Colorectal Cancer ppt medical surgical nursing .pptx
- 1. Presented By Mrs. Anusha. M 1st Year MSc. Nursing GNCK
- 2. INTRODUCTION Tumors of the colon and rectum are relatively common; the colorectal area (the colon and rectum combined) is now the third most common site of new cancer cases in the United States. It is the second leading cause of cancer death in both men and women. Improved screening strategies have helped reduce the number of deaths from colon cancer in recent years.
- 3. COLORECTAL CANCER •Colorectal cancer is the cancer of colon and rectum. It is related to large intestine. Colon forms the major part of large intestine and rectum is the lower part. •Colorectal cancer is more common in western countries. It occurs more frequently after age 50. The incidence continues to rise with increasing age.
- 4. INCIDENCE In the United States, almost 150,000 new cases and 52,000 deaths from colorectal cancer occur annually. The lifetime risk of developing colorectal cancer is 1 in 17. Incidence increases with age (the incidence is highest in people older than 85 years) and is higher in people with a family history of colon cancer and those with IBD or polyps.
- 5. CANCER •Family h/o colorectal cancer (first-degree relative) •Personal h/o inflammatory bowel disease •Personal h/o colorectal cancer, diabetes mellitus •Family or personal h/o familial adenomatous polyposis (FAP) •Family or personal h/o hereditary nonpolyposis colorectal cancer (HNPCC) syndrome
- 6. RISK FACTORS (Conti…) •H/o gastrectomy •H/o inflammatory bowel disease High-fat, high-protein (with high intake of beef), low- fiber diet •Genital cancer (eg, endometrial cancer, ovarian cancer) or breast cancer (in women) •Obesity (body mass index 30 kg/m²) ≥ •Cigarette smoking •Alcohol ( 4 drinks/wk) ≥
- 7. RISK FACTORS (Conti…) Dietary risk factors for the development of colorectal cancer •Increased risk factor : o Red meat: Carcinogenic amines formed during cooking. o Saturated animal fat o High fecal bile acid and fatty acid levels. o May affect colonic prostaglandin turnover.
- 8. RISK FACTORS (Conti…) •Decreased risk factors o Dietary fibre: Effects vary with fibre type. o Fruit and vegetables: o Green contain anticarcinogens, e.g. glucosinolates and flavonoids. o Little evidence for protection from vitamin A, C, E. o Calcium: Binds and precipitates fecal bile acids. o
- 9. ETIOLOGY The exact cause of colorectal cancer is unknown. Patient suffering from inflammatory bowel disease is at higher risk Family history. Diet and decreased bowel movement has been implicated as a causative factor.
- 10. STAGES OF COLORECTAL CANCER • Stage I Cancer occurs through the superficial lining of the colon or rectum. It does not spread beyond the colon wall or rectum. • Stage II Cancer occurs into and through the wall of the colon or rectum. It does not spread to nearby lymph nodes.
- 11. STAGES OF COLORECTAL CANCER • Stage III Cancer has invaded nearby lymph nodes but it is not affecting other parts of the body. • Stage IV Cancer has spread to distant sites for instance to liver or lung.
- 14. Dukes' Classification-Modified Staging System •Class A: Tumor limited to muscular mucosa and submucosa •Class B₁: Tumor extends into mucosa •Class B₂: Tumor extends through entire bowel wall into serosa or pericolic fat, no nodal involvement •Class C₁: Positive nodes, tumor is limited to bowel wall
- 15. •Class C2: Positive nodes, tumor extends through entire bowel wall •Class D: Advanced and metastasis to liver, lung, or bone Another staging system, the TNM (tumor, nodal involvement, metastasis) classification, may be used to describe the anatomic extent of the primary tumor, depending on: oSize, invasion depth, and surface spread oExtent of nodal involvement
- 16. NM Classification of Colorectal Cance T Primary Tumor Tx Primary tumor cannot be assessed because of incomplete information. Tis Carcinoma in situ. Cancer is in earliest stage and has not grown beyond mucosa layer. T1 Tumor has grown beyond mucosa into the submucosa T2 Tumor has grown through submucosa into muscularis propria. T3 Tumor has grown through the muscularis propria into the subserosa but not to neighboring organs or tissues. T4 Tumor has spread completely through the colon or rectal
- 17. N Lymph Node Involvement Nx Lymph nodes cannot be assessed. N0 No regional lymph node involvement is found. N1 Cancer is found in one to three nearby lymph nodes. N2 Cancer is found in four or more nearby lymph nodes.
