Oral red and white lesionss in dentistry
- 1. ORAL RED AND WHITE LESIONS By SAFA AYAD Supervised by DR.MUSTAFA IBRAHIM
- 2. Introduction • Definition: White and red lesions refer to abnormal changes in the oral mucosa color and texture. • Importance: May indicate benign conditions, infections, or potentially malignant disorders.
- 3. White appearance of oral mucosa 1. Hyperkeratosis 2. Abnormal but benign thickening of stratum spinosum (acanthosis). 3. Intra and extracellular fluid accumulation (edema). 4. Whitish pseudomembranes by microbes (plaque). 5. Fibrosis
- 4. Red appearance of oral mucosa 1. Atrophy of epithelium. 2. Increased vascularization.
- 5. Classification INFECTIOUS DISEASE PREMALIGNANT DISORDER IMMUNOPATHOLOGI C DISEASE ALLERGIC REACTIONS TOXIC REACTIONS REACTION TO MECHANICAL TRAUMA OTHERS 01 02 03 04 05 06 07
- 6. I.Infectous disease I.ORAL CANDIDIASIS ■The most prevalent opportunistic infection affecting the oral mucosa. ■majority of cases, the lesions are caused by Candida albican. ■Divided into primary &secondary infections
- 7. ■number of predisposing factors have been shown to convert C. albicans from the normal commensal flora (saprophytic stage) to a pathogenic organism: Denture wearing Smoking Quality and quantity of saliva Immunosuppressive diseases Immunosuppressive medications Endocrine disorders
- 8. Types of primary candidiasis a.pseudomembranous :creamy white, removable plaques or patches on the oral mucosa,may resemble cottage cheese and can be scraped off, often revealing a red, inflamed, or bleeding surface underneath. ●soreness, burning sensation, difficulty swallowing (if it spreads to the throat). asymptomatic in mild cases.
- 9. b.erthematous:doesn't present with white plaques but instead appears as red, inflamed patches on the oral mucosa. It's often associated with a smooth, shiny surface and can be painful.
- 10. C.Chronic Hyperplastic Candidiasis ■(Chronic Plaque Type) •Also known as candidal leukoplakia. •thick, white, adherent plaques that cannot be easily scraped off •Usually asymptomatic but may cause mild discomfort or a rough texture ■(Chronic Nodular Type) rare, small, raised, nodular lesions rather than flat plaques or diffuse redness.
- 11. d.candida assossiated lesion (Denture stomatitis ) Type I minor erthematous site duo to denture trauma Type II major denture covered mucosa Type III granular mucosa
- 12. (Angular cheilitis) ■ infected fissures of the commissures of the mouth surrounded by erythema ■The lesions are frequently infected with both Candida albicans and Staphylococcus aureus. ■Causes :Vitamin B12 deficiency, iron deficiencies, and loss of vertical dimension and Dry skin
- 13. (Median Rhomboid Glossitis) ■ asymptomatic erythematous lesion in the center of the posterior part of the dorsum of the tongue with an oval configuration. ■This area of erythema results from atrophy of the filiform papillae and the surface may be lobulated. ■ the lesion frequent shows a mixed bacterial/fungal microflora
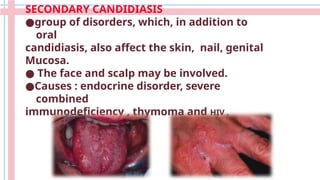
- 14. SECONDARY CANDIDIASIS ●group of disorders, which, in addition to oral candidiasis, also affect the skin, nail, genital Mucosa. ● The face and scalp may be involved. ●Causes : endocrine disorder, severe combined immunodeficiency , thymoma and HIV .
