Biochemical investigations and management of sickle cell nephropathy.pptx
- 1. By Dr Auwal Ahmad Department of Haematology Moderated by Dr J. M. El Bashir 1/29/2024 Biochemical Investigation and Management of Sickle Cell Nephropathy 1
- 2. Outline Introduction Epidemiology Pathophysiology Clinical features Investigations Management Conclusion References 1/29/2024 2
- 3. Introduction Sickle cell disorder is an autosomal recessive disorder caused by a point mutation leading to replacement of glutamic acid for valine at the sixth amino acid of beta-globin In this disorder, RBCs become sickled when exposed to conditions of low oxygen tension Polymerization of deoxygenated haemoglobin Red cell distortion, haemolytic anaemia, micro- vascular obstruction, and ischaemic tissue damage 1/29/2024 3
- 4. Introduction In Sickle cell disease (SCD), there is inheritance of HbS • Homozygous state (HbSS) referred to as Sickle cell anaemia • Heterozygous state Normal: eg HbA (HbAS) is the sickle cell trait Compound: HbC, HbD and HbE refered to as SCD The hallmark of SCD is haemolysis, widespread vaso-occlusion, ischaemia reperfusion injury and subsequent multi-organ damage 1/29/2024 4
- 5. Introduction Sickle cell disorders may lead to a variety of alterations in renal morphology and function leading to clinically significant abnormalities collectively known as Sickle cell nephropathy. These are: • Proteinuria • Hyposthenuria • Renal Papillary necrosis and Haematuria • Sickle cell glomerulopathy • Renal Tubular Disorders Significant renal involvement occurs more frequently in SCD than in sickle cell trait 1/29/2024 5
- 6. Epidemiology SCD is prevalent in malaria-endemic regions due to protective carrier state Increasing occurrence in non-endemic regions due to population movements About 24% in adult Nigerians and about 8% in African-Americans ----WHO 59th WHA Renal complications as significant cause of morbidity and mortality Incidence of renal failure rising with improved patient survival -------Aeddula NR et al island 2022 1/29/2024 6
- 7. Epidemiology Renal involvement occurs in ~60% of patients with SCD only 4-12% will develop end-stage renal disease (ESRD) (Powers et al 2005) SCN accounts for <1% of all new cases of ESRD ( US) Proteinuria is common in SCD occurring in about 30% of patients 16-18% of mortality in SCD is ascribed to kidney disease 1/29/2024 7
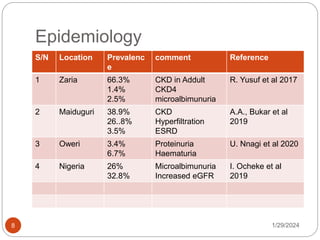
- 8. Epidemiology 1/29/2024 8 S/N Location Prevalenc e comment Reference 1 Zaria 66.3% 1.4% 2.5% CKD in Addult CKD4 microalbimunuria R. Yusuf et al 2017 2 Maiduguri 38.9% 26..8% 3.5% CKD Hyperfiltration ESRD A.A., Bukar et al 2019 3 Oweri 3.4% 6.7% Proteinuria Haematuria U. Nnagi et al 2020 4 Nigeria 26% 32.8% Microalbimunuria Increased eGFR I. Ocheke et al 2019
- 9. Epidemiology---Risk Factors risk factors associated with progression of chronic kidney disease (CKD) in SCN Genetic variants of MYH9 and APOL1 Infection with parvovirus B19 Recurrent Acute chest syndrome Vaso occlusive episodes Nephrotic range proteinuria Underlying hypertension Severe anemia Genetic modifiers may affect renal dysfunction 1/29/2024 9
- 10. Risk Factors Genetic Modifiers and Renal Dysfunction Renal dysfunction more severe in HbSS and HbSb0 thalassaemia genotypes (SCA) Lower HbF levels correlate with renal failure risk and vaso-occlusive complications Co-inheritance of α-thalassaemia reduces HbS concentration, red cell volume, and haemolysis 1/29/2024 10
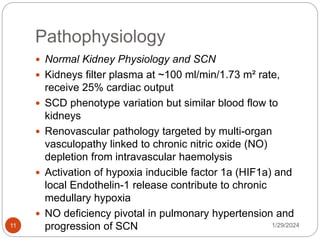
- 11. Pathophysiology Normal Kidney Physiology and SCN Kidneys filter plasma at ~100 ml/min/1.73 m² rate, receive 25% cardiac output SCD phenotype variation but similar blood flow to kidneys Renovascular pathology targeted by multi-organ vasculopathy linked to chronic nitric oxide (NO) depletion from intravascular haemolysis Activation of hypoxia inducible factor 1a (HIF1a) and local Endothelin-1 release contribute to chronic medullary hypoxia NO deficiency pivotal in pulmonary hypertension and progression of SCN 1/29/2024 11
- 14. Renal manifestations of sickle cell disease 1/29/2024 14 Alterations in renal haemodynamics Increased renal blood flow rate Increased renal plasma flow rate Increased glomerular filtration rate Decreased renal vascular resistance Decreased filtration fraction Decreased medullary perfusion Renal and glomerular enlargement Hyperfunction of the proximal tubule Increased reabsorption of phosphate and β2- microglobulin Increased secretion of creatinine and uric acid
