O2 insufficiency
- 1. OXYGEN INSUFFICIENCY Presented by: Ms. Priyanka Kumari F.Y. M.Sc. Nursing
- 2. Specific Objective Discuss factor effecting the oxygenation. Define oxygen insufficiency. Explain the etiology of oxygen insufficiency. List down the signs and symptoms of oxygen insufficiency. Explain the diagnostic evaluation of oxygen insufficiency. Enlist the complications of oxygen insufficiency. Discuss the management of patient with oxygen insufficiency. Discus the nursing management of patient with oxygen insufficiency.
- 4. 1. Environmental Factors: Environmental factors can influence oxygenation. The incidence of pulmonary disease is higher in urban areas than in rural areas. The client’s work place may increase the risk for pulmonary disease.
- 5. SOURCES OF AIR POLLUTION 1.Automobiles 2.Industries 3.Domestic sources 4.Miscellaneous
- 6. HEALTH ASPECTS The health effects of air pollution are both immediate and delayed. Immediate effects are borne by the respiratory system, resulting state is acute bronchitis. If the air – pollution is intense, it may result even in immediate death by suffocation.
- 7. 2. PHYSIOLOGICAL FACTORS Decreased oxygen – carrying capacity Decreased inspired oxygen concentration Increased metabolic rate
- 8. 3. DEVELOPMENT FACTORS Neonate and Infants. Toddlers, School age children and adolescents Young and middle – age adults Other adults
- 9. 4. LIFESTYLE RISK FACTORS: Nutritional factors. Medications. Physiological health. Levels of health.
- 10. Exercise. Smoking. Substance abuse.
- 11. MEANING OF OXYGEN A colorless, odorless gas constituting one fifth of the atmosphere. 21% of oxygen present in the atmospheric air. DEFINITION OF OXYGENATION Oxygenation is a process which occurs in the lungs to the hemoglobin of blood, which is saturated with oxygen to form oxyhemoglobin.
- 13. MEANING OF OXYGEN INSUFFICIENCY : Sufficient amount of oxygen is not getting the organs to maintain their functions.
- 14. ETIOLOGY Decreased hemoglobin & oxygen carrying capacity of blood. Diminished concentration of inspired oxygen. Inability of the tissue to extract oxygen from the blood.
- 15. Decreased diffusion of oxygen from the alveoli to the blood as within pneumonia. Poor tissue perfusion with oxygenated blood. Impaired ventilation.
- 16. OXYGEN INSUFFICIENCY OCCURS DUE TO SOME DISEASE
- 17. MUSCULOSKELETALABNORMALITIES: Musculoskeletal impairments in the thoracic region reduce oxygenation. Such impairments may result from abnormal structural configuration, trauma, muscular diseases and disease of central nervous system.
- 18. TRAUMA: The person with multiple rib fracture can develop a flail chest, a condition in which fractures cause instability in part of the chest wall. The instable chest wall allows the lung underlying the injured area to contract on inspiration and bulge on expiration, resulting in hypoxia.
- 19. NEUROMUSCULAR DISEASES: Disease such as muscular dystrophy affects oxygenation of tissue by decreasing the client’s ability to expand and contract the chest wall. Ventilation is impaired and hypercapnia and hypoxemia can occur.
- 20. CENTRAL NERVOUS SYSTEM ALTERATIONS: Disease or trauma involving the medulla oblongata and spinal cord may result in impaired respiration. When the medulla oblongata is affected neural regulation of respiration is damaged and abnormal breathing patterns may develop.
- 21. MYOCARDIAL ISCHEMIA: When blood supply to the myocardium from the coronary arteries is insufficient to meet the oxygen demand of the organ, two common manifestations of this ischemia are angina pectoris and myocardial infarction.
- 22. Angina pectoris is usually a transient imbalance between myocardial oxygen supply and demand. The pain can last for 1 to 15 minutes. Chest pain may be left sided or substernal and may radiate to the left or both arms and to the jaw, neck and back.
- 23. Myocardial infraction (MI) sudden decrease in coronary blood flow or an increase in myocardial oxygen demand without adequate coronary perfusion. Infarction occurs because of ischemia and necrosis of myocardial tissue.
- 24. HYPOVENTILATION: It occurs when alveolar ventilation is inadequate to meet the body’s oxygen demand or to eliminate sufficient carbon dioxide. HYPOXIA: Hypoxia is inadequate tissue oxygenation at the cellular level. This can result from a deficiency in oxygen delivery or oxygen utilization at the cellular level.