- 15. MANAGEMENT ☆Reduction of predisposing factor like improving denture hygiene , reduction denture porosity , smoke cessation. ☆pseudomembranous ,erythematous__topical antifungal ☆chronic hyperplastic __systemic antifungal ☆type III denture stomatitis __surgical removal ☆Angular cheilitis __topical antifungal like miconazole and moisturizing cream. ☆secondary candidiasis __systemic antifungal
- 16. II.Oral hairy leukoplakia It is caused by the Epstein-Barr virus (EBV). ▪︎ white, corrugated, or "hairy" patches that cannot be ▪︎ scraped off. On the lateral borders of the tongue, though it can ▪︎ occasionally appear on other oral mucosal surfaces like the buccal mucosa or palate. The lesions are typically asymptomatic ▪︎ associated with immunocompromised individuals like ▪︎ HIV/AIDS, organ transplant recipients.
- 17. ■Treatment: Focuses on improving immune function. For example, in HIV patients, antiretroviral therapy can resolve OHL by boosting immunity. Antiviral medications (e.g., acyclovir) may be used ▪︎ to target EBV directly
- 18. 2.premalignant disease I.LEUKOPLAKIA white patches or plaques on the mucous ■ membranes of the mouth that cannot be wiped off it has the potential to develop into oral cancer, ■ particularly squamous cell carcinoma risk factors (smoking , excessive alcohol ■ consumption, chronic irritation (e.g., from sharp cusps or ill-fitting dentures).
- 19. main types include: 1. Homogeneous Leukoplakia • Uniformly white, flat, and smooth plaques with a consistent texture. • lower risk of malignant transformation. 2. Non-Homogeneous Leukoplakia • Irregular, mixed white and red patches (sometimes called erythroleukoplakia), with a nodular, verrucous (warty), or speckled surface. • higher risk of progressing to cancer 15-40%.
- 20. • Subtypes: Nodular: Small, raised bumps on the surface. ■ Verrucous: Warty or corrugated appearance. ■ Speckled: Mixed red and white areas, often with ■ an uneven texture.
- 21. 3. Proliferative Verrucous Leukoplakia (PVL) • A rare, aggressive subtype with multiple, widespread warty lesions that tend to recur and spread over time. • Highly resistant to treatment and has a strong tendency to transform into squamous cell carcinoma (up to 70-100%).
- 22. MANAGEMENT a.homogenous __eliminate the irritant +follow up every (3_6)weeks. b.non homogenous__eliminate the irritant+surgical removal+follow up biopsy to role out cancer. C.PVL__wide surgical excision +biopsy follow up every (1_3)months.if biopsy show malignant transformation then chemotherapy or radiotherapy needed.
- 23. II. ERYTHROPLAKIA • red lesion or patch that has appearance of Smooth, velvety, or granular red areas, often sharply defined. • Commonly found on the floor of the mouth, tongue, or soft palate • Rare, less frequent than leukoplakia. • Risk Factors: smoking or , alcohol consumption, and sometimes human papillomavirus (HPV) infection. •Malignant Potential: High risk-up to 90%
- 24. •asymptomatic or report mild discomfort, burning, or soreness. •Unlike leukoplakia, erythroplakia rarely causes noticeable thickening. •Duration: Lesions persisting beyond 2-3 weeks despite removing potential irritants • Management: • Eliminate Risk Factors. • Surgical Removal. • Follow-Up
- 25. III.ORAL SUBMUCUS FIBROSIS •A progressive, precancerous fibrosis of the submucosal tissues leading to stiffness and restricted mouth opening. • Cause: chronic use of areca nut (betel quid), nutritional deficiencies, genetic predisposition, and autoimmune processes.
- 26. •Pale, marble-like mucosa with palpable fibrous bands in the cheeks, lips, or palate. May develop ulcers . •Reduced mouth opening (trismus), stiff cheeks, difficulty swallowing or speaking, and sometimes hearing loss due to Eustachian tube involvement. MANAGEMENT EARLY __cessation habit +Intralesional steroids +physiotherapy (excersice to adjust mouth opening). ADVANCED __ surgical intervation.
