SupraAD-1.ppt
- 1. SUPRAGLOTTIC AIRWAY DEVICES DR. KUNAL KISHORE GUPTA MODERATOR 1 DR. ADITYA KEJRIWAL MODERATOR 2 DR. JANKI N THAKUR
- 2. SUPRAGLOTTIC Airways that are intended to open, secure & seal the supraglottic area to provide an unobstructed airway in spontaneously breathing or ventilated patients, typically during anesthetic procedures INFRAGLOTTIC Below the glottis opening Definitive airway- ET tube, tracheostomy Emergency airway - cricothyrotomy
- 3. HISTORY Dr Archie Brain - first credited with invention & development of LMA He first used a Goldmans mask and attached it a obliquely cut endotracheal tube. It was introduced in 1982.
- 4. CLASSIFICATION 1st and 2nd GENERATIONS DEVICES 3rd GENERATION SUPRAGLOTTIC AIRWAY DEVICES?
- 5. INDICATION SAD have been recommended as rescue airways during DA management and in particular “cannot intubate ,cannot ventilate” scenario Alternative airway during GA specially in minor surgeries & therapeutic or diagnostic procedures like RT, endoscopy, ECT etc. Cardiopulmonary resuscitation to secure the airway. Essential part of difficult airway trolley. Primary airway device when urgent airway patency is required in lateral position.
- 6. CONTRAINDICATION Limited mouth opening (<2fingers) Local pathology inpharynx,larynxorupperairway. Trismus,facial orupper airwaytrauma Increaseriskof aspiration-Morbid obese, >14week pregnant, full stomach. Prior opioid medication, delayed gastric emptying, acute abdominal orthoracic injury, GERD,hiatushernia Reduced lung compliance/increase workof breathing
- 7. ADVANTAGES OF THE SGAs Avoidance of laryngoscope, less invasive means of securing airway. Increased ease of placement. Can be placed in neutral position. Higher success rate with inexperienced personnel. Better tolerated by patients- less trauma, coughing & post op sore throat. Improved oxygen saturation during emergency Improved hemodynamic stability. Minimal increase in iop, icp during insertion.
- 8. DISADVANTAGES Inadequate positive pressure ventilation. Vascular compression and nerve damage. Can cause laryngospasm if displaces anteriorly. More chances of aspiration of gastric contents.
- 9. ROLE OF THE LMA IN ASA’S DIFFICULT AIRWAY ALGORITHM. LMA or any SAD now find its role in the management of the difficult airway at 5 places in the ASA’s algorithm either as: Ventilatory devices As a conduit to tracheal intubation
- 10. DAS guidelines for management of unanticipated difficult intubation in adult
- 11. THE NEW 2022 ASA DIFFICULT AIRWAY ALGORITHM
- 13. STEPS TO REDUCE THE CHANCE OF ASPIRATION Avoid in patients who are un-fasted, or have factors predispose to regurgitation. Routinely test the cuff for defects before use. Avoid lubricating the anterior surface of the mask, since the lubricant may be aspirated. Insert the LMA only when adequate depth of anesthesia has been reached. Avoid disturbing the patient during emergence from anesthesia. Keep the cuff inflated till the patient is awake. If aspiration does occurs Dr. Brain AIJ recommends leaving the LMA in place, tilting the patient’s head down and suctioning through the LMA
- 14. LMA- Classic Comprised of three main components Airway Tube Mask Inflation line Designed to confirm contours of hypopharynx with its lumen facing the laryngeal opening. Made of silicone, can be autoclaved & reused many times. Seal pressure =25cmH2O
- 15. Mask Size Patient size /Body Weight Maximum Cuff Inflation Volume (Air) 1 Neonates/Infants up to 5 kg Up to 4 mL 1.5 Infants 5–10 kg Up to 7 mL 2 Infants/Children 10–20 kg Up to 10 mL 2.5 Children 20–30 kg Up to 14 mL 3 Children 30–50 kg Up to 20 mL 4 Adults 50–70 kg Up to 30 mL 5 Adults 70–100 kg Up to 40 mL 6 Large Adults over 100 kg Up to 50 mL SIZE SELECTION
- 16. PREPARATIONPRIORTO INSERTION Select proper size of LMA. ▶Inspect for any tear , blockage . ▶Slowly deflate the cuff to form a smooth flat wedge shape . ▶Over inflate: look for leak. ▶Use a water soluble lubricant to lubricate the posterior surface of LMA ▶Avoid excessive of lubricant & lignocaine jelly for lubrication .
