Bedside monitoring of tissue perfusion and oxygenation
- 1. BEDSIDE MONITORING OF TISSUE PERFUSION AND OXYGENATION Dr.Tushar Patil MD
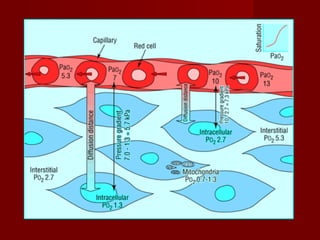
- 3. Oxygen transport involves a series of convective and diffusive processes. Convective transport -bulk movement of oxygen in air or blood -active, energy consuming processes generating flow Diffusive transport - passive movement of oxygen down its concentration gradient across tissue barriers - across the extracellular matrix - depends on the oxygen tension gradient and the diffusion distance
- 6. Capillary blood to individual cells resting extraction ratio from capillary blood is about 25% may increase to 7080% during exercise Factors affecting O2 extraction from cappilary blood 1. Rate of O2 delivery to capillary 2. O2-Hb dissociation relation 3. Size of capillary to cellular PO2 relation 4. Diffusion distance to cells 5. Rate of use of O2 by cells
- 8. Tolerance to hypoxia of various tissues Tissue Survival time 1. Brain<3 min 2. Kidney and liver15-20 min 3. Skeletal muscle60-90 min 4. Vascular smooth muscle24-72 h 5. Hair and nails -Several days
- 9. Tissue Hypoxia in Critically Ill disordered regional distribution of blood Regional and microcirculatory distribution of cardiac output endothelial, receptor, neural, metabolic, and pharmacological factors small resistance arterioles and precapillary sphincters shunting and tissue hypoxia despite high global oxygen delivery and mixed venous saturation. reduce regional distribution, particularly to the renal and splanchnic capillary beds
- 11. EFFECTS OF HYPOXIA PaO2 level approaches 55mmHg-.short term memory loss, euphoria and impaired judgment PaO2 30-50mmHg -Progressive loss of cognitive and motor functions, increasing tachycardia PaO2 below 30mmHg-loss of consciousness
- 12. Clinical features of tissue hypoxia Dyspnoea Altered mental state Tachypnoea or hypoventilation Arrhythmias Peripheral vasodilatation Systemic hypotension Coma Cyanosis (unreliable) Nausea, vomiting, and gastrointestinal disturbance
- 13. Monitoring Tissue Perfusion and Oxygenation 1. Clinical Evaluation 2. Hemodynamic Monitoring 3. Pulse Oximetry 4. End Tidal CO2 Monitoring 5. Monitoring Tissue Hypoxia 6. Cerebral Oxygenation Monitoring
- 14. Clinical Evaluation HISTORY -Dyspnoea -Cough -Fever -Rash -Discolouration of digits/limbs -Palpitations -Altered sensorium -Convulsions
- 15. Clinical Evaluation Level of Consciousness Evaluation of Peripheral & Central Pulses Capillary Refill Time Cyanosis Respiratory Rate & Pattern Blood Pressure Systemic Examination
- 16. Hemodynamic Monitoring Arterial Blood Pressure -Non Invasive -Invasive Central Venous Pressure Monitoring Pulmonary Artery Catheterisation Measuring Cardiac Output
- 17. Monitoring arterial pressure Organ perfusion depends on the organ metabolic demand ,perfusion pressure,local vasomotor tone and cardiac output tissue perfusion is maintained through ‘‘autoregulation’’ Organ perfusion pressure cannot be measured directly at the bedside As a surrogate for tissue perfusion pressure, arterial blood pressure is monitored.
- 19. Noninvasive measurements of arterial pressure can be determined either manually or by oscillometric method . Oscillometric devices, determine MAP and then provide readings for systolic and diastolic pressures. Oscillometric devices tend to underestimate systolic and overestimate diastolic blood pressure noninvasive measurements less reliable with marked hypovolemia or abnormal cardiac function. Oscillometric measurements also limited by cycling delay of the device.