- 18. M Metastasis Mx Presence of distant metastasis cannot be assessed. M0 No distant metastasis is seen. M1 Distant metastasis is present.
- 19. PATHOPHYSIOLOGY Cancer occurs in the following areas Cecum, ascending colon, transverse colon, descending colon, Sigmoid colon and rectum All colorectal cancer is adenocarcinomas that begin as adenomatous polyps. All adenomas are dysplastic and considered premalignant lesions even though only 5% actually become malignant.
- 20. Adenomas may present in various shapes and configuration. They are round and polypoid but may be more elongated and have stalks. Infrequently, adenomas appear flat or even depressed over times; lesions penetrate the colon wall and extend into surrounding tissue. Most tumors develop in the rectum and sigmoid colon, although any portion of
- 21. Tumors grow undetected until symptoms slowly and insidiously appear. • Disease spread by several methods. • It may spread locally into deeper layers of the bowel wall, reaching the serosa and mesenteric fat. • Tumors may enlarge in the lumen of bowel and spread through the lymphatics' or circulatory system.
- 22. Liver and lungs are the major organs of metastasis. Other includes adrenal glands, kidneys, skin, bone and brain. In addition to direct invasion and spread through the lymphatic and circulatory system, It can also spread by peritoneal seeding during surgical resection of the tumor. Seeding of the tumor can occur when the tumor extends through the serosa or during
- 24. CLINICAL MANIFESTATIONS CRC has an insidious onset, and symptoms do not appear until it is advanced. Common manifestations include iron-deficiency anemia, rectal bleeding, abdominal pain, change in bowel habits, and intestinal obstruction or perforation. Physical findings may include the following: Early disease: Nonspecific findings (fatigue, weight loss) or none at
- 25. More advanced : Abdominal tenderness, palpable abdominal mass, hepatomegaly, ascites Bleeding occur both right-and left-sided CRC. Bleeding on the right side, more common than the left, is often unrecognized and an early manifestation is often anemia. Hematochezia (fresh blood in the stool) often caused by left-sided CRC than right-sided CRC. Right-sided lesions are more likely to cause diarrhea, while left-sided tumors usually
- 26. DIAGNOSTIC EVALUATION Medical history or physical examination Complete blood count Fecal occult blood Sigmoidoscopy or colonoscopy Biopsy. Chest X-ray Ultrasonic examination, CT scan, MRI Carcino embryonic antigen levels
- 27. MANAGEMENT Chemotherapy Targeted therapy Immuno therapy Radiation therapy Surgical therapy • Right hemicolectomy • Left hemicolectomy • Abdominal-perineal resection • Laparoscopic colectomy
- 28. CHEMOTHERAPY • Use of drugs helps to destroy the cancer cells. • Used before surgery to shrink a large cancer, so that it is easier to remove. • Given after surgery to eliminate any remaining cancer cells. • 5-Fluorouracil (5-FU) with levamisole is recommended as standard therapy for specific stages of disease, e.g. stage III to
- 29. • Capecitabine, a form of 5-FU. • After surgery, chemotherapy is used to control symptoms of metastasis and reduce metastatic spread. • Intra hepatic arterial chemotherapy, often with 5-FU may be administered to patient with liver metastasis. • Chemotherapy also used to relieve symptoms of colorectal cancer which cannot be removed with surgery.
- 30. TARGETED THERAPIES •Bevacizumab (Avastin): Treat advanced colorectal cancer. It is given with chemotherapy. •Regorafenib: Treat patient with metastatic colorectal cancer who has already received certain types of chemotherapy. •Epidermal growth factor: Receptor inhibitors, such as cetuximab and panitumumab. Recommended for stopping
- 31. IMMUNOTHERAPY Immunotherapy is also known as biologic therapy. A drug which uses immune system to fight cancer is known as immunotherapy. •Pembrolizumab: It is prescribed to treat metastatic colorectal cancer. •Nivolumab: It is used to treat patients who are 12 or older and have MSI-H or dMMR metastatic colorectal cancer.
- 32. RADIATION THERAPY •Preoperative radiation may be administered to patient who has large colorectal cancer. •Aids in certain more definite tumor margins, which facilitates resection of the tumor during surgery. •Uses X-rays and protons which kills the cancer cells. •Used to shrink the large cancer cells before surgery.
- 33. SURGICAL THERAPY Goals of surgical therapy include: •Complete resection of the tumor •A thorough exploration of the abdomen to determine if cancer has spread •Removing all lymph nodes that drain the area where the cancer is located •Restoring bowel continuity so that normal bowel function return •Preventing surgical complications.
