wilsons disease (movement disorder)
- 2. Objective INTRODUCTION PREVALANCE PATHOPHYSIOLOGY CLINICAL FEATURES LABORATORY DIAGNOSIS TREATMENT SUMMARY REFERENCES
- 3. Introduction ● Wilson disease, or hepatolenticular degeneration, is a disease caused by faulty copper metabolism. The toxic effects of copper lead to degeneration of the liver and the basal ganglia ● It was first described in 1854 by German pathologist Friedrich Theodor von Frerichs and is named after British neurologist Samuel Wilson. ● It is inherited as an autosomal recessive trait localization of the gene associated with WD on chromosome 13 the cause of disorder in mutation is gene on chromosome 13 which encodes a copper transporting ATPase ● Inability to excrete copper into bile leads to accumulation in liver and brain
- 4. ● WD can present clinically as liver disease, a progressive neurological disorder (hepatic dysfunction being less apparent or occasionally absent), a psychiatric illness , or as a combination of these ● The age of presentation for symptomatic WD is both younger and older than generally appreciated. 3– 55 years- old. ● WD is increasingly diagnosed in children who are less than5 years- old. Clinical findings may be nonspecific in children who are less than 2 years- old. ● It is caused from the mutation of the ATP7B gene, and leads to the accumulation of copper in key organs such as the liver, central nervous system, kidney, cornea and other tissues, resulting in impaired function. The deposition of copper begins immediately at birth, with symptoms usually presenting in late adolescence.
- 5. PREVALANCE ● Wilson’s disease is a rare condition, affecting only one person in 30,000 in most populations. ● This condition is considered an autosomal recessive. ● The gene frequency for this disease has been found to be 56%, with a carrier frequency of 1 in every 90 people. ● According to recent studies, an increase incidence of this gene mutation has been found in isolated populations ● Symptoms usually begin between the ages of 5 and 35 years. ● 1% of population being heterozygotes
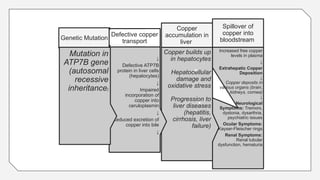
- 6. PATHOPHYSIOLOGY ● the gene associated with WD on chromosome 13, it was identified as encoding a metal- transporting P-type adenosine triphosphatase(ATPase). This gene, ATPase copper transporting beta (ATP7B), is expressed mainly in hepatocytes ● The gene product ATP7B facilitates transmembrane trans-port of copper within hepatocytes. ● Absent or impaired ATP7B function decreases biliary excretion of copper ,resulting in toxic hepatocellular copper accumulation. Eventually exceeding storage capacity, hepatic copper released into the bloodstream deposits in other organs, notably the brain, kidneys, and cornea ● Loss of functional ATP7B diminishes hepatocellular biosynthetic incorporation of copper into ceruloplasmin. This explains the decreased blood level of ceruloplasmin in most patients with WD because apoceruloplasmin has a shorter circulating half-life than ceruloplasmin
- 7. Increased free copper levels in plasma ↓ Extrahepatic Copper Deposition ↓ Copper deposits in various organs (brain, kidneys, cornea) ↓ Neurological Symptoms: Tremors, dystonia, dysarthria, psychiatric issues Ocular Symptoms: Kayser-Fleischer rings Renal Symptoms: Renal tubular dysfunction, hematuria Spillover of copper into bloodstream Copper builds up in hepatocytes Hepatocellular damage and oxidative stress Progression to liver diseases (hepatitis, cirrhosis, liver failure) Copper accumulation in liver ↓ Defective ATP7B protein in liver cells (hepatocytes) ↓ Impaired incorporation of copper into ceruloplasmin ↓ Reduced excretion of copper into bile ↓ Genetic Mutation Mutation in ATP7B gene (autosomal recessive inheritance) Defective copper transport
- 11. CLINICAL FEATURES ● Hepatic • Asymptomatic hepatomegaly • Isolated splenomegaly • Persistently elevated serum aminotransferase activity (AST, ALT) • Fatty liver • Acute hepatitis • Resembling autoimmune hepatitis • Cirrhosis: compensated or decompensated • Acute liver failure
- 13. ● Neurological • Movement disorders (tremor, involuntary movements) • Drooling, dysarthria • Dysphagia • Rigid dystonia • Pseudobulbar palsy • Dysautonomia • Migraine headaches • Insomnia • Seizures
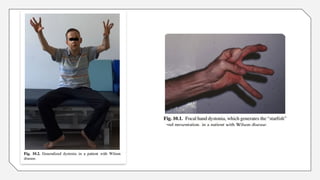
- 15. ● the clinical photograph shows severe generalized dystonia. There are mouth open, limb and truncal dystonia leading to bedridden state, nasogastric feeding, and anarthria.