- 15. Renal manifestations of sickle cell disease 1/29/2024 15 Glomerulopathies Focal segmental glomerulosclerosis Membranoproliferative glomerulonephritis Thrombotic microangiopathy Tubular deposits of iron Chronic tubulointerstitial disease Impaired function of the distal nephron Decreased urinary concentrating ability Partial distal renal tubular acidosis Impaired renal potassium excretion
- 16. Renal manifestations of sickle cell disease 1/29/2024 16 Increased susceptibility to acute kidney injury Chronic kidney disease and its progression to end- stage renal disease Haematuria Renal papillary necrosis Increased susceptibility to urinary tract infections Renal medullary carcinoma
- 18. Clinical Features 1/29/2024 18 Asymptomatic Diminished concentrating ability (hyposthenuria) Present with thirst, nocturia and polyuria Dehydration leading to acute vaso-occlusive crises Sickling in the vasa rectae interferes with countercurrent exchange in the inner medulla Hematuria – Painless microscopic or gross hematuria – Due to papillary infarcts, microthrombosis in peritubular capillaries, infections, or transfusion reaction Renal infarction & papillary necrosis Nausea, vomiting, flank or abdominal pain, fever Hypertension (renin-mediated) Renal tubular acidosis – Diminished medullary blood flow and hypoxia -> Impaired distal H and K secretion -> incomplete dRTA
- 19. Clinical Features 1/29/2024 19 Abnormal proximal tubular function (Supranormal) – Hyperphosphatemia <- increased phosphate reabsorption – Elevated creatinine clearance (due to enhanced creatinine secretion) in relation to the true glomerular filtration rate (GFR) Acute kidney injury Impaired concentrating ability -> dehydration -> prerenal AKI Intrinsic renal causes of AKI include rhabdomyolysis, sepsis, drug nephrotoxicity, renal vein thrombosis, and hepatorenal syndrome (hemosiderosis-induced hepatic failure) Postrenal causes include urinary tract obstruction e.g. secondary to blood clots
- 20. Clinical Features 1/29/2024 20 Urinary tract infection – Impaired immunity (autosplenectomy) -> opsonic antibody deficiency - > encapsulated organisms) Can precipitate a sickle cell crisis Nephrotic Syndrome Rare -> poor prognosis MPGN -> FSGS – Direct effect of sickled RBCs Secondary MPGN <- hepatitis C infection (multiple blood transfusions)
- 21. Clinical Features 1/29/2024 21 CKD Symptoms develop slowly and aren't specific to the disease Asymptomatic, nausea and vomiting, fatigue, loss of appetite, malaise, muscle cramps, swellings, dry and itchy skin, breathlessness, insomnia, polyuria or oliguria, high blood pressure Renal medullary carcinoma Rare; ~ 1 in 20,000 • Almost exclusive with sickle cell trait (less commonly, sickle cell disease) Present with gross hematuria, UTI, flank pain, an abdominal mass, and/or weight loss Diagnosis via imaging (CT scan) Highly aggressive malignancy Metastasis at time of diagnosis Poor prognosis
- 22. Investigations 1/29/2024 22 Biochemical and non biochemical Biochemical Urinalysis with microscopy using spot urine, morning urine or 24hr urine collection Assess proteinuria/albuminuria Renal function panel Electrolytes, urea and critinine eGFR calculation using Inulin eGFR Creatinine eGFR Lipid profile Other markers of renal function
- 23. Investigations --- urinalysis 1/29/2024 23 Physical examination describes the volume, color, clarity, odor, and specific gravity. Chemical examination identifies pH, red blood cells, white blood cells, proteins, glucose, urobilinogen, bilirubin, ketone bodies, leukocyte esterase, and nitrites. Microscopic examination encompasses the detection of casts, cells, crystals, and microorganisms. Proteinuria, haematuria, USG, PH
- 24. Investigations --- urinalysis 1/29/2024 24 Proteinuria can my categorized as a glomerular pattern, a tubular pattern, and an overflow pattern Albuminuria According to the Kidney Disease Improving Global Outcomes (KDIGO) guidelines, albuminuria can be classified into three stages uACR/uPCR
- 25. Investigations --- urinalysis 1/29/2024 25 Albuminuria stage Description ACR (mg/mmol creatinine) A1 Normal to mildly increased <3 Reference ranges: women <3.5 mg/mmol; men <2.5 mg/mmol A2 Moderately increased 3-30 Commonly referred to as ‘’micro- albuminuria’’ A3 Example ; G3bA2 denotes GFR 30- 44mL/min & ACR Severely increased >30 Detectable using conventional dipsticks
- 26. Investigations --- urinalysis 1/29/2024 26 Haematuria Dipstick test for blood detects primarily the peroxidase activity of erythrocytes, but myoglobin and hemoglobin can also catalyze this reaction. Thus, a positive test result indicates hematuria, myoglobinuria, or hemoglobinuria.