- 34. Laparoscopic Surgery •Some patients able to have laparoscopic surgery. •It allows surgeon to carry out surgery through four or five small cuts in patient's abdomen while a patient is under anesthesia. •A telescope camera is inserted into one, through these cuts. It shows an enlarged image of an internal abdominal organ on a screen. •For removal of cancer, laparoscopic surgery is
- 35. Colostomy A colostomy is a surgical procedure that brings one end of the large intestine out through the abdominal wall. It may be temporary or permanent.
- 36. Indications of Colostomy • Cancer of colon/rectum. • Intestinal obstruction. • Diverticular disease. • Hirschsprung's disease (a condition affects the large intestine and causes problem with passing stools) • Crohn's disease. • Ulcerative disease. • Trauma to abdomen.
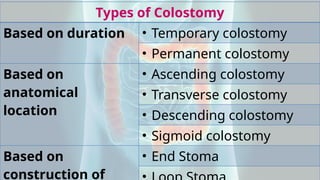
- 37. Types of Colostomy Based on duration • Temporary colostomy • Permanent colostomy Based on anatomical location • Ascending colostomy • Transverse colostomy • Descending colostomy • Sigmoid colostomy Based on construction of • End Stoma
- 38. According to Duration 1.Temporary colostomy: Made to allow colon to rest and heal for a period of time. Kept for weeks, months or years. Once, definitive surgery is done, temporary colostomy is closed and bowel movements will return to normal. 2.Permanent colostomy: A part of colon is removed cannot be used again. Acc. disease/abnormality of intestine, stoma is
- 39. According to Anatomic Location 1.Ascending colostomy: Made on right side of abdomen. Fecal matter - liquid form. 2.Transverse colostomy: Located in upper abdomen towards middle or right side. Fecal content-loose/soft. 3.Descending colostomy: Present on lower left side of abdomen. Fecal content - firm and drain 4.Sigmoid colostomy: Made in sigmoid colon, few inches lower than descending colostomy. Fecal matter - normal stool. Frequency of fecal
- 41. According to Construction of Stoma 1. End stoma: When the proximal end of the bowel is brought to the outside of abdominal wall. If an abdominal perineal resection is done, the rectum is removed and the proximal sigmoid or descending colon is brought out as a stoma. 2. Loop stoma: A loop of bowel, usually the transverse colon, is pulled outside the abdominal wall and a bridge is slipped under the loop to hold it in place. An incisional slit is made on the top of the exposed colon to allow stool to exit
- 42. 3. Double-barrel stoma: Bowel is completely dissected and both ends of the colon are brought to the outside of abdominal wall to form two separate stomas. The proximal stoma is the functioning stoma that expels stool. A double-barrel stoma is often temporary, allowing the bowel to rest during healing after trauma or surgery
- 44. • A common temporary colostomy procedure. • Often performed when a temporary colostomy is required. • Performed in an emergency situation for disease of sigmoid colon or rectum including cancer diverticulitis. • Bowel is fused from its attachment within the abdominal cavity. • Bowel is then cut and diseased segment is removed. • Colon brought out through the abdominal wall and stitched to the skin as colostomy.
- 45. COMPLICATIONS •Bowel perforation with resultant peritonitis, •Abscess formation. •Fistula formation to the urinary bladder or the vagina •Bleeding •Obstruction
- 46. Type of feces according to site of colostomy Location of stoma Type of effluent Ileostomy Liquid to mushy Cecostomy, ascending colostomy Liquid to mushy, foul odor Right transverse colostomy Mushy to semi formed Left transverse Semi formed soft
- 47. NURSING MANAGEMENT •Educate patient & family members about colorectal cancer. •Assess location of stoma & type of colostomy performed. •Teach about surgical procedures to patient and significant others. •A nurse ensures patient has adequately prepared for abdominal surgery and general anesthesia. •Effects of chemotherapy and radiation
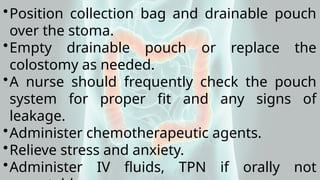
- 48. •Position collection bag and drainable pouch over the stoma. •Empty drainable pouch or replace the colostomy as needed. •A nurse should frequently check the pouch system for proper fit and any signs of leakage. •Administer chemotherapeutic agents. •Relieve stress and anxiety. •Administer IV fluids, TPN if orally not
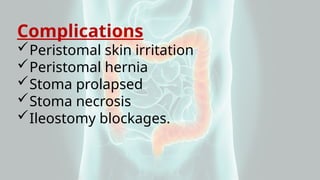
- 49. Complications Peristomal skin irritation Peristomal hernia Stoma prolapsed Stoma necrosis Ileostomy blockages.
