 125IU 5-10yrs 250IU >10yrs.
- 53. Typesof fracture stabilization Splint – Good option if operative fixation not required Internal fixation – Wound is clean and softtissue coverage available External fixation – Dirty wounds or extensivesoft tissue injury
- 54. Primary surgery Timing : •Surgical emergency •Operating within 6-8hrs of injury – contaminated wounds not treated within this time will have sustained bacterialmultiplication to result in earlyinfection.
- 55. Primary surgery Fracture stabilization: •Assoon asprimary wound care is completed, treatment should proceed to fracturereduction and fixation. •Surgeon should rescrub and regown. •Different set of instruments thanthose used for debridement isnecessary.
- 56. Fixation Options External Fixation VsInternal Fixation
- 57. Indications for External Fixation in OpenFractures 1) Severecontamination anysite 2) Periarticular fractures – Definitive • Distal radius • Elbow dislocation – Relative • Knee • Ankle • Elbow • Wrist
- 58. External fixation • Advantages of ExtFixation:- • Canbe applied relatively easily and quickly, • It provides relatively stable fracturefixation, • There is no further damagedone if applied correctly, • Itavoids implantation of hardware in open wound.
- 59. External Fixator • Disadvantages: • Major problems with external fixation are related to pin tract infection, malalignent , delayed union, poor patientscompliance. • Ringfixators may be an optionin open diaphyseal fractures like ilizarov.
- 60. Indications for Internal Fixation in Open Fractures 1)Periarticular fractures – Distal/proximal tibia – Distal/proximal femur – Distal/proximal humerus – Proximal ulnar radius – Selected distal radius/ulna – Acetabulum/pelvis 2) Diaphyseal fractures – Femur – Tibia – Humerus – Radius/ulna
- 61. Plates • Open diaphyseal fractures of the radius andulna as well asthe humerus are best managedwith plate fixation. • The plate fixation of lower extremity diaphyseal fractures is generally not recommended due to higher rate of infections.
- 63. INTRAMEDULLARY NAILING • Locked intramedullary nailing has been established as the treatment of choice for most diaphyseal fractures in lower extremity. • Intramedullary nails can be inserted with no further disruption of the already injured soft-tissue envelope and preserves the remaining extra osseous blood supply to corticalbone.
- 64. IM NAILING • Data showing that solid intramedullary nails inserted without reaming have a lower risk of infection. • On the other hand reamed intramedullary nails can reliably maintain fracture reduction with regards to angulation, rotation, displacement, and length. • Prospective randomised trails that compared reamed with unreamed interlocked IM nails did not show any significant difference concerning outcome and risk of complication.
- 66. Open wound coverage after primary surgery
- 67. Primary Closure The following criteria must be met:- 1.The original wound must have been fairly clean, and not have occurred in a highly contaminated environment. 2.All necrotic tissue and foreign material have been debrided. 3.Circulation to the limb is essentially normal. 4.Nerve supply to the limb is intact. 5.The patient's general condition is satisfactory and allows careful postoperative assessment. 6.The wound can be closed without tension. 7.Closure will not create a dead space. 8.The patient does not have multisystem injuries.
- 68. Delayed primary closure • Closure before the 5th day is termed delayed primary closure. • As long as closure is achieved before the fifth day, wound strengths at 14 days are comparable with those in wounds closed on the first day. • Leaving the wound open minimizes the risk of anaerobic infection, and the delay allows the host to mount local wound defensive mechanisms that permit safer closure than is possible on the first day.
- 69. • Current standard of care for all open fracture wounds is to be left open initially. • Delayed closure is accomplished within 2- 7days • VAC assisted wound closure is presently recommended for temporary management of open fracture wounds.
- 70. VAC • Thewound bed is exposed to mechanically induced negative pressure in aclosed system. • Thesystem removes fluid from extravascular space,reduces edema, improves micro circulation and enhancesthe proliferation of preparative granulation tissue. • Polyurethane foam dressing is placed in wound and ensures an even distribution of negative pressure.