- 16. ● The connection of copper with metabolism may account for the basal ganglia involvement. ● Neuronal degeneration is present in the globus pallidus and putamen and to a lesser extent in the caudate nucleus(together called the lenticular nucleus). Atrophy- in the gray matter of the cortex and the dentate nucleus of the cerebellum ● The postures and movement patterns seen in people with Wilson disease include dystonic movements involving twisting and rotation of limbs, with sustained contraction at the end of the movement ● Wilson disease progresses, the classic abnormal posture of increased flexion occurs, along with rigidity that can progress to the inability to move if severe enough.
- 18. ● Dystonia, like bradykinesia and choreoathetosis, belongs on a continuum of the extraneous movements present with basal ganglia involvement. ● Dysfunction of the cerebellum and intralaminar nuclei of the thalamus may also contribute to these impairments of posture and movement. ● A peculiar aspect of dystonia is that it can be decreased with proprioceptive or tactile inputs.
- 19. ● Dystonia in WD can be focal, segmental, or generalized; the focal dystonia of facial expression causing involuntary smiling (risus sardonicus) is fairly common. ● Tremor can also be present at rest, with posture, or with action. The well- described rubral wing- beating tremor occurs infrequently. ● Sensory symptoms and weakness representing peripheral neuropathy are very unusual as the presentation of WD.
- 20. THE NEUROLOGIC CLASSIFICATIONS OF DISEASE ● A dystonic form presents with dysarthria, dysphagia, and drooling of saliva due to dystonia of the face and bulbar musculature. In contrast to a pseudobulbar palsy, the jaw jerk is not increased. Eventually there may be a characteristic fixed facial dystonia and sometimes stridor. Dystonia of the limbs leads to rigidity, abnormal postures, and a dystonic gait . the patient becomes severely dysarthric, unable to swallow, and immobile ● the tremor-predominating form are those with cerebellar which occurs in adults with a relatively mild disease course (also called the pseudosclerosis form); an akinetic-rigid presentation with prominent resting or postural tremor and variable bradykinesia, rigidity, and facial immobility. The tremor of the arms may be very severe (wing beating tremor) causing injury ● gait ataxia, dysarthria, loss of limb co-ordination, and titubation of the head.
- 23. ● Psychiatric • Depression-The prevalence of depression inpatients with WD varies broadly (4%– 47% • Neurotic behaviours • Personality changes • Psychosis • Anxiety • Sleep disturbance • Cognitive problems- • Bipolar disorders/bipolar spectrum-Prevalence of bipolar disorder in patients with WD is approximately 18%– 39% ● Approximately two thirds of patients had psychiatric symptoms at the beginning of their illness, with or without hepatic or neurological findings
- 24. ● Other Systems • Ocular: Kayser-Fleischer rings, sunflower cataracts • Cutaneous: lunulae ceruleae • Kidney: Renal abnormalities: aminoaciduria and nephrolithiasis • Skeletal abnormalities: premature osteoporosis and arthritis • Cardiomyopathy, dysrhythmias • Pancreatitis • Hypoparathyroidism • Menstrual irregularities; infertility, repeated miscarriages
- 25. ● Wilson's can also have an ocular manifestation as a Kayser-Fleischer ring around the eye from copper deposits and a sunflower cataracts in the lens, which is less commonly observed compared to the Kayser-Fleischer ring ● The deposition of the excess copper in the cornea results in the classic diagnostic sign of Wilson disease, the KayserFleischer ring: a brownish-green or brownish-red ring found in the sclerocorneal junction ● Descemet's membrane ● The rings first appear in the superior cornea and may not be visible unless looked for specifically with a slit lamp by an experienced ophthalmologist ● In patients with non-neurological presentations of Wilson's disease, KF rings are less reliable. Not only may they be absent in hepatic Wilson's disease but some other forms of liver disease such as primary biliary cirrhosis may be associated with them.
- 27. Stages of the Disease ● The first symptom of Wilson disease is usually a change in the individual’s personality ● when this becomes severe enough or when the movement disorder appears, a diagnosis can be made by the presence of the Kayser-Fleischer ring in the eye or by an analysis of copper metabolism ● If left untreated, the dystonia becomes worse and the person becomes more rigid. In addition, muscle weakness can occur and progress, seizures may develop, and the dementia and personality disorder also become worse
- 28. Medical Management ● Pharmacological treatment of Wilson’s disease is based around the removal of excess copper from the body, as well preventing the accumulation of it in target organs ● Chelation therapy drugs, such as Penicillamine and Trientine are used to remove excess copper from the affected organs; they act as binding agents and are removed through urinary excretion. ● Zinc salts are also used to block the intestinal absorption of copper, reducing its accumulation in the body. ● Zinc salts are shown to be very effective, and is an advantage over other pharmacological agents because of its lack of side effects ● If the copper imbalance is treated, the neurological signs do not progress ● D-Penicillamine: ● Trientine Dosage: ● Zinc Dosage
- 29. Diagnosis ● Biochemical liver tests ● Ceruloplasmin ● uric acid-Urine copper is elevated in Wilson's disease and is collected for 24 hours . Levels above 100 μg/24h (1.6 μmol/24h) confirm Wilson's disease ● Liver biopsy ● Radiocopper study ● Magnetic resonance imaging (MRI) ● Computerized tomography (CT) and other radiologic imaging ● Genetic studies
- 34. diet ● In general, a diet low in copper-containing foods is recommended. High-copper foods avoided in Wilson's disease include mushrooms, nuts, chocolate, dried fruit, liver, sesame seeds, sesame oil, and shellfish.