- 50. Colostomy Care Whether temporary or permanent, a colostomy can be very distressing to the patient. Patients with colostomies require encouragement, understanding and assistance in overcoming the negative emotions associated with a colostomy and in learning independence and self sufficiency in living with a colostomy.
- 51. Assessment 1. Stoma color. 2. Size and shape. 3. Stomal bleeding. 4. Any redness and irritation of the peristomal skin. 5. Amount and type of feces. 6. The patient's and family members' learning needs regarding the colostomy and selfcare. 7. The patient's emotional status, especially strategies used to cope with the ostomy. 8. The used appliance for leakage of effluent.
- 52. Assemble Equipment and Supplies •Disposable gloves. •Electric or safety razor. •Bedpan •Solvent •Moisture proof bag. •Cleaning materials, including tissues, warm water, mild soap optional, washcloth or cotton balls and towel. •Tissue or gauze pad.
- 53. •Skin barrier. •Stoma measuring guide. •Pen or pencil and scissors. •Clean colostomy appliance with optional belt. •Tail closure clamp. •Special adhesive, if needed. •Stoma guide strip, if needed. •Deodorant (liquid or tablet) for a non odor proof colostomy bag.
- 54. Procedure Check physician's order and patient's identification. Explain procedure to the patient. Wash hands and apply clean gloves. Provide for patient privacy. Assist the patient to a comfortable sitting or lying position in bed or preferably, a sitting or standing position in the bathroom. Shave the peristomal skin as needed. Use an
- 55. • Empty pouch through the bottom opening into a bedpan. • Assess consistency and amount of effluent. • Peel the bag off slowly by holding the patient's skin taut • If the appliance is disposable, discard it in a moisture proof bag. Clean and dry the peristomal skin and stoma: • Use toilet tissue to remove excess stool • Use warm water, mild soap (optional) and cotton balls or a washcloth and towel to clean the skin and stoma.
- 56. Assess the stoma and peristomal skin: • Inspect the stoma for color, size, shape and bleeding. • Inspect the peristomal skin for any redness, ulceration or irritation. • Place a piece of tissue or gauze pad over the stoma and change abnormal stoma color, as needed. Apply paste type skin barrier, if needed: • Fill in abdominal creases or dimples with paste. • Allow the paste to dry for 1 to 2 minutes or as recommended by the manufacturer. • Prepare and apply the skin barrier (peristomal
- 57. For a solid water or disc skin barrier •Use the guide to measure the size of the stoma. •On the backing of the skin barrier, trace a circle the same size as the stomal opening. •Cut out the traced stoma pattern to make an opening in the skin barrier. •Make the opening not more than 0.3-0.4 cm (1/8- 1/6 in) larger than the stoma. •Remove the backing to expose the sticky adhesive side. •Center the skin barrier over the stoma and gently press it onto the patient's skin, smoothing out any
- 58. • Either wipe or apply the product evenly around the peristomal skin to form a thin layer of the liquid plastic coating to the same area. • Allow the skin sealant to dry until it no longer feels tacky. Fill any exposed skin around an irregularly shaped stoma: • Apply paste to any exposed skin areas. • Use a non-alcoholic based product, if the skin is excoriated. • Sprinkle peristomal powder on the skin, wipe off the excess and dab the powder with slightly moist
- 59. Remove the tissue over the stoma before applying the pouch. For a disposable pouch with adhesive square • If the appliance does not have a precut opening, trace a circle 0.3-0.4 cm (1/8-1/6 in) larger than the stoma size on the appliance's adhesive square. • Cut out a circle in the adhesive. • Peel off the backing from the adhesive seal. • Center the opening of the pouch over the patient's stoma and apply it directly onto the
- 60. •Gently press the adhesive backing onto the skin and smooth out any wrinkles, working from the stoma outward. •Remove the air from the pouch. •Place a deodorant on the pouch (optional). •Close the pouch by turning up the bottom a few times, fanfolding its end lengthwise and securing it with a tail closure clamp.