- 17. INSERTIONTECHNIQUE Position: Neck flexed and head extended. Use non-inserting hand to stabilize occiput. Grasp like a pen with index finger pressing the point where tube joins mask. Place tip of LMA against inner surface of patient’s upper teeth. Aperture facing forward, the tip pressed upwards against hard palate. Mask is advanced into pharynx to ensure that tip remains flattened and avoids tongue.
- 18. Neck is kept flexed and head extended. Continue pushing with index finger and guide it downward. Grasp tube firmly with other hand & then withdraw index finger. Press gently downward with other hand to ensure mask is fully inserted.
- 19. Inflate the mask with the recommended volume of air. Normally it should be allowed to rise up slightly out of hypo pharynx as it is inflated to find its correct position. Insert a bite-block or roll of gauze to prevent occlusion of the tube. Now the LMA can be secured.
- 21. OTHERMETHODS OF INSERTION Thumb index method. Partial inflation method. 180degree rotationmethod. Laryngoscopy aided method. Stylet ora bougieaided method. Insertion from side of mouth opening. In a patient with restricted mouth opening LMA can be placed retromolar and subsequently LMA tube is brought forward to lie centrally.
- 22. SIGNS OF CORRECT PLACEMENT slight outward movement of tube upon LMA inflation. presence of smooth oval swelling in the neck around thyroid and cricoid area, or no cuff visible in oral cavity. Ventilate the patient while confirming equal breath sounds over both lungs in all fields and the absence of ventilatory sounds over epigastrium Distal tip of silicone cuff- Upper esophageal sphincter Sides of cuff- Pyriform fossa Upper part of cuff -Tongue base
- 23. PROBLEMS Failure to press the deflated mask up against hard palate or inadequate lubrication or deflation can cause the mask tip to fold back on itself. Folding mask tip may progress, pushing the epiglottis causing mechanical obstruction . inadequately deflated mask may either – 1. Push down the epiglottis 2.Enter the glottis.
- 24. PROSEAL LMA Reusable , silicon made , most specialized modification of c-LMA. Modifications:- (i)oesophageal drain tube (ii)posterior inflatable cuff (iii)reinforced airway tube (iv)integral bite block (v)introducer Higher leak pressure(35cm of H2O) than c- LMA(25cm of H2O). Size- in 7 sizes (1-5) like C-LMA with drainage tube of 8, 10, 10, 14, 16, 16 &18 Fr respectively.
- 25. ADVANTAGES Increased airway seal improves the PPV. Decreased chance of aspiration- 1.Oesophageal opening is isolated from the airway. 2.Drain tube vents gas leaked into the oesophagus. 3.On regurgitation drain tube vents the fluid & small solid particles beyond the pharynx. 4.The large bulk of the PLMA reduces the space available for regurgitated fluid to ‘pool’. 5.Increased oesophageal and pharyngeal seal decreases the risk of any pooled fluid entering the laryngeal inlet. Simple tests enable correct positioning of the PLMA to be confirmed. The stomach may be accessed with an orogastric tube.
- 26. LMA - UNIQUE Single use PVC made Cheaper. Tube – stiffer Cuff- less compliant Less rise of intracuff pressure with N2O. Size same as cLMA.
- 27. LMA - SUPREME Single use, PVC made 2nd generation LMA. Has features of P-LMA, I-LMA & LMA unique. (i) Large inflatable plastic cuff, but no posterior cuff (ii)Oesophageal drain tube (iii)Preformed semi-rigid tube (iv) Fins in the mask bowl to prevent epiglottic obstruction Pharyngeal seal is intermediate between cLMA and PLMA( 26–30 cm H2O)
- 28. ADVANTAGES The reinforced tip reduces the risk of fold-over, compared with the PLMA. Anatomic curve that facilitates easy insertion. A drain tube to allow gastric aspiration: I. A high value / low pressure cuff which generates higher seal pressure II. A built-in bite block and fixation tab to help secure the airway. III. An oval airway cross section for improved stability of the airway.