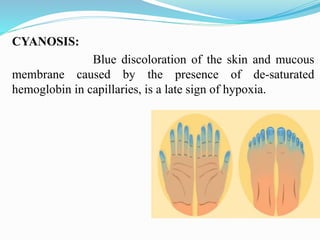
- 25. CYANOSIS: Blue discoloration of the skin and mucous membrane caused by the presence of de-saturated hemoglobin in capillaries, is a late sign of hypoxia.
- 26. CEREBRAL PALSY: Cerebral palsy is a non-progressive neurological disorder that is present from birth and usually involves motor function.
- 27. SYNCOPE: Temporary loss of consciousness, feeling faint. It may indicate decreased cardiac output, fluid deficit or defects in cerebral perfusion. Syncope frequently occurs as a result of postural hypotension.
- 28. DIAGNOSIS EVALUATION OF THE PATIENT THAT WHO IS HAVING OXYGEN INSUFFICIENCY
- 29. HISTORY COLLECTION: Nursing history should focus on the client’s ability to meet oxygen needs. History for cardiac function includes pain, dyspnea, fatigue, peripheral circulation, cardiac risk factors, presence of past or current conditions.
- 31. MEASUREMENT NORMAL RANGE CLINICAL SIGNIFICANCE Tidal volume (Vt) Volume of air inhaled or exhaled per breath. Residual volume (Rv) Volume of air left in lungs after a maximal exhalation. Functional residual capacity Volume of air left in lungs after a normal exhalation. 500 ml 1000 – 1200 ml 2000 – 2400 ml Decreased in restrictive lung disease and older client. Increase in clients with COPD and older clients due to decreased respiratory muscle mass, strength, elastic recoil and chest wall compliance. Increased in clients, with COPD and older clients due to decreased respiratory muscle mass, strength, elastic recoil and chest wall compliance.
- 32. MEASUREMENT NORMAL RANGE CLINICAL SIGNIFICANCE Vital capacity Volume of air exhaled after a maximal inhalation Total lung capacity(TLC) Total volume of air in lungs following a maximal inhalation 4500 – 4800 ml 5000 – 6000 ml Decreased in pulmonary edema atelectasis and changes associated with a giving. Decreased in restrictive lung disease increase in obstructive lung disease.
- 33. ARTERIAL BLOOD GAS: Measures the hydrogen concentration partial pressure of carbon dioxide, partial pressure of oxygen, oxygen concentration.
- 34. SPIROMETRY: Spirometry measure, the volume of air in liters exhaled or inhaled by a patient over time.
- 35. PULSE OXIMETRY CHEST X – RAY: Usually posterior-anterior and lateral films are taken to adequately visualize all of the lung fields. Radiography of the thorax is used to observe the lung field for fluid (pneumonia), masse (lung cancer), other abnormal process.
- 37. BREATHING EXERCISES DEEP BREATING EXERCISES: When hypoventilation occur a decreased amount of air enters and leaves the lungs. However deep – breathing exercises can be used to overcome hypoventilation.
- 38. ABDOMINALAND PURSED LIP BREATHING- Assume comfortable semi-sitting position in a bed or chair or a lying position in bed with one pillow. Flex your knees to relax the muscle of abdomen. Place one or both hands on your abdomen just below the ribs.
- 39. Breath in deeply through the nose keeping the mouth closed. Concentrate on feeling or skin and tighter the abdomen muscle breathing out to enhance effective exhalation. If indicated, cough two or more time during exhalation. Use this exercise whenever feeling short of breath and increase gradually to 5 – 10 minutes a day.
- 40. NEBULISATION: Nebulization is a process of adding moisture or medication to inspired air by mixing particle of varying sizes with air. Purpose To relieve respiratory insufficiency due to bronchospasm. To correct the underlying respiratory disorder responsible bronchospasm.
- 41. To liquefy and remove retained thick secretion form the lower respiratory tract. To reduce inflammatory and allergic response in the upper respiratory tract. To correct humidity deficit.
- 42. CHEST PHYSIOTHERAPY Chest physiotherapy is a group of therapies used in combination to mobilize pulmonary secretion. These therapies include postural drainage, chest percussion and vibration. Chest physiotherapy should be followed by productive coughing and suctioning of the client who has a decreased ability to cough.
- 43. Positional drainage is use of positioning technique that draw secretions form specific segments of the lungs and bronchi into the trachea. Coughing or suctioning normally removes secretion from the trachea.