- 61. adhesive disc to the faceplate of the appliance. • Insert a coiled paper guide strip into the faceplate opening. • The strip should protrude slightly from the opening and expand to fit it • Using the guide strip, center the faceplate over the stoma. • Firmly press the adhesive seal to the peristomal skin. • Place a deodorant in the bag, if the bag is not odor- proof. • Close the end of the pouch with the designated
- 62. Discard a disposable bag If feces are liquid, measure the volume. Note the feces character, consistency and color Wash reusable bags with cool water and mild soap, rinse and dry. Wash the soiled belt with warm water and mild soap, rinse and dry. Remove and discard gloves. Document the procedure in the patient's record. Report and record:
- 63. Colostomy Irrigation Irrigation should be done at the same time each day in order to establish regularity of bowel evacuation. Unless contraindicated or otherwise ordered by the physician, it is best to establish a routine of daily irrigation in accordance with the patient's former bowel habits..
- 64. Articles Required a. Irrigation kit (irrigation bag with clamp and tubing, cone tip irrigation catheter, irrigation drain pouch). b.Water soluble lubricant. c. IV pole (or other suspending hook). d.Soap and water. e. Washcloth and towel. f. Ostomy appliance. g.Waste receptacle. h.Prescribed irrigating solution, usually 500-1000 ml warm (100-105°F) tap water.
- 65. •Review the procedure with the patient, if necessary. •Wash hands and don gloves. •Provide privacy to patient. •If the patient is ambulatory, have the patient sit on the toilet or on a chair facing the toilet. If the patient is bedridden, elevate the head of the bed 45-90° and position rubber sheet around the patient. •Fill the irrigation bag with the prescribed
- 66. •The bottom of the bag should be at the patient's shoulder level when he/she is seated to prevent fluid from entering the bowel too rapidly. •The bottom of the bag should be placed 18 to 20 inches above the stoma when the patient is in bed. •Open the clamp on the irrigation tubing and allow the solution to fill the tubing. Reclamp (This prevents the administration of air into
- 67. •Remove the Ostomy pouch, if applicable and place the irrigation drain pouch over the stoma. (Attach stoma belt, if required). •Place the bottom, open end of the irrigation drain pouch in the toilet (or bedpan) to facilitate drainage by gravity. •Connect the cone tip catheter to the tubing and flush with solution. •Lubricate the cone with the water soluble lubricant to avoid irritating the mucous
- 68. •Lubricate the cone with the water soluble lubricant to avoid irritating the mucous membranes. •Gently insert the cone into the stoma, so that the stoma is occluded. •Unclamp the irrigating tubing and allow the water to flow in slowly. •Allow water to enter the colon over a period of 10 to 15 minutes.
- 69. •If cramping occurs, slow down the flow rate and ask patient to deep breathe until cramps subside. Cramping during irrigation may indicate that: i. The bowel is ready to empty. ii. The water is too cold. iii. The flow is too fast. iv. The tube contains air. •Clamp the catheter and remove from the stoma. Fold down the top opening of the
- 70. toilet for about 15 to 20 minutes so the initial colostomy re- turns can drain into the toilet. (If the patient is on bed rest, allow the colostomy to drain into the bedpan). •Close the colostomy irrigation drain pouch with a rubber band or pouch clip, then ambulate the patient or return him/her to bed. a.Ambulating stimulates elimination, producing improved irrigation return. b.Have the non-ambulatory patient lean forward or massage his/her abdomen to
- 71. •Wait approximately 1 hour for the rest of the colostomy return, then remove the irrigation drain pouch from the patient. •Gently clean the area around the stoma with mild soap and water. •Be careful not to rub the skin. •Rinse and dry the area with a towel. •Apply a clean pouch or dressing, as applicable. •Provide for the patient's comfort. •Remove and dispose off used supplies.
- 72. •Record the procedure and significant nursing observations in the patient's clinical record and report it to incharge nurse. a.Note color and condition of stoma and peristomal skin. b.Record color, consistency and amount of drainage. c. Note amount of irrigating solution used. •As recovery progresses, the nursing personnel should gradually assume a more passive role in colostomy care, allowing the patient to assume
- 75. Nursing Diagnosis •Acute pain related to surgical intervention. •Risk for impaired skin integrity related to fecal drainage and pouch adhesive. •Imbalanced nutrition: Less than body requirements related to decreased appetite. •Fear or anxiety related to knowledge deficit. •Disturbed body image related to colostomy.
- 76. CONCLUSION Patients have more treatment choices today. Early detection increases the chance of cure. The evolving colorectal cancer treatments improve the survival in colorectal cancer patients. Biomarker can predict the patient's response to targeted therapies. Future studies to explore more predictive biomarkers in the cancer treatment to identify the right patient to receive tailored targeted therapy.