- 20. Arterial Catheterisation INDICATIONS ABSOLUTE- As a guide to synchronization of intra-aortic balloon counter pulsation PROBABLE- 1. Guide to management of potent vasodilator drug infusions 2. Guide to management of potent vasopressor drug infusion 3. As a port for the rapid and repetitive sampling 4. As a monitor of cardiovascular deterioration in patients
- 22. Arterial Catheterisation USEFUL APPLICATIONS Differentiating cardiac tamponade (pulsus paradoxus) from respiration-induced swings in systolic BP Differentiating hypovolemia from cardiac dysfunction as the cause of hemodynamic
- 23. Arterial Catherisation COMPLICATIONS - temporary occlusion - hematomas - Serious ischemic damage - sepsis - pseudoaneurysm
- 24. Central venous pressure monitoring Pressure in the large central veins proximal to the right atrium relative to atmosphere. METHODS - central venous line / Swan-Ganz catheter with distal tip connected to manometer/ pressure transducer - noninvasively as jugular venous pressure
- 25. Factors affecting measured CVP 1.Central venous blood volume Venous return/cardiac output Total blood volume Regional vascular tone 2.Compliance of central compartment Vascular tone RV compliance Myocardial disease Pericardial disease Tamponade 3.Tricuspid valve disease Stenosis Regurgitation
- 26. Factors affecting measured CVP 4.Cardiac rhythm Junctional rhythm Atrial fibrillation (AF) Atrio ventricular (A-V) dissociation 5.Reference level of transducer Positioning of patient 6.Intrathoracic pressure Respiration IPPV Positive end-expiratory pressure (PEEP) Tension pneumothorax
- 27. Limitations of CVP Being wrongly used as a parameter/ goal for replacement of intravascular volume The validity as index of RV preload nonexistent Poor correlation with cardiac index, stroke volume, left ventricular end-diastolic volume, and right ventricular end-diastolic volume
- 28. Pulmonary artery catheterization Developed in the 1940s and later refined by Swan and Ganz in 1970 INDICATIONS Diagnostic – Diagnosis of shock states – high- versus low-pressure pulmonary edema – primary pulmonary hypertension (PPH) – valvular disease, intracardiac shunts, cardiac tamponade, and pulmonary embolus (PE) – Monitoring complicated AMI – hemodynamic instability after cardiac surgery Therapeutic - Aspiration of air emboli
- 30. PAC CONTRAINDICATIONS Tricuspid or pulmonary valve mechanical prosthesis Right heart mass (thrombus and/or tumor) Tricuspid or pulmonary valve endocarditis
- 31. PAC MEASURED PARAMETERS 1. Central Venous Pressure 2. Pulmonary Capillary Wedge Pressure 3. Cardiac Index 4. Stroke Volume Index 5. LV Stroke Work Index 6. RVSWI 7. RV Ejection Fraction 8. RV End Diastolic Volume 9. Systemic Vascular Resistance Index 10. Pulmonary Vascular Resistance Index 11. Mixed Venous O2 Saturation 12. O2 delivery 13. O2 uptake 14. O2 exraction Ratio
- 32. Complications of PAC Venous access complications - include arterial puncture - hemothorax - Pneumothorax Arrhythmias - PVCs or nonsustained VT - Significant VT or ventricular fibrillation Right bundle-branch block (RBBB) PA rupture PAC related infection Pulmonary infarction
- 33. Measuring Cardiac Output 1. Pulmonary Artery Catheter 2. Pulse Contour Analysis -Lithium dilution -Transpulmonary Thermodilution -Without diluion calibration 3. CO2 Rebreathing 4. Trans thoracic Electrial Bioimpedence 5. Trans Thoracic Echo 6. Esophageal Doppler Monitoring
- 34. Pulse Oximetry PRINCIPLE Displayed readings determined primarily by two components: 1. The different absorption spectra of oxyhemoglobin and deoxyhemoglobin at different wavelengths 2. Pulsatile arterial blood Probe (finger, ear, or forehead) contains two light- emitting diodes that emit light at 660 nm and 940 nm. Photoreceptor receives light, and compares absorption two wavelengths,
- 36. Pulse Oximetry APPLICATIONS indicated in circumstance where hypoxaemia May occur. should be included in the routine vital signs. . continuous monitoring. pattern of oxygenation can be recorded. can replace arterial blood gas analysis in cases where assessment of oxygenation is indication. Regulation of oxygen therapy Testing adequecy of circulation
- 37. Pulse Oximetry Improving oximeter signals • Warm and rub the skin • Apply a topical vasodilator • Try a different probe site, especially the ear • Try a different probe • Avoid motion artefact • Use a different machine
- 39. Pulse Oximetry PITFALLS 1. Dyshemoglobinemias 2. Poor function wiyh poor performance 3. Difficulty in detecting high oxygen partial pressures 4. Delayed detection of hypoxic events 5. Erratic performance with irregular rhythms 6. Nail polish and coverings 7. Loss of accuracy at low values 8. Electrical interference 9. Failure to detect hypoventilation
- 40. Monitoring ventilation using end- tidal carbon dioxide provides information regarding alveolar ventilation. PetCO2 - concentration of carbon dioxide at end expiration . measured in both mechanically ventilated and spontaneously breathing patients. displayed as either numerical value (capnometry) or as a graphic waveform plotted against time (capnography). PetCO2 underestimatesPaCO2 by 2 to 5 mm Hg because of the influence of dead space ventilation relationship between PetCO2 and PaCO2 is unreliable in critically ill patients.