- 35. Physiotherapy management • Goals of Physiotherapy: • Improve motor function and coordination. • Manage muscle rigidity and tremors. • Enhance balance and prevent falls. • Support overall physical conditioning and quality of life. • Techniques: • Motor Training: Exercises focusing on fine and gross motor skills. • Balance Training: Exercises to improve stability and prevent falls. • Coordination Exercises: Activities to enhance hand-eye coordination. • Strengthening Exercises: Focused on improving muscle strength and reducing rigidity. • Patient Education: • Importance of adherence to treatment. • Guidance on home exercises and fall prevention.
- 36. ● treatment techniques should be wholly based on symptoms. Examination is similar to that of the person with Parkinson or Huntington disease. ● It consists of describing the type of extraneous movement present, when it is present, and factors that influence the degree of dystonia. ● Ease of movement should also be assessed and may be timed as for the patient with Parkinson disease. In addition, range of movement and strength should be evaluated, especially if the disease is progressing. ● Treatment is then designed to alleviate the problems. Extraneous movements may be reduced by any technique that will reduce tone. ● Positioning is important. ● If bradykinesia is the major sign, then treatment would be similar to that used for people with Parkinson disease. The client with Wilson disease has knowledge of what normal movement feels like and usually has good cognitive abilities at the time treatment is started. Because of the emotional lability, which is one of the first symptoms in this disease, the treatment session should be well planned and quite structured
- 40. REFERENCES ● Brain's Diseases of the Nervous System-Book by Russell Brain ● UMPHRED’S NEUROLOGICAL REHABILITATION ● Wilson Disease Association- www.wilsons disease.org ● A multidisciplinary approach to the diagnosis and management of Wilson disease: 2022 practice guidance on Wilson disease
Editor's Notes
- #3: Inability to excrete copper into bile leads to accumulation in liver and brain Common to all forms of Wilson disease that involve brain structures are difficulty in speaking and swallowing, incoordination, and personality changes. The personality changes are the first signs of the disease, especially emotional lability and impaired judgment
- #4: WD is increasingly diagnosed in children who are less than5 years- old. Clinical findings may be nonspecific in children who are less than 2 years- old.[16–22] More severe liver disease, including cirrhosis in a 3-year- old acute liver failure (ALF) in a 5-year- old,[24] was infrequently reported. WD was also confirmed by molecular genetic studies in patients in their early 70s and80s
- #5: Wilson's disease is a classic example of an autosomal recessive disorder. If both parents carry a mutated ATP7B gene, their child has a chance of inheriting the condition, depending on the combination of genes they receive
- #8: Ceruloplasmin is concomitantly reduced. The increase in tissue copper may interfere with various enzyme systems of particular cells. The connection of copper with metabolism may account for the basal ganglia involvement
- #11: NEUROLOGICAL – 50% Hepatic-40% Psychatric -10%
- #13: Evaluation of the extrapyramidal system should include observation for posturing of the extremities or torso (i.e., dystonia), irregular dance- like movements (chorea), determination of tone (parkinsonism and dystonia), and evidence of tremor at rest,with posture or action, or as a rubral wing- beating tremor. Dysautonomia” is the general term for disorders that disrupt your autonomic nervous system (ANS). It can describe several disorders, each with varying symptoms. This may affect the functioning of the heart, bladder, intestines, sweat glands, pupils, and blood vessels. Pseudobulbar palsy is a medical condition characterized by the inability to control facial movements (such as chewing and speaking) and caused by a variety of neurological disorders. The pyramidal system is primarily evaluated by checking reflexes and tone (hyperreflexia andspasticity). Cerebellar function is typically evaluatedby having the patient perform finger to nose andheel/knee/shin testing
- #19: Risus sardonicus or rictus grin is a highly characteristic, abnormal, sustained spasm of the facial muscles that appears to produce grinning
- #20: . The third group of neurological cases are those with a cerebellar (pseudosclerotic) presentation in which there is gait ataxia, dysarthria, loss of limb co-ordination, and titubation of the head. There are usually additional extrapyramidal signs.
- #25: The Kayser–Fleischer ring is a dark ring in the periphery of the cornea, the anterior portion of the outermost layer of the eye, which does not interfere with visual function and consists of corneal granular pigment copper deposits, which infiltrate from the aqueous humor.
- #28: D-penicillamine and Trien-tine [2], while zinc salts act as metallothinoin inducers and contribute to the negative balance of copper, reducing free copper in plasma, and improving symptoms
- #29: blood and urine tests show low levels of ceruloplasmin (plasma protein that carries copper to the blood) and high levels of urinary copper, increased transaminases, coagulation disorders, and hypoglycemia