- 27. Electrolytes, urea and critinine 1/29/2024 27 INCREASED Potassium Urea Creatinine Hydrogen ion Phosphate Magnesium DECREASED Sodium Bicarbonate Calcium
- 29. 1/29/2024 29 CKD Stage GFR (mL/min/1.73m2) Description 1 >90 Normal or increased GFR with other evidence of kidney damage 2 60-89 Mild reduction in GFR, with other evidence of kidney damage 3 30-59 3a 45-59 3b 30-44 Moderately reduced GFR, with or without evidence of kidney injury 4 15-29 Severely reduced GFR 5 <15 End-stage or approaching end-stage kidney failure 5D <15 On dialysis
- 30. Investigations 1/29/2024 30 Can be classified base on the renal structure affected by the pathological process Markers of glomerular damage Transferrin igG Ceruloplasmin Type IV collagen Laminin Glycosaminoglycans Lipocalin type prostaglandin D synthase Fibronectin Podocalyxin VEGF Cystatin C nephrin
- 31. Investigations 1/29/2024 31 Tubular damage markers Neutrophils gelatinase associated lipocalin(NGAL) Alpha-1-microglobulin Kidney injury molecule-1(KIM-1) N-acetyl-beta-D-glucosaminidase Angiotensinogen Uromodulin Liver type fatty-acid binding protein (L-FABP) Heart-type fatty acid binding protein (H-FABP)
- 32. Investigations 1/29/2024 32 Non biochemical Hb electrophoresis Full blood count and Differential Viral serologies Renal ultrasound – Early - > large, variable echogenicity – Shrink with CKD – Papillary necrosis • Increased echogenicity of the inner medulla • In more advanced cases, a filling defect in the area of the medullary tip can be seen
- 33. Management 1/29/2024 33 This can be divided into management of SCD and the management of nephropathy SCD complications such as frequent crisis and anaemia are controlled by; - Blood transfusion - Hydroxyurea (HU) HU may reduce proteinuria and hyperfiltration, better urine concentrating ability and less renal enlargement
- 34. Management 1/29/2024 34 Patients with proteinuria (uACR>50mg/mmol) should be treated Either with an angiotensin converting enzyme inhibitor (ACEI) or an angiotensin receptor blocker (ARB) starting at a low dose When taken at night these drugs also reduce nocturia Treatment of anaemia; the target Hb level should be no greater than 10-10.5g/dL A rise in haematocrit of greater than 1-2% per week should be avoided
- 35. Management 1/29/2024 35 Erthrocyte-stimulating agents (ESA) such as erythropoietin can improve Hb level and reduce transfusion requirement in some patients Though blood transfusion provides higher amount of HbA compared with patients own blood Addition of ESA may allow administration of higher doses of HU and improve foetal Hb
- 36. Management 1/29/2024 36 Haematuria in SCN is typically self-limiting Treatment consists of bed rest and maintenance of high urine flow rate In cases of massive haematuria include; Urine alkalinization to minimize Hb precipitation, loop diuretics to prevent micro- tubular obstruction and blood transfusion to reduce HbS and sickling
- 37. Management 1/29/2024 37 Refractory cases may require high doses of oral urea which has an inhibitory effect on gelation of deoxygenated sickled Hb Treatment with vasopressin or epsilon amino caproic acid to promote clotting Angiographic embolization of renal vessels or balloon tamponade may be considered
- 38. Management 1/29/2024 38 The relatively small size of the SCD-ESRD population has limited the development of optimal management strategies Renal replacement therapy is considered in ESRD The therapeutic options include; 1. Haemodialysis 2. peritoneal dialysis 3. Kidney transplantation
- 39. Conclusion 1/29/2024 39 SCD may lead to a variety of alterations in renal morphology and function, some of which produce clinically significant abnormalities that may be present from the first year of life. The lack of diagnostic test capable of detecting those at risk, and detecting onset of symptoms remains a barrier to instituting therapy. The absence of therapeutic strategy compounds the management of SCN
- 40. 1/29/2024 40 Thank you all for listening