- 71. VAC
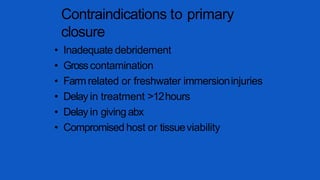
- 72. Contraindications to primary closure • Inadequate debridement • Grosscontamination • Farmrelated or freshwater immersioninjuries • Delay in treatment >12hours • Delay in givingabx • Compromised host or tissueviability
- 73. Dressings • Temporary closures – rubber bands • Wet to dry dressings • Semi-permeable membranes • Antibiotic bead pouch • VAC
- 74. Reconstructive ladder: options for wound coverage Type1open fx Type3Bopen fx Type2/3A open fx
- 75. FLAPCOVERAGE FOR TYPE 3B
- 76. Gunshot injuries • Energydissipated at impact =damage severity • High velocity rifles and closerange shotguns – Worst, high energy of impact – Huge secondary cavitation – Secondary effects of shatteredbone fragments • Bullets lodged in joints should beremoved – avoid lead arthropathy and systemiclead poisoning
- 77. Low velocity GSW<2000ft/sec • Lowvelocity handguns – Lesssevere, not treated like openfractures – Cavitation is not significant – Secondary missile effects are minimal – Bone fragments rarely stripped of softtissue attachments and blood supply – Soft tissue injuries not severe and skin woundsare small
- 78. ADVANCES • BMPs – 40%decreased infection rate with BMPin type3 open tibia fractures • Antibiotic LadenBoneGraft – Tobramycin-impregnated calcium sulfate pellets with demineralized bonematrix – successful in preventinginfection *BESTTStudyGroup, Govender S,CsimmaC,Genant H, Valentin-OpranA. “Recombinant HumanBoneMorphogenetic Protein-2 for Treatment of OpenTibial Fractures: Aprospective, controlled, randomized study of four hundred andfifty patients.” JBJS-A2002. 84(12): 2123-2134. **Beardmore AA,BrooksDE,WenkeJC,ThomasDB.“Effectiveness of local antibiotic delivery with an osteoinductive and osteoconductive bone-graft substitute.” JBJS-A2005. 87(1): 107-112.
- 79. S ummary
- 80. Complications • Hypovolemic shock • Compartment syndrome • Fat embolism • ARDS • Neurovascular injuries • Infection • Morel-Lavallee syndrome
- 82. Hypovolemic shock - management • Two large-bore IV lines should be started. • Once IV access is obtained, initial fluid resuscitation is performed with an isotonic crystalloid, such as Ringer lactate solution or normal saline. • An initial bolus of 1-2 L is given in an adult (20 mL/kg in a pediatric patient), and the patient's response is assessed.
- 83. HYPOVOLEMIC SHOCK • Type of fluid:- • Colloid – albumin, dextran, plasma. Crystalloid – NS, D5, RL. • Blood – uncrossed ‘O’ –ve. • Basic Rule:- • 3:1 rule when using crystalloids.Eg. If blood loss is 100cc the patient should receive 300cc of normal saline or Ringer lactate. • 1:1 rule for colloids.
- 85. Morel-Lavallee syndrome • Skin is separated from the fascia. • This creates a pocket under which considerable bleeding can occur. • Usually this is a subcutaneous hematoma, but the hematoma can become so large that it seriously threatens the viability of the skin above it . • This syndrome occurs frequently in patients with pelvic fractures, especially in obese individuals. • MRI and ultrasonography have been recommended to confirm the diagnosis. • Multiple treatments present but PERCUTANEOUS DRAINAGE is mostly accepted and done.
- 87. Compartment syndrome 34 • Classically 5 "Ps" associated with compartment syndrome:— 1)Pain out of proportion to what is expected 2)Paresthesia 3)Pallor 4)Paralysis 5)Palpable pulse absent.
- 88. Compartment syndrome • Treatment -Fasciotomy
- 89. Fat embolism • Definition - Occlusion of small vessels by fat globules. • Types:- 1.cerebral – drowsy, restless and disoriented. 2.pulmonary – tachypnea, tachycardia, petechial rash(in front of neck, ant axillary fold, chest and conjunctiva )
- 90. Fat embolism • Diagnosis:– • Triad : hypoxia, neurological abnormalities , petechial rash • signs of retinal artery emboli(striate hemorrhages and exudate) may be present. • Sputum and urine may reveal presence of fat globules. • X-ray of chest shows patchy pulmonary infarcts.
- 91. Fat embolism • Treatment:- • Respiratory support • Heparinization • Intravenous low-molecular weightdextran and corticosteriods.
- 92. ARDS • Is caused by release of inflammatory mediators which cause disruption of pulmonary vasculature. • Signs and symptoms– Tachypnea, low BP, Cyanosis. • Treatment – 100% oxygen inhalation.
- 93. Vascularinjury • Absent peripheral pulses in an injured limb should be considered to be due to vascular damage unless proved otherwise. • Classical signs of arterial injury:- (a)absent pulses (b)active hemorrhage (c)expanding hematoma, and (d)bruit or thrill.
- 94. Vascularinjury • • • Investigations:- Colour doppler study Arteriography. Treatment:- Arterial reconstruction Bypassgrafts. Timing:- loss of total blood supply to the limb for >8 hours nearly always results in amputation.
- 95. Nerve injury • Nerve repair should be done within 3 weeksof injury for betterresults
- 96. THANKING YOU