- 42. End Tidal Carbon Dioxide APPLICATIONS Confirming endotracheal tube placement detecting endotracheal tube dislodgment detecting ventilator malfunction assessing the success of cardiopulmonary resuscitation evaluation of weaning from mechanical ventilation determining the optimal level of PEEP
- 43. End Tidal CO2 sudden loss of the capnogram waveform –ET obstruction -extubation - ventilator malfunction –cardiac arrest sudden drop of the waveform -partial obstruction of ET -an airway leak -hypotension
- 44. End Tidal CO2 Capnography can be used to monitor patients in whom hypercarbia may be detrimental PetCO2 values greater than 40 mm Hg correlate with equal or higher value of PaCO2 Elevated PetCo2 indicate sthe need for alterations in management
- 45. Monitoring Tissue Hypoxia Global markers of tissue hypoxia - serum lactate -central venous oxygen saturation (ScvO2) Monitoring regional hypoxia -Sublingual Capnometry –Gastric Tonometry - Orthogonal Polarization Spectroscopy (OPS) - Near Infra Red Spectroscopy (NIRS) -Trans cutaneous Oxygen Tension -Resonance Raman Spectroscopy
- 46. Serum Lactate byproduct of anaerobic metabolism, resulting from the inabilityof pyruvate to enter the Krebs cycle. The normal serum value - less than 2 mmol/L. lactate levels above 4mmol/L strongly associated with worse outcome. more important is the time to normalization of lactateLevels- ‘‘lactate clearance time.’’ Prolonged lactate clearance time(>48hrs)-significantly higher rates of infection, organ dysfunction, and death Better survival correlates with a lactate clearance time <24 hrs.
- 47. Central venous oxygen saturation Mixed venous oxygen saturation (SvO2) - a measure of tissue hypoxia. o Obtained with pulmonary artery catheter. FACTORS INFLUENCING SvO2 - arterial oxygen saturation - hemoglobin concentration - cardiac output - tissue oxygen consumption. - NORMAL VALUES- 70% to 75%. - Values below 60% indicate cellular oxidative impairment - values below50% associated with anaerobic metabolism pulmonary artery catheters not placed routinely ScvO2 - surrogate For SvO2
- 49. ScvO2 venous oxygen saturation near the junction of the superior vena cava and right atrium. obtained from subclavian or internal jugular central venous catheter. Because ScvO2 neglects venous return from the lower body, values for ScvO2 typically are 3% to 5% less than SvO2 values < 65% -ongoing oxidative impairment. values > 80% - cellular dysfunction with impaired oxygen consumption. - seen in late stages of shock To be used in context with other markers of tissue perfusion (eg, lactate).
- 50. Sublingual capnometry studies perfusion of the splanchnic circulation. sensor placed under the tongue measures partial pressure of carbon dioxide in the sublingual tissue (PslCO2). Normal values for PslCO2 - 43 to 47 mmHg PslCO2 >70 mm Hg - correlates with elevated arterial lactate levels more important is the ‘‘PslCO2 gap.’’- difference between PslCO2 and PaCO2 A PslCO2 gap of> 25 mm Hg identifies patients at a high risk of mortality.
- 51. Gastric Tonometry Offers an index of aerobic metabolism in gut mucosa. Based on increase in tissue CO2 A balloon in stomach,measures intramucosal pCO2 Using this and arterial (HCO3), gastric intramucosal PH is calculated
- 53. Orthogonal polarization spectroscopy uses polarized light to visualize the microcirculation directly. hemoglobin absorbs polarized light real-time images reflected to videomicroscope functional capillary density measured. sensitive marker of tissue perfusion and an indirect measurement of oxygen delivery. Tissues evaluated- oral mucosa, sublingual mucosa, rectal mucosa,and vaginal mucosa. LIMITNG FACTORS- -movement artifacts -presence of saliva -observer related bias
- 56. Near-infrared spectroscopy measures the concentrations of hemoglobin, oxygen saturation, and cytochrome aa3 Cytochrome aa3- final receptor in the electron transport chain - responsible for 90% cellular O2 consumption - remains in a reduced state during hypoxia used primarily to evaluate the perfusion of skeletal muscles. PROBLEMS -signal contamination by light scatter -variable interpretations of the data -lack of a reference standard for comparison
- 59. Transcutaneous oxygen tension measure transcutaneous oxygen or carbon dioxide. Use heated probes placed on the skin •markers of regional tissue hypoperfusion increased mortality in patients with low transcutaneous oxygen or high CO2 •LIMITATIONS -Tissue trauma from probe insertion, - thermal injury if probes are not moved every4 hours - lack of established critical values to guide resuscitation .