- 41. References 1/29/2024 41 Aeddula NR, Bardhan M, Baradhi KM. Sickle Cell Nephropathy. Ncbi. 2020. Available from https://www.ncbi.nlm.nih.gov . [Date accessed July, 2020] Alpers CE, Chang A. The Kidney. Robbins and Cotran Pathologic Basis of Diseases. Saunders Elsevier. Ninth Edition. Chapter 20. Pg 911-919 Inusa BPD, Mariachiara L, Giovanni P, Ataga KI. Sickle Cell Nephropathy: Current Understanding of the Presentation, Diagnostic and Therapeutic Challenges. Intechopen. 2018. Available from https://www.intechopen.com .[Date accessed July, 2020] Kumar V, Abbas AK, Aster JC. Red Blood Cell and Bleeding Disorders. Robbins and Cotran Pathologic Basis of Diseases. Saunders Elsevier. Ninth Edition. Chapter 14. Pg 635 Marshal WJ, Lapsley M, Day A. The Kidneys. Clinical Chemistry. Elsevier. Eight Edition. Pg 86 Mohan Harsh. The Kidney and Lower Urinary Tract. Textbook of Pathology. Jaypee. Seventh Edition. Chapter 20. Pg 636-638 Pham PT. Renal Manifestations of Sickle Cell Disease. Medscape. 2019. Available from http://emedicine.medscape.com. [Date accessed July, 2020]
- 42. References 1/29/2024 42 Bukar, A. A., Sulaiman, M. M., Ladu, A. I., Abba, A. M., Ahmed, M. K., Marama, G. T., & Abjah, U. M. (2019). Chronic kidney disease amongst sickle cell anaemia patients at the University of Maiduguri Teaching Hospital, Northeastern Nigeria: A study of prevalence and risk factors. Mediterranean Journal of Hematology and Infectious Diseases, 11(1). Yusuf, R., Hassan, A., Ibrahim, I. N., Babadoko, A. A., & Ibinaiye, P. O. (2017). Assessment of kidney function in sickle cell anemia patients in Zaria, Nigeria. Sahel Medical Journal, 20(1), 21. Nnaji, U. M., Ogoke, C. C., Okafor, H. U., & Achigbu, K. I. (2020). Sickle cell nephropathy and associated factors among asymptomatic children with sickle cell anaemia. International Journal of Pediatrics, 2020. Ocheke, I. E., Mohamed, S., Okpe, E. S., Bode-Thomas, F., & McCullouch, M. I. (2019). Microalbuminuria risks and glomerular filtration in children with sickle cell anaemia in Nigeria. Italian journal of pediatrics, 45, 1- 6. BRAIMOH, R. W., Ale, O. K., & Adewunmi, J. A. (2017). Evaluation of urinary tract infection and nephropathy in adult Nigerians with sickle cell anaemia. Tropical Journal of Nephrology, 12(2), 23-30. WHO FIFTY-NINTH WORLD HEALTH ASSEMBLY A59/9 Provisional agenda item 11.4 24 April 2006 Aeddula NR, Bardhan M, Baradhi KM. Sickle Cell Nephropathy. [Updated 2022 Sep 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK526017/
Editor's Notes
- #4: Sickle cell disorder is an autosomal recessive disorder caused by a point mutation causing substitution of thymine for adenine in the sixth codon of the beta globin-chain gene, this causes coding of amino acid valine instead of glutamate in position 6 of the beta-globin chain
- #5: In Sickle cell disease (SCD), there is inheritance of HbS in the homozygous state or with another abnormal Hb (compound heterozygotes) and clinical manifestations
- #7: Claire C. Sharpe, Swee L. Thein, Sickle cell nephropathy – a practical approach British Journal of Haematology September 2011
- #8: Claire C. Sharpe, Swee L. Thein, Sickle cell nephropathy – a practical approach British Journal of Haematology September 2011
- #10: Onset of CKD gradual, requires ongoing monitoring Microalbuminuria: early manifestation, prevalent in older patients Endstage Renal Disease (ESRD): serious complication in a minority
