Afb staning
- 2. For Smear preparation Sputum container of 50 ml capacity to collect sputum Wire loop with an inner diameter of 3mm or applicator stick to spread sputum on the slide New glass slide (no grease and no scratches on the slide) Diamond marker/ marking pencil to enter identification number on the slide Forceps to hold slide with smear Bunsen burner or spirit lamp to sterilize wire loop, fix smeared slide and flame the same during staining Metal waste bin/can with disinfectant to discard infected material Alcohol-sand flask to remove and disinfect excess sputum on the wire loop
- 3. Wire loop New glass slide Sputum container Forceps Alcohol spirit lamp
- 4. Balance Staining rack to hold smeared slides to stain 1% Carbol fuchsin to stain acid-fast bacilli 25% Sulphuric acid to decolorize stained smears 0.1% Methylene blue to counter stain decolorized material in the smear Water to rinse/ wash the staining solution Slide rack to place stained slides to air dry
- 5. Carbol fuchsin Sulphuric acid Methylene blue
- 6. Microscope Immersion oil for 100X objective Tissue paper to absorb immersion oil on stained slides before storing. Slide box to store stained slides for quality assurance (Blinded rechecking) 70% ethanol to clean lenses (frequent use is not recommended) Clean, dry lens tissue to clean microscope lenses
- 8. TB laboratory register Laboratory Request/Report form Red pen to write positive result
- 9. Three specimens should be collected for the laboratory diagnosis of tuberculosis as follows: One spot specimen when the patient first visits the health facility One early morning specimen (preferably the next day) One spot specimen when the early morning specimen is being submitted for examination
- 10. An essential prerequisite for the safe collection and transport of satisfactory specimens is the use of a proper container. The following specifications are recommended to facilitate the choice of a proper container for sputum specimen collection: Wide-mouthed so that patient can expectorate easily inside the container without contaminating the outside Approximately 50 ml in capacity Made of transparent material to ease observation of specimen volume and quality without opening the container Screw-capped to obtain a water tight seal & to reduce the risk of leakage during transport Easily labeled to allow permanent identification Rigid, to avoid breakage during transit
- 11. The patient is given a container on his first visit to health facility. He/she should be instructed, with demonstration by actual actions, to Inhale deeply 2- 3 times Cough out deep from the chest during exhalation Open the container and spit the sputum into the container Avoid saliva or nasal secretions Close the container Instruct the patient to collect an early morning specimen in a similar manner and bring it to the laboratory. On the second attendance, a third specimen (spot) is collected
- 12. Physical appearance of sputum sample should be thick, purulent or and/or bloodstained. Sufficient quantity of at least 3-5 ml. Contains no food particles or other remnants
- 13. Label a new clean, unscratched slide at one end with the laboratory serial number. Label frosted slides with pencil and non-frosted slides with diamond pencil.
- 14. Use muco-purulent, opaque, grayish or yellowish portion for smear preparation. Transfer an appropriate portion of the specimen to the slide by using an applicator stick or wire
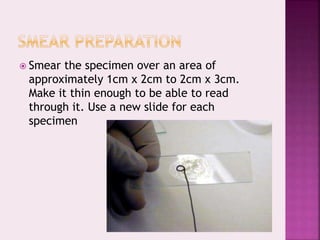
- 15. Smear the specimen over an area of approximately 1cm x 2cm to 2cm x 3cm. Make it thin enough to be able to read through it. Use a new slide for each specimen
- 16. Allow smears to air-dry for 15 minutes. Do not use heat for drying.
- 17. Pass slide through a flame three or four times with the smear uppermost. Do not overheat. Allow to cool before staining.
- 18. Discard the applicator stick in disinfectant and use a new one for each specimen. Remove particles of adherent sputum from wire loop by moving it up and down through a sand alcohol bottle containing 70% alcohol. Flame wire loop thoroughly prior to re-use.
- 19. AFB resists decolourization by weak acid and retains the primary stain. The counter stain is used to stain other materials and the background which gives a contrast background for the easy visibility of the Acid Fast Bacilli. After the smear is stained with Ziehl Neelsen technique, AFB appears red against a blue background.
- 20. 1. Place the numbered slides on a staining rack with the smeared side facing up (individual or in batch of maximum 12 slides). Ensure to leave a finger thickness gap between slides to prevent the transfer of material from one smear to another and the solution running off from slides.
- 21. 2. Flood the entire surface of slide with Ziehl-Neelsen 1% Carbol fuchsin solution
- 22. 3. Heat each slide slowly until steam arises. Maintain steaming for 5 minutes by using intermittent heat. (In no case must the stain solution boil or dry during staining process.)
- 23. 4. Rinse each slide individually in a gentle flow of water until all free stain is washed away. Drain off excess rinse water by tilting the slide.
- 24. 5. Flood the slide with the decolorizing solution (25% Sulphuric acid) for 3 minutes. (If the slide is under decolorized after 3 minutes, further decolorize for 1 minute.)
- 25. 6. Rinse the slide thoroughly with water. Drain off excess water from the slide
- 26. 7. Wipe off back of slide with cotton soaked in decolorizer to clean the dried stains.