- 29. DISADVANTAGES Drain tube runs through the middle of the airway tube (rather than next to it in the PLMA) dividing it into two narrow lumens. This limits its use for airway inspection. and for use as a conduit for intubation. Being made of PVC, the SLMA may cause more trauma than silicone devices.
- 30. GUARDIAN SUPREME AIRWAY It is new silicone based single use extraglottic airway device. It forms a seal with the glottis for ventilation and with hypopharynx for airway protection. Provides a gastric drainage port. In addition it has a port with suctioning material from the hypopharynx and pilot balloon valve with pressure logo ( Yellow< 40 cm H2O, Green 40-60 cm H2O and Red > 60 cm H2O), that indicate visual intra-cuff pressure.
- 31. In addition it has a port with suctioning material from the hypopharynx and pilot balloon valve with pressure logo ( Yellow< 40 cm H2O, Green 40-60 cm H2O and Red > 60 cm H2O), that indicate visual intra-cuff pressure.
- 32. FLEXIBLELMA Flexometallic tube- narrower & longer. ▶ Has a rigid preformed angle at cuff. ▶ Seal pressure = 20cmH2O ▶ Introducer helps to stabilize airway tube during insertion ▶ less incidence of dislodgement once placed. ▶ More useful in head & neck surgeries, ENT and upper torso procedures where need to reposition the airway ▶ Problems- Disruption of spiral reinforce wire, Increased airway resistance , limits endoscope & tracheal tube passage , unsuitable for MRI.
- 33. AMBU AURA LMA single-use LM with a preformed curve. ▶ The Ambu Aura40 is the reusable, silicone version. ▶ The Ambu Aura-i designed to facilitate intubation like ILMA. ▶ 3 parts- an airway tube, a mount area, and a bowl including the inflatable cuff.. ▶ A reinforced tip reduces the risk of folding back during insertion. ▶ integrated inflation line and no epiglottic bars at the airway orifice.
- 34. COBRA PERILARYNGEAL AIRWAY (PLA) single use, PVC made, latex free . has a breathing tube with large inner diameter to increase air flow. Novel head design- Grill of soft bar with Cobra head shape. Bars allow ventilation & instrumentation. Internal ramp to guide ETT Proximal high volume low pressure cuff- seals hypopharynx. offers a more effective seal, and a better fiberoptic score as the c-LMA.
- 35. LARYNGEAL TUBE Cough pressure60cmH2O 4types- LT, LT-D,LTS-II, LTs-D
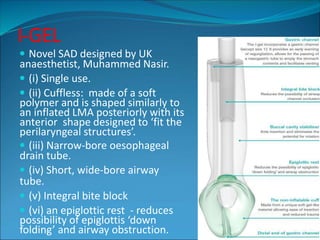
- 36. I-GEL Novel SAD designed by UK anaesthetist, Muhammed Nasir. (i) Single use. (ii) Cuffless: made of a soft polymer and is shaped similarly to an inflated LMA posteriorly with its anterior shape designed to ‘fit the perilaryngeal structures’. (iii) Narrow-bore oesophageal drain tube. (iv) Short, wide-bore airway tube. (v) Integral bite block (vi) an epiglottic rest - reduces possibility of epiglottis ‘down folding’ and airway obstruction.
- 37. i-gel Size Patient size Patient weight guidance(Kg) 1 Neonates 2-5 1.5 Infants 5-12 2 Small paediatric 10-25 2.5 Large paediatric 25-35 3 Small adult 30-60 4 Medium adult 50-90 5 Large adult 90+ SIZE SELECTION
- 38. ADVANTAGES 1. Easy to insert: due to a combination of a very low coefficient of friction when lubricated & absence of cuff. 2. Wide lumen make it well worth for both airway rescue and as a conduit for assisted intubation. 3. A gastric channel allows for suctioning and placement of a nasogastric tube. 4.Though oesophageal seal is low but enough (according to the manufacturer).
- 39. STREAMLINEDLINEROF THE PHARYNGEAL AIRWAY(SLIPA) Plastic made, uncuffed, disposable ,2nd generation SAD. ▶ Anatomically pre-shaped to line the pharynx. ▶ Hollow & boot shaped distal part- 1. Toe- rest in oesophageal entrance 2. Bridge- fits to pyriform fossa. 3. Heel- anchor in position & connect the airway tube. 4. Two lateral bulges- relieve pressure on hypoglossal& recurrent laryngeal n. 5. Large capacity chamber-stores regurgited fluid. Available in 6 sizes- : 47, 49, 51, 53, 55& 57 mm.