- #13: The pathobiology of sickle cell disease. The formation of deoxyHbS leads to RBC sickling and vascular stasis. Stasis induces vascular occlusion, which either leads to infarction or resolves and causes ischaemia–reperfusion and its accompanying processes. Recurrent cycles of ischaemia–reperfusion in microcirculatory beds amplify organ injury (the ‘big bang’ effect) because they induce inflammation and endothelial dysfunction, both regionally and systemically. Endothelial dysfunction promotes adhesion of RBCs and WBCs to the endothelium. This adhesion is critical because it impedes the transit of RBCs through the microcirculation, thereby promoting RBC sickling and vascular stasis. This vascular stasis explains why RBC sickling occurs in the microcirculation, despite the fact that the time required for sickling usually exceeds RBC transit through the microcirculation. Additional pathobiological pathways include haemolysis and increased free plasma haemoglobin. Plasma haemoglobin scavenges NO from the endothelium. Autoxidation and degradation of HbS lead to the release of free haem, which is toxic to the endothelium via its pro-oxidant and proinflammatory properties. Abbreviations: deoxyHbS, deoxygenated HbS; HbS, sickle haemoglobin; NO, nitric oxide; pO2, partial pressure of oxygen; RBC, red blood cell; WBC, white blood cell. Nath, K., Hebbel, R. Sickle cell disease: renal manifestations and mechanisms. Nat Rev Nephrol 11, 161–171 (2015). https://doi.org/10.1038/nrneph.2015.8
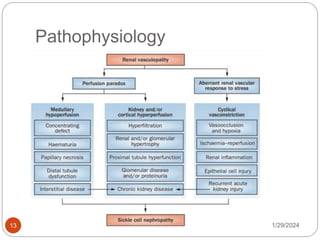
- #14: Salient pathogenetic processes in the development of sickle cell nephropathy. Sickle cell nephropathy largely reflects an underlying functional vasculopathy. This vasculopathy leads to a perfusion paradox, wherein medullary hypoperfusion occurs in conjunction with kidney and/or cortical hyperperfusion. The renal vasculopathy also leads to aberrant renal vascular responses to stress that occur systemically or in distant organs and tissues. This response is characterized by enhanced renal vasoconstriction and resultant vasoocclusion. Recurrent cycles of ischaemia and ischaemia–reperfusion injury thus occur, thereby leading to subclinical and clinical acute kidney injury. These processes summate in the initiation and progression of sickle cell nephropathy
- #18: https://doi.org/10.1111/j.1365-2141.2011.08853.x
- #22: Symptoms develop slowly and aren't specific to the disease Can have no symptoms, but people may experience: Whole body: fatigue, high blood pressure, loss of appetite, malaise, or water-electrolyte imbalance Nausea and vomiting, muscle cramps, loss of appetite, swelling via feet and ankles, dry, itchy skin, shortness of breath, trouble sleeping, urinating either too much or too little
- #24: Urine is an unstable fluid; it changes composition as soon as it is eliminated through micturition.[7] Accurate collection, storage, and handling are crucial to maintaining the sample’s integrity. A complete urinalysis consists of three components or examinations: physical, chemical, and microscopical. Preservatives: Although used occasionally, they can alter the accuracy of the results. Some examples include:Thymol: May generate false-positive reactions for albumin. Formaldehyde: May cause false-positive results for leukocyte esterase, peroxidase reaction, urobilinogen, and glucose if strips are used. Hydrochloric Acid: Although used to preserve cell structures and determine steroid concentrations, it affects the sample's pH. Mercury Salts: May produce false-negative results for leukocyte esterase reaction. Boric Acid: While commonly used to preserve bacteria present in urine, this substance may reduce the sensitivity of the leukocyte reagent on dipsticks and alter initial pH values. Moreover, excessive concentrations may prevent bacterial growth in samples reserved for culture. roteinuria can my categorized as a glomerular pattern, a tubular pattern, and an overflow pattern According to the Kidney Disease Improving Global Outcomes (KDIGO) guidelines, albuminuria can be classified into three stages: A1 (less than 30 mg/g creatinine; normal to mildly increased), A2 (30 mg/g to 300 mg/g creatinine; moderately increased, formerly termed as "microalbuminuria"), and A3 (greater than 300 mg/g creatinine; severely increased) Haematuria Dipstick test for blood detects primarily the peroxidase activity of erythrocytes, but myoglobin and hemoglobin can also catalyze this reaction. Thus, a positive test result indicates hematuria, myoglobinuria, or hemoglobinuria.



