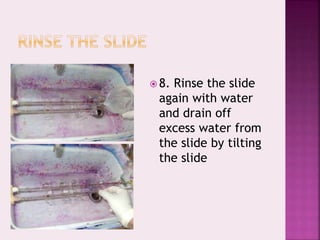
- 27. 8. Rinse the slide again with water and drain off excess water from the slide by tilting the slide
- 28. Flood the slide with 0.1% Methylene blue and counter-stain for 60 seconds
- 29. Rinse the slide thoroughly with water and drain off any excess stain from the slide by placing the slide under gentle stream of running water
- 30. Stand the rinsed slide on the slide holding block and allow the smear to air dry. (Do not heat or use blotting paper to dry the smear. Do not place the slide under direct sunlight to dry the smear.)
- 31. To obtain excellence in smear examination, a good microscope and a comfortable work area are required. Reading of smears must be systematic and standardized to ensure that a representative area of the smear is examined. To ensure that an area is covered only once, the smear should be examined in an orderly manner and the following procedure is recommended:
- 32. Focus the stained slide under low power objective lens (5x or 10x) and, observe the staining quality and evenness of smear. Select the field where the smear is evenly distributed and WBCs & mucus can be seen.
- 33. Apply a drop of immersion oil on the stained smear and focus the smear using 100x objective lens. Do not touch the smear with the dropper. Doing so may contaminate the applicator whereby may spread AFB from one slide to the next resulting in false- positive results.
- 34. Always examine ZN-stained smears with a 100x objective lens under oil immersion.
- 35. Include a known positive slide and a known negative slide each day. The positive control ensures the staining capability of the solutions and of the staining procedure. The negative control confirms that acid-fast contaminants are not present in the stains or other solutions. Make a series of systematic examination over the length of the smear. After examining a microscopic field, move the slide longitudinally so that the neighboring field to the right can be examined. Search each field thoroughly
- 36. Examine a minimum of 100 fields before the smear is reported as negative. For skilled microscopists this will take approximately five minutes. In a smear of 2.0 cm x 1.0 cm size, the number of microscopic fields in one length of the slide corresponds to around 100. If the smear is moderately or heavily positive, fewer fields may be examined and a report of “positive” may be made even though the entire smear has not been examined. Before examining the next slide, wipe the immersion lens with a piece of lens tissue.
- 37. Unexpected objects may be seen when using the microscope. If these objects move only when the slide is moved, they may be materials occasionally found in the specimen or object, precipitated stains, contaminants from the stains or contaminants in the immersion oil. Artifacts that move only when the eyepiece is rotated are in the eyepiece or on its lenses. Artifacts may also be caused by material on the condenser, lenses, mirror or light source. Keep all the slides for quality control according to established procedures
- 40. No of acid-fast bacilli Fields Report No AFB In 100 immersion fields Negative 1-9 AFB In 100 immersion fields Positive scanty Record exact figure 10 to 99 AFB In 100 immersion fields 1+ 1 to 10 AFB Per field (examine 50 fields 2+ More than 10 AFB Per field (examine 50 fields 3+
- 41. Connected with the specimen Inadequate specimen volume and/or poor quality. Carelessness in marking the container. Marking should be done on the body of the container and not on its lid.
- 42. Insufficient or poorly lit work surface. Mixing-up of slides. Preparing too many slides at once. A maximum of 12 is recommended per batch. Re-use of slides that had been positive earlier. These should be discarded. Specimen contamination due to careless use of loops/wooden applicators.
- 43. Using scratched slides on which deposits of stain may look like bacilli. Using unfiltered fuchsin, which may contain crystals. Carelessness in heating the fuchsin, allowing it to dry and crystallize on the smear. Inadequate decolorizing of the smear, which may leave red stain on saprophytic bacilli which then appear to be acid-fast.
- 44. Failure to check the slides and renumber them, if the number is obscured during staining. This may lead to substitutions. Failure to clean the immersion lens with lens tissue after each examination, especially after a smear was found to be positive. Carry-over of bacilli from a positive smear due to immersion oil dropper touching the smear. The oil drop should be allowed to fall without any contact between the dropper and slide. Erroneous recording of the results.
- 45. Problem Possible causes Solution The field is dim Condenser may be too low Condenser iris may be closed Raise the condenser. Open the diaphragm Dark shadows in the field which move when eye piece is moved Eyepiece may be dirty. Eyepiece or objective may be contaminated with fungi. Surface of eyepiece may be scratched. Clean the eye piece Eye piece or objective may need cleaning A new eye piece may be needed The image is not clear The smeared portion of the slide may be upside down There may be an air bubble in the oil The oil may be of poor quality There may be dirt on the lens Turn the slide over Move the 100x lens from side to side Use only good quality immersion oil. Clean the lens The image through low power is not clear There may be oil on the lens There may be dust on the upper surface of the lens The lens may be broken Clean the lens Clean the lens A new lens may be needed
- 46. ‘‘NEVER TRUNED BEHIND BE SUCCESS IN YOUR LIFE’’ Thank you