- 40. BASKA MASK
- 42. INTUBATINGLMA modification of c-LMA. A rigid (stainless steel) anatomically curved, short & wide bored shaft that follows anatomical curve of palate & post pharyngeal wall. An epiglottic elevator bar at mask aperture Armoured flexible ET tube with a longitudinal and a horizontal black line- coincides with epiglottic elevating bar. Stabilizer Rod of 25cm. Seal pressure=60cmof H2O max. Body weight ILMA size Air volume Tracheal Tube 30-50kg 3 20ml 7mm 50-70kg 4 30ml 7.5mm 70-100kg 5 40ml 8mm
- 43. LMA C-Trach Enables combined ventilation, visualization& intubation. ⚫ High first attempt intubation success rate of 91%. ⚫ Fiberoptic technology allows real time visualization of glottic opening & of ET tube passing through vocal cords. ⚫ Ideal in rescue/difficult airway situations ⚫ Completely portable and wireless system - weighs less than 8 ounces. ⚫ Easy to learn and very effective
- 44. AIR-Q (INTUBATING LARYNGEAL AIRWAY AND COOK GAS ) Designed as intubating conduit No aperture bars Shorter, allows ETT to reach vocal cords Accommodates conventional ETT Can be left in situ during case which may be utilized during emergence
- 45. ESOPHAGEAL- TRACHEALCOMBITUBE PVC double lumen SAD with 2 inflatable balloons 2 Lumens : tracheal and pharyngeal Proximal balloon- seals oral & nasal cavity Distal balloon - seals either esophagus or trachea, depending on which of these ETC has been sited. Size- 37 Fr for height up to 5 ft. 41 Fr for height above 5.5 ft. Between 5-5.5ft – either of these.
- 48. Classification based on evolution 1st generation devices 2nd generation devices Classic LMA Flexible LMA Laryngeal tube Cobra PLA Proseal LMA I-Gel LMA supreme SLIPA 3rd generation devices- Baska mask
- 49. Based on sealing mechanism (MILLER’S CLASSIFICATION)– 1.Cuffed perilaryngeal sealer:- Non-directional non esophageal Sealers- cLMA, Flexible LMA, LMA unique. Directional Non-esophageal sealing- Fastrach LMA, ALMA. Directional esophageal sealing- Proseal LMA, Supreme LMA. 2.Cuffed pharyngeal sealer:- Without esophageal sealing: COPA, PAX. With esophageal sealing: Combitube, LT, LTS. 3.Cuff less preshaped sealer: - With esophageal sealing- Baska mask, i-gel. Without esophageal sealing- SLIPA , AirQ-SP.
- 50. BASED ON THE NUMBER OF LUMEN- 1. Single Lumen Devices:- LMA-classic, LMA-unique, LMA-flexible, I LMA, C-trach, Laryngeal Tube, SLIPA 2. Double Lumen Devices:- Proseal LMA, Combitube, I gel , Laryngeal Tube Suction, Airway Management Device(AMD) 3 . Triple Lumen Devices:- Elisha Airway Device(EAD)
- 51. SEALING PRESSURES OF DIFFERENT SADs
- 52. SOME IMPORTANT FEATURES OF THE PRESENT DAY SUPRAGLOTTIC AIRWAY DEVICES
- 53. CONTINUE….
- 54. SUMMARY Recent advances in SAD design have significantly enhanced the clinical utility. SADs play an important role in rescue ventilation in DA(DMV,DL,TI). Can be used as conduit for intubation and bronchoscopy. Can be used by paramedics with adequate training to secure airway. Knowledge about indications and contraindications and features of device essential for their appropriate use. Correct insertion technique must be carefully followed to ensure optimal positioning. Concerns such as pulmonary aspiration of gastric contents remain, necessitating careful patient selection, device selection. Checks for function and position should be done everytime the device is placed.
- 55. If you are not willing to learn, No one can help you! If you are determined to learn, No one can stop you! THANK YOU!
- 56. Questions 1. Advantages of SGA’s ? 2. Contraindications of SGA’s ? 3. DAS guidelines for management of unanticipated difficult intubation in adult ? 4. Steps to reduce the chance of aspiration ? 5. Advantages of Proseal LMA ?