![References
1/29/2024
41
Aeddula NR, Bardhan M, Baradhi KM. Sickle Cell Nephropathy. Ncbi.
2020. Available from https://www.ncbi.nlm.nih.gov . [Date accessed July,
2020]
Alpers CE, Chang A. The Kidney. Robbins and Cotran Pathologic Basis
of Diseases. Saunders Elsevier. Ninth Edition. Chapter 20. Pg 911-919
Inusa BPD, Mariachiara L, Giovanni P, Ataga KI. Sickle Cell
Nephropathy: Current Understanding of the Presentation, Diagnostic
and Therapeutic Challenges. Intechopen. 2018. Available from
https://www.intechopen.com .[Date accessed July, 2020]
Kumar V, Abbas AK, Aster JC. Red Blood Cell and Bleeding Disorders.
Robbins and Cotran Pathologic Basis of Diseases. Saunders Elsevier.
Ninth Edition. Chapter 14. Pg 635
Marshal WJ, Lapsley M, Day A. The Kidneys. Clinical Chemistry.
Elsevier. Eight Edition. Pg 86
Mohan Harsh. The Kidney and Lower Urinary Tract. Textbook of
Pathology. Jaypee. Seventh Edition. Chapter 20. Pg 636-638
Pham PT. Renal Manifestations of Sickle Cell Disease. Medscape.
2019. Available from http://emedicine.medscape.com. [Date accessed
July, 2020]](https://image.slidesharecdn.com/biochemicalinvestigationsandmanagementofsicklecellnephropathy-240129160413-631f7e64/85/Biochemical-investigations-and-management-of-sickle-cell-nephropathy-pptx-41-320.jpg)
![References
1/29/2024
42
Bukar, A. A., Sulaiman, M. M., Ladu, A. I., Abba, A. M., Ahmed, M. K., Marama, G. T., & Abjah, U. M. (2019).
Chronic kidney disease amongst sickle cell anaemia patients at the University of Maiduguri Teaching
Hospital, Northeastern Nigeria: A study of prevalence and risk factors. Mediterranean Journal of Hematology
and Infectious Diseases, 11(1).
Yusuf, R., Hassan, A., Ibrahim, I. N., Babadoko, A. A., & Ibinaiye, P. O. (2017). Assessment of kidney
function in sickle cell anemia patients in Zaria, Nigeria. Sahel Medical Journal, 20(1), 21.
Nnaji, U. M., Ogoke, C. C., Okafor, H. U., & Achigbu, K. I. (2020). Sickle cell nephropathy and associated
factors among asymptomatic children with sickle cell anaemia. International Journal of Pediatrics, 2020.
Ocheke, I. E., Mohamed, S., Okpe, E. S., Bode-Thomas, F., & McCullouch, M. I. (2019). Microalbuminuria
risks and glomerular filtration in children with sickle cell anaemia in Nigeria. Italian journal of pediatrics, 45, 1-
6.
BRAIMOH, R. W., Ale, O. K., & Adewunmi, J. A. (2017). Evaluation of urinary tract infection and nephropathy
in adult Nigerians with sickle cell anaemia. Tropical Journal of Nephrology, 12(2), 23-30.
WHO FIFTY-NINTH WORLD HEALTH ASSEMBLY A59/9 Provisional agenda item 11.4 24 April 2006
Aeddula NR, Bardhan M, Baradhi KM. Sickle Cell Nephropathy. [Updated 2022 Sep 12]. In: StatPearls
[Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from:
https://www.ncbi.nlm.nih.gov/books/NBK526017/](https://image.slidesharecdn.com/biochemicalinvestigationsandmanagementofsicklecellnephropathy-240129160413-631f7e64/85/Biochemical-investigations-and-management-of-sickle-cell-nephropathy-pptx-42-320.jpg)