- 61. Cerebral Perfusion and Oxygenation monitoring 1. Jugular venous bulb oximetry 2. Direct brain tissue oxygen tension 3. Near inrared spectroscopy 4. Cerebral Microdialysis 5. Cerebral Blood Flow Monitoring 6. Oxygen-15 PET
- 62. Jugular venous oxygen saturation(SjvO2) Retrograde placement of jugular venous catheter with oximeter cannulate dominant IJV catheter tip positioned in jugular bulb compatible with MRI. SjvO2 - result of the difference between cerebral oxygen delivery (supply) and cerebral metabolic rate of oxygen (demand) Low SjvO2 (!50% for O10 minutes) -hypoperfusion / increased . cerebral metabolism. APPLICATIONS - comatose patients (GCS <8) -treatment of SAH - - neurosurgical procedures
- 64. SjvO2 LIMITATIONS - changes in arterial oxygen content - hemodilution - prone position of catheter - necessity for frequent calibrations - infection - increase in ICP - thrombosis - arterial Puncture - pneumothorax - reflects global cerebral oxygenation and does not detect regional ischemia in smaller regions ipsilateral or in contralateral hemisphere
- 65. Brain tissue oxygen pressure(PBO2) Small flexible microcatheter inserted into brain parenchyma. marker of the balance between regional oxygen supply and use. ICP, brain temperature (Licox, Integra Neurosciences) or tissue partial pressure of carbon dioxide (PBCO2) and pH (Neurotrend, Johnson & Johnson) can be monitored Licox device uses polarographic technique by Clark electrode Neurotrend uses ‘‘optimal luminescence’’ catheter should pass through gray matter into white matter tunneled after craniotomy or placed through a double or triple lumen bolt measured tissue volume 17 mm3. PBO2 levels highest in dense population of neurons and lower in white matter PBO2 and amplitude of changes lower with Neurotrend than Licox compatible with MRI
- 69. Near infrared spectroscopy monitoring of transmittance across the brain at two or more wavelengths optical attenuation of the spectra converted into changes of cerebral oxygenation methods include time-resolved, spatially resolved, and phase-resolved spectroscopy INVOS system provides a numerical value for oxygen saturation using rSO2 normal range-60-80% NIRO oximeters present values for oxygenated and total Hb concentration, cytochrome aa3, and a tissue oxyge index
- 71. NIS APPLICATIONS detection of changes during carotid cross-clamping during carotid endarterectomy & cardiac surgery to detect cerebral vasospasm causing delayed cerebral ischemic deficit after SAH assessment of perfusion reductions in stroke Reconstruction of a three-dimensional image using optical tomography attractive because applied by attaching pads to the forehead or other regions of interest.
- 73. NIS LIMITATIONS limited and variable penetration of infrared light through the skull (2–3 mm, limited to gray matter) contamination by extra- and intracranial sources (mixture of capillary, venous,and arterial blood), and uniform distribution of infrared light in the CSF layer. degree of scatter unpredictable inconsistent impact of monitoring of decreased oxygenation on neurologic outcome
- 75. Cerebral Microdialysis bedside monitor to provide on-line analysis of brain tissue biochemistry during neurointensive care. The principles and clinical double-lumen probe, lined at it tip with dialysis membrane. perfused by an inlet tube with fluid isotonic to the tissue interstitium perfusate passes along the membrane before exiting collecting chamber. catheter acts as an artificial blood capillary. Measures microdialysate concentrations of glucose, lactate, pyruvate, glycerol, and glutamateThe concentration of these substances in the microdialysate does not correspond to their true extracellular fluid concentration proportion of the extracellular fluid concentration the ‘‘relative recovery”
- 77. MD data display Brain Tissue O2 monitor MD Bedside Analyser Jugular Venous Saturation Monitor
- 78. Applications of MD Most clinical experience with TBI and SAH Severe cerebral hypoxia /ischemia associated with marked increases in the lactate-pyruvate ratio Ratio greater than 20 to 25 associated with poor outcome Glycerol is a marker of ischemic cell damage Increased MD glycerol concentrations associated with poor outcome Increased excitatory amino acids and reduced brain ECF glucose associated with metabolic catastrophes after acute brain injury.
- 79. Cerebral Blood Flow Monitoring Kety-Schmidt method Radioactive tracer techniques Continuous quantitative cerebral blood flow monitoring -Laser Doppler flowmetry -Thermal diffusion flowmetry Double-indicator dilution technique Transcranial Doppler ultrasonography
- 81. Neuroimagong [18F]2-deoxy-D-glucose PET oxygen-15 PET SPECT Xenon-enhanced CT scanning perfusion CT Perfusion weighted imaging (PWI)
- 82. THANKS
















































































![Neuroimagong
[18F]2-deoxy-D-glucose PET
oxygen-15 PET
SPECT
Xenon-enhanced CT scanning
perfusion CT
Perfusion weighted imaging (PWI)](https://image.slidesharecdn.com/bedsidemonitoringoftissueperfusionandoxygenation-121005110829-phpapp02/85/Bedside-monitoring-of-tissue-perfusion-and-oxygenation-81-320.jpg)