- 27. 3.lmmunopathologic disease I. LICHEN PLANUS (LP) is a common chronic immunologic inflammatory mucocutaneous disorder. (Skin lesion ) characterized by Kobner's phenomena (development of new lesion on normal looking skin following trauma as scratching).
- 28. (Oral lesion) •Bilateral esions surrounded by a network of bluish white lines called Wickham's striae radiating from periphery of the lesion. •pain or discomfort, which interferes with function. FORMS OF THE LESION RETICULAR PAPULAR PLAQUE ATROPHIC EROSIVE BULLOUS
- 29. Causes . Autoimmune reaction . Stress . Medications . Hepatitis c . Diabetes millitus MANAGEMENT Reticular, plaque, papules __No treatment and follow up Atrophic, erosive__ Corticosteroids + Retinoids
- 30. II.LICHENOID REACTION associated with the administration of a drug, contact with a metal, the use of a food flavoring, or systemic disease. resolution when the drug or other factor was eliminated
- 31. III.LUPUS ERYTHEMATOUS •Systemic lupus erythematosus (SLE) multi-organ damage with disk shaped skin scar . • Discoid lupus erythematosus (DLE) is affecting the oral cavity+skin lesion has butterfly distribution on tip and bridge of the nose. • Subacute cutaneous lupus erythematosus intermediate between SLE
- 32. Causes 1-Immunologic formation. 2- Genetic factors. 3-Infectious (EBV, CMV, VZV). 4. environmental (e.g.sun exposure). 5- Endocrine factors: (hormones). (Oral lesion) •central atrophy, scar formation, and occasional loss of surface pigmentation. • The primary locations for these lesions include the buccal mucosa, palate, tongue
- 33. MANAGEMENT Improve oral hygiene DLE__Topical corticosteroids SLE __ Systemic corticosteroids
- 34. 4.Allergic reactions Dentifrices and mouthwashes allergy •The Lesions are usually located on the Mucobuccal folds and Gingiva. •irregular in shape, white, covered with a pseudomembrane, and very painful.
- 35. 5.Toxic reactions I.SMOKLESS TOBACCO INDUCED KERATOSIS •The surface of mucosa appears white and granular or wrinkled. •These lesions are accepted as precancerous. • area of gingival recession with periodontal-tissue destruction in the area of contact on facial aspect of the teeth . •The lesion is asymptomatic .
- 36. II.NECOTINE STOMATITIS Due to the chronic insult, the palatal mucosa becomes diffusely gray or white. Numerous slightly elevated papuleswith punctate red centers that represent inflamed altered minor salivary gland ducts are noted.
- 37. 6.Reaction to mechanical trauma I.LINEA ALBA It is a horizontal white streak on the buccal Mucosa bilaterally at the level of the occlusal plane from the commissure of mouth to the posterior teeth.
- 38. II. FRICTIONAL KERATOSIS • Frictional (traumatic) keratosis is defined as a white plaque with a rough surface that is clearly related to a source of mechanical irritation . •Frictional keratosis is frequently associated with rough or maladjusted dentures and with sharp cusps .
- 39. 7.others I.LEUKOEDEMA • Diffuse grayish-white milky appearance of thebuccal mucosa • Appearance will disappear when cheek is stretched. Managment • No treatment is indicated
- 40. II. BENIGN MIGRATORY GLOSSITIS asymptomatic red, smooth patches on the tongue with irregular white borders. • Patches change in size, shape, and location over time (hence "migratory"). •papillae are absent or flattened in certain areas, creating smooth, red patches. •The loss of papillae in these patches is temporary and reversible.
- 41. III.WHITE SPONGY NEVUS • rare autosomal dominant disorder. It present from birth and appear during childhood. • Presents as bilateral white, soft, "spongy," or velvety thick plaques of the buccal mucosa. • Other sites in the oral cavity may be involved, including the ventral tongue, floor of the mouth, labial mucosa, soft palate, and alveolar mucosa. • asymptomatic • require no treatment
- 42. THANK YOU