- 44. SUCTIONING: The suctioning technique includes oropharyngeal and nasopharyngeal suctioning. Oro-tracheal and naso- tracheal suctioning should perform after suctioning of the oropharynx trachea, by using a rounded – tipped catheter.
- 45. OXYGEN THERAPY: Oxygenation by applying an oxygen mask Nasal catheter Oxygen tent Oxygen therapy in the home
- 47. NURSING MANAGEMENT Nursing care plan of patient with oxygen insufficiency according to prioritize the problem on the basis of:
- 48. Ineffective Airway clearance: May be related to: Obstruction of airway by the tongue. Upper airway obstruction caused by edema of larynx or glottis.
- 49. Obstruction of trachea or a bronchus by foreign body aspiration. Partial occlusion of the bronchi and bronchioles by infection. Occlusion of the more distal airways by association with emphysema.
- 50. Goal: To promote airway clearance. To maintain a patent airway. Nursing intervention: Teach effective coughing: Effective coughing should be preceded by slow, deep breaths.
- 51. Assisting the client to a sitting position. Provide oral care. Assess the sputum produced by coughing, noting the amount, color and odor. Initiate postural drainage and chest physiotherapy. Monitor hydration status of the client.
- 52. Administer the prescribed medication. Monitor environment and lifestyle conditions. Introduce artificial airways in case where obstruction cannot be removed. (nasal airways, oral airways)
- 53. Ineffective breathing pattern: May be related to: Restricted pulmonary disease or CNS disorder or thoracic surgery. Any major abnormal or thoracic surgery or whose mobility is restricted.
- 54. Neuromuscular disease that can weaken the respiratory muscles. Abnormal curvature like alteration of spine.
- 55. Goal: To promote lung expansion. To improve breathing pattern. Intervention: To provide proper positioning. Teach controlled breathing exercises. Introduced chest drainage system.
- 56. Impaired gas exchange: May be related to: Ventilation perfusion mismatching. Widespread shunting as with atelectasis and pneumonia.
- 57. Goal: To improve oxygen uptake and delivery. Intervention: Administer oxygen to the client.
- 58. Decreased cardiac output: This may be related to CHF causing pulmonary edema, heart failure or shock. Goal: To maintain a normal cardiac output.
- 59. Intervention: Manage fluid balance by: Limited sodium and reduced fluid intake in case of CHF. Give diuretics. Maintaining daily weight and intake output. Monitoring electrolyte balance if the client is receiving
- 60. CURRENT TREND “Comparison of Mask Oxygen Therapy and High-Flow Oxygen Therapy after Cardiopulmonary Bypass in Obese Patients” By- Mazlum Sahin. Background To clarify the efficiency of mask O2 and high-flow O2 (HFO) treatments following cardiopulmonary bypass (CPB) in obese patients.
- 61. Methods During follow-up, oxygenation parameters including arterial pressure of oxygen (PaO2), peripheral oxygen saturation (SpO2), and arterial partial pressure of carbon dioxide (PaCO2) and physical examination parameters including respiratory rate, heart rate, and arterial pressure were recorded respectively. Presence of atelectasis and dyspnea was noted. Also, comfort scores of patients were evaluated.
- 62. Results: Mean duration of hospital stay was 6.9 ± 1.1 days in the mask O2group, whereas the duration was significantly shorter (6.5 ± 0.7 days) in the HFO group (p= 0.034). The PaO2values and SpO2 values were significantly higher, and PaCO2 values were significantly lower in patients who received HFO after 4th, 12th, 24th, 36th, and 48th hours. In postoperative course, HFO leads patients to achieve better postoperative FVC (p < 0.001).
- 63. Conclusion: Our study demonstrated that HFO following CPB in obese patients improved postoperative PaO2, SpO2, and PaCO2 values and decreased the atelectasis score, reintubation, and mortality rates when compared with mask O2.
- 64. Oxygen is very essential component for living things so as a nurse it is fundamental to assess the level of oxygen in body, and if it is less than necessary action should be taken.
- 65. Bibliography Suzanne .C. Smeltzer, Brenda Bare (2004) “Brunner & Suddarth’s text book of medical surgical nursing” published by Lippincott Williams and wilkins 10th edition. Page no 577, 600,601. Potter and Perry (2005) “Fundamental of nursing” Elsevier Publisher, 6th edition. Page no 1068 – 1071. Navdeep Kaur Brar, HC Rawat (2017) “Textbook of Advanced Nursing Practice” JAYPEE Publications 1st edition. Page no 317-334. https:/www.ncbi.nlm.nih.gov > pubmed.